doi: 10.56294/mw2023110
ORIGINAL
Doctor-Patient Trust and Communication: A Dyadic Perspective on Relationship Interdependence and Reciprocity
Confianza y comunicación entre médico y paciente: Una perspectiva diádica de la interdependencia y la reciprocidad en la relación
Avir Sarkar1 ![]() , Manoranjan Dash2
, Manoranjan Dash2 ![]()
1Noida International University, Department of Obstetrics and Gynaecology. Greater Noida, Uttar Pradesh, India.
2Siksha ‘O’ Anusandhan (Deemed to be University), Department of Management. Bhubaneswar, Odisha, India.
Cite as: Sarkar A, Dash M. Doctor-Patient Trust and Communication: A Dyadic Perspective on Relationship Interdependence and Reciprocity. Seminars in Medical Writing and Education. 2023; 2:110. https://doi.org/10.56294/mw2023110
Submitted: 06-09-2022 Revised: 18-12-2022 Accepted: 24-02-2023 Published: 25-01-2023
Editor: PhD.
Prof. Estela Morales Peralta ![]()
ABSTRACT
Interpersonal trust shows a fundamental role in shaping the quality of doctor-patient interactions, directly influencing communication effectiveness, patient satisfaction, and adherence to medical recommendations. Understanding the dynamic interplay between doctor and patient trust levels can provide deeper insights into how communication processes unfold and how trust influences these exchanges. This exploration aims to explore the association between interpersonal trust and the quality of dyadic communication in healthcare settings. 200 participants were selected and participated in structured interviews and completed trust and communication quality assessments. Data were analyzed using SPSS (version 26) and AMOS for Structural Equation Modeling (SEM). Analysis of Variance (ANOVA) and regression analysis were performed to explore associations among the variables, while SEM was applied to test the structural relationships between trust perception, communication effectiveness, and adherence. The findings revealed a regression analyses of trust perception (β = 0,68, t =8,92) and doctor’s responsiveness (β = 0,64, t = 8,11). SEM results confirmed that higher trust perception significantly improves doctor communication (β = 0,68, p < 0,01), enhances patient trust (β = 0,64, p < 0,01), and doctor responsiveness (β = 0,63, p < 0,01). Additionally, improved communication effectiveness acted as a mediator between trust perception and patient adherence, reinforcing the importance of trust-building efforts. The investigation highlights that interpersonal trust plays a crucial role in enhancing doctor-patient communication. Higher trust levels lead to clearer information exchange, stronger emotional support, and greater adherence to medical advice.
Keywords: Doctor-Patient; Communication; Structural Equation Modeling (SEM); Emotional Support.
RESUMEN
La confianza interpersonal desempeña un papel fundamental en la calidad de las interacciones médico-paciente, ya que influye directamente en la eficacia de la comunicación, la satisfacción del paciente y el cumplimiento de las recomendaciones médicas. Comprender la interacción dinámica entre los niveles de confianza del médico y el paciente puede proporcionar una visión más profunda de cómo se desarrollan los procesos de comunicación y cómo influye la confianza en estos intercambios. El objetivo de esta investigación es explorar la asociación entre la confianza interpersonal y la calidad de la comunicación diádica en entornos sanitarios. Se seleccionaron 200 participantes que participaron en entrevistas estructuradas y completaron evaluaciones de la confianza y la calidad de la comunicación. Los datos se analizaron con SPSS (versión 26) y AMOS para el modelado de ecuaciones estructurales (SEM). Se realizaron análisis de varianza (ANOVA) y análisis de regresión para explorar las asociaciones entre las variables, mientras que el SEM se aplicó para probar las relaciones estructurales entre la percepción de confianza, la eficacia de la comunicación y la adherencia. Los resultados revelaron un análisis de regresión de la percepción de confianza (β = 0,68, t = 8,92) y la receptividad del médico (β = 0,64, t = 8,11). Los resultados del SEM confirmaron que una mayor percepción de confianza mejora significativamente la comunicación del médico (β = 0,68, p < 0,01), aumenta la confianza del paciente (β = 0,64, p < 0,01) y la receptividad del médico (β = 0,63, p < 0,01). Además, la mejora de la eficacia de la comunicación actuó como mediador entre la percepción de confianza y la adherencia del paciente, lo que refuerza la importancia de los esfuerzos de creación de confianza. La investigación pone de relieve que la confianza interpersonal desempeña un papel crucial en la mejora de la comunicación médico-paciente. Un mayor nivel de confianza conduce a un intercambio de información más claro, un mayor apoyo emocional y una mayor adherencia al consejo médico.
Palabras clave: Médico-Paciente; Comunicación; Modelización de Ecuaciones Estructurales (SEM); Apoyo Emocional.
INTRODUCTION
Doctor-patient trust and successful communication demand doctor and patient respect for each other as well as openness and active listening with empathy and clear sharing of information to enhance healthcare relationships and outcomes.(1) Underlying features of successful healthcare services are doctor-patient trust and communication because these elements drive patient outcomes and the degree of patient gratification and treatment adherence.(2) Patients who have confidence in their healthcare providers can willingly provide critical clinical information, thereby facilitating accurate medical diagnosis and appropriate treatment plans.(3) The establishment and operation of faith among patients and healthcare workers rely on the proper utilization of both verbal and non-verbal communication techniques.(4) The system allows patients to understand their state of health along with potential treatment options and medical rationale for health care decisions, hence allowing them to make informed health decisions.(5) Good communication habits include active listening along with empathy and non-judgmental behaviour that contribute to improved patient comfort coupled with increased trust in the physician.(6) Follow-up care and continuity of care are essential factors that support the doctor-patient relationship outside of clinical contact.(7) It assesses trust along with communication in healthcare environments through an extensive analysis of their impacts on treatment provision and their improvement strategies while examining provider issues for building meaningful relationships.(8)
Petrocchi S et al.(9) was trust variance structure using different analysis methods by verifying the interdependence of data to diagnose three various variance effects - doctor and patient variables, relationship variables, and reciprocal effects. Trust establishment through agreement in the case of patient-doctor relationships resulted in better health outcomes than traditional treatment practices. Multiple relationships among doctors and patients with a lack of affection by relating variables to various patient results through the Affection Exchange Theory (AET) are examined in Hesse C et al.(10). The results showed both affectionate communication and affection deprivation negatively affecting the majority of outcomes. Psychological contract violation that affects antisocial behaviour in patients was investigated in Chang PC et al.(11). The results established that psychological contract violations connected to patient trust created positive associations with patient antisocial behaviour.
An empathetic perspective of medical receptionists, nurses, and doctors to investigate interaction capabilities during diagnostic phases and therapeutic activities was explored in Akseer R et al.(12). Medical receptionists employ intake procedures that center on establishing patient rapport through important listening, compassionate behaviour, and professional courtesy. The way European patients felt about seven different facets of communication between doctors and patients was determined in Mazzi MA.(13). Placing more value on the doctor than on the patient gave doctors more responsibility, especially when it came to handling the patient as a person, and a partner, and maintaining stability of care. The way Patient-Centered Communication (PCC) influenced two essential consequences through patients’ trust development and improved assessment of healthcare superiority was evaluated in Hong H et al.(14). The strength of trust as a mediator factor between PCC and patient healthcare quality assessments increased when patients visited the hospital more frequently. Evidence-based strategies for General Practitioner (GP) interactions regarding oral medication initiation and evaluation or termination with the patients had been presented in Parker L et al.(15). The process of starting or changing oral medications became easier when healthcare professionals allocated additional time to discussions and used written educational materials while asking for help from pharmacist colleagues.
Hypothesis Development
H1: The communication style of doctors positively impacts patient adherence to medical recommendations.
Patients will believe medical information combined with explicit explanations and also opt to adhere to medical advice when their doctor comes to them with patient-centered communication.
H2: Patient trust perception positively impacts patient adherence to medical recommendations.
Trust in health relationships is critical because it serves to reduce anxiety among patient, increases their trust in medical decisions and facilitates their ongoing treatment compliance.
H3: Emotional support from physicians positively impacts the effect on patient adherence to medical recommendations.
Emotional support provides patients with a safe environment, which results in improved healthcare decision involvement as well as improved compliance with medical advice.
H4: Responsiveness of doctors positively impacts patient adherence to medical recommendations.
Patients feel more valued when physicians pay attention and respond to their personal needs; thus, their treatment adherence is enhanced.
H5: Patient health literacy positively impacts patient adherence to medical recommendations.
Knowledge of the medical condition and treatment needs of their doctor makes patients adhere to treatment protocols successfully.
METHOD
The exploration analyzes how trust between doctors and patients influences their communication effectiveness as well as their ability to share information, show emotional support and follow medical instructions. Doctor's communication style, patient trust perception, emotional support, doctor's responsiveness, and patient health literacy are the independent variables in this paradigm. The dependent variable is the patient's compliance with medical advice. The conceptual framework establishes interactions between trust, communication, and adherence to direct exploration analysis of their impacts on doctor-patient relationships, and the final results are shown in figure 1.
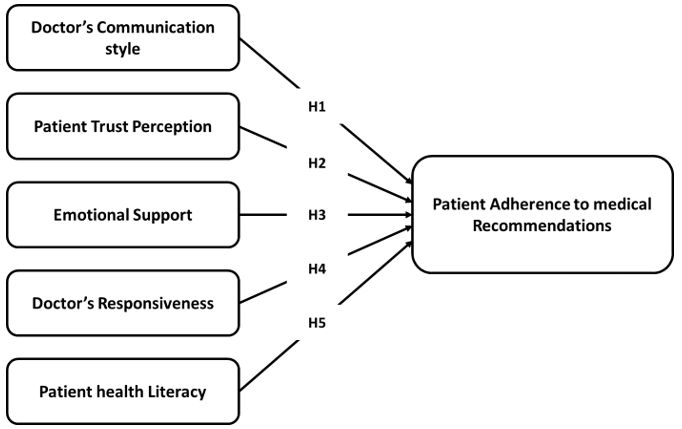
Figure 1. Conceptual Framework
Data Collection
The exploration gathered information from 200 volunteers who experienced structured interviews using standardized tests for measuring trust and communication quality. Purposive sampling enabled the exploration to select participants whose healthcare backgrounds diversified among the population. The chosen participant sample consisted of patients who had experienced recent doctor visits so explorers could analyze current dynamics of trust and communication quality in medical settings. Table 1 describes the demographic data of variables. The distribution of participants by healthcare experience and primary healthcare setting is represented as (a) and (b) in figure 2.
|
Table 1. Demographic data of variables |
|||
|
Demographic Variables |
Categories |
Frequency (n=200) |
Percentage (%) |
|
Gender |
Male |
95 |
47,5 |
|
Female |
105 |
52,5 |
|
|
Age Group |
18–30 |
50 |
25 |
|
31–45 |
60 |
30 |
|
|
46–60 |
55 |
27,5 |
|
|
61+ |
35 |
17,5 |
|
|
Healthcare Experience |
First-time patients |
40 |
20 |
|
Regular patients |
100 |
50 |
|
|
Chronic illness patients |
60 |
30 |
|
|
Doctor Visit Frequency
|
Rarely (≤1 visit/year) |
45 |
22,5 |
|
Occasionally (2-4 visits/year) |
85 |
42,5 |
|
|
Frequently (≥5 visits/year) |
70 |
35 |
|
|
Primary Healthcare Setting |
Public Hospital |
80 |
40 |
|
Private Hospital/Clinic |
90 |
45 |
|
|
Community Health Center |
30 |
15 |
|
|
Preferred Doctor-Patient Communication Style |
Directive (Doctor-Led) |
85 |
42,5 |
|
Collaborative (Shared Decision-Making) |
115 |
57,5 |
|
|
Language Proficiency in Healthcare |
Native Speaker |
160 |
80 |
|
Non-Native Speaker |
40 |
20 |
|
|
Previous Negative Medical Experiences |
Yes |
70 |
35 |
|
No |
130 |
65 |
|
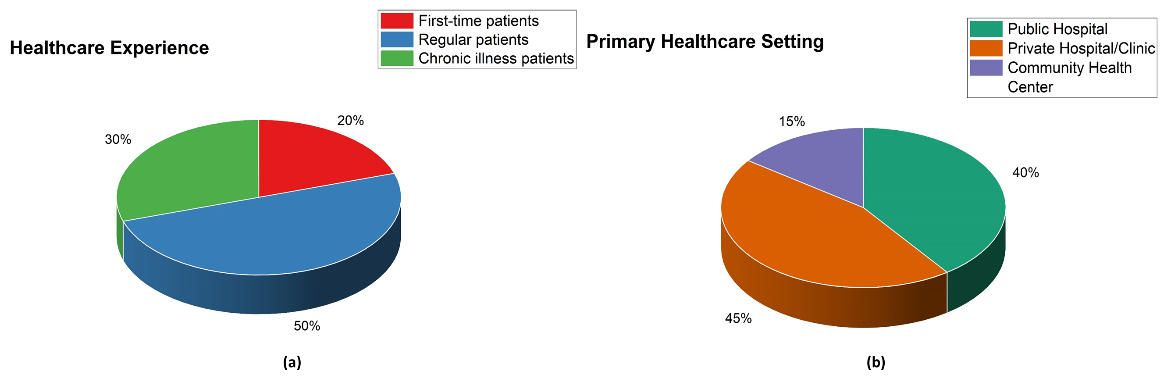
Figure 2. Distribution of Participants by Demographic variables (a) Healthcare Experience and (b) Primary healthcare setting
Structure of Questionnaires
Doctor’s communication style: This section contains four questions to evaluate a doctor's communication style. The questions address monitoring doctor-patient interactions regarding directive or collaborative approaches as well as explanation clarity, question encouragement and shared treatment decision-making.
Patient trust perception: Four questions are included in this part to assess several facets of patient trust perception. It focuses on patients’ trust in doctors’ honest behaviour together with their open communication and specialized skills and their willingness to listen leads patients to trust medical advice while building healthcare provider confidence.
Emotional support: This section contains four questions meant to assess emotional support. The inquiry focuses on survey explorers to assess how doctors listen to patients' medical concerns and demonstrate empathy along with offering reassurance for improved satisfaction outcomes.
Doctor’s responsiveness: This section contains four questions to evaluate a doctor's responsiveness. The questions explore the doctor's approach to rapid and efficient care of patient apprehensions and time distribution and explanation modifications to meet patient comprehension while preventing medical interactions from being rushed.
Patient health literacy: This section contains four questions meant to assess patient health literacy. The questions assess how well the patient understands medical explanations while determining their need for clarification and their independent exploration activity and health management confidence based on medical instructions. The sample questionnaires are represented in table 2.
|
Table 2. Sample Questionnaires |
||
|
Variables |
Number of Questions |
Survey Questions |
|
Doctor’s communication style |
4 |
1. How would you describe the doctor's communication approach? |
|
|
2. Does the doctor encourage you to ask questions during consultations? |
|
|
|
3. How clearly does the doctor explain medical conditions and treatments? |
|
|
|
|
4. Do you participate in the process of making decisions about your care? |
|
Patient trust perception |
4 |
1. How confident are you that the doctor acts in your best interest? |
|
|
2. Do you believe the doctor provides honest and transparent information? |
|
|
|
3. How comfortable do you feel sharing personal health concerns with your doctor? |
|
|
|
4. Do you trust the doctor’s medical expertise and recommendations? |
|
|
Emotional support |
4 |
1. How well does the doctor acknowledge your concerns and emotions? |
|
|
2. Does the doctor show empathy and understanding during consultations? |
|
|
|
3. How supported do you feel after speaking with your doctor? |
|
|
|
4. Does the doctor provide reassurance and encouragement during treatment discussions? |
|
|
Doctor’s responsiveness |
4 |
1. How quickly does the doctor respond to your concerns or questions? |
|
|
2. Does the doctor provide enough time for discussions during consultations? |
|
|
|
3. How well does the doctor adjust explanations based on your level of understanding? |
|
|
|
4. Have you ever felt rushed during a consultation with the doctor? |
|
|
Patient health literacy |
4 |
1. How confident are you in understanding the medical information provided by your doctor? |
|
|
2. Do you often need additional explanations or clarifications about medical terms? |
|
|
|
3. How frequently do you research your medical condition after a doctor’s consultation? |
|
|
|
4. Do you feel well-informed about managing your health based on the doctor’s advice? |
|
Statistical Assessment
The exploration utilized SPSS and AMOS to perform statistical evaluations about the connections in trust between healthcare workers and patients and their communication methods and medicine-taking practices. ANOVA served to evaluate trust and communication quality levels between groups while detecting distinct effects on adherence outcomes. Regression analysis determined how much trust influences actual communication results. The SEM analysis confirmed the influence of trust on clarity as well as emotional support and patient adherence through testing structural associations and mediation effects.
RESULTS
The exploration aimed to assess the key variables such as the doctor's communication style, patient trust perception, emotional support, doctor's responsiveness, and patient health literacy. Statistical analyses, which include ANOVA, Regression Analysis, and SEM Analysis, are used to examine relationships between trust, communication, and patient adherence.
ANOVA
Effective doctor-patient communication is a cornerstone of quality healthcare, influencing both clinical outcomes and patient satisfaction. Statistical results indicating ANOVA from five hypotheses (H1-H5) are presented below. Each of these five hypotheses is set with the mean square, degree of freedom (df = 1), F-value, p-value, sum of squares, and the size of the effect. H1 assigned values for the sum of squares 12,35, F-value 9,21, p-value 0,003, and least effect size 0,18, thus proving significance. H2 has the highest F-value (13,62), with a sum of squares of 18,45 and a p-value of 0,001. It also has the biggest effect size (0,24) and confirms strong significance. H3 shows the highest for the sum of squares (1078), effect size = 0,15, p-value = 0,005, F-value = 7,89, thus demonstrating significance. H4 gives a sum of squares of 9,12, an F-value (6,95), a p-value (0,009), and a minimum effect size (0,13), but is yet significant. H5 concludes by scoring an F-value of 10,42, the sum of squares of 14,2, a p-value (0,002), and an effect size (0,2), thus viewing strong significance. All hypotheses show strong statistical significance (p < 0,01) yet varying effect sizes, which indicate meaningful effective contributions for any model development. Table 3 and figure 3 illustrate the variables using ANOVA.
|
Table 3. ANOVA Analysis of Predictors Influencing Doctor-Patient Communication |
|||||||
|
Predictor Variable |
Sum of Squares |
Degree of Freedom (df) |
Mean Square |
f-value |
p-values |
Effect size |
Result |
|
H1 |
12,35 |
1 |
12,35 |
9,21 |
0,003 |
0,18 |
significant |
|
H2 |
18,45 |
1 |
18,45 |
13,62 |
0,001 |
0,24 |
significant |
|
H3 |
1078 |
1 |
1078 |
7,89 |
0,005 |
0,15 |
significant |
|
H4 |
9,12 |
1 |
9,12 |
6,95 |
0,009 |
0,13 |
significant |
|
H5 |
14,22 |
1 |
14,22 |
10,42 |
0,002 |
0,20 |
significant |

Figure 3. Visualization of F-Values across Predictor Variables
Regression Analysis
The doctor-patient relationship plays a pivotal role in healthcare outcomes, with trust and communication serving as foundational elements. The results indicate that all the predictor variables (H1 to H5) significantly affect the dependent variable, as their p-values are all less than 0,01. The strongest effect and explanatory power is that of H2 with a β-coefficient of 0,68 and an R² of 0,46, followed by H4 with a β of 0,64 and an R² of 0,41, and then H1 with a β of 0,62 and an R² of 0,38, both with high predictive correlations. H3 and H5 have comparatively weaker but significant effects, with β-coefficients of 0,57 and 0,55, and R² values of 0,33 and 0,30, respectively. The t-values ranging from 6,35 to 8,92 confirm the strength of the relationships, whereby H1 to H5 are significant in explaining variation in the dependent variable. Table 4 and figure 4 represent the variable using Regression Analysis.
|
Table 4. Regression Analysis of Predictors Influencing Doctor-Patient Communication |
||||
|
Predictor Variable |
β- Coefficient (β) |
t-value |
p-value |
R2 |
|
H1 |
0,62 |
7,85 |
<0,01 |
0,38 |
|
H2 |
0,68 |
8,92 |
<0,01 |
0,46 |
|
H3 |
0,57 |
6,74 |
<0,01 |
0,33 |
|
H4 |
0,64 |
8,11 |
<0,01 |
0,41 |
|
H5 |
0,55 |
6,35 |
<0,01 |
0,30 |
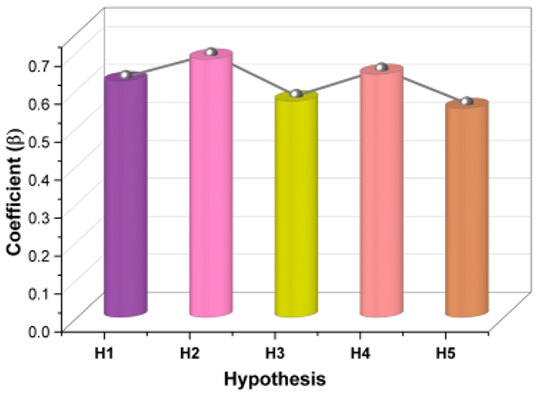
Figure 4. Regression Coefficients (β) across Predictor Variables
SEM
The findings show that all the hypothesized relationships were confirmed, with positive significant effects on patient adherence. The doctor's communication style showed a strong impact on patient adherence (β = 0,68, p < 0,01), emphasizing the significance of good communication in promoting adherence. Likewise, patient trust perception had the greatest effect (β = 0,64, p < 0,01), indicating that increased levels of trust significantly promote adherence. Emotional support also contributed significantly (β = 0,58, p < 0,01), emphasizing the importance of an empathetic doctor-patient relationship. Second, the doctor's responsiveness also showed an important effect on adherence (β = 0,63, p < 0,01), reinforcing the importance of responsiveness and timeliness. Finally, patient health literacy was related positively to adherence (β = 0,61, p < 0,01), emphasizing the significance of patient education in adhering to medical advice. These results collectively underscore the complex factors that shape adherence, with perceived trust being the most powerful predictor. Table 5 and figure 5 represent the variables using SEM Analysis.
|
Table 5. Structural Path Estimates for Factors Influencing Patient Adherence |
||||
|
Variable |
Path |
Standardize Estimate |
p-value |
Result |
|
H1 |
Doctor’s Communication Style → Patient Adherence |
0,68 |
< 0,01 |
Supported |
|
H2 |
Patient Trust Perception → Patient Adherence |
0,64 |
< 0,01 |
Supported |
|
H3 |
Emotional Support → Patient Adherence |
0,58 |
< 0,01 |
Supported |
|
H4 |
Doctor’s Responsiveness → Patient Adherence |
0,63 |
< 0,01 |
Supported |
|
H5 |
Patient Health Literacy → Patient Adherence |
0,61 |
< 0,01 |
Supported |
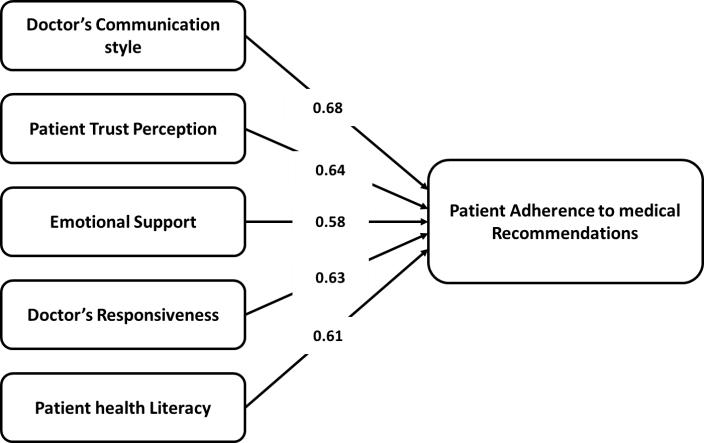
Figure 5. Path Diagram for Predictor Variables
DISCUSSION
Effective doctor-patient communication is a keystone of superior healthcare, playing a pivotal role in shaping patient outcomes, treatment observance, and complete satisfaction. The ANOVA results highlight the very important aspects of interpersonal trust, communication style, and emotional support in constructing adherence. The highest impact among H3 (Sum of Squares = 1078, f-value = 7,89, p = 0,005, effect size = 0,15), followed closely by H2 (Sum of Squares = 18,45, f-value = 13,62, p = 0,001, effect size = 0,24), indicate that emotional support and patient trust perception seems to significantly impact adherence. In regression analysis, H2 revealed a rather eloquent contribution regarding adherence among the various health factors in the setting (β = 0,68, t-value = 8,92, R² = 0,46, p < 0,01), followed closely by H4 (β = 0,64, t-value = 8,11, R² = 0,41, p < 0,01). A Structural Equation Modeling (SEM) disclosed that H1 (Doctor's Communication Style→Patient Adherence) has the highest standardized estimate (β = 0,68, Z = 3,23, p < 0,01) followed by H2 (Patient Trust Perception→Patient Adherence; β = 0,64, p < 0,01), further asserting that communication and trust both foster adherence. All these results support that better communication, trust, and responsiveness between doctors and patients will guarantee better adherence to physicians' recommendations, thus enhancing general health care in and improving the healthcare outcomes of patients.
CONCLUSIONS
Effective doctor-patient communication and trust are fundamental pillars of healthcare delivery, impacting patient satisfaction, compliance, and overall outcomes. The exploration emphasizes the significant role played by the communication style of the doctor in patient adherence, affirmed by the SEM analysis showing the highest standardized estimate (β = 0,68; p < 0,01). ANOVA H3 (Sum of Squares = 1078, f-value = 7,89, p = 0,005, effect size = 0,15), and regression H2 (β = 0,68, t-value = 8,92, R² = 0,46, p < 0,01), both exhibit statistically significant results. Hence, this result denotes a need for clear and effective communication to convince the patients to trust the medicine they are to take. By setting up better communication strategies in healthcare, better adherence could be accessed, leading to better patient outcomes. Future exploration could investigate technological advancements, such as artificial intelligence-guided patient engagement systems, that will improve communication between doctors and patients. Longitudinal effects of the trust-building strategies can be investigated further, along with insights from behavioural psychology models to fine-tune adherence-improvement strategies. These advances will enrich the development of a more individualized and effective communication framework in healthcare, thus improving patient satisfaction and treatment outcomes.
BIBLIOGRAPHIC REFERENCES
1. Gu L, Deng J, Xu H, Zhang S, Gao M, Qu Z, Zhang W, Tian D. The impact of contract service policy and doctor communication skills on rural patient-doctor trust relationship in the village clinics of three counties. BMC Health Services Research. 2019 Dec; 19:1-9. https://doi.org/10.1186/s12913-019-3875-x
2. Wei D, Xu A, Wu X. The mediating effect of trust on the relationship between doctor-patient communication and patients’ risk perception during treatment. PsyCh journal. 2020 Jun; 9(3):383-91. https://doi.org/10.1002/pchj.327
3. Du L, Wu R, Chen X, Xu J, Ji H, Zhou L. Role of treatment adherence, doctor–patient trust, and communication in predicting treatment effects among tuberculosis patients: difference between urban and rural areas. Patient preference and adherence. 2020 Nov 24:2327-36. https://doi.org/10.2147/PPA.S277650
4. Du L, Xu J, Chen X, Zhu X, Zhang Y, Wu R, Ji H, Zhou L. Rebuild doctor–patient trust in medical service delivery in China. Scientific reports. 2020 Dec 15; 10(1):21956. https://doi.org/10.1038/s41598-020-78921-y
5. Jiang S. The relationship between face-to-face and online patient-provider communication: examining the moderating roles of patient trust and patient satisfaction. Health communication. 2020 Feb 23.https://doi.org/10.1080/10410236.2018.1563030
6. Honavar SG. Patient–physician relationship–Communication is the key. Indian journal of ophthalmology. 2018 Nov 1; 66(11):1527 https://doi.org/10.4103/ijo.IJO_1760_18
7. Chakr VC. Building up trust in the doctor-patient relationship. Andes Pediatrica. 2021 Jun 22; 92(3):480-2.
8. Ray A, Pathak-Ray V. Withering trust: Redefining the doctor patient relationship. Indian journal of ophthalmology. 2018 Nov 1; 66(11):1529-30. https://doi.org/10.4103/ijo.IJO_821_18
9. Petrocchi S, Iannello P, Lecciso F, Levante A, Antonietti A, Schulz PJ. Interpersonal trust in doctor-patient relation: Evidence from dyadic analysis and association with quality of dyadic communication. Social science & medicine. 2019 Aug 1; 235:112391. https://doi.org/10.1016/j.socscimed.2019.112391
10. Hesse C, Rauscher EA. The relationships between doctor-patient affectionate communication and patient perceptions and outcomes. Health communication. 2019 Jul 3; 34(8):881-91. https://doi.org/10.1080/10410236.2018.1439269
11. Chang PC, Wu T, Du J. Psychological contract violation and patient’s antisocial behaviour: A moderated mediation model of patient trust and doctor-patient communication. International Journal of Conflict Management. 2020 Jun 18; 31(4):647-64. https://doi.org/10.1108/IJCMA-07-2019-0119
12. Akseer R, Connolly M, Cosby J, Frost G, Kanagarajah RR, Lim SH. Clinician–patient relationships after two decades of a paradigm of patient-centered care. International Journal of Healthcare Management. 2021 Jul 3; 14(3):888-97. https://doi.org/10.1080/20479700.2020.1713535
13. Mazzi MA, Rimondini M, van der Zee E, Boerma W, Zimmermann C, Bensing J. Which patient and doctor behaviours make a medical consultation more effective from a patient point of view. Results from a European multicentre study in 31 countries. Patient education and counseling. 2018 Oct 1; 101(10):1795-803. https://doi.org/10.1016/j.pec.2018.05.019
14. Hong H, Oh HJ. The effects of patient-centered communication: exploring the mediating role of trust in healthcare providers. Health communication. 2020 Mar 20; 35(4):502-11. https://doi.org/10.1080/10410236.2019.1570427
15. Parker L, Ryan R, Young S, Hill S. Medications and doctor-patient communication. Australian journal of general practice. 2021 Oct 1; 50(10):709 https://search.informit.org/doi/10.3316/informit.079370789996250
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Avir Sarkar, Manoranjan Dash.
Data curation: Avir Sarkar, Manoranjan Dash.
Formal analysis: Avir Sarkar, Manoranjan Dash.
Drafting - original draft: Avir Sarkar, Manoranjan Dash.
Writing - proofreading and editing: Avir Sarkar, Manoranjan Dash.