doi: 10.56294/mw2023104
ORIGINAL
Investigating the contribution of peer-assisted learning to student competency in medical education
Investigación de la contribución del aprendizaje asistido por compañeros a la competencia de los estudiantes de medicina
1Noida International University, Department of General Medicine. Greater Noida, Uttar Pradesh, India.
2Department of Management, Siksha ‘O’ Anusandhan (Deemed to be University). Bhubaneswar, Odisha, India.
Cite as: Malla D, Das A. Investigating the Contribution of Peer-Assisted Learning to Student Competency in Medical Education. Seminars in Medical Writing and Education. 2023; 2:104. https://doi.org/10.56294/mw2023104
Submitted: 04-09-2022 Revised: 16-12-2022 Accepted: 22-02-2023 Published: 23-02-2023
Editor: PhD.
Prof. Estela Morales Peralta ![]()
ABSTRACT
Peer Assisted Learning (PAL) is a cutting-edge teaching and learning approach that allows students to work with their peers to develop greater comprehension and proficiency. Comparing PAL to conventional pedagogical techniques, the research examines how PAL helps medical students improve their abilities, especially in the clinical and theoretical areas. The main goal was to determine how well PAL improved medical students’ proficiency in the practical and cognitive components of medical education. Using a quasi-experimental approach, 70 medical students were evaluated over the course of a semester; 35 in the PAL intervention group engaged in structured peer-teaching sessions, while 35 in the control group received traditional instructor-led lectures. Data collection included formative assessments, summative exams, peer evaluations, clinical skills assessments, and student self-assessments. The analysis of covariance (ANCOVA) and the Mann-Whitney U test were implemented to evaluate group differences, adjusting for baseline performance and non-parametric distributions. The PAL group exhibited statistically significant improvements in assessment at p<0,005. Peer evaluations indicated substantial growth in teaching and clinical competencies among the peer-teachers. ANCOVA and the Mann-Whitney U test results confirmed that PAL significantly enhanced teaching effectiveness and practical skills. The findings underscore PAL’s potential as an effective pedagogical strategy for bridging theoretical concepts with practical applications in medical education. Further examination with larger sample sizes and longitudinal data is recommended to explore the long-term impact and scalability of PAL in medical curricula.
Keywords: Peer Assisted Learning (PAL); Analysis of Covariance (ANCOVA); Formative Assessments; Clinical Skills Assessment; Cognitive Self-Assessment.
RESUMEN
El aprendizaje asistido por compañeros (PAL) es un método de enseñanza y aprendizaje de vanguardia que permite a los estudiantes trabajar con sus compañeros para desarrollar una mayor comprensión y competencia. Comparando PAL con las técnicas pedagógicas convencionales, la investigación examina cómo PAL ayuda a los estudiantes de medicina a mejorar sus capacidades, especialmente en las áreas clínica y teórica. El objetivo principal era determinar en qué medida PAL mejoraba la competencia de los estudiantes de medicina en los componentes prácticos y cognitivos de la enseñanza de la medicina. Mediante un enfoque cuasiexperimental, se evaluó a 70 estudiantes de medicina a lo largo de un semestre; 35 del grupo de intervención PAL participaron en sesiones estructuradas de enseñanza entre iguales, mientras que 35 del grupo de control recibieron clases tradicionales impartidas por un instructor. La recogida de datos incluyó evaluaciones formativas, exámenes sumativos, evaluaciones entre compañeros, evaluaciones de habilidades clínicas y autoevaluaciones de los estudiantes. Se aplicaron el análisis de covarianza (ANCOVA) y la prueba U de Mann-Whitney para evaluar las diferencias entre los grupos, ajustando el rendimiento inicial y las distribuciones no paramétricas. El grupo PAL mostró mejoras estadísticamente significativas en la evaluación con p<0,005. Las evaluaciones de los compañeros indicaron un crecimiento sustancial en las competencias docentes y clínicas entre los compañeros-profesores. Los resultados del ANCOVA y de la prueba U de Mann-Whitney confirmaron que PAL mejoró significativamente la eficacia docente y las habilidades prácticas. Los resultados subrayan el potencial de PAL como estrategia pedagógica eficaz para vincular los conceptos teóricos con las aplicaciones prácticas en la enseñanza de la medicina. Se recomienda realizar nuevos análisis con muestras de mayor tamaño y datos longitudinales para explorar el impacto a largo plazo y la escalabilidad de PAL en los planes de estudios de medicina.
Palabras clave: Aprendizaje Asistido por Pares (PAL); Análisis de Covarianza (ANCOVA); Evaluaciones Formativas; Evaluación de Habilidades Clínicas; Autoevaluación Cognitiva.
INTRODUCTION
Medical education denotes organized learning experiences intended to support healthcare providers in preserving, improving, and advancing their expertise in their specialties. A range of approaches are covered that comprise educational programs, professional guidance, and networks of practices.(1) Medical education includes both conventional teaching methods like repetition, textbook-based learning, and instructional lecturing and advanced techniques that comprise a variety of artificial intelligence (AI) techniques.(2) A popular teaching and learning strategy in medical education around the world is peer-assisted learning (PAL). In preliminary medicine in the fields of architecture, physiology, and problems-based instruction, PAL is well established with the knowledge.(3) The advantageous character of PAL is that provide enough time to develop the abilities of the early carrier learner enabling them to learn surgical skills and providing confidence for clinical placements.(4) Student engagement, critical thinking, and confidence levels are enhanced by PAL through fostering collaborative learning. Also, it offers professional competence and patient care by fostering independent learning and encouraging a place for skill development.(5) PAL can take many different forms, such as official mentoring, guidance, and informal learning communities formed by peers and act as a significant learning program.(6) In PAL, the communal and intellectual consistency is essential. With the help of peer teachers, anxiety in the classroom is decreased and they act as role models for younger students.(7)
The impact of the flipped learning method in health professions education was compared to typical educational environments.(8) A total number of 28 contrasting investigations with an emphasis on medical pupils, citizens, and other health trainees offered the key information. The question was implemented to rate the efficacy of the method. The outcomes showed that the flipped classrooms had a considerable impact and offered a very effective approach, based on the SMD (0,33) and, p < 0,001 that were chosen by students over regular ones.
To improve the earning outcomes by diagnosing learning issues and providing timely feedback, the research employed the technique named Formative Assessment Classroom Techniques (FACT).(9) The required statistics were obtained from 200 first-grade medical learners with the assistance of the survey assessment and the learners were split into two distinct groups. Seven FACT methods were implemented for the efficient analysis. By utilizing a t-test, the findings showed that improvements in Absolute Learning Gain (ALG) of 68,5 % - 75 % and the effect size of 1.12, proved the significance of the model.
The examination explored strategies for teaching the muscles and tendons of Year 1 MBBS students using active, student-focused techniques.(10) The approach includes scenario-based learning, collaborative instruction, and flipped classrooms. Through the discussions on a variety of musculoskeletal subjects, the necessary information was obtained and evaluations were performed both before and after the discussions. The results from zero-order correlations, independent T-test and paired t-tests confirmed a significant enhancement in spotter assessments, and mid-course tests, proven by the value of p < 0,01.
To enhance medical learners and the transformation of the healthcare settings, the investigation introduced the integration of theatre into medical education.(11) Eight years of cooperation between medical instructors and students in curriculum activities was utilized to gather the data. The methods comprised two processes, namely Freire’s and Boal’s theatre of the oppressed, were implemented with courses centered on critical teaching, interactive performing, and exercises that improved empathy. The findings demonstrated that theatre improved equitable practices in medical practice and helped the medical pupils to become change agents for health care by fostering personal and professional development.
The examination analysed the disparity between theory and practice that medical learners encounter, especially in managing clinical crises. (12) The responses from final year students, based on the organized questionnaire and a high-fidelity simulation-based sub-module that was taught by clinical tutors utilizing the Sim-Man 3GTM were employed. The findings demonstrated that the simulated training greatly increased their trust and enhanced their ability to handle clinical difficulties and participants gave positive comments.
Utilizing a near-peer training scheme run by younger medical professionals, the investigation was to introduce undergraduates in medicine to Quality Improvement (QI) approaches.(13) In participatory sessions, 111 University of Cambridge fifth-year students discussed subjects including data analysis, engagement with stakeholders, and the framework for transformation. Before and after the treatment, questionnaires were used to evaluate the pupil’s understanding and attitude. The findings demonstrated that students’ comprehension (p < 0,05) and confidence (p < 0,05) in using QI procedures had significantly improved.
The students’ attitudes toward recent teaching techniques in medical education, such as mind maps (MM), crossword puzzles (CWP), and internet resources were examined.(14) The data gathering was performed in the Institute of pathologists over a year and involved 206 learners. Then, the strategies of CWPs and MMs were introduced. The majority of students preferred CWPs for collaborative work and MMs for improved memory retention, based on the results, which demonstrated strong engagement, promoted creativity, and improved learning.
The research explored the progress of medical education as implemented by the National Medical Commission competency-based medical education (CBME) mode.(15) The necessary information was obtained through observational materials on CBME’s development. The approach involves investigating the effect of CBME on abilities-based learning, such as mental health training and skill-based training valued on attitude, ethics, and communication (AETCOM) abilities. The findings highlighted that the framework could produce holistic medical practitioners and flexible options for learning.
The effectiveness of visual mapping approaches in Community-Based Medical Education (CBME) for local medicine was evaluated.(16) The quantity of 60 medical student participants was split into two groups and an experimental inquiry while the interventional assessment was performed. By reporting better memory and organized responses, the outcomes showed the advantages of visual mapping in CBME learning through the random examination values of 9,85 ± 3,22, which was higher than the traditional group.
The research investigated the way of increasing professional happiness and participation in medical education achieved via promoting inventiveness and interest.(17) Interviews and conversations with clinicians regarding their professional experiences were used to gather data. By analyzing the responses, the technique was able to determine the main causes of discontent, including regulatory constraints and the absence of independence. The findings showed that incorporating creative learning strategies into training supports long-term wellbeing and productivity leading to enhanced patient care results.
The purpose of the research is to analyse the effectiveness of the PAL system for enhancing the medical students’ competency in the two groups by evaluating its impact on distinct variables engaged in the multiple assessments.
Organization of the analysis: The next part explains the methodology section and then the result was provided. The final section gives the discussion and conclusion of the analysis.
METHOD
A comprehensive discussion of the data collection process, research instruments, and key assessment variables is presented. In addition, the statistical analysis methods, including ANCOVA and the Mann-Whitney U test, are detailed to evaluate competency development. These measurements confirm an accurate assessment of the impact of PAL on medical students.
Participants details
A total number of 70 medical students engaged in the quasi-experimental analysis over one semester to assess the impact of PAL on competency development. The key demographic variables were observed for the analysis. These students were split into two groups, such as 35 students in the control group attended traditional instructor-led lectures, whereas 35 students in the PAL intervention group engaged in organized peer-teaching activities. The PAL sessions concentrated on collaborative learning, active discussions, and peer assessments, whereas the control group tracked a conventional lecture-based approach. An evaluation of competence growth in both theoretical knowledge and clinical abilities was made possible by the organized comparison. Table 1 demonstrates the summary of 70 medical student’s profiles.
The PAL intervention group comprised 51 % males and 49 % females, whereas the control group had 49 % males and 51 % females. The majority (54 %) of students in both groups fell within the 22–23 age range. The examination evaluated the students from different academic years, with 17 % in 1st-year, 26 % in 2nd-year, 29 % in 3rd-year, and 29 % in the final year. The learning hours fluctuated across participants 20 % studied less than 5 hours, nearly 51 % spent 5 to 10 hours, and around 29 % exceeded 8 hours per day. Clinical skills confidence levels were categorized as low (23 %), approximately 51 %, and 26 % for moderate and high respectively.
|
Table 1. Medical student’s demographics |
|||||
|
Characteristics |
Category |
PAL Group (N = 35) |
Percentage (%) |
Control Group (N = 35) |
Percentage (%) |
|
Gender |
Male |
18 |
51 |
17 |
49 |
|
|
Female |
17 |
49 |
18 |
51 |
|
Age |
20–21 |
8 |
23 |
7 |
20 |
|
|
22–23 |
19 |
54 |
19 |
54 |
|
|
24–25 |
8 |
23 |
9 |
26 |
|
Year of Study |
1st Year |
6 |
17 |
6 |
17 |
|
|
2nd Year |
9 |
26 |
9 |
26 |
|
|
3rd Year |
10 |
29 |
10 |
29 |
|
|
Final Year |
10 |
29 |
10 |
29 |
|
Average Learning Hours |
<5 |
7 |
20 |
7 |
20 |
|
|
5 - 8 |
18 |
51 |
17 |
49 |
|
|
>8 |
10 |
29 |
11 |
31 |
|
Clinical Skills Confidence |
Low |
8 |
23 |
8 |
23 |
|
|
Moderate |
18 |
51 |
17 |
49 |
|
|
High |
9 |
26 |
10 |
28 |
Assessment type
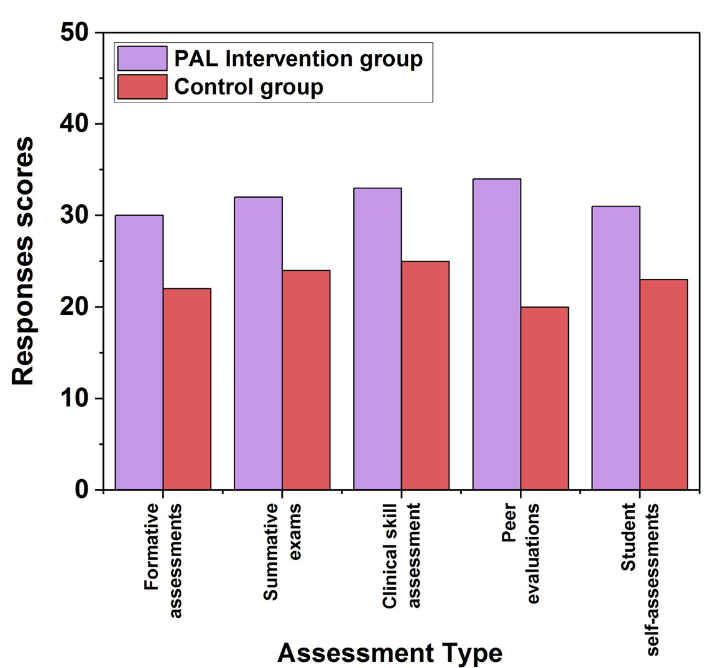
Figure 1. Student’s response score for the assessments
To analyse the competence growth accurately, multiple assessment methods were conducted. Here, specifically five assessment methods were performed on the medical students. To provide both educators and students insight into their development, these evaluations have been carried out at different times during the learning process that serves as instructional resources. Quizzes, short assignments, and classroom activities are prime instances of formative assessments in the context of PAL that assist students in measuring their understanding and improving their abilities before finals. After a course, like a semester, summative exams are utilized for evaluating the overall achievement of students. These tests measure the way learners have understood the topic and usually contribute toward their final score. Typically, written or practical assessments examined the students’ clinical-theoretical expertise level in PAL. The students can evaluate each other’s performance through peer evaluations, which usually take place in collaboration or cooperative situations. Students who engaged in peer tutoring within the framework of PAL had the opportunity to assess their colleagues’ clinical expertise and efficacy as teachers. These assessments offer insight into teaching effectiveness and assist in identifying areas of strength and potential development. To examine students’ practical skills in actual or simulated clinical environments, clinical assessments are carried out. To ensure that students can convert their theoretical knowledge into practical abilities, these tests are essential in medical education. Different assessments, including physical examinations, diagnoses, and real-world applications are the major techniques in clinical assessment. Self-assessments encourage the students to replicate on their learning, strengths, weaknesses, progress, and performance. The students can rate their clinical skills, theoretical knowledge, or involvement with peer teaching as part of their self-assessments. To gain more self-awareness and responsibility, these assessments are vital. Figure 1 illustrates the response score of the students.
Performance indicators
The performance indicators play a major role in the effective analysis of medical students’ competency development. By incorporating these indicators, the assessment confirms a holistic evaluation of both theoretical knowledge and practical skills, highlighting the effectiveness of PAL.
· Learning process: The learning process in medical education includes acquiring knowledge, skills, and competencies through organized instruction, practice, and assessment. For the development of analytical abilities, clinical proficiency, and handling patient skills, the learning process is necessary. Through improving participation, retention, interaction, collaboration, and the practical application of medical principles, PAL improves learning abilities.
· Clinical-theoretical expertise: A precise diagnosis and effective treatment of patients depend on the integration of theoretical medical knowledge with actual clinical abilities, which is known as clinical-theoretical expertise. By encouraging peer conversations, engaged instruction, and practical experience, PAL strengthens the expertise and promotes greater comprehension, enhanced critical thinking, and improved execution of medical principles in practical settings.
· Teaching effectiveness: The capacity to promote student learning via involvement, transfer of information, and clear communication is referred to as teaching effectiveness. Due to its skill acquisition and understanding capability, it is necessary in medical education. PAL significantly improved teaching effectiveness by improving the instructional process and interaction and strengthening information retention.
· Practical skills: In medical education, practical skills refer to practical skill sets, such as clinical procedures, procedures for diagnosis, and receptive measurement. These competencies are essential for providing patients with secure and effective treatment. By encouraging instruction, enhancing confidence, and enabling students to develop their abilities via group practice and feedback, PAL improves practical skills.
· Self-awareness: Self-awareness is the willingness of a student to recognize their learning requirements, areas of strength, and weaknesses. For career advancement, improving communications and clinical decision-making is essential. PAL measures self-awareness by encouraging peer feedback and reflection, leading to improved confidence, adaptability, and sustainable learning habits in medical practice.
Data analysis
To evaluate the variations between the PAL and control groups while controlling for any possible initial distinctions, the collected data were analysed using statistical analysis. Two distinct methods named Analysis of Covariance (ANCOVA) and the Mann-Whitney U test were performed in this research.
ANCOVA
To explore the impact of PAL on student competency while controlling for baseline performance disparities, the ANCOVA approach was used. The post-test results evaluate dependent and autonomous indicators. To reflect on early differences in competence, the pre-test scores were used as the covariate. Equation (1) provides the effective calculation of the ANCOVA.
![]()
Where, Xji is the dependent variable that under jth observation and ith collection of categories. In covariates, the variable of yji had the ith observation and jth collection. The overall mean and the effects of treatments are determined by μ and τj respectively. The B is the regression coefficient and the average pre-test scores are denoted by y ̅. Finally, the error term (∈ji) offers the residual variance.
Mann-Whitney U test
To compare non-uniformly distributed factors between the two groups, the approach employs the Mann-Whitney U test concentrated on peer evaluations and self-assessment scores. The statistically significant effect of the discrepancies in median grades was evaluated using the test and it calculates the U statistic and ranks in every observation, which is provided in equation (2).
![]()
Where U1 is the u-statistics that offers the variations. The sample sizes of the two groups are determined by l1 and l2 and K1 is the sum of the rank.
RESULTS
Table 2 demonstrates the outcomes of the ANCOVA focused on the key performance indicators. The average score for every factor is determined by the mean. The standard deviation (SD) represents the quantity of fluctuations from the mean. Typically decreased SD is required for improved outcomes. The statistical significance is measured by the p-value. The p-value is usually less than 0,005 and the symbol of ** indicates that there is a clear differentiation of both groups. The F-statistic calculates the proportion of the variations within the groups to the variance explained by the variables. Higher F-statistics, which are above 5,0 deliver the stronger effect of the characteristics. The amount of the variations in the two groups is explained by the effect size (η²). A high effect >0,06 is required for the increased performance.
|
Table 2. ANCOVA results for two groups across different indicators |
|||||
|
Indicators |
PAL Intervention group |
Control group |
F-statistics |
p-value |
η² |
|
Mean ± SD |
Mean ± SD |
||||
|
Learning process |
88,2 ± 6,0 |
74,5 ± 6,8 |
12,31 |
0,001** |
0,138 |
|
Clinical-theoretical expertise |
86,4 ± 5,8 |
78,3 ± 6,5 |
10,56 |
0,002** |
0,125 |
|
Teaching effectiveness |
84,6 ± 6,2 |
76,8 ± 7,1 |
8,24 |
0,004** |
0,105 |
|
Practical skills |
85,7 ± 5,9 |
77,1 ± 7,2 |
9,67 |
0,003** |
0,118 |
|
Self-awareness |
83,5 ± 6,5 |
75,4 ± 7,4 |
7,92 |
0,002** |
0,098 |
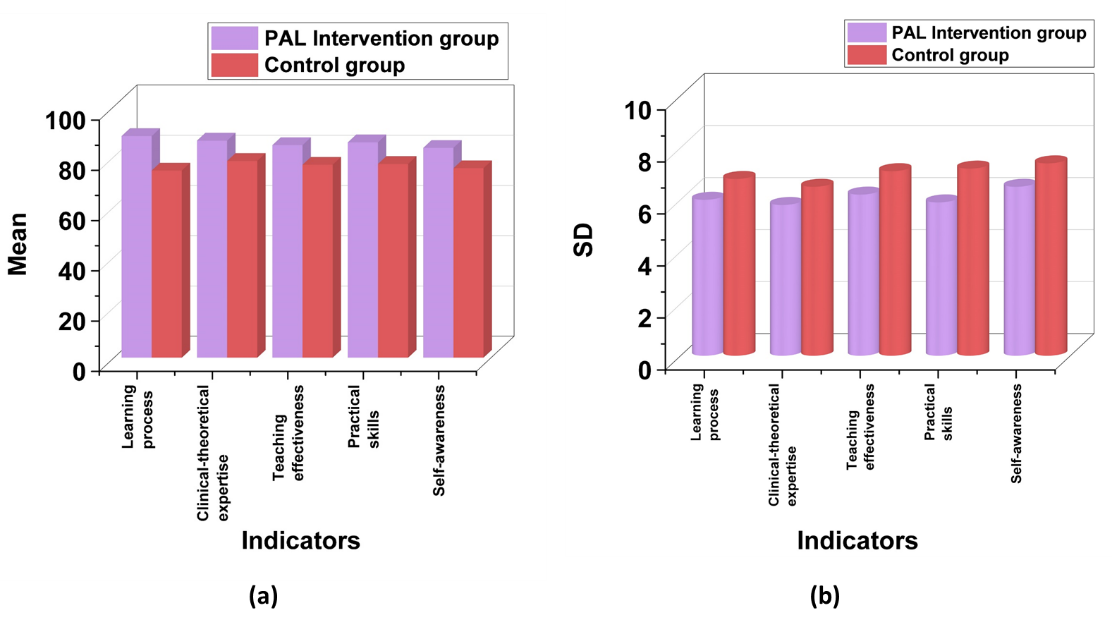
Figure 2. ANCOVA outcomes of (a)Mean and (b) SD of the two groups
The F-statistics range from 7,92 to 12,31 proving the enhanced effects. With the highest F-statistic of 12,31, the learning process and clinical-theoretical expertise demonstrate a superior impact on medical students’ competency. With the lowest p-values of 0,001 and 0,002 these variables show highly significant enhancements in the learning process and clinical-theoretical expertise, respectively. Compared to control groups the PAL intervention group had a decreased SD in all indicators, particularly 5,8 (clinical-theoretical expertise) proving the positive impacts of PAL on students. All the η² values above 0,098 expect self-awareness delivered the rapid performance; specifically the highest robust contribution is highlighted by the η² of the learning process (0,138) and clinical-theoretical expertise (0,125). Figure 2 (a) and (b) provide the mean and SD values for ANCOVA.
Table 3 provides the findings of the Mann-Whitney U test with necessary indicators. The mean rank provides the average rank assigned to each group based on score distribution, denoting relative performance. The sum of ranks is the total of all assigned ranks that assists in measuring the Mann-Whitney U statistic. The Mann-Whitney U-value exhibits the group differences, where lower values indicate a higher distinction. The p-value (Sig.) offers statistical significance, with values less than 0,005 suggesting a significant difference between groups.
|
Table 3. Group performance comparison on key indicators by Mann-Whitney U test |
||||||
|
Indicators |
PAL Intervention Group |
Control group |
Mann-Whitney U |
p-value (Sig.) |
||
|
Mean Rank |
Sum of Ranks |
Mean Rank |
Sum of Ranks |
|||
|
Learning process |
42,8 |
1498,0 |
28,2 |
987,0 |
310,5 |
0,001 |
|
Clinical-theoretical expertise |
41,6 |
1456,0 |
29,4 |
1029,0 |
335,0 |
0,003 |
|
Teaching effectiveness |
44,1 |
1544,0 |
26,9 |
941,0 |
295,0 |
0,0005 |
|
Practical skills |
43,5 |
1523,0 |
27,5 |
962,0 |
305,0 |
0,0007 |
|
Self-awareness |
40,9 |
1432,0 |
30,1 |
1053,0 |
350,5 |
0,006 |
The highest mean rank of 44,1 and sum of ranks (1544,0) of teaching effectiveness in the intervention group, with the lowest p-value (0,0005), indicate a highly significant improvement. Similarly, practical skills exhibited a mean rank of 43,5 and the sum of ranks (1523,0), with a p-value of 0,0007, confirming its strong effectiveness. The decreased Mann-Whitney U values of 295,0 for teaching effectiveness and 305,0 for practical skills confirmed the noteworthy rank differences. Figure 3 (a) and (b) visualize the mean and sum of ranks.
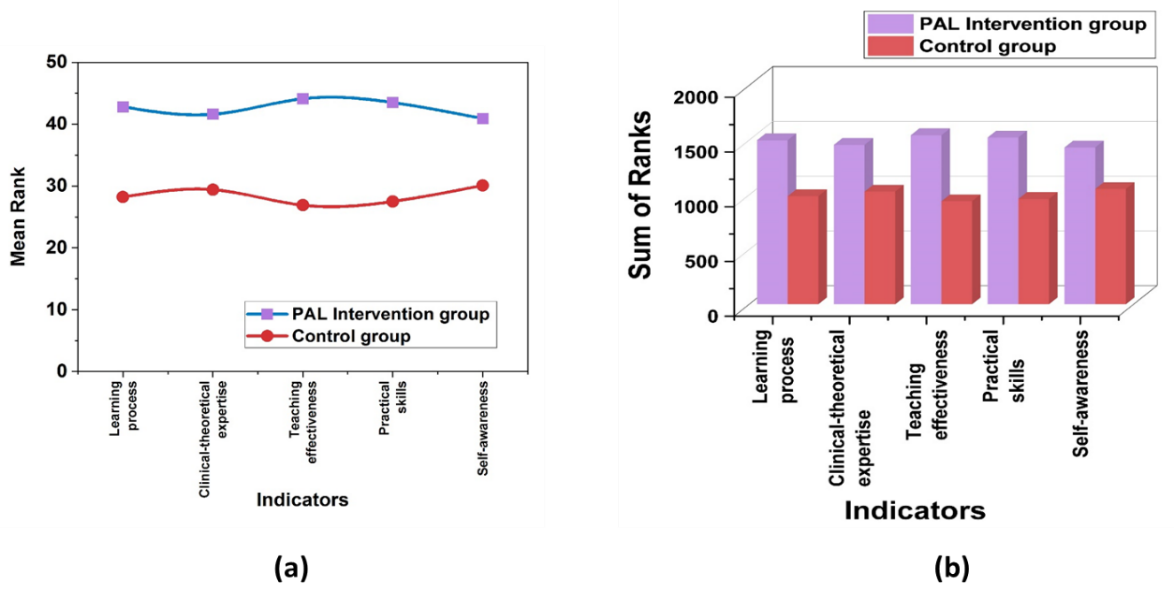
Figure 3. Mann-Whitney U test (a) mean rank and (b) sum of rank for two group
DISCUSSION
The findings of the Mann-Whitney U and ANCOVA tests confirmed the intervention’s greater effect on significant performance indicators. The medical competitiveness of students had substantially enhanced as evidenced by the greatest F-statistics and lowest p-values for the learning process and clinical-theoretical expertise. Further, the consistent performance and the strong effects were obtained by the lowest SD and η² scores. Mann-Whitney U test findings reinforced these findings, with teaching effectiveness and practical skills emerging as the most effective as demonstrated by the mean and sum of ranks. The effectiveness of the intervention is demonstrated by the lowest U and p-values, which indicate significant group differences. These findings underscored the enhanced learning outcomes facilitated by PAL, particularly in teaching effectiveness and practical skills.
CONCLUSIONS
The research underscored the effectiveness of PAL in enhancing medical students’ competency development. A total of 70 medical students participated in the evaluation and were evenly split into intervention and control groups. The evaluation process incorporated five assessment techniques, including formative assessments, summative exams, peer evaluations, clinical skills assessments, and student self-assessments. These techniques measured key performance indicators, like a learning process, clinical-theoretical expertise, teaching effectiveness, practical skills, and self-awareness. The statistical analysis methods of ANCOVA and Mann-Whitney U test were implemented to test the findings. The outcomes from ANCOVA proved that the PAL group exhibited statistically significant improvements in all indicators of p<0,005. In addition, the Mann-Whitney U test confirmed the PAL significantly enhanced teaching effectiveness, and practical skills in students. Overall, integrating PAL into medical education could enhance all the necessary performance indicators, contributing to more competence and awareness for healthcare professionals.
BIBLIOGRAPHIC REFERENCES
1. Thi Nguyen VA, Könings KD, Scherpbier AJ, van Merriënboer JJ. Attracting and retaining physicians in less attractive specialties: the role of continuing medical education. Human resources for health. 2021 May 19;19(1):69. https://doi.org/10.1186/s12960-021-00613-z
2. Wartman SA, Combs CD. Medical education must move from the information age to the age of artificial intelligence. Academic Medicine. 2018 Aug 1;93(8):1107-9. doi: 10.1097/ACM.0000000000002044
3. Siddiqi HS, Rehman R, Syed FF, Martins RS, Ibrahim MT, Alam F. Peer-Assisted Learning (PAL): An innovation aimed at engaged learning for undergraduate medical students. JPMA. The Journal of the Pakistan Medical Association. 2020;70(11):1996. )DOI: https://doi.org/10.5455/JPMA.29714
4. Bennett SR, Morris SR, Mirza S. Medical students teaching medical students surgical skills: the benefits of peer-assisted learning. Journal of surgical education. 2018 Nov 1;75(6):1471-4. https://doi.org/10.1016/j.jsurg.2018.03.011
5. Carey MC, Kent B, Latour JM. Using meta‐ethnography to develop a conceptual model of peer‐assisted learning of nursing students in clinical practice. Nursing open. 2019 Apr;6(2):473-81. https://doi.org/10.1002/nop2.229
6. Hunt T, Jones TA, Carney PA. Peer‐assisted learning in dental students’ patient case evaluations: an assessment of reciprocal learning. Journal of dental education. 2020 Mar;84(3):343-9. doi: 10.21815/JDE.019.182
7. Omar F, Zaheer M, Ahmed M. Effectiveness of peer teaching in medical education: medical student’s perspective. Advances in Medical Education and Practice. 2018 Mar 23:199-201.DOI: 10.2147/AMEP.S161507
8. Hew KF, Lo CK. Flipped classroom improves student learning in health professions education: a meta-analysis. BMC medical education. 2018 Dec;18:1-2. https://doi.org/10.1186/s12909-018-1144-z
9. SrivaSTava TK, Mishra V, Waghmare LS. Formative Assessment Classroom Techniques (FACTs) for better learning in pre-clinical medical education: A controlled trial. Journal of Clinical and Diagnostic Research. 2018 Sep 1;12(9):JC01. DOI: 10.7860/JCDR/2018/35622.11969
10. Singh K, Bharatha A, Sa B, Adams OP, Majumder MA. Teaching anatomy using an active and engaging learning strategy. BMC medical education. 2019 Dec;19:1-8. https://doi.org/10.1186/s12909-019-1590-2
11. de Carvalho Filho MA, Ledubino A, Frutuoso L, da Silva Wanderlei J, Jaarsma D, Helmich E, Strazzacappa M. Medical education empowered by theater (MEET). Academic Medicine. 2020 Aug 1;95(8):1191-200. DOI: 10.1097/ACM.0000000000003271.
12. Morris MC, Conroy P. Development of a simulation-based sub-module in undergraduate medical education. Irish Journal of Medical Science (1971-). 2020 Feb;189:389-94. https://doi.org/10.1007/s11845-019-02050-3
13. McGeorge E, Coughlan C, Fawcett M, Klaber RE. Quality improvement education for medical students: a near-peer pilot study. BMC Medical Education. 2020 Dec;20:1-7. https://doi.org/10.1186/s12909-020-02020-9
14. RAMYA C, SANDHYA VK, RAMYA P, RENUKA IV, ATCHYUTA M, ANUSHA M, GARIMA B, MEGHANA B. A Study on Perception of Students Regarding Newer Teaching Methods in Medical Education. Journal of Clinical and Diagnostic Research. 2020 Aug 1;14(8). DOI10.7860/JCDR/2020/44221.13925
15. Sahadevan S, Kurian N, Mani AM, Kishor MR, Menon V. Implementing competency‐based medical education curriculum in undergraduate psychiatric training in India: Opportunities and challenges. Asia-pacific psychiatry. 2021 Dec;13(4):e12491. https://doi.org/10.1111/appy.12491
16. Choudhari SG, Gaidhane AM, Desai P, Srivastava T, Mishra V, Zahiruddin SQ. Applying visual mapping techniques to promote learning in community-based medical education activities. BMC medical education. 2021 Dec;21:1-4. https://doi.org/10.1186/s12909-021-02646-3
17. Kopel J, Brower G, Culberson JW. Teaching methods fostering enjoyment and creativity in medical education. Journal of Community Hospital Internal Medicine Perspectives. 2021 Nov 2;11(6):821-4 https://doi.org/10.1080/20009666.2021.1979739
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Deepak Malla, Aurolipy Das.
Data curation: Deepak Malla, Aurolipy Das.
Formal analysis: Deepak Malla, Aurolipy Das.
Drafting - original draft: Deepak Malla, Aurolipy Das.
Writing - proofreading and editing: Deepak Malla, Aurolipy Das.