doi: 10.56294/mw2023113
ORIGINAL
Evaluating the Impact of Digital Communication on Healthcare Service Efficiency and Patient Treatment Outcomes
Evaluación del impacto de la comunicación digital en la eficiencia de los servicios sanitarios y los resultados del tratamiento de los pacientes
RenukaJyothi S1
![]() *,
Nidhi Srivastava2
*,
Nidhi Srivastava2 ![]() , Srikant Kumar Dhar3
, Srikant Kumar Dhar3
![]()
1JAIN (Deemed-to-be University), Department of Biotechnology and Genetics. Bangalore, Karnataka, India.
2School of Pharmacy, Noida International University. Greater Noida, Uttar Pradesh, India.
3IMS and SUM Hospital, Siksha ‘O’ Anusandhan (deemed to be University), Department of General Medicine. Bhubaneswar, Odisha, India.
Cite as: S RJ, Srivastava N, Dhar SK. Evaluating the Impact of Digital Communication on Healthcare Service Efficiency and Patient Treatment Outcomes. Seminars in Medical Writing and Education. 2023; 2:113. https://doi.org/10.56294/mw2023113
Submitted: 07-09-2022 Revised: 19-12-2022 Accepted: 24-02-2023 Published: 25-02-2023
Editor:
PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: RenukaJyothi S *
ABSTRACT
Processes for patient treatment and service provision have changed as a product of the practice of digital communication expertise in the medical sector. The research assesses how digital communication affects patient treatment results and the effectiveness of healthcare services. A sample of 60 medical professionals and 200 patients was chosen from telemedicine platforms, clinics, and hospitals. In addition to healthcare service indicators like wait times and consultation lengths, data were gathered through surveys and questionnaires that evaluated patient satisfaction, treatment adherence, and healthcare professional efficiency. Key trends in service efficiency and satisfaction were compiled using descriptive statistics, and healthcare service measures were compared before and after the use of digital communication technologies using a paired sample t-test. The findings show that digital communication skills have a major effect on increased coordination among healthcare practitioners, shorter wait times, and quicker reaction times. Patients expressed better participation and satisfaction with their treatment schedules, especially after having access to up-to-date health information. However, problems like digital accessibility and data security exist. The findings suggest that while digital communication enhances healthcare efficiency and treatment outcomes, these obstacles must be tackled to harness the advantages. It emphasizes the vital role of continuous innovation and adaptation in healthcare to provide effective, efficient, and fair healthcare delivery in the digital era.
Keywords: Digital Communication; Healthcare Service; Patient Satisfaction; Treatment Adherence; Healthcare Professional Efficiency.
RESUMEN
Los procesos de tratamiento de pacientes y prestación de servicios han cambiado como consecuencia de la práctica de la experiencia en comunicación digital en el sector médico. La investigación evalúa cómo afecta la comunicación digital a los resultados del tratamiento de los pacientes y a la eficacia de los servicios sanitarios. Se eligió una muestra de 60 profesionales médicos y 200 pacientes de plataformas de telemedicina, clínicas y hospitales. Además de indicadores de servicios sanitarios como tiempos de espera y duración de las consultas, se recopilaron datos mediante encuestas y cuestionarios que evaluaban la satisfacción de los pacientes, la adherencia al tratamiento y la eficiencia de los profesionales sanitarios. Las principales tendencias en eficiencia y satisfacción de los servicios se recopilaron mediante estadísticas descriptivas, y las medidas de los servicios sanitarios se compararon antes y después del uso de tecnologías de comunicación digital mediante una prueba t de muestras pareadas. Los resultados muestran que las habilidades de comunicación digital tienen un efecto importante en una mayor coordinación entre los profesionales sanitarios, tiempos de espera más cortos y tiempos de reacción más rápidos. Los pacientes se mostraron más participativos y satisfechos con sus programas de tratamiento, sobre todo después de tener acceso a información sanitaria actualizada. Sin embargo, existen problemas como la accesibilidad digital y la seguridad de los datos. Las conclusiones sugieren que, si bien la comunicación digital mejora la eficiencia de la asistencia sanitaria y los resultados de los tratamientos, es preciso superar estos obstáculos para aprovechar sus ventajas. Se subraya el papel vital de la innovación y la adaptación continuas en la atención sanitaria para proporcionar una asistencia sanitaria eficaz, eficiente y equitativa en la era digital.
Palabras clave: Comunicación Digital; Servicio Sanitario; Satisfacción del Paciente; Cumplimiento Terapéutico; Eficiencia del Profesional Sanitario.
INTRODUCTION
The digitization of healthcare is the result of developments in medical technology and digital communications. clinicians’ decision-making in the setting of electronic health records (EHRs) is heavily influenced by the vast volumes of potentially useful data that are produced by increased access and adoption of such technology by patients and clinicians. In the medical field, self-reported data is often employed. Real-world medical information is provided by patient-level data, which also offers chances for better professional judgment, patient empowerment, better health outcomes, and cost savings.(1)
Technology is improving, life expectancy is increasing, and the dissemination of medications is accelerating an unprecedented rate. The benefits are indisputable, despite issues and inquiries. The development of healthcare begins with the development of a mindset: well-being should be viewed as both a communal and financial asset, a catalyst for progress that creates collective welfare among those who provide technical apparatus (businesses), utilize it for routine care and emergencies (clinics and the health providers), and benefit from it (patients). The cost, both human and financial, must be the beginning point. Healthcare cannot be sustained if business models improve service quality do not raise costs beyond affordable limits. Given the increasing need for help in terms of both patient numbers and technology advancements (new services, innovative treatment approaches, and monitoring), the task is difficult.(2)
Digital Transformation (DT) of health facilities is an essential process that has already had a significant impact on medical services and healthcare organizations today. It is expected to play even more crucial role in the future of health care and medical care. The fact that DT of health services is a complicated and multidimensional subject is also instantly acknowledged. The application of digital tools in the creation and distribution of goods is declared as digitalization. These digital technologies provide advanced methods for the production, delivery, and organization of healthcare services.(3) This phenomenon is transforming the corporate sector as a whole and has gained a lot of attention in several areas of business administration, like promotion, policy, and data systems. Healthcare includes all services offered by health professionals to keep an individual’s physical and mental welfare, is one of the main industries where DT has been practiced for a long time.(4)
Low-cost sensing devices that can be used for a variety of purposes have become more widely available due to technological advancements and mass market need (for instance, wireless sensors that are lightweight, non-invasive, miniature, low-power, and able to record a lot of data while monitoring physiological processes or the environment).(5) Globally, an aging population with several chronic illnesses poses numerous issues. Healthcare resources will be burdened by the health, existence, and individual well-being requirements of aging populations. This analysis examines how digital communication influences patient treatment outcomes and healthcare services efficiently. By analyzing healthcare service indicators and patient satisfaction, it highlights both the benefits and challenges of participating digital skills into healthcare organizations.(6) The part of digital technology in healthcare management is depicted in figure 1. The research explores how digital transformation is affecting healthcare, with an emphasis on enhancing patient outcomes, cost-effectiveness, and service delivery. Even with the development of technology, problems, like integration and cost still exist. The analysis investigates in which digital solutions, such as inexpensive sensors and remote care, improve healthcare sustainability. To maximize technology adoption for improved accessibility, patient monitoring, and economical virtual care models, implementation blockages must be addressed.

Figure 1. Role of Digital Technology in Healthcare Management
Healthcare was being transformed into healthcare 4.0, enabled by industrial revolution technologies, such as the Internet of Things (IoT), Cloud and Fog Computing, and Big Data, which were changing conventional services and goods.(7) The service of the technologies in the healthcare sector was examined through a selective literature analysis. Along with the strengths, cross-disciplinary challenges, and application potential, the key enabling technologies were determined. Security, privacy, complexity, and regulation inhibit the integration of healthcare 4.0. The research protracted the Technology Acceptance Model (TAM) to examine the influence of communication traits and reasoning perceptions on patients’ acceptance of healthcare expertise.(8) Adoption was influenced by perceived utility, ease of use, trust, and concerns for privacy, as revealed through statistical equation modeling and survey results among 416 patients. Generalizability was limited by the focus on primary health facilities and the exclusion of socioeconomic and cultural factors.
Testing, tracing, health management, and social distancing measures were all supported by evidence-based public policy decisions based on pseudonymized patient data.(9) Involvement of clinical data, medical history, genomic data, and demographics to enhance healthcare management and disease control. Disadvantages, such as privacy issues, data security threats, and standardization issues of data are present. Successful implementation relies on guaranteeing ethical data integration and utilization. The objective of healthcare digital transformation was to integrate Artificial Intelligence (AI), Machine Learning (ML), and IoT to control costs and improve patient outcomes.(10) Diagnostics, patient care, and preventive care were enhanced through operational intelligence, real-time monitoring, and a solid health database. The result was improved patient experience, increased resource utilization, and enhanced clinical decision support. However, complete deployment was delayed due to issues such as security, diverse data sources, and legacy systems. The challenges have to be resolved for value-based care and patient experiences without hindrance.
Incorporating digital twin technology into healthcare was intended to enhance the management of senior citizens’ health.(11) Using wearable medical devices and digital twin healthcare (DTH) in a cloud setting, the CloudDTH framework was created. The viability in real-time health condition monitoring, diagnosis, and prediction was demonstrated by the results. The accomplishment of full lifecycle health management and the smooth fusion of virtual and physical healthcare were obstacles. Ensuring security, scalability, and accuracy while maintained them was a major constraint.
The research explored the use of social media platforms in capturing patient-reported outcomes for Multiple Myeloma (MM) and how health-related quality of life (HRQoL) was indicated.(12) Natural language processing was used to analyze the data from the Belong Life patient-centered research network (PCRN). Among 230 patients, some of the symptoms included neuropathy, spinal discomfort, burnout, nausea, and skeletal discomfort, with spinal discomfort often preceding diagnosis. The findings indicated the potential of social media in uncovering patient experience and enabled individual treatment plans. However, limitations such as self-report data biases, unvalidated data, and underrepresentation of some groups were threats. Social media was a valuable way of collecting real-world patient opinions.
The study examined the organizational digital maturity and the impact on clinical outcomes in National Health Service (NHS) hospitals using data for 13 150 669 admissions in 139 hospitals (2015–2016).(13) A regression model examined the correlation with digital maturity and significant medical results. There was no significant correlation between short term mortality, rehospitalization, or adverse events, but there was greater harm-free care and longer patient stays in digitally mature hospitals. The findings confirmed that digital maturity influences some of the results. Nonetheless, also associated with other determinants at the institutional level. Additional analysis needs to be conducted to know how health IT enhances hospital quality improvements.
METHOD
Considering how ongoing innovation and adaptation can improve the efficacy, efficiency, and equity of healthcare delivery in the age of digitalization. This research is based on a quantitative cross-sectional study to investigate the effects of digital communication technology on healthcare services. Workflow effectiveness, coordination between services, satisfaction of patients, and treatment adherence are evaluated in 60 doctors and 200 patients through their surveys. Important points concerning the effectiveness of a consultation and retrieval of health information are evaluated through two questionnaires. Data is processed using the International Business Machines (IBM) Statistical Package for Social Science (SPSS) software, version 27, with a paired sample t-test and descriptive statistics. A consequence level of 0,05 determines statistical significance, ensuring a comprehensive valuation of the role of digital communication in improving healthcare.
Analysis Design
In the digital age, consider how innovation and adaptation can improve the efficacy, efficiency, and equity of healthcare delivery. The research takes a quantitative cross-sectional approach, focusing on the impacts of digital communication technologies on healthcare service quality and patient treatment outcomes. The analysis is carried out in telemedicine platforms, clinics, and hospitals that have adopted digital communication methods, like virtual medical consultations and digital health records. The central goal is to assess the effect of digital communication on some of the key healthcare service indicators like waiting times, consultation durations, and healthcare professionals’ coordination. It also seeks to analyze patient outcomes, such as satisfaction, treatment compliance, and general involvement in the healthcare process.
Data Collection
Examining the important of continuous innovation and adaptation to improve the standard, effectiveness, and equity of healthcare delivery in the digital age. Data collection involved a sample of 60 healthcare professionals and 200 patients from telemedicine platforms, clinics, and hospitals. Data are collected via investigations and questionnaires that are administered to both healthcare professionals and patients. For the healthcare professionals, the survey will quantify how frequently they use digital communication technology, their perceptions of the effectiveness of such technologies in coordination with patients, and their overall satisfaction with the technologies in reducing their workflow. Health service indicators, such as waiting time and consultation duration will be gathered. For the patients, the survey will ask questions regarding their contentment with online consultations, ease of access to information about health, and how digital technology has affected treatment adherence and engagement. Measures of healthcare services, including patient waiting times and compliance with treatment schedules will be collected to compare the state of healthcare delivery before and after the adoption of digital communication technologies.
Research Questionaries’
In the digital age, constant innovation and adaptability are essential to guaranteeing effective, efficient, and equitable healthcare delivery. Healthcare practitioners’ use of digital communication tools in practice, their satisfaction with the tools, and their views on how the tools influence their productivity that will be addressed in the questionnaire. The frequency of digital tool use, saving time on consultation, and improving patient coordination will be incorporated into the questions.
Patient Questionnaire
Focuses on patient satisfaction, treatment adherence, and their experience with digital communication technologies.
Example questions:
1. How satisfied are you with the speed of your consultation?
2. Did you find the digital platform easy to use for accessing health information?
3. How often did you follow treatment recommendations shared through digital communication?
4. Did digital communication help you better understand your treatment plan?
Healthcare Professional Questionnaire
Focuses on efficiency of service delivery, coordination among colleagues, and response times.
Example questions:
1. Has digital communication improved coordination with your colleagues?
2. Have you noticed a reduction in patient wait times since implementing digital communication?
3. How would you rate the efficiency of the telemedicine platform you use?
4. Has digital communication reduced the time required to update and share patient records?
Statistical Analysis
Effective, efficient, and fair healthcare delivery in the digital age depends on ongoing innovation and adaptability. SPSS software can be effectively utilized to conduct both Descriptive statistics and a paired sample t-test are employed to observe the data. Descriptive statistics provide a summary of the central tendencies, dispersion, and frequency distributions of the data gathered. For example, mean values will be obtained for wait times, consultation duration, and patient satisfaction scores. Standard deviations and variance are used to measure the spread of the responses. A paired sample t-test is utilized to contrast patient outcomes and healthcare service indicators before and after the implementation of digital communication technologies. The test can determine if a notable statistical disparity exists in patient outcomes (e.g., satisfaction, adherence) and service efficiency (e.g., wait times). The paired sample t-test presumes that the data is uniformly distributed and also that the comparisons are before and after and thus paired, i.e., they relate to each other directly. A 0,05 significance level will be employed to determine whether the changes are statistically significant.
RESULTS
A comparative analysis of the most critical indicators of healthcare services prior to and subsequent to digital communication technology deployment. The indicators encompass wait time, consultation duration, patient satisfaction, treatment adherence, and health practitioners’ productivity. Descriptive statistics summarize the distribution of the indicators by reporting the differences in minimum, maximum, mean, and standard deviation values. To establish the statistical differences, a paired sample t-test was conducted to compare the pre- and post-implementation.
Demographic
A sum of 260 individuals took part in the analysis, comprising 200 patients and 60 medical professionals who were chosen from a variety of healthcare environments, including hospitals, clinics, and telemedicine platforms are depicted in table 1.
|
Table 1. Demographic Characteristics of Analysis Applicants |
|||
|
Demographic Variable |
Category |
Frequency (n) |
Percentage (%) |
|
Medical Professionals |
Physicians |
30 |
50,0 |
|
Nurses |
20 |
33,3 |
|
|
Other Healthcare staff |
10 |
16,7 |
|
|
Patients Age Group |
18-30 |
50 |
25,0 |
|
31-45 |
70 |
35,0 |
|
|
46-60 |
50 |
25,0 |
|
|
60+ |
30 |
15,0 |
|
|
Patients Gender |
Male |
90 |
45,0 |
|
Female |
110 |
55,0 |
|
|
Healthcare Setting |
Telemedicine platforms |
80 |
40,0 |
|
Clinics |
60 |
30,0 |
|
|
Hospitals |
60 |
30,0 |
|
Physicians made up 50 % of the medical professions, followed by nurses 33,3 % and other healthcare workers 16,7 %. Patient sample stratified by age and gender was varied, with the majority, 35 %, being in the 31–45 age range, followed by 25 % in the 18–30 and 46–60 age ranges, and 15 % in the 60+ age range. Of the patients, female (55 %) and male (45 %). In terms of medical facilities, 40 % of patients used telemedicine platforms, 30 % were treated in clinics, and another 30 % were treated in hospitals. This demographic distribution offers a thorough foundation for assessing how digital communication technologies disturb the effectiveness of healthcare services and the results of patient treatment in various healthcare settings.
Descriptive statistics
Descriptive statistics, such as the mean and standard deviation are needed to summarize the main trends in the treatment of patients and the efficiency of healthcare services. In this analysis, these statistics identify how digital communication technology has affected the provision of services. By computing the mean (µ) and standard deviation (σ), variations in patient satisfaction, treatment adherence, and healthcare professional efficiency can be analyzed before and after implementing digital communication technologies. These measures help identify the central tendencies and distribution of responses, offering a clear understanding of the overall impact of digital communication on healthcare outcomes.
Mean (µ)
The mean represents the average value of a dataset and is calculated using the equation (1).
![]()
Where Xi signifies individual data points and denotes the overall count of observations.
Standard Deviation (σ)
Standard deviation (σ) refers to the extent of deviation or spread in a dataset relative to its mean (µ). The analysis helps measure response consistency regarding patient satisfaction, treatment compliance, and healthcare provider effectiveness before, and after the utilization of digital communication technology. A low standard deviation means that the majority of the data points are grouped around the mean, indicating homogenous responses, whereas a higher standard deviation suggests greater heterogeneity in the data. Using equation (2), the dispersion of healthcare service measures e.g., consultation time and waiting times, can be measured, which provides a greater insight into how digital communication technologies affect healthcare outcomes.
![]()
Where Xi means separate data points, µ represents the mean value of the data, and N denotes the overall total of observations. Table 2 shows the health service metrics result of descriptive statistics.
|
Table 2. Descriptive Statistics Healthcare Service Metrics Before and After Digital Communication Implementation |
||||||||
|
Measure |
Before Digital Communication |
After Digital Communication |
||||||
|
(Min) |
(Max) |
(SD) |
(Mean) |
(Min) |
(Max) |
(SD) |
(Mean) |
|
|
Wait Time (Minutes) |
25 |
50 |
5,1 |
35,2 |
10 |
30 |
4,7 |
20,4 |
|
Consultation Length (Minutes) |
15 |
30 |
3,6 |
20,7 |
10 |
25 |
3,1 |
15,3 |
|
Patient Satisfaction (%) |
50 |
80 |
7,4 |
65,8 |
60 |
95 |
5,9 |
80,3 |
|
Treatment Adherence (%) |
60 |
85 |
6,9 |
72,1 |
70 |
95 |
5,4 |
85,5 |
|
Healthcare Professional Efficiency (Rating 1-10) |
4 |
8 |
1,3 |
6,4 |
6 |
10 |
1,1 |
8,2 |
The evaluation identifies the impression of digital communication tools on clinical results and the proficiency of healthcare. Wait times and consultation duration were considerably reduced, enhancing service access. Patient satisfaction and treatment compliance rose, indicative of increased involvement and adherence. Healthcare providers felt more efficient, implying enhanced coordination and workflow optimization. The statistical significance of the observed changes (p < 0,001) attests that digital communication significantly contributes to maximizing healthcare service delivery.
Paired t-test
Paired t-test is employed to contrast two related sets of data—before and subsequent to the introduction of digital communication technologies to healthcare. This statistical test compares whether there exists a significant difference regarding chief indicators like patient satisfaction, compliance with treatment, efficiency of healthcare professionals, length of consultation, and waiting times. By calculating the test statistic (t-value) using equation (3), the analysis assesses whether the changes in the efficiency of healthcare services and the outcome are statistically significant or if they may have occurred chance. A larger absolute t-value implies a higher probability that digital communication plays a significant role in healthcare service provision.
![]()
Where D ̅ represents the average variance between corresponding values (post-pre), sD denotes the SD of the variance, and n signifies the number of corresponding observations. The p-value is derived from the t-distribution and determines whether the difference is statistically important. Table 3 offers the paired sample t-test outcomes. Paired sample test outcomes of healthcare metrics earlier and later digital communication are illustrated in table 3.
|
Table 3. Paired Sample t-test Results |
|||||
|
Measure |
Before Digital Communication (Mean) |
After Digital Communication (Mean) |
Mean Difference (Post - Pre) |
t-value |
p-value |
|
Wait Time (Minutes) |
35,2 |
20,4 |
-14,8 |
-12,45 |
< 0,001 |
|
Consultation Length (Minutes) |
20,7 |
15,3 |
-5,4 |
-9,73 |
< 0,001 |
|
Patient Satisfaction (%) |
65,8 |
80,3 |
14,5 |
13,26 |
< 0,001 |
|
Treatment Adherence (%) |
72,1 |
85,5 |
13,4 |
11,57 |
< 0,001 |
|
Healthcare Professional Efficiency (Rating 1-10) |
6,4 |
8,2 |
1,8 |
10,34 |
< 0,001 |
The outcomes of the paired sample t-test show substantial increases in healthcare efficiency after the adoption of digital communication technologies. Wait times and consultation lengths were reduced, while patient satisfaction, treatment compliance, and healthcare professional efficiency improved. The negative t-values for wait time (-12,45) and consultation length (-9,73) affirm a decrease in these metrics, while the positive t-values for patient satisfaction (13,26), treatment compliance (11,57), and professional efficiency (10,34) reflect significant improvements. All p-values are < 0,001, validating the statistical significance of these optimizations. Digital communication has successfully optimized healthcare service delivery and patient outcomes. The effect of digital communication on healthcare performance is shown in figure 2.
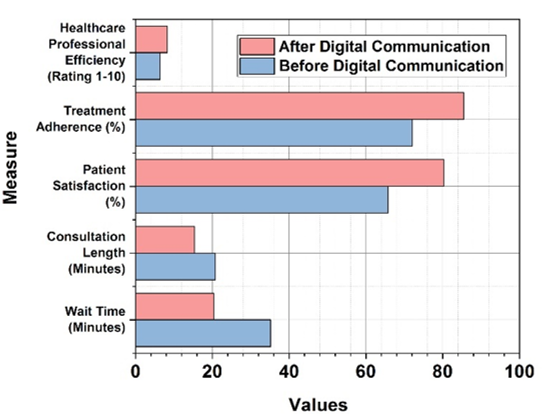
Figure 2. Effect of Digital Communication on Healthcare Performance Metrix
Figure 2 illustrates the impact of digital communication technologies on various indicators of healthcare services through a comparison of pre-and post-implementation statistics. A significant reduction in waiting time and consultation duration reflects improved patient flow and interaction efficiency. Patient satisfaction and compliance with treatment reflect significant improvement, indicating that digital communication has enhanced patient engagement and compliance with medical recommendations. In addition, the efficiency of healthcare workers has been enhanced marginally, meaning enhanced workflow and coordination. In general, the results indicate the facilitatory function of electronic communication in enhancing the optimization of healthcare service delivery towards greater efficiency, patient satisfaction, and compliance with treatment plans.
DISCUSSION
Digital communication solutions facilitate patient involvement, workflow optimization, and provider coordination, which improve patient results and the efficiency of healthcare services. It is challenging to integrate new technology into healthcare systems, particularly when it comes to resolving adoption disparities and guaranteeing continuous interoperability. The dependence of earlier research on theoretical models or small-scale datasets has impeded real-world usefulness. Numerous studies have examined the practice of prioritizing physician productivity over patient-oriented goals, like treatment plan compliance, satisfaction, and general health improvement. To cross these limitations, this research assesses the impact of digital communication on healthcare service delivery by using both actual clinical data and a larger dataset. Improved coordination, reduced administrative waste, and real-time patient information exchange are all facilitated by digital solutions. By allowing doctors to make more informed decisions, timely communication eliminates delays in diagnosis and treatment. Additionally, interactive health tracking, computer-aided reminders, and electronic consultations significantly enhance patient engagement, which enhances therapy outcomes and rates of compliance. In addition, social and cultural determinants of technology adoption have not been investigated in existing research. To bridge this gap, this research investigates how patient demographics, digital literacy, and access to healthcare influence the use of digital healthcare platforms. The findings show that solving these problems increases the efficacy of digital interventions and ensures equal access to healthcare. This research sheds light on the critical function of digital communication in enhancing treatment processes and general healthcare quality through the use of both provider efficiency and patient outcome-driven results.
CONCLUSIONS
Digital communication technology enables improvements in patient satisfaction, treatment adherence, service coordination, and workflow performance. Using information collected from 200 patients and 60 healthcare professionals in different healthcare facilities, its effects were investigated using a quantitative cross-sectional approach. The efficacy of consultations, coordination of providers, patient compliance, and the use of digital technologies were assessed through investigations and surveys. Electronic communication has been found to enhance the capability of delivering services, facilitate the ease of collaboration among providers, and promote patient engagement. By enabling communication, simplifying processes, and promoting patient outcomes in general, technology continues to transform healthcare. The statistical analysis showed considerable decreases in waiting times (35,2 to 20,4 minutes, p < 0,001) and consultation times (20,7 to 15,3 minutes, p < 0,001). Patient satisfaction increased from 65,8 % to 80,3 %, and treatment adherence increased from 72,1 % to 85,5 % (p < 0,001). Healthcare workers noted increased efficiency, with scores increasing from 6,4 to 8,2 (p < 0,001), which may indicate less administrative work and better resource management. The limitations are cross-sectional analysis design, self-reporting bias, and limited generalizability. Longitudinal analysis, representative and larger samples, and comparison of various digital tools should be used in future studies. Consideration of AI integration and patient-specific factors would further maximize digital communication in care delivery.
BIBLIOGRAPHIC REFERENCES
1. Aapro M, Bossi P, Dasari A, Fallowfield L, Gascón P, Geller M, Jordan K, Kim J, Martin K, Porzig S. Digital health for optimal supportive care in oncology: benefits, limits, and future perspectives. Supportive care in cancer. 2020 Oct;28:4589-612. https://doi.org/10.1007/s00520-020-05539-1
2. Laurenza E, Quintano M, Schiavone F, Vrontis D. The effect of digital technologies adoption in healthcare industry: a case based analysis. Business process management journal. 2018 Jul 12;24(5):1124-44.
3. Ricciardi W, Pita Barros P, Bourek A, Brouwer W, Kelsey T, Lehtonen L. How to govern the digital transformation of health services. European journal of public health. 2019 Oct 1;29(Supplement_3):7-12. https://doi.org/10.1093/eurpub/ckz165
4. Kraus S, Schiavone F, Pluzhnikova A, Invernizzi AC. Digital transformation in healthcare: Analyzing the current state-of-research. Journal of Business Research. 2021 Feb 1;123:557-67. https://doi.org/10.1016/j.jbusres.2020.10.030
5. Aceto G, Persico V, Pescapé A. The role of Information and Communication Technologies in healthcare: taxonomies, perspectives, and challenges. Journal of Network and Computer Applications. 2018 Apr 1;107:125-54.
6. Kelly JT, Campbell KL, Gong E, Scuffham P. The Internet of Things: Impact and implications for health care delivery. Journal of medical Internet research. 2020 Nov 10;22(11):e20135. https://doi.org/10.2196/20135
7. Aceto G, Persico V, Pescapé A. Industry 4.0 and health: Internet of things, big data, and cloud computing for healthcare 4.0. Journal of Industrial Information Integration. 2020 Jun 1;18:100129.
8. Dhagarra D, Goswami M, Kumar G. Impact of trust and privacy concerns on technology acceptance in healthcare: an Indian perspective. International journal of medical informatics. 2020 Sep 1;141:104164. https://doi.org/10.1016/j.ijmedinf.2020.104164
9. Peek N, Sujan M, Scott P. Digital health and care in pandemic times: impact of COVID-19. BMJ Health & Care Informatics. 2020 Jun 21;27(1):e100166. https://doi.org/10.1136/bmjhci-2020-100166
10. Gopal G, Suter-Crazzolara C, Toldo L, Eberhardt W. Digital transformation in healthcare–architectures of present and future information technologies. Clinical Chemistry and Laboratory Medicine. 2019 Mar 1;57(3):328-35. https://doi.org/10.1515/cclm-2018-0658
11. Liu Y, Zhang L, Yang Y, Zhou L, Ren L, Wang F, Liu R, Pang Z, Deen MJ. A novel cloud-based framework for the elderly healthcare services using digital twin. IEEE access. 2019 Apr 11;7:49088-101. https://doi.org/10.1109/ACCESS.2019.2909828
12. Gries KS, Fastenau J. Using a digital patient powered research network to identify outcomes of importance to patients with multiple myeloma. Journal of Patient-Reported Outcomes. 2020 Dec;4:1-9. https://doi.org/10.1186/s41687-020-00242-5
13. Martin G, Clarke J, Liew F, Arora S, King D, Aylin P, Darzi A. Evaluating the impact of organizational digital maturity on clinical outcomes in secondary care in England. NPJ digital medicine. 2019 May 16;2(1):41. https://doi.org/10.1038/s41746-019-0118-9
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: RenukaJyothi S, Nidhi Srivastava, Srikant Kumar Dhar.
Methodology: RenukaJyothi S, Nidhi Srivastava, Srikant Kumar Dhar.
Software: RenukaJyothi S, Nidhi Srivastava, Srikant Kumar Dhar.
Drafting - original draft: RenukaJyothi S, Nidhi Srivastava, Srikant Kumar Dhar.
Writing - proofreading and editing: RenukaJyothi S, Nidhi Srivastava, Srikant Kumar Dhar.