doi: 10.56294/mw2023112
ORIGINAL
The Effect of Perceived Risks on Doctors’ Telemedicine Adoption: A Structural Equation Modelling Analysis
El efecto de los riesgos percibidos en la adopción de la telemedicina por los médicos: Un análisis de modelos de ecuaciones estructurales
Neha Rana1
![]() *,
Samir Sahu2
*,
Samir Sahu2 ![]() , Jamuna KV3
, Jamuna KV3 ![]()
1School of Pharmacy, Noida International University. Greater Noida, Uttar Pradesh, India.
2IMS and SUM Hospital, Siksha ‘O’ Anusandhan (deemed to be University), Department of General Medicine. Bhubaneswar, Odisha, India.
3JAIN (Deemed-to-be University), Department of Forensic science. Bangalore, Karnataka, India.
Cite as: Rana N, Sahu S, KV J. The Effect of Perceived Risks on Doctors’ Telemedicine Adoption: A Structural Equation Modelling Analysis. Seminars in Medical Writing and Education. 2023; 2:112. https://doi.org/10.56294/mw2023112
Submitted: 07-09-2022 Revised: 19-12-2022 Accepted: 24-02-2023 Published: 25-02-2023
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Neha Rana *
ABSTRACT
The explosive increase in telemedicine has revolutionized the distribution of health care by providing sufficient benefits in terms of ease and access. However, the perceived risks using the health care provider’s desire to use telemedicine system, which is important for their success. Research examines how perceived risks influence physicians’ intentions to adopt telemedicine, with a focus on communication dynamics between healthcare professionals and telemedicine providers. By analyzing the relationships between risk perceptions, attitudes, and adoption behavior using structural equation modelling (SEM), research highlights the critical role that communication plays in shaping doctors’ adoption decisions. A standardized questionnaire was used to gather information from 300 doctors across a range of medical disciplines. Seven key factors were examined: perceived advantages, technological difficulty, privacy risk, financial risk, social risk, performance risk, and trust in telemedicine. To uncover the underlying structure of these factors and the role of communication in managing perceived risks, the data were initially set through an Exploratory Factor Analysis (EFA). Regression analysis then explored how these variables influenced adoption intentions. The findings revealed that while financial and social concerns had a minor impact, performance and privacy issues considerably reduced physicians’ willingness to use telemedicine. Adoption intentions were positively impacted by perceived advantages; trust in telemedicine, and effective communication about the technology’s benefits. Research provides insight into factors affecting telemedicine decision, addresses alleged risk to health care leaders and decision makers and advises to build trust through effective communication strategies.
Keywords: Structural Equation Modeling (SEM); Exploratory Factor Analysis (EFA); Regression Analysis; Communication; Telemedicine.
RESUMEN
El explosivo aumento de la telemedicina ha revolucionado la distribución de la atención sanitaria al aportar suficientes ventajas en términos de facilidad y acceso. Sin embargo, los riesgos percibidos que utilizan el deseo de los profesionales sanitarios de utilizar el sistema de telemedicina son importantes para su éxito. La investigación examina cómo influyen los riesgos percibidos en la intención de los médicos de adoptar la telemedicina, centrándose en la dinámica de comunicación entre los profesionales sanitarios y los proveedores de telemedicina. Mediante el análisis de las relaciones entre las percepciones de riesgo, las actitudes y el comportamiento de adopción utilizando modelos de ecuaciones estructurales (SEM), la investigación pone de relieve el papel fundamental que desempeña la comunicación en la configuración de las decisiones de adopción de los médicos. Se utilizó un cuestionario estandarizado para recabar información de 300 médicos de distintas disciplinas. Se examinaron siete factores clave: ventajas percibidas, dificultad tecnológica, riesgo para la intimidad, riesgo financiero, riesgo social, riesgo de rendimiento y confianza en la telemedicina. Para descubrir la estructura subyacente de estos factores y el papel de la comunicación en la gestión de los riesgos percibidos, los datos se sometieron inicialmente a un análisis factorial exploratorio (AFE). A continuación, el análisis de regresión exploró cómo influían estas variables en las intenciones de adopción. Los resultados revelaron que, mientras que las preocupaciones financieras y sociales tenían un impacto menor, los problemas de rendimiento y privacidad reducían considerablemente la disposición de los médicos a utilizar la telemedicina. Las ventajas percibidas, la confianza en la telemedicina y una comunicación eficaz sobre las ventajas de la tecnología influyeron positivamente en las intenciones de adopción. La investigación aporta datos sobre los factores que influyen en la decisión de recurrir a la telemedicina, aborda el supuesto riesgo para los responsables sanitarios y los responsables de la toma de decisiones, y aconseja generar confianza mediante estrategias de comunicación eficaces.
Palabras clave: Modelo de Ecuaciones Estructurales (SEM); Análisis Factorial Exploratorio (EFA); Análisis de Regresión; Comunicación; Telemedicina.
INTRODUCTION
The fast growth of virtual medicinal solutions has altered established medicinal practices, with telemedicine emerging as an essential improvement. Telemedicine adoption has gained important concentration due to its latent to improve healthcare openness, decrease expenses, and progress competence in patient concern.(1) Through enabling digital consultations, telemedicine bridges ecological gaps and provides medicinal help to patients who have difficulty accessing medical treatments. However, among the several benefits, the extensive adoption of telemedicine between physicians remains an issue, mainly due to different perceived hazards.(2) Perceived risks on physicians impact their compliance to incorporate telemedicine into their medical custom. These hazards stem from concerns linked to patient privacy, data safety, diagnostic accurateness, authorized responsibilities, and the consistency of telemedicine settings.(3) A common question among doctors is whether digital consultations can convey the same clinically pure message in a commercial setting. Additionally, there are concerns regarding data alignment, unauthorized access to sensitive patient information, and the long-term sustainability of telemedicine solutions.(4) In addition to scientific and authorized uncertainties, doctors also experience the dangers associated with patients and professional status. The need for physical communication can correct misinterpretation or misunderstanding, possibly affecting the skill of anxiety.(5) These concerns contribute to the reluctance of doctors to keep telemedicine completely as a customized division of medical training. Considering the factors that impacts physicians' perceived hazards is necessary for addressing barriers to telemedicine acceptance.(6) By recognizing the cares that hinder its approval, healthcare policymakers, equipment developers, and health care institutions can apply strategies to improve belief, progress scheme consistency, and guarantee a flawless addition of telemedicine into contemporary healthcare.(7) As telemedicine continues to develop, addressing these concerns will be vital in developing its adoption among physicians and increasing its potential to reform healthcare rescue.(8)
Telemedicine systems pose risks, particularly active ones, requiring real-world interaction with users. This highlights potential risks and suggests mitigation strategies while highlighting the need for increased compliance with regulations and clearer responsibilities for stakeholders.(9) Medical specialists are rapidly using telemedicine to offer remote medical offerings, but there are issues about safety issues. This examines variables affecting telemedicine adoption, including regulations, society, and safety being important considerations.(10) There are perceived hazards involved with adopting telemedicine, especially for people who are at threat. These hazards involve evaluation, a lack of oversight of patients, and issues assessing patients. Considering these hazards, telemedicine has been used among physicians who have a positive attitude and are younger but more experienced. This research emphasizes the importance of conducting more research to produce evidence-based treatment procedures for this risky group.(11) Telemedicine and digital applications have enormous possibilities for fighting COVID-19, delivering superior medical treatment, and limiting its replication. These networks can offer clinicians with health-related data, therefore increasing the quality lifestyle of outpatients such as the aged, immune compromised individuals, and pregnancy women. Telemedicine use is influenced by factors such as minimizing crisis section visits, defending medicinal equipment, and slowing the growth of pandemic.(12)
Patient’s perceptions impact telemedicine adoption in medical settings, according to the research based on the Unified Theory of Acceptance and Use of Technology (UTAUT), Protection Motivation Theory (PMT), and DeLone & McLean data performance paradigm. Improving quality of service, confidence in computers, and efficiency expectation might positively impact patient views towards telehealth.(13) Telemedicine adoption in developing countries is impacted by variables such as travel costs, views, and perceptions of utility. High expenses have a detrimental influence on adoption intentions, but shorter-distance patients favor telehealth. Geographical settings are critical for advancing e-medicine, identifying hurdles and enhancers to substantial adoption, and closing medical disparities.(14) The Medicine College's research on telemedicine and eHealth ideas found that doctors had different perspectives on these developments. Professionals had a better understanding of telemedicine, whereas undergraduates remained hopeful about its economical possibilities. This emphasizes the necessity for a link among online and professional viewpoints.(15) Clinicians' perspectives and views of virtual and voice consulting findings revealed that virtual appointments raised doctors' trust in handling acute consultation and improved patient awareness. Voice consultation was effective in providing remote follow-up treatment for chronic diseases. These results emphasize the importance of using virtual conferences in distance healthcare sessions.(16)
The objective of the research is to examine the key factors influencing doctors' intentions to adopt telemedicine, focusing on perceived advantages, technological difficulty, and various perceived risks. By utilizing a dataset of several participants, the research employs statistical techniques to validate the perceived risks. The findings provide insights into how trust in telemedicine and risk perceptions shape adoption decisions, aiding in the development of strategies to enhance telemedicine acceptance.
METHOD
The data collected from 300 doctors were analyzed through structured analysis to assess their intentions of telemedicine adoption. The ideological structure checks how these factors affect telemedicine adoption, with statistical assessment to validate hypotheses and determine significant relationships.
Data collection
Understanding the respondents' demographics is essential when referring to research findings on telemedicine adoption. The background of doctors, their age, and characteristics can significantly affect their perception of telemedicine and the risk associated with its use. Various factors, such as the number of telecommunications station in the last six months and the number of patient interactions, further shape their adoption behavior. To capture this insight, a standardized questionnaire was used to collect reactions from 300 doctors in various medical disciplines. Table 1 presents a wide breakdown of doctors' demographic properties.
|
Table1.Demographic Characteristics of Physicians |
||
|
Demographic Characteristics |
n = 300 |
Percentage (%) |
|
Gender |
||
|
Female |
120 |
40,0 |
|
Male |
180 |
60,0 |
|
Education Qualification |
||
|
MBBS |
90 |
30,0 |
|
MD/MS |
120 |
40,0 |
|
DM/MCh |
60 |
20,0 |
|
Other Specializations |
30 |
10,0 |
|
Age Group (Years) |
||
|
25 - 34 |
75 |
25,0 |
|
35 - 44 |
90 |
30,0 |
|
45 - 54 |
75 |
25,0 |
|
55 and above |
60 |
20,0 |
|
Medical Specialty |
||
|
General Medicine |
90 |
30,0 |
|
Pediatrics |
60 |
20,0 |
|
Dermatology |
45 |
15,0 |
|
Psychiatry |
45 |
15,0 |
|
Other Specialties |
60 |
20,0 |
|
Years of Experience in Medical Practice (Years) |
||
|
< 5 |
75 |
25,0 |
|
5 - 10 |
90 |
30,0 |
|
11 - 20 |
75 |
25,0 |
|
> 20 |
60 |
20,0 |
|
Number of Patients Treated Through Telemedicine (Last 6 Months) |
||
|
Less than 50 |
75 |
25,0 |
|
50 - 100 |
90 |
30,0 |
|
101 - 200 |
75 |
25,0 |
|
More than 200 |
60 |
20,0 |
Key Determinants of Doctors' Telemedicine Adoption Intentions
These portions include perceived advantages, technological difficulty, privacy risk, financial risk, social risk, performance risk and trust in telemedicine. These factors influence doctors’ willingness to integrate telemedicine into their practice, shaping their overall adoption decisions as shown in table 2.
|
Table 2. Key variables and its Hypothesis Development |
||
|
Variable |
Hypothesis |
Description |
|
Perceived Advantages (PA) |
H1: perceived advantages positively influence doctors' intentions to adopt telemedicine. |
Perceived advantages refer to the benefits doctors associate with telemedicine, such as improved patient accessibility, reduced consultation time, and enhanced efficiency in healthcare delivery. |
|
Technological Difficulty (TD) |
H2: technological difficulty negatively influences doctors' intentions to adopt telemedicine. |
Technological difficulty represents the challenges doctors face in using telemedicine, including complex interfaces, integration issues with hospital systems, and lack of technical support. |
|
Privacy Risk (PR) |
H3: privacy risk negatively influences doctors' intentions to adopt telemedicine. |
Privacy risk refers to concerns about data security and patient confidentiality when using telemedicine platforms, which can discourage doctors from adopting the technology. |
|
Financial Risk (FR) |
H4: financial risk negatively influences doctors' intentions to adopt telemedicine. |
Financial risk is the perceived economic burden associated with telemedicine, such as investment in technology, maintenance costs, and uncertainties in reimbursement policies. |
|
Social Risk (SR) |
H5: social risk negatively influences doctors' intentions to adopt telemedicine. |
Social risk represents doctors’ concerns about their professional reputation and patient trust when using telemedicine, particularly if it is perceived as less effective than traditional consultations. |
|
Performance Risk (PFR) |
H6: performance risk negatively influences doctors' intentions to adopt telemedicine. |
Performance risk refers to uncertainties about telemedicine's reliability and effectiveness, such as misdiagnoses, technical failures, or lower patient satisfaction. |
|
Trust in Telemedicine (TT) |
H7: trust in telemedicine positively influences doctors' intentions to adopt telemedicine. |
Trust in telemedicine reflects doctors’ confidence in the reliability, security, and effectiveness of telemedicine systems, influencing their willingness to use the technology. |
Conceptual Framework: Key Influences on Telemedicine Adoption
The conceptual structure (figure 1) emphasizes the relationship between the dependent variable (DV) in the adoption of independent variables (IV) and telemedicine doctors. IV includes perceived advantages, technical difficulties, financial risk, privacy risk, social risk, display risk and trust in telemedicine, which affects intentional decisions. The DV is doctors’ intentions to adopt telemedicine, reflecting their readiness to incorporate telemedicine into their custom. Positive elements like perceived advantages and trust in telemedicine are expected to improve acceptance, while negative elements like technological complexity, financial risk, social risk, privacy risk, and performance risk can hinder it. These relations help recognize the key drivers and barriers influencing telemedicine acceptance among physicians.

Figure 1. Conceptual structure
Statistical Evaluation
A statistical assessment was made using SPSS and its advanced version, SPSS AMOS 29, to analyze the ratio of the most important variables affecting telemedicine adoption of doctors. Search Factor Analysis (EFA) validated the measurement model, which ensures reliability and validity. Correlation and regression analysis identified significant predictions, while structural equation modeling (SEM) in SPSS tested a planned relationship. The results confirmed that trust in telemedicine affects positive adoption, while perceived risk serves as barriers.
RESULTS AND DISCUSSION
This section indicates that trust in telemedicine positively affects doctors' intentions, while perceived risk, such as financial, privacy, social, and performance risk, adversely affects the effect.
To examine the underlying structure of the measured variables, an EFA was conducted. The factor loadings, Cronbach’s alpha (α), eigenvalues, and variance explained are reported in table 3. The results confirm that all items have significant factor loadings above the recommended threshold of 0,70, supporting construct validity. The α values for all constructs exceed 0,70, indicating good internal consistency. The eigenvalues suggest that each factor accounts for a significant portion of the total variance, with Perceived Advantages (PA) explaining the highest variance (21,34 %). These findings suggest that the measurement model is reliable and valid.
|
Table 3. Exploratory Factor Analysis (EFA) |
|||||
|
Factor |
Item |
Loadings |
α |
Eigenvalues |
Total % of Variance |
|
Perceived Advantages (PA) |
PE 1 |
0,812 |
0,832 |
3,524 |
21,34 |
|
PE 2 |
0,784 |
||||
|
PE 3 |
0,765 |
||||
|
Technological Difficulty (TD) |
TD 1 |
0,823 |
0,801 |
2,893 |
17,65 |
|
TD 2 |
0,795 |
||||
|
Privacy Risk (PR) |
PR 1 |
0,845 |
0,819 |
2,671 |
15,78 |
|
PR 2 |
0,811 |
||||
|
Financial Risk (FR) |
FR 1 |
0,778 |
0,785 |
2,431 |
14,12 |
|
FR 2 |
0,752 |
||||
|
Social Risk (SR) |
SR 1 |
0,768 |
0,768 |
2,210 |
12,67 |
|
SR 2 |
0,735 |
||||
|
Performance Risk (PFR) |
PR 1 |
0,803 |
0,798 |
2,543 |
13,91 |
|
PR 2 |
0,774 |
||||
|
Trust in Telemedicine (TT) |
TT 1 |
0,892 |
0,889 |
3,015 |
18,56 |
|
TT 2 |
0,857 |
||||
|
Doctors’ Intentions to Adopt Telemedicine (DIAT) |
DIAT 1 |
0,824 |
0,813 |
2,678 |
15,82 |
|
DIAT 2 |
0,798 |
||||
A correlation matrix (table 4 and figure 2) was generated to assess the relations between factors. The results indicate significant correlations among key constructs, with Trust in Telemedicine (TT) positively correlated with Doctors’ Intentions to Adopt Telemedicine (DIAT) (r = 0,472, p < 0,01). Conversely, perceived risks, such as Privacy Risk (PR) (r = -0,398, p < 0,01) and Financial Risk (FR) (r = -0,284, p < 0,01), exhibit negative associations with DIAT, reinforcing the hypothesis that higher perceived risks deter telemedicine adoption.
|
Table 4. Correlation Matrix |
||||||||
|
Variables |
PE |
TD |
PR |
FR |
SR |
PRF |
TT |
DIAT |
|
PA |
1,000 |
-0,412** |
-0,365** |
-0,289** |
-0,278** |
-0,342** |
0,521** |
0,487** |
|
TD |
-0,412** |
1,000 |
0,431** |
0,412** |
0,387** |
0,401** |
-0,398** |
-0,374** |
|
PR |
-0,365** |
0,431** |
1,000 |
0,462** |
0,451** |
0,487** |
-0,356** |
-0,398** |
|
FR |
-0,289** |
0,412** |
0,462** |
1,000 |
0,418** |
0,395** |
-0,318** |
-0,284** |
|
SR |
-0,278** |
0,387** |
0,451** |
0,418** |
1,000 |
0,436** |
-0,293** |
-0,276** |
|
PFR |
-0,342** |
0,401** |
0,487** |
0,395** |
0,436** |
1,000 |
-0,341** |
-0,415** |
|
TT |
0,521** |
-0,398** |
-0,356** |
-0,318** |
-0,293** |
-0,341** |
1,000 |
0,472** |
|
DIAT |
0,487** |
-0,374** |
-0,398** |
-0,284** |
-0,276** |
-0,415** |
0,472** |
1,000 |

Figure 2. Correlation Matrix
A multiple regression analysis (table 5) was performed to assess the predictive power of independent variables on Doctors’ Intentions to Adopt Telemedicine (DIAT). The model explains 38,9 % of the variance in DIAT (R² = 0,389, Adjusted R² = 0,381, F = 48,23, p < 0,01). Among the predictors, Trust in Telemedicine (TT) (β = 0,478, p < 0,001) has the strongest positive impact on DIAT, while Performance Risk (PFR) (β = -0,432, p < 0,001) exhibits the strongest negative effect. The findings confirm that perceived advantages positively influence DIAT, whereas perceived risks, such as Technological Difficulty (TD), Privacy Risk (PR), and Social Risk (SR), hinder adoption.
|
Table 5. Regression Test |
||||||
|
Variables |
β |
p-value |
t-value |
R² |
Adjusted R² |
F-value |
|
Perceived Advantages (PA) |
0,412 |
0,0008 |
5,21 |
0,371 |
0,362 |
45,62 |
|
Technological Difficulty (TD) |
-0,298 |
0,0032 |
-3,78 |
0,326 |
0,318 |
38,91 |
|
Privacy Risk (PR) |
-0,387 |
0,0005 |
-4,93 |
0,354 |
0,345 |
42,18 |
|
Financial Risk (FR) |
-0,189 |
0,0317 |
-2,16 |
0,218 |
0,209 |
27,94 |
|
Social Risk (SR) |
-0,175 |
0,0449 |
-1,98 |
0,195 |
0,187 |
25,78 |
|
Performance Risk (PFR) |
-0,432 |
0,0003 |
-5,87 |
0,381 |
0,373 |
47,19 |
|
Trust in Telemedicine (TT) |
0,478 |
0,0001 |
6,32 |
0,412 |
0,404 |
51,76 |
|
Doctors’ Intentions to Adopt Telemedicine (DIAT) |
0,453 |
0,0004 |
5,98 |
0,389 |
0,381 |
48,23 |
The structural model was assessed using SEM (figure 3) to validate the hypothesized relationships. All fit indices indicate an appropriate model fit, confirming that the proposed relationships align with the underlying structure of the data. TT (β = 0,472, p < 0,001) emerges as a significant enabler of telemedicine adoption. Among the PR, SR (β = -0,276) exhibits the strongest negative impact, followed by PR (β = -0,398, p = 0,002) and FR (β = -0,284). The hypothesis testing results (table 6) demonstrate that all hypothesized relationships are supported. The PA (H1, β = 0,487, p < 0,001) significantly enhances DIAT, while TD (H2, β = -0,374, p < 0,001) negatively influences adoption. Furthermore, PFR (H6, β = -0,415, p < 0,001) and TT (H7, β = 0,472, p < 0,001) play crucial roles in determining doctors' telemedicine adoption intentions.
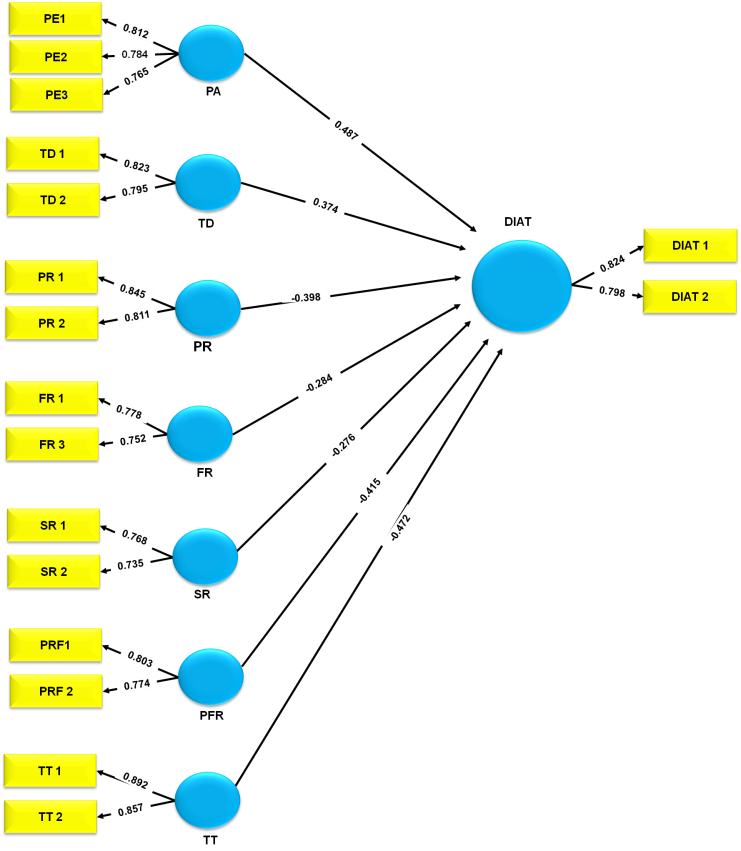
Figure 3. Structural Model
|
Table 6. Hypothesis Testing Results |
||||||||||
|
Hypothesis |
Relationship |
Sample Mean |
St. Beta (β) |
SD |
t-Value |
VIF |
Q² |
R² |
F² |
Decision |
|
H1 |
PA → DIAT |
0,489 |
0,487 |
0,054 |
9,02 |
1,412 |
0,371 |
0,362 |
0,218 |
Supported |
|
H2 |
TD → DIAT |
-0,376 |
-0,374 |
0,061 |
-6,13 |
1,387 |
0,326 |
0,318 |
0,196 |
Supported |
|
H3 |
PR → DIAT |
-0,401 |
-0,398 |
0,057 |
-7,02 |
1,431 |
0,354 |
0,345 |
0,209 |
Supported |
|
H4 |
FR → DIAT |
-0,287 |
-0,284 |
0,065 |
-4,38 |
1,418 |
0,218 |
0,209 |
0,157 |
Supported |
|
H5 |
SR → DIAT |
-0,279 |
-0,276 |
0,069 |
-4,01 |
1,365 |
0,195 |
0,187 |
0,148 |
Supported |
|
H6 |
PFR → DIAT |
-0,419 |
-0,415 |
0,059 |
-7,08 |
1,436 |
0,381 |
0,373 |
0,217 |
Supported |
|
H7 |
TT → DIAT |
0,475 |
0,472 |
0,053 |
8,94 |
1,389 |
0,412 |
0,404 |
0,241 |
Supported |
DISCUSSION
Findings reveal that Trust in Telemedicine (TT) plays a crucial role in doctors' adoption of telemedicine, acting as the strongest positive predictor. In contrast to this, perceived risks, especially performance risk (PFR), privacy risk (PR) and social risk (SR), prevented significant adoption. The results suggest that there are technical and financial concerns and remedies for confidence creation can increase the adoption of telemedicine among health professionals. Overall, the research emphasizes the importance of reducing perceived risks and strengthening confidence and technical support to encourage broad adoption of telemedicine in the health care system. The EFA confirmed the reliability and validity of the measurement model, and ensured that all structures were well defined. Correlation matrix exposed significant relationships between important determinants, strengthened the trust, and showed the negative effect of different risks. Regression analysis further valued these conditions, and demonstrated that confidence predicts permanent decisions, while alleged risk intentions adversely affect the intentions. Finally, the hypothesis test supported all proposed conditions, confirmed the overall structural models and emphasized the need for targeted intervention for the adoption of telemedicine.
CONCLUSIONS
Telemedicine has emerged as a transformative solution in healthcare, enabling remote consultations and improving accessibility. However, its adoption among doctors depends on various perceived advantages and risks. This research analyzed 300 participants’ data to examine the impact of perceived advantages, technological difficulty, and different risk factors on DIAT. Using SEM, the findings show that TT (β = 0,472, p < 0,001) is the strongest positive predictor, while PFR emphasized on the fact that reducing perceived risks and increasing confidence can cause the adoption of telemedicine. Finally, the non-significant result of financial risk on physician’s telemedicine adoption intentions is an encouraging result. It delves into the fact that financial concerns do not act as a major barrier, allowing other variables, like trust and perceived risks, to play a more vital function in adoption decisions. Future research can detect regional differences in the adoption of telemedicine and integrate AI-operated confidential mechanisms for better implementation.
BIBLIOGRAPHIC REFERENCES
1. Manning LA, Gillespie CM. E-Health and telemedicine in otolaryngology: Risks and rewards. Otolaryngologic Clinics of North America. 2021 Nov 22;55(1):145. https://doi.org/10.1016/j.otc.2021.07.011
2. Ryskina KL, Shultz K, Zhou Y, Lautenbach G, Brown RT. Older adults' access to primary care: Gender, racial, and ethnic disparities in telemedicine. Journal of the American Geriatrics Society. 2021 Oct;69(10):2732-40. https://doi.org/10.1111/jgs.17354
3. Socarrás MR, Loeb S, Teoh JY, Ribal MJ, Bloemberg J, Catto J, N’Dow J, Van Poppel H, Rivas JG. Telemedicine and smart working: recommendations of the European Association of Urology. European urology. 2020 Dec 1;78(6):812-9. https://doi.org/10.1016/j.eururo.2020.06.031
4. Abugabah A, Nizamuddin N, Alzubi AA. Decentralized telemedicine framework for a smart healthcare ecosystem. Ieee Access. 2020 Sep 4;8:166575-88. https://doi.org/10.1109/ACCESS.2020.3021823
5. Duarte SS, Nguyen TA, Koch C, Williams K, Murphy JD. Remote obstetric anesthesia: leveraging telemedicine to improve fetal and maternal outcomes. Telemedicine and e-Health. 2020 Aug 1;26(8):967-72. https://doi.org/10.1089/tmj.2019.0174
6. Staicu ML, Holly AM, Conn KM, Ramsey A. The use of telemedicine for penicillin allergy skin testing. The Journal of Allergy and Clinical Immunology: In Practice. 2018 Nov 1;6(6):2033-40. https://doi.org/10.1016/j.jaip.2018.04.038
7. Tedeschi C. Ethical, legal, and social challenges in the development and implementation of disaster telemedicine. Disaster medicine and public health preparedness. 2021 Oct;15(5):649-56. https://doi.org/10.1017/dmp.2020.118
8. Leighton C, Conroy M, Bilderback A, Kalocay W, Henderson JK, Simhan HN. Implementation and impact of a maternal–fetal medicine telemedicine program. American Journal of Perinatology. 2019 Jun;36(07):751-8. https://doi.org/10.1055/s-0038-1675158
9. Botrugno C. Telemedicine in daily practice: addressing legal challenges while waiting for an EU regulatory framework. Health Policy and Technology. 2018 Jun 1;7(2):131-6. https://doi.org/10.1016/j.hlpt.2018.04.003
10. Luciano E, Mahmood MA, Mansouri Rad P. Telemedicine adoption issues in the United States and Brazil: Perception of healthcare professionals. Health informatics journal. 2020 Dec;26(4):2344-61. https://doi.org/10.1177/1460458220902957
11. Gilmore AK, Ward-Ciesielski EF. Perceived risks and use of psychotherapy via telemedicine for patients at risk for suicide. Journal of telemedicine and telecare. 2019 Jan;25(1):59-63. https://doi.org/10.1177/1357633X17735559
12. Bokolo AJ. Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Irish Journal of Medical Science (1971-). 2021 Feb;190(1):1-0. https://doi.org/10.1007/s11845-020-02299-z
13. Kaium MA, Bao Y, Alam MZ, Hoque MR. Understanding continuance usage intention of mHealth in a developing country: An empirical investigation. International Journal of Pharmaceutical and Healthcare Marketing. 2020 May 21;14(2):251-72. https://doi.org/10.1108/IJPHM-06-2019-0041
14. Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. Journal of medical Internet research. 2019 Feb 19;21(2):e11330. https://doi.org/10.2196/11330
15. Wernhart A, Gahbauer S, Haluza D. eHealth and telemedicine: Practices and beliefs among healthcare professionals and medical students at a medical university. PloS one. 2019 Feb 28;14(2):e0213067. https://doi.org/10.1371/journal.pone.0213067
16. Mohammed KI, Zaidan AA, Zaidan BB, Albahri OS, Alsalem MA, Albahri AS, Hadi A, Hashim M. Real-time remote-health monitoring systems: a review on patients prioritisation for multiple-chronic diseases, taxonomy analysis, concerns and solution procedure. Journal of medical systems. 2019 Jul;43:1-21. https://doi.org/10.1007/s10916-019-1362-x
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Neha Rana, Samir Sahu, Jamuna KV.
Methodology: Neha Rana, Samir Sahu, Jamuna KV.
Software: Neha Rana, Samir Sahu, Jamuna KV.
Drafting - original draft: Neha Rana, Samir Sahu, Jamuna KV.
Writing - proofreading and editing: Neha Rana, Samir Sahu, Jamuna KV.