doi: 10.56294/mw2023101
ORIGINAL
Evaluating the Impact of Simulation-Based Training on Nursing Student Clinical Decision-Making Skills
Evaluación del impacto de la formación basada en la simulación en las habilidades de toma de decisiones clínicas de los estudiantes de enfermería
Malathi H1 ![]() *,
Ashutosh Niranjan2
*,
Ashutosh Niranjan2 ![]() , Sasmita Das3
, Sasmita Das3 ![]()
1JAIN (Deemed-to-be University), Department of Biotechnology and Genetics. Bangalore, Karnataka, India.
2Noida International University, Department of General Surgery. Greater Noida, Uttar Pradesh, India.
3SUM Nursing College, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Medical Surgical Nursing. Bhubaneswar, Odisha, India.
Cite as: H M, Niranjan A, Das S. Evaluating the Impact of Simulation-Based Training on Nursing Student Clinical Decision-Making Skills. Seminars in Medical Writing and Education. 2023; 2:101. https://doi.org/10.56294/mw2023101
Submitted: 03-09-2022 Revised: 15-12-2022 Accepted: 22-02-2023 Published: 23-02-2023
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Malathi H *
ABSTRACT
Nursing students must be able to make clinical decisions that have a direct impact on patient outcomes and quality of care. Traditional clinical training may not provide sufficient hands-on experience in complex or high-risk situations. Simulation-based training (SBT) provides a controlled environment where students can practice clinical decision-making (CDM), but its direct impact on decision-making competence requires further research. To evaluate the ability of SBT to improve nurse trainees’ competence in CDM. To compare progress in reaction time, critical thinking, problem-solving, confidence, and decision-making before and after simulation training. A quasi-experimental pre-test/post-test approach was used, with nursing students in the clinical training phase. Participants underwent high-fidelity simulation (HFS) scenarios to evaluate their decision-making ability. Data were gathered by structured observational checklists, self-reported confidence questionnaires, and performance evaluations. ANOVAs and paired t-tests were used to compare the results before and after the intervention. Results showed that SBT significantly improved nursing students’ ability to evaluate critical thinking, their level of confidence, and their ability to respond time effectively under pressure. The findings demonstrated that following the intervention, decision-making abilities significantly improved; SBT is an effective educational technique to help nursing students improve their CDM skills.
Keywords: Nursing Students; Clinical Decisions; SBT; Training Phase.
RESUMEN
Los estudiantes de enfermería deben ser capaces de tomar decisiones clínicas que tengan un impacto directo en los resultados de los pacientes y en la calidad de los cuidados. La formación clínica tradicional puede no proporcionar suficiente experiencia práctica en situaciones complejas o de alto riesgo. La formación basada en la simulación (SBT) proporciona un entorno controlado en el que los estudiantes pueden practicar la toma de decisiones clínicas (CDM), pero su impacto directo en la competencia para la toma de decisiones requiere más investigación. Evaluar la capacidad del SBT para mejorar la competencia de los estudiantes de enfermería en la toma de decisiones clínicas. Comparar el progreso en el tiempo de reacción, el pensamiento crítico, la resolución de problemas, la confianza y la toma de decisiones antes y después del entrenamiento con simulación. Se utilizó un enfoque cuasi-experimental de pre-test/post-test, con estudiantes de enfermería en la fase de formación clínica. Los participantes se sometieron a escenarios de simulación de alta fidelidad (HFS) para evaluar su capacidad de toma de decisiones. Los datos se recopilaron mediante listas de control de observación estructuradas, cuestionarios de confianza autoinformados y evaluaciones del rendimiento. Se utilizaron ANOVA y pruebas t pareadas para comparar los resultados antes y después de la intervención. Los resultados mostraron que el SBT mejoró significativamente la capacidad de los estudiantes de enfermería para evaluar el pensamiento crítico, su nivel de confianza y su capacidad para responder al tiempo eficazmente bajo presión. Los resultados demostraron que, tras la intervención, las capacidades de toma de decisiones mejoraron significativamente; el SBT es una técnica educativa eficaz para ayudar a los estudiantes de enfermería a mejorar sus habilidades de MDL.
Palabras clave: Estudiantes de Enfermería; Decisiones Clínicas; SBT; Fase de Entrenamiento.
INTRODUCTION
Clinical decision-making serves as the most essential skill for nursing students because it directly influences patient health together with overall care quality. Transitioning from complex clinical cases requires healthcare practitioners to use their essential knowledge to find successful interventions for patients.(1) The acquisition of clinical decision-making skills forms a core part of nursing student education while serving as a professional competency assessment. The process demands a direct understanding of CDM together with critical thinking and clinical reasoning that emerge from rigorous education and practical experience under continuous mentorship.(2) It was emphasized that clinical decision-making is not a linear process but a dynamic and complex skill that develops as students gain experience.(3) New nurses use formal rules and guidelines, whereas experienced nurses use intuition and a more gestalt knowledge of clinical situations. Therefore, nursing students must be accustomed to a range of medical circumstances that test their cognitive and decision-making skills.(4) This can be enabled through simulation learning, which makes it possible to have a simulated environment of control whereby students can practice and enhance their decision-making skills without compromising real patients.(5)
Simulation learning is increasingly seen as an effective educational tool to enhance CDM. By simulating real-life scenarios, students are empowered to think critically, prioritize patient care, and examine outcomes in a risk-free environment.(6) Simulation provides an excellent opportunity for students to reflect and critique, helping them to identify areas for improvement and increase their confidence. Such sessions promote active learning and problem-solving, and simulation-based nursing students are more competent in CMD.(7) In addition, the role of trainers in the development of CDM cannot be overemphasized. Faculty who utilizes a combination of theoretical and practical pedagogical methods case-based learning, discussion, and reflective practice can have a significant impact on the development of these key skills in students. With the continuing development of nursing education, new method must be sought out to enhance the CDM student’s capabilities, enabling them to better respond to the complex and unpredictable dynamics of practice within the healthcare setting.(8) A major challenge in developing CDM skills in students of nursing is the complexity of real-world clinical scenarios that require a balance of knowledge, critical thinking, and experience. Students face difficulties making correct and timely decisions with confidence because limited case exposure interacts with inadequate feedback in high-pressure environments.
Computer-based scenarios were found to affect nursing students’ decision-making capacity.(9) 112 students who participated in a course on medical care were divided into two groups and given either paper-based or computer-based situations to complete. The findings indicated that the computer-based group’s decision-making scores were noticeably higher. The brief evaluation period was a drawback that could have an impact long-term learning outcome. To examined the impact of organized pre-simulation training on nursing students’ learning outcomes. An 80-student pilot project revealed that the participants in the experiment showed significant improvements in clinical judgment, decision-making, and confidence.(10) Independent t-tests confirmed the significance of the findings. Despite the success of the evaluation, its generalizability is tempered by the fact that it focused on a single university.
The research evaluated that nursing students’ clinical performance and competency were affected by simulation-based learning (SBL).(11) Data was gathered using a contrast group design with practicum grades and surveys. Although there was no change in clinical performance, the results indicated considerable gains in skills. One major drawback was the requirement for more investigation into how SBL affects practical application. Nursing experiences of students with simulated learning and its connection to clinical practice were investigated.(12) Through thematic analysis of eight focus group interviews with 32 students, three main themes emerged: improved collaboration, improved clinical skills, and increased confidence. Although effective, there were drawbacks, such as the need for a more diverse participants and the potential for self-report bias.
The objective was to investigate effect of cognitive biases on CDM in simulations.(13) It examined healing and decision-making during debriefings and created situations to elicit biases. Bias was found in 55 % of the 20 sessions and some of them did not recover. Limitations included a small sample size and limited real-world application, even though debriefings increased bias awareness. It determined that conventional clinical training (TCT) and HFS compared to TCT affected the clinical competence and knowledge of maternity nursing graduates.(14) Results from a quasi-experimental study including 74 students revealed no discernible group differences. A drawback that might impact generalizability was the limited sample size.
To assess how nursing students’ clinical reasoning was affected by simulation-based triage instruction.(15) A quasi-experimental approach was used to compare three groups: one control group that learned through lectures, and two intervention groups that received training based on simulations. In the post-test results, the simulation groups’ clinical reasoning significantly improved. A drawback was the use of self-reported data. The emotions and perceptions of nursing students acting as patients in a catastrophic role-playing activity were examined.(16) Interviews in focus groups were used to analyze data from 23rd-year students in a qualitative manner. The results showed three main areas: initial responses, adaptability, and inference. The limited sample size was one of the limitations, which might restrict generalizability.
Analyzing how well simulation-based training (SBT) improves nursing students’ clinical decision-making abilities is the aim of the investigation. It assesses how well SBT interacts with students’ critical thinking, problem-solving, and confidence by actively engaging them in high-fidelity simulation training throughout their clinical training time and evaluating their performance both before and after the simulation.
METHOD
A quasi-experimental pretest/posttest approach measures students’ clinical decision-making skills before receiving simulation-based training (SBT) and then reassesses these skills. This design allows examination to compare student performance at two different time points (pre-intervention and post-intervention), helping to determine whether changes in skills and confidence can be attributed to simulation training. This SBT is evaluated based on 5 key criteria variables, including critical thinking, problem-solving, confidence levels, making correct decisions, and response time before and after simulation training. Figure 1 illustrates the proposed evaluation basic concept.
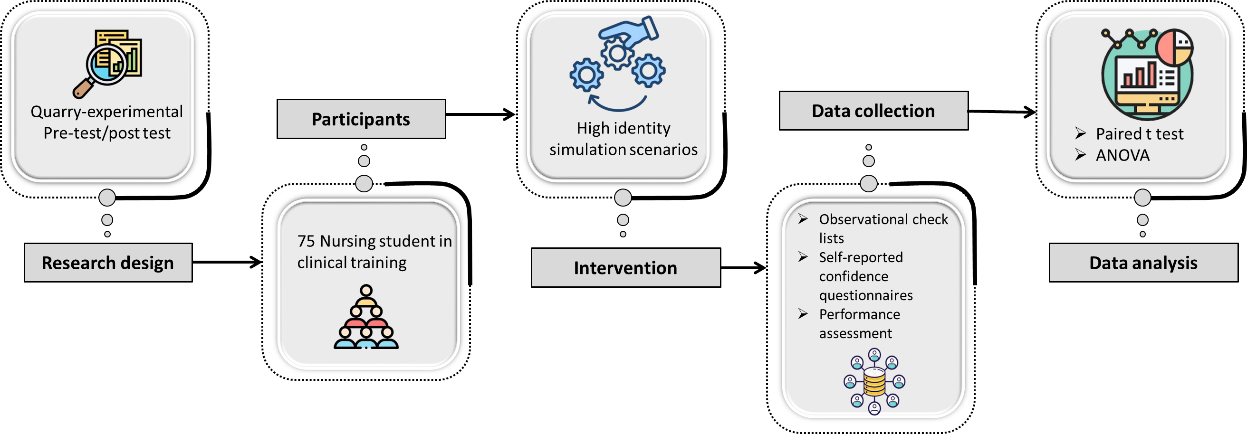
Figure 1. Basic concept of proposed flow diagram
Participants
85 nursing students have signed up for simulation training. 10 students who did not attend the second round of training or provided incomplete questionnaires were eliminated from the data, resulting in 75 total participants. The students were at the last stage of formal nursing education; thus, they were the best candidates to test the efficacy of SBT in enhancing clinical decision-making skills. Because they already had basic knowledge and clinical experience, they were able to participate in high-fidelity simulation scenarios that closely resembled real-world healthcare circumstances, allowing the researchers to test their ability to make crucial decisions under pressure. Table 1 summarizes the participants’ characteristics. The participants were mostly female (73,30 %) and ranged in ages from twenty to thirty years old and bachelor’s graduates (66,70 %). In figure 2, the majority (73,33 %) were employed as paid temporary nursing students at local hospitals to offer medical care figure 2(a), and approximately half of them were assigned to the medical department for 1-2 years figure 2(b).
|
Table 1. Participants’ Demographic Data |
|||
|
Variable |
Category |
Frequency (n=75) |
Percentage (%) |
|
Age (years) |
20–22 |
40 |
53,30 |
|
23–25 |
25 |
33,30 |
|
|
25-30 |
10 |
13,40 |
|
|
Gender |
Female |
55 |
73,30 |
|
Male |
20 |
26,70 |
|
|
Qualification |
UG Nursing |
50 |
66,70 |
|
BG Nursing Science |
25 |
33,30 |
|
|
Having working as an temporary nursing student |
Yes |
55 |
73,33 |
|
No |
20 |
26,67 |
|
|
Years worked as a temporary nursing student |
< 1 year |
37 |
49,3 |
|
1–2 years |
25 |
33,30 |
|
|
> 2 years |
13 |
16,70 |
|
|
Temporary nursing student Specialty |
Medical |
30 |
40 |
|
Surgical |
25 |
33,3 |
|
|
Others |
20 |
26,70 |
|
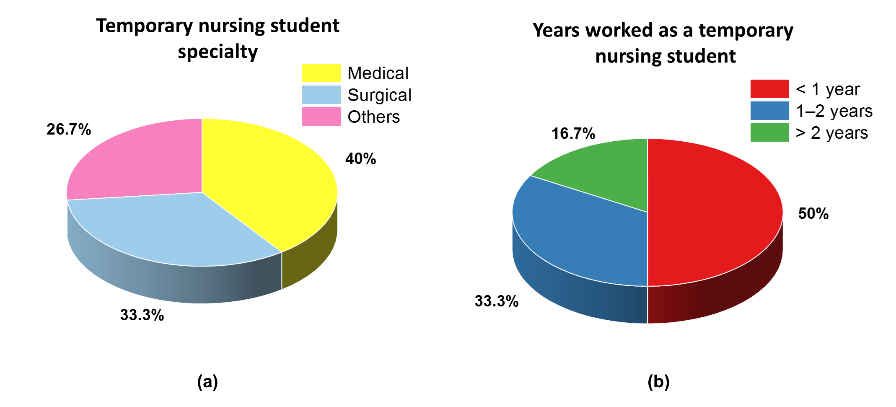
Figure 2. Employment status of nursing students as (a) Temporary Nursing Students, and (b) their department assignment of years
Intervention
Intervention within this examination consisted of high-fidelity simulation situations that resembled near-real clinical emergencies that could occur in real healthcare environments for nursing students. The simulations were created to allow students to practice clinical decision-making under pressure, ensuring that they can respond to emergencies in a simulated risk-free environment. These simulations replicated extreme situations like cardiac arrest, respiratory failure, and treatment of sepsis treatment, where students were required to evaluate patients, make quick decisions, and implement them. 75 nursing students were measured before the intervention to account for decision-making capacity, level of confidence, and competency. After the students completed the simulation training, they were re-measured.
Data collection
To assess the efficacy of SBT, data are gathered with a variety of evaluation instruments pre- and post-intervention for 75 nursing students according to observational checklists, self-assessment confidence questionnaires, and performance assessments.
Observational Checklists
Instructors mark students’ decision-making through simulations. Students were evaluated before simulation training in a simulated clinical emergency. Observers (clinical educators) rated the students on several decision-making criteria using a pretested checklist. Students were retested with the same checklist after the simulation training to measure improvement in decision-making ability. Students were retested with the same checklist after the simulation training to measure improvement in decision-making ability. Table 2 depicts the outcome of the observational checklist for CDM abilities of students in nursing before and after Simulation-Based Training (SBT).
|
Table 2. Observational Checklist Scores for Students’ CDM before and After SBT |
|||
|
Criteria |
Rating Scale |
Score (1-5) |
Score (1-5) |
|
Critical Thinking |
Did the student demonstrate logical reasoning and analysis of the situation? |
3 (Needs Improvement) |
5 (Excellent) |
|
Problem-Solving |
The student able to identify the problem and come up with a possible solution? |
3 (Needs Improvement) |
5 (Excellent) |
|
Confidence Levels |
Did the student appear uncertain or hesitant when making decisions? |
2 (Low Confidence) |
5 (High Confidence) |
|
Ability to Make Correct Decisions |
Did the student choose the appropriate intervention or action? |
3 (Inconsistent) |
5 (Accurate) |
|
Response Time |
How quickly did the student respond to the clinical emergency? |
2 (Slow) |
4 (Fast) |
Self-Reported Confidence Surveys
Students must self-assess their confidence in clinical scenarios. In this survey, students assessed their confidence in handling clinical circumstances using a Likert scale with 1–5 range.
You can logically analyze a patient’s condition and make appropriate decisions.
Do you feel confident in identifying clinical problems and implementing effective solutions?
Do you feel self-assured when making clinical decisions in high-pressure situations?
Do you trust your ability to make accurate and timely decisions in clinical settings?
You can respond quickly and effectively in clinical emergencies.
· Not confident, scale 1
· Slightly confident, scale 2
· Neutral, scale 3
· Confident, scale 4
· Very confident, scale 5
Performance Evaluations
Simulation-based tests evaluate decision-making improvements. Pre- and post-simulation training data are contrasted to determine effectiveness.
Statistical analysis
The IBM SPSS v26.0 program was used to examine the data. To assess development on an individual basis, paired t-tests were used to compare the results of learners before and after simulation training. ANOVA was employed to evaluate group differences. These tests were employed to find out if SBT had a significant impact on making clinical decisions as nursing students.
Performance evaluation
The SBT impacted the CDM ability of nursing students. The findings are founded on data obtained from observational checklists, self-assessed confidence questionnaires, and simulation-based tests. ANOVA and paired t-tests using statistical analysis were employed to contrast the skills of the students before and after the simulation training.
Paired t-test
A test of statistics that compares the means of two related groups in this t-test, also known as the dependent t-test. They are usually before-and-after measures in the same cases. Similar to the one-sample t-test, the test statistics for the paired samples t-test, represented by the letter t, the identical equations (1-2) as follows.
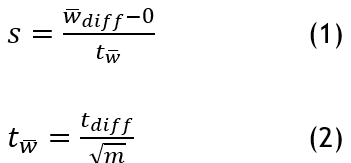
The sample mean of the differences is w ̅diff, m is the number of observations, and tdiff is the sample SD of the variations. The calculated SE of the mean is tw ̅ .
|
Table 3. Paired t-test for Pre-intervention based on nursing students before training |
|||||||
|
Criteria |
x ̅ |
σ |
SEM |
95 % CI |
t |
df |
P-value |
|
Critical Thinking |
5,8 |
1,9 |
0,22 |
5,36 – 6,24 |
1,97 |
74 |
0,052 |
|
Problem-Solving |
5,5 |
1,7 |
0,2 |
5,10 – 5,90 |
1,85 |
74 |
0,067 |
|
Confidence Levels |
4,9 |
2,1 |
0,24 |
4,42 – 5,38 |
1,63 |
74 |
0,103 |
|
Make Correct Decisions |
5,2 |
1,8 |
0,21 |
4,78 – 5,62 |
1,89 |
74 |
0,061 |
|
Response Time |
28,4 |
3,2 |
0,37 |
27,66 – 29,14 |
1,75 |
74 |
0,08 |
|
Note: mean -x ̅, Std. Deviation-σ, Std. Error Mean- SEM, and Confidence Interval -CI |
|||||||
|
Table 4. Paired t-test for Pre-intervention based on nursing students before training |
|||||||
|
Criteria |
x ̅ |
σ |
SEM |
95 % CI |
t |
df |
P-value |
|
Critical Thinking |
9,9 |
1,5 |
0,17 |
9,56 – 10,24 |
19,95 |
74 |
<0,001 *** |
|
Problem-Solving |
9,4 |
1,4 |
0,16 |
9,08 – 9,72 |
21,67 |
74 |
0,03 ** |
|
Confidence Levels |
10 |
1,6 |
0,18 |
9,64 – 10,36 |
22,17 |
74 |
0,02 ** |
|
Make Correct Decisions |
9,7 |
1,7 |
0,2 |
9,30 – 10,10 |
20,45 |
74 |
0,002 *** |
|
Response Time |
21,6 |
2,8 |
0,32 |
20,96 – 22,24 |
-25,19 |
74 |
0,002 *** |
|
Note: ** P<0,05, *** P<0,003 |
|||||||
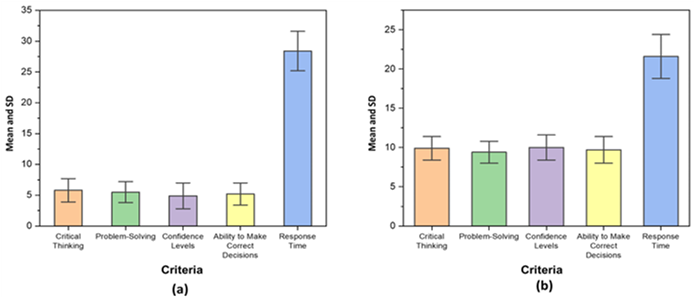
Figure 3. Mean and SD values for SBT for nursing student based on (a) before and (b) After training
Pre-training, nursing students scored lower in critical thinking, problem-solving, confidence, and decision-making with longer response times as shown in figure 3(a) and table 3. The p >0,05, indicates no statistical difference of significance in their pre-simulation training performance. Post-training, the students had improved significantly in all aspects with increased scores in decision-making abilities and faster response times as shown in figure 3(b) and table 4. The p <0,001, indicates a statistically significant improvement after simulation-based training. SBT enhances nursing students’ critical thinking, problem-solving skills, confidence level, decision-making ability, and response time, particularly the ability to assess critical thinking, confidence level, and response time effectively under stress, which indicates that SBT is an effective training method for clinical training.
ANOVA
A statistical method for contrasting the means of more than one group is called Analysis of Variance, or ANOVA, and identifying whether they have a difference of significance among them. It’s an extension of the t-test in the case of more than two groups.
|
Table 5. ANOVA outcome for nursing students before and after training in SBT |
|||||
|
Criteria |
SS |
df |
MS |
F-value |
P-value |
|
Critical Thinking |
245,6 |
1 |
245,6 |
98,24 |
<0,001 *** |
|
Problem-Solving |
210,4 |
1 |
210,4 |
95,12 |
<0,001 *** |
|
Confidence Levels |
265,2 |
1 |
265,2 |
102,45 |
<0,001 *** |
|
Make Correct Decisions |
230,8 |
1 |
230,8 |
97,35 |
<0,001 *** |
|
Response Time |
310,6 |
1 |
310,6 |
110,87 |
<0,001 *** |
|
Error |
184,2 |
73 |
2,52 |
|
|
|
Total |
1446,8 |
74 |
|
|
|
|
Notes: Sum of Squares-SS, Mean square –MS |
|||||
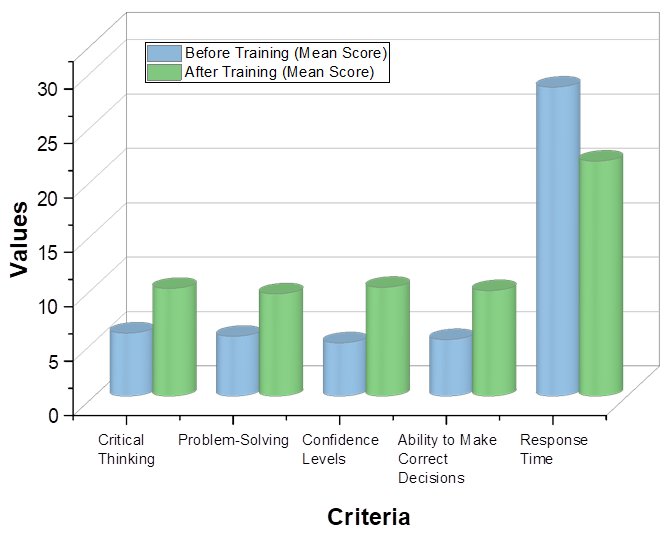
Figure 4. ANOVA Outcome for nursing student before and after training
ANOVA findings indicate that there exists a significant variation in nursing students’ critical thinking, problem-solving, confidence, decision-making, and response time following simulation-based training as shown in table 5. Figure 4 illustrates the mean scores before and after simulation-based training. High F-values and p-values of <0,001 confirm that the change is significant. This indicates that SBT is extremely effective in improving clinical decision-making skills.
DISCUSSION
SBT provides nursing students a structured, simulated setting in which they can practice CDM in high-risk situations. To assess the efficacy of SBT in increasing critical thinking, confidence, and response time in clinical situations. Paired t-test results indicated that pre-training nursing students scored lower on critical thinking, problem-solving, confidence, decision-making, and response time length, with p>0,05, indicating no significant differences. However, after SBT, students showed statistically significant improvements on all criteria (p<0,001), indicating improved decision-making skills, confidence, and response time. ANOVA results further support these results, with high F values and p <0,001 demonstrating that there was significant variation in student performance before and after SBT. This strongly indicates that SBT is an effective training method for improving nursing students’ CDM, critical thinking, and reaction time efficiency under stress.
CONCLUSIONS
Examine that SBT has affected medical students’ CDM abilities in response time, self-assurance, critical thinking, problem-solving, and decision-making. Using a pre-test/post-test quasi-experimental approach, nursing students in the clinical instruction phase participated. HDS trainings were conducted by the participants, and data were gathered through structured observational checklists, self-report confidence questionnaires, and performance assessments. The statistical comparisons were conducted using ANOVA and paired t-tests. The results showed that SBT might enhance nurse students’ CDM skills by increasing their post-training critical thinking, problem-solving, and confidence scores. The students also delivered quicker and more accurate responses during simulated emergency conditions. Statistical analysis confirmed an overall significant improvement (p<0,001) in all parameters assessed. The results confirm that SBT is an effective teaching method for nursing students to acquire CDM skills under pressure. The research is limited to a single group of nursing students, which restricts its generalizability. Factors such as previous experience and learning styles were not considered. Future researchshould explore long-term retention of skills, multi-center studies, and integration with real-world clinical settings. Advancements in AI-driven simulations could further enhance training effectiveness.
BIBLIOGRAPHIC REFERENCES
1. Ludin SM. Does good critical thinking equal effective decision-making among critical care nurses? A cross-sectional survey. Intensive and Critical Care Nursing. 2018 Feb 1; 44:1-0. https://doi.org/10.1016/j.iccn.2017.06.002
2. Dickison P, Haerling KA, Lasater K. Integrating the National Council of State Boards of Nursing clinical judgment model into nursing educational frameworks. Journal of Nursing Education. 2019 Feb 1; 58(2):72-8. https://doi.org/10.3928/01484834-20190122-03
3. Ahmady S, Shahbazi S. Impact of social problem-solving training on critical thinking and decision making of nursing students. BMC nursing. 2020 Oct 7; 19(1):94. https://doi.org/10.1186/s12912-020-00487-x
4. Padilha JM, Machado PP, Ribeiro A, Ramos J, Costa P. Clinical virtual simulation in nursing education: randomized controlled trial. Journal of medical Internet research. 2019 Mar 18; 21(3):e11529. https://doi.org/10.2196/11529
5. Abubakar AM, Elrehail H, Alatailat MA, Elçi A. Knowledge management, decision-making style and organizational performance. Journal of Innovation & Knowledge. 2019 Apr 1;4(2):104-14. https://doi.org/10.1016/j.jik.2017.07.003
6. Murray DJ, Boyle WA, Beyatte MB, Knittel JG, Kerby PW, Woodhouse J, Boulet JR. Decision-making skills improve with critical care training: Using simulation to measure progress. Journal of Critical Care. 2018 Oct 1;47:133-8. https://doi.org/10.1016/j.jcrc.2018.06.021
7. Hung CC, Kao HF, Liu HC, Liang HF, Chu TP, Lee BO. Effects of simulation-based learning on nursing students’ perceived competence, self-efficacy, and learning satisfaction: A repeat measurement method. Nurse Education Today. 2021 Feb 1; 97:104725. https://doi.org/10.1016/j.nedt.2020.104725
8. Giordano C, Brennan M, Mohamed B, Rashidi P, Modave F, Tighe P. Accessing artificial intelligence for clinical decision-making. Frontiers in digital health. 2021 Jun 25; 3:645232. https://doi.org/10.3389/fdgth.2021.645232
9. Elcokany NM, Abdelhafez AI, Samuel Sharaby VM, Belal S. Use of computer-based scenarios for clinical teaching: Impact on nursing students’ decision-making skills. Healthcare 2021 Sep 17 (Vol. 9, No. 9, p. 1228). MDPI. https://doi.org/10.3390/healthcare9091228
10. Kim HK, Ryu S, Jang KS. Effect of structured pre-simulation preparation and briefing on student’s self-confidence, clinical judgment, and clinical decision-making in simulation. Contemporary Nurse. 2019 Sep 3; 55(4-5):317-29. https://doi.org/10.1080/10376178.2019.1641420
11. Lee BO, Liang HF, Chu TP, Hung CC. Effects of simulation-based learning on nursing student competences and clinical performance. Nurse education in practice. 2019 Nov 1; 41:102646. https://doi.org/10.1016/j.nepr.2019.102646
12. Hustad J, Johannesen B, Fossum M, Hovland OJ. Nursing students’ transfer of learning outcomes from simulation-based training to clinical practice: A focus-group study. BMC nursing. 2019 Dec; 18:1-8. https://doi.org/10.1186/s12912-019-0376-5
13. Altabbaa G, Raven AD, Laberge J. A simulation-based approach to training in heuristic clinical decision-making. Diagnosis. 2019 Jun 26; 6(2):91-9. https://doi.org/10.1515/dx-2018-0084
14. Raman S, Labrague LJ, Arulappan J, Natarajan J, Amirtharaj A, Jacob D. Traditional clinical training combined with high‐fidelity simulation‐based activities improves clinical competency and knowledge among nursing students on a maternity nursing course. Nursing Forum 2019 Jul (Vol. 54, No. 3, pp. 434-440). https://doi.org/10.1111/nuf.12351
15. Hu F, Yang J, Yang BX, Zhang FJ, Yu SH, Liu Q, Wang AL, Luo D, Zhu XP, Chen J. The impact of simulation-based triage education on nursing students’ self-reported clinical reasoning ability: a quasi-experimental study. Nurse Education in Practice. 2021 Jan 1; 50:102949. https://doi.org/10.1016/j.nepr.2020.102949
16. Kose G, Unver V, Tastan S, Ayhan H, Demirtas A, Kok G, Guvenc G, Basak T, Bagcivan G, Kurtoglu PG, Acavut G. Embedded participants in simulation-based disaster education: experiences of nursing students. Clinical Simulation in Nursing. 2020 Oct 1;47:9-15. https://doi.org/10.1016/j.ecns.2020.06.011
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Malathi H, Ashutosh Niranjan, Sasmita Das.
Data curation: Malathi H, Ashutosh Niranjan, Sasmita Das.
Formal analysis: Malathi H, Ashutosh Niranjan, Sasmita Das.
Drafting - original draft: Malathi H, Ashutosh Niranjan, Sasmita Das.
Writing - proofreading and editing: Malathi H, Ashutosh Niranjan, Sasmita Das.