doi: 10.56294/mw2023107
ORIGINAL
Analyzing Surgical Competency Development through Robotic and Laparoscopic Simulation-Based Training
Análisis del desarrollo de competencias quirúrgicas mediante formación basada en simulación robótica y laparoscópica
Harsh Bhati1 ![]() , Jitendra Narayan Senapati2
, Jitendra Narayan Senapati2
![]()
1Noida International University, Department of General Surgery. Greater Noida, Uttar Pradesh, India.
2IMS and SUM Hospital, Siksha ‘O’ Anusandhan (deemed to be University), Department of General Surgery. Bhubaneswar, Odisha, India.
Cite as: Bhati H, Senapati JN. Analyzing Surgical Competency Development through Robotic and Laparoscopic Simulation-Based Training. Seminars in Medical Writing and Education. 2023; 2:107. https://doi.org/10.56294/mw2023107
Submitted: 05-09-2022 Revised: 17-12-2022 Accepted: 23-02-2023 Published: 24-02-2023
Editor:
PhD. Prof. Estela Morales Peralta ![]()
ABSTRACT
Minimally invasive surgery is becoming increasingly common, yet laparoscopic techniques often present a steep learning curve. Robotic surgical systems can offer a more efficient training pathway. The research compared robotic and laparoscopic simulation-based training in developing surgical competency among surgical trainees and medical students. A total of 230 participants were randomly assigned to two groups: surgical trainees (group 1, n=115) and medical students (group 2, n=115). Group 1 received 6 hours of laparoscopic or robotic simulation training before completing three surgical tasks with cadaveric varieties. Group 2 underwent 3 hours of training on either platform and completed a single surgical task. Performance was assessed using the Surgical Competency Assessment Tool (SCAT, maximum score of 30), the time taken to complete each task and the number of suture errors. The results showed that group 1 demonstrated significantly better performance after robotic training, with a median SCAT score of 27,00 for the robotic group compared to 18,00 for the laparoscopic group (P < 0,001). The robotic group also made fewer errors in both continuous and interrupted sutures (P < 0,001). Similarly, group 2 completed more interrupted sutures with fewer errors and less time when trained on the robotic platform (P < 0,001). Additionally, both groups reported reduced fatigue and greater physical comfort with robotic training (P < 0,001). Using SPSS (version 25), data were analyzed by applying descriptive statistics, Mann-Whitney U tests for non-parametric data, and independent t-tests for continuous variables. These findings suggest that robotic simulation-based training enhances the development of surgical competency more effectively than laparoscopic training.
Keywords: Laparoscopic Techniques; Surgical Competency; Surgical Trainees; Medical Students; Robotic Training; Cadaveric Specimens.
RESUMEN
La cirugía mínimamente invasiva es cada vez más frecuente, pero las técnicas laparoscópicas suelen presentar una curva de aprendizaje pronunciada. Los sistemas quirúrgicos robóticos pueden ofrecer una vía de formación más eficiente. La investigación comparó la formación basada en simulación robótica y laparoscópica en el desarrollo de la competencia quirúrgica entre aprendices de cirugía y estudiantes de medicina. Un total de 230 participantes fueron asignados aleatoriamente a dos grupos: aprendices de cirugía (grupo 1, n=115) y estudiantes de medicina (grupo 2, n=115). El grupo 1 recibió 6 horas de formación en simulación laparoscópica o robótica antes de completar tres tareas quirúrgicas con variedades cadavéricas. El grupo 2 recibió 3 horas de formación en cualquiera de las plataformas y completó una única tarea quirúrgica. El rendimiento se evaluó mediante la herramienta de evaluación de la competencia quirúrgica (SCAT, puntuación máxima de 30), el tiempo empleado en completar cada tarea y el número de errores de sutura. Los resultados mostraron que el grupo 1 demostró un rendimiento significativamente mejor tras la formación robótica, con una puntuación media SCAT de 27,00 para el grupo robótico en comparación con 18,00 para el grupo laparoscópico (p < 0,001). El grupo robótico también cometió menos errores tanto en las suturas continuas como en las interrumpidas (P < 0,001). Del mismo modo, el grupo 2 completó más suturas interrumpidas con menos errores y en menos tiempo cuando se entrenó en la plataforma robótica (P < 0,001). Además, ambos grupos informaron de una menor fatiga y una mayor comodidad física con el entrenamiento robótico (P < 0,001). Utilizando SPSS (versión 25), se analizaron los datos aplicando estadísticas descriptivas, pruebas U de Mann-Whitney para datos no paramétricos y pruebas t independientes para variables continuas. Estos resultados sugieren que la formación basada en la simulación robótica mejora el desarrollo de la competencia quirúrgica de forma más eficaz que la formación laparoscópica.
Palabras clave: Técnicas Laparoscópicas; Competencia Quirúrgica; Aprendices de Cirugía; Estudiantes de Medicina; Formación Robótica; Muestras Cadavéricas.
INTRODUCTION
Surgical trials present methodological issues as surgeon training, experience, and skills impact the delivery of surgical therapies, resulting in diversity in health practices and results. Surgical quality assurance can aid adherence to pre-defined criteria and outcome metrics, allowing for valid comparison across numerous clinical trial locations.(1) Technical competency and surgical abilities have an influence on patients' Quality of Life (QoL) and oncological consequences, independent of surgeon experience. Robot aided surgery has various advantages for the patients, including fewer blood transfusions, quicker rehabilitation, lower blood loss, and faster recovery, as well as increased dexterity, simplified suturing, access to deep anatomical regions, magnification, and 3-D imaging.(2)
Laparoscopic surgery, a type of minimally invasive surgery, is helping patients to improve their quality of life. In the operating room, a camera assistant guides the laparoscope based on verbal directions from the surgeon. Commercialization has occurred for 3D high-definition laparoscopes.(3) To master laparoscopy, students must have a certain set of talents. Simulation-based training (SBT) is an efficient way to obtain these people. Simulation training has proven to be transferable to clinical settings and has the possible to improve safety of the patient and care productivity.(4)
SBT is a significant tool for skill growth in a competency based course, particularly for laparoscopic surgery, because of its exclusive learning curve, the requirement for the practice, and safety problems for the patients.(5) Robotic surgery has been widely accepted in a variety of surgical disciplines. With new surgical tools, robotic surgery like laparoscopy necessitates intensive training that establishes current and evidence-based teaching paradigms.(6)
To minimize major adverse outcomes for patients as a result of the learning curve, simulation training in robotic surgery is required prior to entering clinical practice. Surgical simulation is a technique that immerses the learner in a scenario that is most similar to reality to teach both basic skills and full interventions.(7) To help surgical trainees and medical students increase their surgical competency, this research compared the robotic and laparoscopic simulation-based training.
To evaluate skill transference and examine learning curves in first-year medical students, the research (8) evaluated the performance of robotic and laparoscopic surgery. Simulator tests were administered to forty randomly selected pupils. Laparoscopic abilities were found to enhance robotic performance. The lack of a long-term evaluation and a limited sample size are among the limitations. 33 obstetrics and gynecology residents participated, to measure and improve their fundamental laparoscopic abilities via simulation.(9) Five surgical activities were completed by participants using a modified OSATs scale; senior trainees scored higher than juniors. After many sessions, scores improved noticeably. The limited sample size and single-institution research design are limitations. The effect of several training platforms on robotic surgical trainees was examined in research.(10) A summary of the literature from PubMed and Google Scholar was part of the methodology. The findings demonstrated that new platforms, courses, and simulations improve robotic proficiency. Peer evaluation is scarce in the curriculum, and little is known about how simulation abilities translate to success in the real world. The absence of approved curricula and outcomes data that connect simulation to patient outcomes is one of the limitations.
A virtual reality simulator for teaching and evaluating robotic surgical abilities was validated.(11) Over the course of four sessions, surgeons with different levels of competence finished five activities on the da Vinci Skills Simulator. The findings indicated a modest relationship between performance and robotic experience, with notable variations in scores throughout experience levels. With practice, every group got better. The requirement for further validation prior to use in certification or high-stakes evaluation is one of the limitations.
Laparoscopic training and its effect on robotic surgical abilities were assessed(13) along with the effects of a robotic simulation curriculum. There were three groups of twenty-seven trainees: robotic simulator training, FLS box trainer, and no training. According to the results, FLS training outperformed robotic simulation in improving knot tying. The comparison between robotic training versus no training revealed no discernible differences. Both the small sample size and the short training period are limitations. The predictive usefulness of surgical skills from robotic virtual reality simulators for intraoperative performance was evaluated(14) along with their transferability to the operating room. Eight qualitative and three quantitative research were systematically reviewed and meta-analyzed utilizing a random-effects model and correlation coefficients. A positive correlation (r = 0,67) and skill transfer were demonstrated by the results. Potential bias in research selection and a limited sample size are among the limitations.
The effectiveness of parameter-based feedback in laparoscopic training for surgical residents was evaluated.(15) MaxForce, route length, and time measurements were used to assess the residents' proficiency with instruments and tissue manipulation using the ForceSense system. After training, the results indicated a considerable improvement in every measure. However, the lack of long-term follow-up to assess persistent skill retention and the small sample size are its limitations. For robotic surgery, a simulation-based evaluation for operational competency in vaginal cuff closure was approved.(16) The VR module was completed six times by eleven inexperienced and eleven seasoned gynecological surgeons, and 18 metrics were evaluated. A pass/fail criterion of 75/100 was created when the results revealed notable performance discrepancies. False positives and negatives were among the limitations, indicating that the proficiency-based training standard can be enhanced.
METHOD
The methodology section describes the design, participant selection, training protocols, assessment tools and statistical analysis utilized in the research to compare robotic and laparoscopic simulation-based training for surgical competency development.
Participants
A total of 230 participants were collected for the research and separated into two groups: 115 surgical trainees (group 1) and 115 medical students (group 2). These participants were randomized either into the robotic or laparoscopic simulation training modules. Group 2 had minimal experience with group 1, but group 1 had significant field training. Table 1 and figure 1 represent the participant’s demographic features.
|
Table 1. Participant’s Demographic Features |
||
|
Features |
Group 1 (n (%) |
Group 2 (n (%) |
|
Age (years) |
||
|
22–25 |
13 (11,3) |
77 (67,0) |
|
26–30 |
74 (64,3) |
38 (33,0) |
|
31–35 |
28 (24,4) |
0 (0,0) |
|
Gender |
||
|
Female |
49 (42,6) |
57 (49,6) |
|
Male |
66 (57,4) |
58 (50,4) |
|
Prior Simulation Training |
||
|
Yes |
47 (40,9) |
35 (30,4) |
|
No |
68 (59,1) |
80 (69,6) |
|
Previous Laparoscopic Experience |
||
|
Yes |
71 (61,7) |
18 (15,7) |
|
No |
44 (38,3) |
97 (84,3) |
|
Previous Robotic Experience |
||
|
Yes |
30 (26,1) |
5 (4,3) |
|
No |
85 (73,9) |
110 (95,7) |
|
Hand Dominance |
||
|
Right |
108 (93,9) |
110 (95,7) |
|
Left |
7 (6,1) |
5 (4,3) |
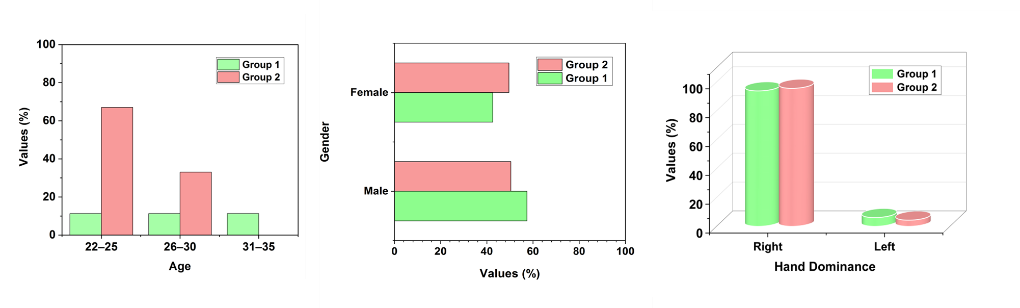
Figure 1. Graphical Representation of Participant’s Demographic
More participants (64,3 %) in group 1 were between the ages of 26 and 30 than in group 2, where the majority (67,0 %) was between the ages of 22 and 25. Both groups had a similar gender composition, with men making up 50,4 % of group 2 and 57,4 % of group 1. Prior experience differed greatly; for example, group 1 had more robotic experience (26,1 %) than group 2 (4,3 %), and 61,7 % of group 1 had laparoscopic experience compared to just 15,7 % in group 2.
Training Protocol
To accommodate the participant's varying degrees of expertise, the training protocols for both groups differed in length and difficulty.
· Group 1: this group consisted of 115 participants who underwent six hours of simulated training on the robotic or laparoscopic platforms before completing three surgical tasks with cadaveric varieties. The cadaveric specimens enriched the teaching environment since learners were able to hone their skills on real human flesh.
· Group 2: group 2 had 115 medical students who were trained for three hours on the robotic or laparoscopic simulation platforms. Unlike group 1, this group performed only one surgical procedure after they completed their training.
Assessment Tools
The Surgical Competency Assessment Tool (SCAT) was used to measure overall surgical competency with a maximum score of 30. It measured a variety of skills, including accuracy, coordination, and procedural knowledge. Suturing ability of the participants was also measured by quantifying interrupted and continuous suture errors, fewer errors indicating improved performance.
Statistical Analysis
IBM SPSS 25 was applied to analyze the data of the research. Descriptive statistics were employed first to get an overview of the characteristics of the data for continuous data like SCAT scores and time taken to complete tasks. Non-parametric data like the number of suture errors were compared using Mann-Whitney U tests between the robotic training group and laparoscopic training group. Independent t-tests were employed to determine significant differences in task completion time for continuous variables.
RESULTS
In this section, statistics were calculated using the three statistical tests through SPSS version 25.0. The SCAT was used to measure performance, and the number of suture errors and the time spent on each task.
Performance Evaluation of SCAT Scores
To compare the SCAT results with the robotic and laparoscopic groups, a Mann-Whitney U test was employed. The robotic group also possessed a higher median SCAT score in group 1 as well as group 2, reflecting increased operating capability with robot training as shown in figure 2 and table 2.
|
Table 2. Outcomes of SCAT Scores |
||||
|
Groups |
Training Type |
Median SCAT Score |
U Value |
P-Value |
|
Group 1 |
Robotic |
27,00 |
2,431,5 |
<0,001 |
|
Laparoscopic |
18,00 |
|||
|
Group 2 |
Robotic |
21,00 |
2,617,0 |
<0,001 |
|
Laparoscopic |
15,00 |
|||
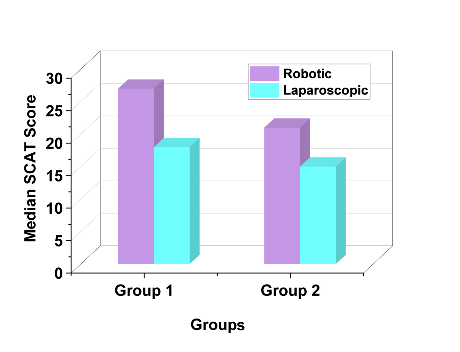
Figure 2. Graphical representation of Median SCAT Score
It reveal that group 1 had a median SCAT score of 27,00 in the robotic training group compared with 18,00 for laparoscopic training (U = 2 431,5, P < 0,001). Group 2 scored 21,00 on the robotic team compared with 15,00 on the laparoscopic team (U = 2 617,0, P < 0,001). These findings indicate that robotic training improves surgical competency more effectively than traditional laparoscopic approaches.
Suture Errors
The number of suture errors was compared using independent t-tests for both continuous and interrupted suturing. The robotic training group produced far fewer errors than the laparoscopic group, showing greater accuracy and control as shown in figure 3 and table 3.
|
Table 3. Outcomes of Suture Errors |
|||||
|
Groups |
Training Type |
Continuous Suture Errors (Mean ± SD) |
Interrupted Suture Errors (Mean ± SD) |
t Value |
P-Value |
|
Group 1 |
Robotic |
2,1 ± 0,8 |
3,0 ± 1,2 |
4,21 |
<0,001 |
|
Laparoscopic |
4,5 ± 1,3 |
6,2 ± 1,8 |
|||
|
Group 2 |
Robotic |
2,9 ± 0,9 |
4,1 ± 1,5 |
3,78 |
<0,001 |
|
Laparoscopic |
5,3 ± 1,5 |
7,4 ± 2,1 |
|||
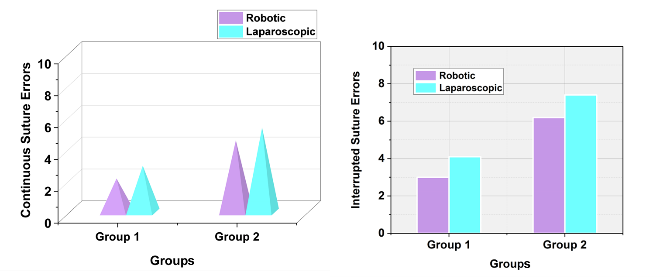
Figure 3. Graphical representation of Suture Errors
It shows that the robotic training group produced considerably fewer errors in both continuous and intermittent suturing than the laparoscopic group among both groups. In group 1, the robotic group had an average of 2,1 ± 0,8 continuous suture errors and 3,0 ± 1,2 interrupted suture errors, while the laparoscopic group had 4,5 ± 1,3 and 6,2 ± 1,8, respectively (P < 0,001). In group 2, robotic trainees had significantly lower errors (2,9 ± 0,9 continuous, 4,1 ± 1,5 interrupted) than laparoscopic trainees (5,3 ± 1,5 continuous, 7,4 ± 2,1 interrupted) (P < 0,001).
Completion Time of Surgical Task
To compare the time needed to execute each surgical task, a Mann-Whitney U test was utilized. The robotic group finished tasks substantially faster than the laparoscopic group, indicating more efficiency as given in figure 4 and table 4.
|
Table 4. Outcomes of Completion Time |
||||
|
Groups |
Training Type |
Median Time (Minutes) |
U Value |
P-Value |
|
Group 1 |
Robotic |
15,2 |
2 618,0 |
<0,001 |
|
Laparoscopic |
22,4 |
|||
|
Group 2 |
Robotic |
18,7 |
2 754,5 |
<0,001 |
|
Laparoscopic |
27,3 |
|||
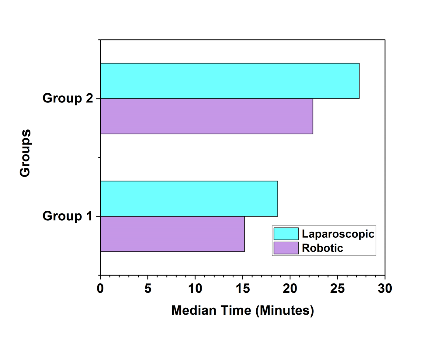
Figure 4. Graphical representation of Completion Time
It show that both group 1 and group 2 used significantly fewer minutes to finish surgical activities in the robotic training group. The median time for robotically trained group 1 was 15,2 minutes, whereas the median time for laparoscopically trained trainees was 22,4 minutes. Comparably, group 2 who received training on the robotic platform finished tasks in 18,7 minutes as compared to 27,3 minutes for those who received laparoscopic training. Compared to standard laparoscopic training, the results (P < 0,001) imply that robotic simulation training enhances procedural efficiency, allowing for quicker completion of tasks.
Fatigue and Physical Comfort Scores
The degree of physical comfort and self-reported fatigue were measured as given in figure 5 and table 5. Higher comfort ratings and noticeably less fatigue were observed by the robotic training group, indicating a more ergonomic and user-friendly learning environment.
|
Table 5. Outcomes of Fatigue and Physical Comfort Scores |
|||||
|
Group |
Training Type |
Fatigue Score (Mean ± SD) |
Comfort Score (Mean ± SD) |
t Value |
P-Value |
|
Group 1 |
Robotic |
2,3 ± 0,7 |
8,4 ± 1,1 |
5,02 |
<0,001 |
|
Laparoscopic |
4,8 ± 1,2 |
5,9 ± 1,5 |
|||
|
Group 2 |
Robotic |
2,7 ± 0,8 |
7,9 ± 1,3 |
4,76 |
<0,001 |
|
Laparoscopic |
5,2 ± 1,3 |
5,5 ± 1,7 |
|||
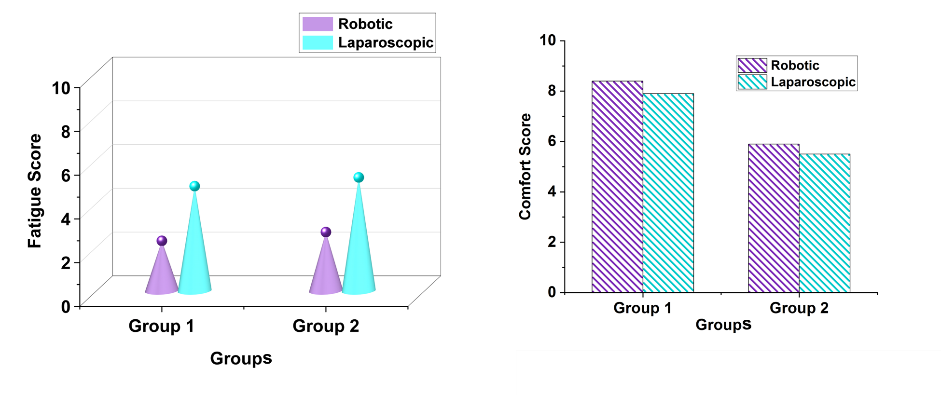
Figure 5. Graphical representation of Fatigue and Physical Comfort Scores
Participants in the robotic training group expressed considerably less weariness and more comfort than those in the laparoscopic group. Group 2 exhibited a similar tendency (2,7 ± 0,8 vs. 5,2 ± 1,3), whereas group 1 achieved a mean fatigue score of 2,3 ± 0,7 with robotic training, compared to 4,8 ± 1,2 in the laparoscopic group. Moreover, the robotic group reported higher levels of comfort (8,4 ± 1,1 in group 1 and 7,9 ± 1,3 in group 2) compared to the laparoscopic group (5,9 ± 1,5 and 5,5 ± 1,7, respectively). By lowering physical strain and enhancing overall training conditions, these results imply that robotic training provides a more ergonomic and user-friendly experience.
Descriptive Statistics
Descriptive statistics summarize and arrange data to give a clear image of its essential features, such as mean, median, standard deviation (SD). When examining surgical competency development, these data aid in comparing performance indicators (SCAT scores, errors, and Task completion time, Fatigue Score) between two groups as given in figure 6 and table 6. They include an overview of trends and variability in trainee outcomes. This helps to identify general performance differences before running inferential tests. Table 6 shows summary data for four important performance metrics such as SCAT Score, Suture Errors, Fatigue Score and Task Completion Time. The SCAT Score assesses surgical ability, Suture Errors indicate technical correctness, and Completion Time (minutes) evaluates efficiency.
|
Table 6. Outcomes of the Descriptive Statistics |
||
|
Metric |
Group 1 |
Group 2 |
|
SCAT Score (Median, IQR) |
23,00 (20,0-27,0) |
20,50 (17,0-24,0) |
|
Suture Errors (Mean ± SD) |
2,5 ± 1,1 |
3,2 ± 1,4 |
|
Task Completion Time (Min, Mean ± SD) |
15,7 ± 2,9 |
18,4 ± 3,2 |
|
Fatigue Score (VAS, Mean ± SD) |
3,4 ± 1,2 |
4,6 ± 1,5 |
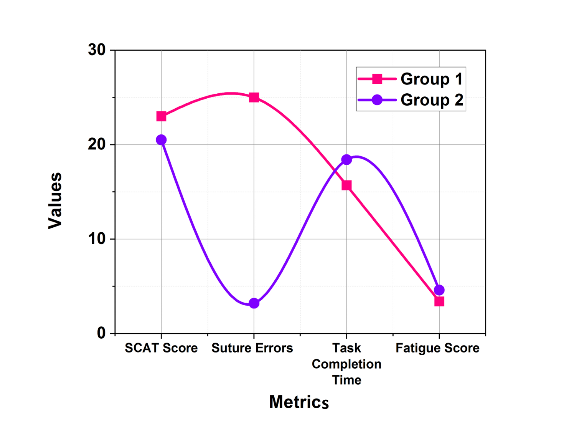
Figure 6. Graphical representation of Descriptive Statistics
The performance measures show that group 1 had a higher median SCAT score (23,00) than group 2 (20,50), indicating more competency. Group 1 also had fewer suture errors (2,5 vs. 3,2) and finished activities quicker (15,7 vs. 18,4 minutes). Furthermore, group 1 reported lower fatigue levels (3,4 vs. 4,6), indicating improved physical comfort during training. These data emphasize surgical trainees' higher efficiency and lower fatigue compared to medical students.
Mann-Whitney U Test
The Mann-Whitney U test is a non-parametric test for associating two independent groups whose data is not regularly distributed. It helps to assess differences in SCAT scores, errors, and completion times between two groups. This test ensures a valid comparison as competency scores cannot follow a normal distribution. A significant result suggests that one training method leads to superior skill development. It evaluates the variances between both groups as shown in table 7 for non-normally distributed data. This test reports the U statistic, Mean Rank, sum of Mean Rank and P-value after comparing the two groups' SCAT scores, suture errors, and completion times. The rank-based difference between two independent groups is represented by the U statistic. A lower number indicates a significant difference between groups. The P-value establishes the statistical significance.
|
Table 7. Outcomes of the Mann-Whitney U Test |
|||||
|
Variable |
Group |
Mean Rank |
Sum of Ranks |
U statistic |
P-value |
|
SCAT Score |
Group 1 |
130,5 |
15 007,5 |
850,5 |
< 0,001 |
|
Group 2 |
100,5 |
11 557,5 |
870,0 |
< 0,001 |
|
|
Suture Errors |
Group 1 |
125,0 |
14 375,0 |
720,0 |
< 0,001 |
|
Group 2 |
106,0 |
12 190,0 |
735,5 |
< 0,001 |
|
|
Completion Time |
Group 1 |
128,0 |
14 720,0 |
800,0 |
< 0,001 |
|
Group 2 |
103,0 |
11 845,0 |
815,0 |
< 0,001 |
|
It reveals that group 1 had considerably higher SCAT scores (Mean Rank = 130,5, Sum of Ranks = 15 007,5, U = 850,5, P < 0,001) than group 2 (Mean Rank = 100,5). Group 1 made fewer suture errors (Mean Rank = 125,0, U = 720,0, P < 0,001) compared to group 2 (Mean Rank = 106,0). Group 1 performed tasks quicker (Mean Rank = 128,0, U = 800,0, P < 0,001) than group 2 (Mean Rank = 103,0).
Independent t-Test
The independent t-test analyzes the means of two independent groups to examine if they differ statistically significantly. The research assesses whether robotic training significantly improves SCAT scores, lowers suture errors, and shortens completion times when compared to laparoscopic training. The test presupposes normality in data distribution as it is appropriate for continuous variables. A substantial p-value provides support to the concept that surgical ability is improved more efficiently through robotic simulation. It returns t-values, Degrees of freedom (df), P-values, and effect sizes (d) as shown in table 8. The t-value is a statistic that evaluates the difference between means of two groups when compared with the data's variance. The df = 228 is the number of independent values in a statistical computation that influence the test's reliability. The P-value indicates the probability of achieving the reported findings assuming there is no genuine difference between groups. Effect size is the amount of the difference between two groups, with d > 0,8 demonstrating a strong impact.
|
Table 8. Outcomes of the Independent t-Test |
||||||
|
Variable |
Comparison |
Groups |
t-value |
df |
P-value |
d |
|
SCAT Score |
Robotic vs. Laparoscopic |
Group 1 |
10,85 |
228 |
< 0,001 |
1,92 |
|
Group 2 |
9,95 |
1,75 |
||||
|
Suture Errors |
Robotic vs. Laparoscopic |
Group 1 |
-7,65 |
228 |
< 0,001 |
-1,43 |
|
Group 2 |
-6,98 |
-1,32 |
||||
|
Completion Time |
Robotic vs. Laparoscopic |
Group 1 |
-8,72 |
228 |
< 0,001 |
-1,55 |
|
Group 2 |
-7,95 |
-1,48 |
||||
The t-test indicates considerable performance increases in robotic training, with high t-values and large effect sizes (d > 1,3) for all variables. The large effect sizes show that the differences are both statistically significant and practically important. This test's benefit is that it can measure the strength of differences between groups. This demonstrates the practical application of robotic training to surgical skill improvement.
DISCUSSION
The results demonstrate that robotic simulation-based training is more effective than laparoscopic training at developing surgical competency. Based on the descriptive statistics, robotic trainees completed tasks faster, made fewer suture errors, and recorded higher SCAT scores. The results were maintained even with data that was not evenly distributed since the Mann-Whitney U test showed statistically significant differences between the groups. The independent t-test also revealed significant effect sizes, proving the effectiveness of robotic training. These results suggest that robotic platforms provide an easier-to-use and more ergonomic learning space with reduced physical and mental stress and improved accuracy. Employing a range of techniques, the research achieves robust statistical validation for training effectiveness, ensuring reliability and real-world applicability in surgical training.
CONCLUSIONS
The research established that robotic simulation-based training was superior to laparoscopic training in the establishment of surgical competence among surgical trainees and medical students. Students trained on the robotic platform scored higher SCAT scores, committed fewer suture errors, and completed tasks quicker than students trained on the laparoscopic platform. Robotic training is also fewer fatiguing and enhances physical comfort, and therefore, it is ideal for training surgeons. According to the results, group 1 performed significantly better after robotic training with the robotic group's median SCAT score was 27,00, when the laparoscopic group’s median SCAT score was 18,00. Statistical comparison between the two training methods showed significant differences, which confirmed the findings. In general, the results suggested that robotic simulation was a more efficient and ergonomically beneficial training method, potentially enhancing skill acquisition and surgical performance for minimally invasive surgery. Disadvantages of the research include brief training duration, lack of realistic patient cases, and high student learning curve heterogeneity, which can affect generalizability. Future research could be aimed at long-term skill retention, real surgical competency, and cost-effectiveness of robot training in many surgical subspecialties.
BIBLIOGRAPHIC REFERENCES
1. Moloney, K., Janda, M., Frumovitz, M., Leitao, M., Abu-Rustum, N.R., Rossi, E., Nicklin, J.L., Plante, M., Lecuru, F.R., Buda, A. and Mariani, A., 2021. Development of a surgical competency assessment tool for sentinel lymph node dissection by minimally invasive surgery for endometrial cancer. International Journal of Gynecological Cancer: Official Journal of the International Gynecological Cancer Society, 31(5), pp.647-655. https://doi.org/10.1136/ijgc-2020-002315
2. Chen J, Oh PJ, Cheng N, Shah A, Montez J, Jarc A, Guo L, Gill IS, Hung AJ. Use of automated performance metrics to measure surgeon performance during robotic vesicourethral anastomosis and methodical development of a training tutorial. The Journal of urology. 2018 Oct 1;200(4):895-902. https://doi.org/10.1016/j.juro.2018.05.080
3. Kawashima K, Kanno T, Tadano K. Robots in laparoscopic surgery: current and future status. BMC Biomedical Engineering. 2019 Dec;1:1-6. https://doi.org/10.1186/s42490-019-0012-1
4. Fjørtoft K, Konge L, Gögenur I, Thinggaard E. The implementation gap in laparoscopic simulation training. Scandinavian Journal of Surgery. 2019 Jun;108(2):109-16. https://doi.org/10.1177/1457496918798201
5. Charokar K, Modi JN. Simulation-based structured training for developing laparoscopy skills in general surgery and obstetrics & gynecology postgraduates. Journal of Education and Health Promotion. 2021 Jan 1;10(1):387. https://doi.org/10.4103/jehp.jehp_48_21
6. Bresler L, Perez M, Hubert J, Henry JP, Perrenot C. Residency training in robotic surgery: the role of simulation. Journal of Visceral Surgery. 2020 Jun 1;157(3):S123-9.. https://doi.org/10.1016/j.jviscsurg.2020.03.006
7. Scott SI, Dalsgaard T, Jepsen JV, von Buchwald C, Andersen SA. Design and validation of a cross‐specialty simulation‐based training course in basic robotic surgical skills. The International Journal of Medical Robotics and Computer Assisted Surgery. 2020 Oct;16(5):1-0. https://doi.org/10.1002/rcs.2138
8. Kanitra JJ, Khogali-Jakary N, Gambhir SB, Davis AT, Hollis M, Moon C, Gupta R, Haan PS, Anderson C, Collier D, Henry D. Transference of skills in robotic vs. laparoscopic simulation: a randomized controlled trial. BMC surgery. 2021 Dec;21:1-8. https://doi.org/10.1186/s12893-021-01385-y
9. Mannella P, Malacarne E, Giannini A, Russo E, Caretto M, Papini F, Montt Guevara MM, Pancetti F, Simoncini T. Simulation as tool for evaluating and improving technical skills in laparoscopic gynecological surgery. BMC surgery. 2019 Dec;19:1-9. https://doi.org/10.1186/s12893-019-0610-9
10. Azadi S, Green IC, Arnold A, Truong M, Potts J, Martino MA. Robotic surgery: the impact of simulation and other innovative platforms on performance and training. Journal of minimally invasive gynecology. 2021 Mar 1;28(3):490-5. https://doi.org/10.1016/j.jmig.2020.12.001
11. Havemann MC, Dalsgaard T, Sørensen JL, Røssaak K, Brisling S, Mosgaard BJ, Høgdall C, Bjerrum F. Examining validity evidence for a simulation-based assessment tool for basic robotic surgical skills. Journal of Robotic Surgery. 2019 Feb 11;13:99-106. https://doi.org/10.1007/s11701-018-0811-8
12. Kanitra JJ, Khogali-Jakary N, Gambhir SB, Davis AT, Hollis M, Moon C, Gupta R, Haan PS, Anderson C, Collier D, Henry D. Transference of skills in robotic vs. laparoscopic simulation: a randomized controlled trial. BMC surgery. 2021 Dec;21:1-8. https://doi.org/10.1186/s12893-021-01385-y
13. Schmidt MW, Köppinger KF, Fan C, Kowalewski KF, Schmidt LP, Vey J, Proctor T, Probst P, Bintintan VV, Müller-Stich BP, Nickel F. Virtual reality simulation in robot-assisted surgery: meta-analysis of skill transfer and predictability of skill. BJS open. 2021 Mar;5(2):zraa066. https://doi.org/10.1093/bjsopen/zraa066
14. Hardon SF, van Gastel LA, Horeman T, Daams F. Assessment of technical skills based on learning curve analyses in laparoscopic surgery training. Surgery. 2021 Sep 1;170(3):831-40. https://doi.org/10.1016/j.surg.2021.04.024
15. Newcomb LK, Bradley MS, Truong T, Tang M, Comstock B, Li YJ, Visco AG, Siddiqui NY. Correlation of virtual reality simulation and dry lab robotic technical skills. Journal of minimally invasive gynecology. 2018 May 1;25(4):689-96. https://doi.org/10.1016/j.jmig.2017.11.006
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Harsh Bhati, Jitendra Narayan Senapati.
Data curation: Harsh Bhati, Jitendra Narayan Senapati.
Formal analysis: Harsh Bhati, Jitendra Narayan Senapati.
Drafting - original draft: Harsh Bhati, Jitendra Narayan Senapati.
Writing - proofreading and editing: Harsh Bhati, Jitendra Narayan Senapati.