doi: 10.56294/mw2023114
ORIGINAL
Developing Patient-Centered Communication Models to Improve Patient Engagement and Enhance Clinical Efficiency
Desarrollo de modelos de comunicación centrados en el paciente para mejorar su participación y aumentar la eficacia clínica
Debasmita Tripathy1 ![]() *, Malathi H2
*, Malathi H2
![]() , Pallavi Prakash Chandra3
, Pallavi Prakash Chandra3
![]()
1IMS and SUM Hospital, Siksha ‘O’ Anusandhan (deemed to be University), Department of General Medicine. Bhubaneswar, Odisha, India.
2JAIN (Deemed-to-be University), Department of Biotechnology and Genetics. Bangalore, Karnataka, India.
3School of Allied Health Sciences, Noida International University. Greater Noida, Uttar Pradesh, India.
Cite as: Tripathy D, H M, Prakash Chandra P. Developing Patient-Centered Communication Models to Improve Patient Engagement and Enhance Clinical Efficiency. Seminars in Medical Writing and Education. 2023; 2:114. https://doi.org/10.56294/mw2023114
Submitted: 07-09-2022 Revised: 19-12-2022 Accepted: 24-02-2023 Published: 25-02-2023
Editor:
PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Debasmita Tripathy *
ABSTRACT
The importance of communication, centered around the patients, has proven effective in enhancing patient engagement and improving clinical efficiency despite restrictions of time and ability often preventing effective communication in circumstances surrounding trauma care. Breakdown of communication in such an environment shall bid a huge impact on the outcome of a patient; hence, that sets the background of developing a context within which communication strategies can happen to be responsive to the dynamics of the trauma team. Research recruited 126 medical hospital staff within trauma teams who had undergone communication training completely focused on patient-centered approaches. The training was to improve patient engagement and team communication during trauma encounters. Participants engaged in simulated trauma scenarios both before and after the training, which was followed by a 6-week follow-up. Data was analyzed with one way ANOVA with post-hoc Tukey’s test and regression analysis aimed at investigating the effect and sustainability of communication improvement. There was a significant improvement in communication and patient engagement behaviors after the training (p<0,05), and, although quite a renaissance regarding some loss of retention (p>0,05), those effects were maintained at the 6-week follow-up. Regression analysis showed that pre-training knowledge about communication and intensity of training for the retention of improved communication performance in the longer run were the two major factors. Research shows that brief training interventions can greatly improve trauma team communications for a long period of time, consequently leading to enhanced patient engagement as well as improved clinical efficiency.
Keywords: Patient Engagement; Clinical Efficiency; Patient-Centered Communication; Trauma; Emergency Settings.
RESUMEN
La importancia de la comunicación, centrada en los pacientes, ha demostrado ser eficaz para mejorar el compromiso de los pacientes y la eficiencia clínica, a pesar de las restricciones de tiempo y capacidad que a menudo impiden una comunicación eficaz en circunstancias relacionadas con la atención traumatológica. La interrupción de la comunicación en un entorno de este tipo tendrá un enorme impacto en el resultado de un paciente; por lo tanto, esto establece el trasfondo de desarrollar un contexto en el que las estrategias de comunicación puedan responder a la dinámica del equipo de traumatología. La investigación reclutó a 126 miembros del personal médico hospitalario de equipos de traumatología que habían recibido una formación en comunicación totalmente centrada en los enfoques centrados en el paciente. El objetivo de la formación era mejorar el compromiso del paciente y la comunicación del equipo durante los encuentros traumatológicos. Los participantes participaron en escenarios de trauma simulados antes y después de la formación, a la que siguió un seguimiento de 6 semanas. Los datos se analizaron mediante un ANOVA unidireccional con la prueba post hoc de Tukey y un análisis de regresión destinado a investigar el efecto y la sostenibilidad de la mejora de la comunicación. Hubo una mejora significativa en las conductas de comunicación y compromiso del paciente tras la formación (p<0,05) y, aunque bastante renacida en cuanto a cierta pérdida de retención (p>0,05), esos efectos se mantuvieron en el seguimiento de 6 semanas. El análisis de regresión mostró que los conocimientos previos al entrenamiento sobre comunicación y la intensidad del entrenamiento para la retención de la mejora del rendimiento comunicativo a largo plazo eran los dos factores principales. La investigación demuestra que las intervenciones breves de formación pueden mejorar en gran medida las comunicaciones del equipo de traumatología durante un largo periodo de tiempo, lo que, en consecuencia, conduce a una mayor implicación de los pacientes, así como a una mejora de la eficacia clínica.
Palabras clave: Compromiso del Paciente; Eficiencia Clínica; Comunicación Centrada en el Paciente; Trauma; Urgencias.
INTRODUCTION
The medical field relies heavily on patient centered communications, particularly in trauma care settings where prompt decisions and effective communication can have a big impact on patient outcomes. Effective communication not only ensures that patients’ needs and concerns are recognized and met in high stress settings like trauma units but also builds confidence between patients and medical professionals.(1) Enhancing patient engagement, increasing treatment regimen adherence, and raising overall care satisfaction all depend on trust. In trauma teams, efficient communication is especially essential for coordination, reducing mistakes and ensuring prompt and precise treatments. Patient centered communications enhance the efficiency of clinical processes and the standard of care by considering the patients viewpoint and preference while making decisions.(2) To encourage positive treatment outcomes and opinions about the caliber of care received, patient-centered care refers to the delivery of healthcare services that honor and attend to the needs of patients and their caregivers. The emotion of worry or interest in something or someone in need of care is called care.(3) An aging population, rising prices, and the increasing burden of chronic diseases are all contributing factors to the current state of healthcare. Conventional fee-for-service (FFS) models, which reward medical professionals according to the number of services they give, are becoming less and less viable.(4) Through systematic exposure to targeted and focused information, health literacy can also be seen as a personal asset, a collection of transferable, personalized skills that can be developed to encourage more autonomy in health decision-making. Previous analysis have identified an order of three levels of health literacy skills, which are explained here.(5) The idea of patient-centered care in cancer survival has not yet been completely established or applied in clinical settings. More information and understanding about life after cancer treatment, as well as resources to help patients participate in their care, Numerous research that have examined patient preferences have found that greater care coordination, particularly during care transitions, easier utilization of risk-management and health promotion programs, and enhanced provider-patient communication are all essential.(6) Increasing patient engagement in their treatment is one strategy to make healthcare more patient-centered and enhance the patient experience. To provide patient-centered care, doctors must ascertain the values and preferences of their patients, and patients must be ready to participate fully in their appointments. By talking to their provider about their wants, worries, and inquiries, patients who actively participate in their appointments take charge of their treatment. Due to communication norms, physicians typically reciprocate when patients engage in active communication activities.(7)
To improve healthcare delivery, integrating effective communication with patient-centered care is the goal of the patient communication paradigm of care, as medical and technological advancements have revolutionized patient-provider interactions, as described.(8) Only the first two factors, genetic susceptibility and clinical health care, have a direct biological relationship to health. The term social determinants of health refer to a combination of socioeconomic factors, including educational attainment, employment, income, marital status, and ethnicity, as well as physical and environmental factors, including residence location, quality of air and water, buildings, spaces, and transportation. The social factors that were indicative of health were basically the circumstances around a person's birth, development, life, employment, and aging.(9) Little was understood about how the patient-centered care influences relationships between physicians and patients, despite well-known medical advancements. The narrative investigation examines interpersonal abilities in therapeutic and diagnostic contacts and intake processes as seen by doctors, nurses, and healthcare greeters.(10) The significance of including patients, families, and other stakeholders in research was emphasized.(11) In order to improve clinical and public health services, this research would explain the way to establish patient-centered outcomes research (PCOR) using participatory research in the community concepts. Building capacity for collaborative engagement, acknowledging stakeholder-driven objectives, encouraging shared ownership in health priorities, and acknowledging the continuous commitment to adoption, dissemination, and sustainability were some of the guiding principles. The benefits of patient-driven research in head and neck cancer were discussed along with the insights gained from collaborations with patients and caregivers.(12) To act as a template for further studies. Head and neck cancer survivors led weekly meetings with a multidisciplinary team led by a physician champion and got training in research methods and good communication. Obstructive sleep apnea was a common disorder that could have impacts on metabolism, cardiovascular health, and neurocognition. Patient involvement was necessary for effective therapy, and the management of this illness has changed from diagnosis to long-term care. Patient outcomes could be improved by a patient-centered approach that includes identifying the needs of each patient, learning about their values and preferences, employing shared decision-making, improving patient education and support, encouraging involvement, and maximizing care coordination, continuity of care, and access to care.(13) Enhancing patient participation, improving care coordination, guaranteeing continuity of treatment, and evaluating patient-centered outcomes were all part of the strategy. To deliver person-centered patient care services as outlined, Johns Hopkins Aramco Healthcare (JHAH) is integrating telecommunication technologies, including phone and video consultation, in a pharmacist-led medication management clinic (MMC).(14) Timely concerns along with insufficient preparation and communication problems in trauma care reduce patient management effectiveness by creating major issues, which lead to incomplete evaluations and cause essential decisions to suffer delays with negative effects on patient outcomes that minimize care standard and operational productivity.(15)
Objective of the research
To develop and assess a patient-centered communications training program for trauma care terms, aimed at improving patient engagement and enhancing clinical efficiency. The research uses simulated trauma scenarios and follow-up evaluations to assess skill uptake and the effect of the team's communication on patient outcomes in high-stress conditions.
METHOD
To increase patient involvement and clinical efficiency, this part explains data collecting, variable explanation, questionnaire innovations, and data analysis for patient-centered communication models.
Data collection
Research endeavor designed to assess the effectiveness of patient-centered communication training in trauma care environments recruited 126 medical staff included doctors, nurses, Emergency Medical Technician (EMT), and other healthcare personnel specializing in trauma teams. Staff members in the trauma care unit ranged in age from 22 to 55. The participants' backgrounds varied, but most had between six and ten years of experience. Their educational background varied, including undergraduate degrees, master’s degrees, specialized certifications, and a few holding doctoral qualifications. The salary range also differed, reflecting the variety of roles, with physicians earning higher salaries compared to nurses and EMTs. Demographic details, including age, gender, years of experience, education, and income levels, are summarized in table 1.
|
Table 1. Demographic table |
||
|
Category |
Subcategory |
N (%) |
|
Age |
25-35 years |
40 (31,75) |
|
36-45 years |
50 (39,68) |
|
|
46-55 years |
36 (28,57) |
|
|
Gender |
Female |
66 (52,38) |
|
Male |
60 (47,62) |
|
|
Experience |
< 5 years |
35 (27,78) |
|
6-10 years |
55 (43,65) |
|
|
11-15 years |
36 (28,57) |
|
|
Education level |
Undergraduate |
35 (27,78) |
|
Master’s degree |
45 (35,71) |
|
|
Doctorate |
12 (9,52) |
|
|
Specialized certification |
34 (26,98) |
|
|
Income level |
30 000-50 000 |
50 (39,68) |
|
50 000-90 000 |
60 (47,62) |
|
|
90 000-150 000 |
16 (12,70) |
|
Survey instrument
The analysis presents the questionnaire based on key evaluation variables related to patient-centered communication training. The survey assesses five critical dimensions: Decision-making, communication clarity, team confidence, situational awareness coping with stress, and patient satisfaction. A quantitative approach was adopted using an online survey distributed via Google Forms. A Likert scale, with 5 denoting "strongly agree" and 1 denoting "strongly disagree," was used to gather participant responses. Each variable consists of two questions, totaling 10 questions, designed to capture participants' perceptions of the impact of the training intervention.
· Decision-making: decision-making refers to the ability of healthcare professionals to evaluate available information, assess risks, and choose the best course of action in critical and time-sensitive situations, ensuring effective patient care and team coordination under pressure.
· Communication clarity: communication clarification is composed of the ability to convey information efficiently, ensure that all team members and patients actually understand what is being discussed, encourage the safe decision-making process, and minimize errors when under extreme pressure.
· Team confidence: team confidence refers to the prevailing feeling of trust and assurance that members of the health team have for each other; it is built on successful teamwork, mutual respect, and an exchange of knowledge, thus aiding team performance and the agile and synchronicity responses in traumatic situations.
· Situational awareness coping with stress: health care workers have to act on that situation, whether they are treating trauma or responding to an emergency. Situational awareness is the ability to recognize, comprehend and anticipate in real-time the changing aspects of a situations. Coping with stress entails controlling both emotional and physical responses to pressure with poise and strength. Also, the use of mechanisms for avoiding burnout while rendering the best services within the limits of captivated emotional stress-filled trauma environments.
· Patient satisfaction: patients’ experiences, trust, and general opinion of the quality of care they receive are all directly affected by the extent to which their wants, worries, and preferences are recognized and attended by their care providers, as demonstrated by the patient's Sari faction.
Disruption of Training program (6 weeks)
The training initiative's 6-week breakdown evaluated the abilities acquired during the patient-centered interactions training that were kept and used over time. The key objectives of the training, were actively assessed and participated in during the 6 weeks course.
· Actively involving the patients in discussions about their care: the importance of patient's decision-making in the treatment was highly emphasized throughout the course.
· The healthcare professionals are motivated to actively inform patients of their treatment options and to involve them in key decisions taken on their behalf. This approach is geared toward the overall empowerment and engagement of the patients with the aim of enhancing patient outcomes and satisfaction.
· Providing clear explanations, even in high-stress situations: one of the foremost aims was to enable health professionals to communicate effectively under pressure. The training taught participants to stay calm and offer crisp, brief answers in stressful trauma situations. This element was crucial to reduce miscommunication and further the cause of patient safety, especially in settings where prompt and unambiguous communication is critical.
· Ensuring the patient feels heard, understood, and supported: the need for empathy and emotional support in patient encounters was upheld throughout the training. The framework is expected to enhance trust among providers, thereby increasing patient satisfaction and overall healthcare. In this regard, patients have mainly been taken into concern in terms of blaming care professionals for making patients feel heard, seen, and cared for.
Exploration of variables
Several key variables that are crucial for enhancing patient-centered communication in trauma care settings, focusing on improving clinical efficiency and patient engagement, were evaluated. The variables are grouped into five key dimensions. These dimensions were selected based on their relevance to effective communication and their trauma team dynamics and patient outcomes. Figure 1 presents these variables along with their respective explanations, highlighting their role in improving both team performance and patient care in a high-pressure trauma environment.

Figure 1. Evaluation of key variables
· Decision Making: in trauma care, where medical personnel must quickly analyze data, weigh risks, and choose the course of action, decision-making is an important ability. Involving the patient in decision-making in patient-centered communication ensures that medical professionals are aware of their alternatives for treatment and can participate in the process, predicting a sense of autonomy. By consolidating patient trust, this partnership raises patient satisfaction and engagement. In high-stress, time-sensitive trauma settings, effective decision-making also promotes therapeutic efficiency by minimizing delays, misunderstandings, and ensuring a coordinated response, which results in quicker treatment and improved patient outcomes.
· Community Clarity: as misunderstandings can lead to blunders, a clear transfer of communications is very important in trauma care. Healthcare providers have much to communicate with respect to complex medical information in a way that is rightly understood and without ambiguity, be it relayed to the patients or among team members. Patient-centered communication is mostly focused on language that is clear so that patients understand what their problems are or their treatment options. This creates trust and reduces fear in the patients, hence allowing them to make informed decisions regarding their care. Also, team clarity promotes good teamwork that enhances coordination of care and allows for quicker and more effective responses. This effective communication enhances therapeutic outcomes, reduces error chance, and engages patients.
· Team Confidence: in trauma care, where rapid response is workable enough team confidence plays a permeable role. As mutual trust exists among the communicating team members, their confidence grows in parallel lines. This mutual trust is evident in improved team performance. Patient-centered communication contributes positively by instilling mutual respect, open-forum discussion, and shared-forum collaboration. Teams with confidence feel quicker in fulfilling their decision-making processes and consequently in improved patient care. A confident team eases patients in most stressful situations to grow their trust and participation. This collective confidence improves patient outcomes and satisfaction, makes fewer errors, and increases efficiency in care.
· Situational awareness and coping with stress: a critical element for trauma treatment, since situations could change rapidly and healthcare professionals will face a significant challenge in addressing these critical problems. Healthcare professionals are supposed to be informed about all dynamic situations going on, like the status of the patient, current situation, and environmental features affecting clinical decisions. The stress management practice allows healthcare workers to achieve a controlled emotional reaction while concentrating on stressful situations. Patient-centered interactions will keep doctors in touch even in crushing situations because that gives the patients a feeling of care and understanding. The situational awareness with stress management enhances line efficiency through error reduction, facilitating cooperation, and assuring optimal patient results in accident emergencies.
· Patient satisfaction: patient satisfaction measures how well healthcare professionals cater to the needs, desires, and concerns of the patients. Trauma care relies heavily on the principle of patient-centered communication since it allows the patients to feel respected, heard, and incorporated in their own treatment. If patients are satisfied, they will most likely adhere to the treatment plans, disclose their feelings freely, and participate actively in their own rehabilitation, thus improving patient outcomes. High satisfaction instills faith in the medical professional, which is enhanced in trauma settings where the patients oftentimes feel helpless. A care approach focusing on patient satisfaction leads to increased engagement, compliance, and therefore effective treatment by improving communication and addressing emotional and psychological needs.
Data analysis
Data analysis is essential to deriving insights from complex datasets, empowering decision-making and strategic planning. In this research, data analysis will be employed to assess clinical efficacy and patient-centered communication effectiveness. The SPSS v29 statistical software is used to perform the analysis. Three key approaches, such as regression analysis, one way ANOVA, and post-hoc Tukey’s test is used to evaluate the influence of communications. training on trauma team performance and its sustainability over time, these methods provide a comprehensive understanding of training effectiveness and behavioral changes.
One Way ANOVA: the unbiased evaluations of one-way ANOVA can be determined as an wji∈R,1≤i≤mj,1≤j≤l among l with various splitting of O1,…,Ol, decompositions of ANOVA have been illustrated in the equations (1-4).
Here:
![]()
Represents j group-wise mean and:
![]()
Determines total mean values, thus the overall detection can be illustrated in the equation (5):
![]()
Post-hoc Tukey’s test: tukey's test assists in identifying which groups are different if an ANOVA reveals that at least one group differs from the others significantly. It does this by comparing each pair of groups' means and determining if the differences are statistically significant.
For Tukeys’s test, the statis R for each pair of group comparison is calculated as equation (6).
![]()
Where Wj-Wi are the means of the two groups being compared, MSE is the mean square error from the ANOVA, M is the number of observations in each group.
Regression analysis: this analysis is utilized to investigate relationships between design preferences for sustainability and cultural appreciation. Equation (7) indicates the basic formula for evaluating regression analysis.
![]()
Where the dependent variable is denoted by Bj. The variableF is the function, Aj is an independent variable, β is an unknown parameter and ϵj is the error indicator. This analysis is used in modern innovative works as an effective method to comprehend complex relationships between variables, allowing for reliable assessments and intelligent choice-making in a variety of fields, including technology and marketing, especially in areas where complex patterns need to be found and large data are available.
RESULTS
The evaluation performance of quantitative assessments and data analysis techniques are examined in this phase.
Evaluation of One-way ANOVA with post-Tukey's test
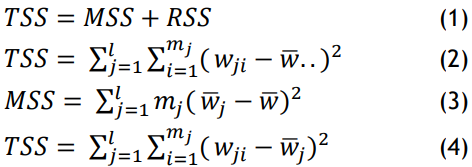
Table 2 and figure 2 (a and b) present the results of the ANOVA and post hoc Tukey's test for five key variables related to patient communications training. Table 2 shows the pre-and post-test mean scores for each variable, along with the corresponding F-values and p-values from the ANOVA. The significant P-values (<0,05) indicate that there were notable improvements in the means after training. The post-hoc Tukey's test further confirms the significance of the difference between pre-post test scores for each variable, with p-values also under 0,05, highlighting that the training effectively enhanced communication-related skills across all dimensions.
|
Table 2. outcomes of One-way ANOVA with post Tukey's test |
|||||
|
Variable |
Pre-test Mean |
Post-test Mean |
F-value |
P-value (ANOVA) |
Post-hoc Tukey's test (p-value) |
|
Decision making |
3,45 |
4,56 |
6,35 |
0,015 |
Pre vs post: 0,032 |
|
Communication clarity |
3,20 |
4,00 |
7,12 |
0,010 |
Pre vs post: 0,042 |
|
Team confidence |
3,55 |
4,30 |
5,75 |
0,020 |
Pre vs post: 0,028 |
|
Situational awareness Coping with stress |
3,25 |
3,95 |
4,55 |
0,045 |
Pre vs post: 0,055 |
|
Patient Satisfaction |
3,80 |
4,60 |
8,80 |
0,008 |
Pre vs post: 0,010 |
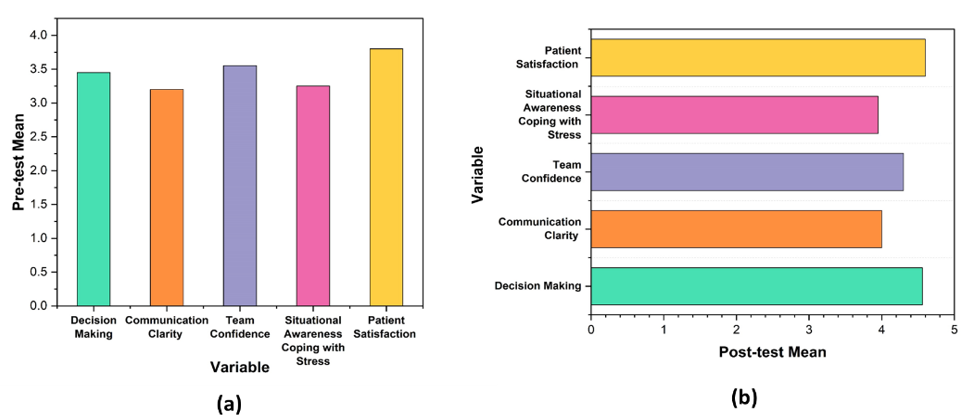
Figure 2. Comparison of One-way ANOVA with post Tukey's test (a) Pre-test mean; (b) Post-test mean
Evaluation of Regression analysis
Regression analysis of results for pre-test data
Table 3 and figure 3(a) present the result of regression analysis for five key variables, including the Regression coefficient (β), Standard error (SE), T-value, P-value, and R2 Values. The regression coefficients represent the degree and direction of each outcome variable's link with the independent variable (training). The statical importance of the correlations is shown by the T-value and P-value, with p-values less than 0,05, indicating that the training had a substantial impact on each variable. The R2 values between 0,30 and 0,35 show a moderate effect of training on these variables.
|
Table 3. Regression analysis of results for pre-test data outcomes |
|||||
|
Variable |
Regression coefficient (β) |
Standard error (SE) |
T-value |
p-value |
R2 |
|
Decision making |
0,70 |
0,22 |
3,18 |
0,002 |
0,32 |
|
Communication clarity |
0,60 |
0,20 |
3,00 |
0,004 |
0,30 |
|
Team confidence |
0,65 |
0,18 |
3,61 |
0,001 |
0,33 |
|
Situational awareness Coping with stress |
0,75 |
0,25 |
3,00 |
0,004 |
0,35 |
|
Patient Satisfaction |
0,80 |
0,26 |
3,08 |
0,003 |
0,34 |
Regression analysis of results for post-test data
The table 4 and figure 3 (b) present the result of a regression analysis for five key variables, including the Regression coefficient (β), Standard error (SE), T-value, P-value, and R2 Values. The regression coefficients represent the degree and direction of each outcome variable's link with the independent variable (training). The T-value and P-value indicate the statical significance of those relationships, with p-values less than 0,05, confirming that each variable is significantly influenced by the training. The R2 values, ranging from 0,38 to 0,45, demonstrate a sustainable effect of the training on these communication-related variables.
|
Table 4. Regression analysis of results for post-test data |
|||||
|
Variable |
Regression coefficient (β) |
Standard error (SE) |
T-value |
p-value |
R2 |
|
Decision making |
0,95 |
0,23 |
4,13 |
0,001 |
0,43 |
|
Communication clarity |
0,80 |
0,21 |
3,81 |
0,002 |
0,38 |
|
Team confidence |
0,85 |
0,18 |
4,72 |
0,000 |
0,41 |
|
Situational awareness Coping with stress |
1,05 |
0,26 |
4,04 |
0,001 |
0,44 |
|
Patient Satisfaction |
1,10 |
0,28 |
3,93 |
0,003 |
0,45 |
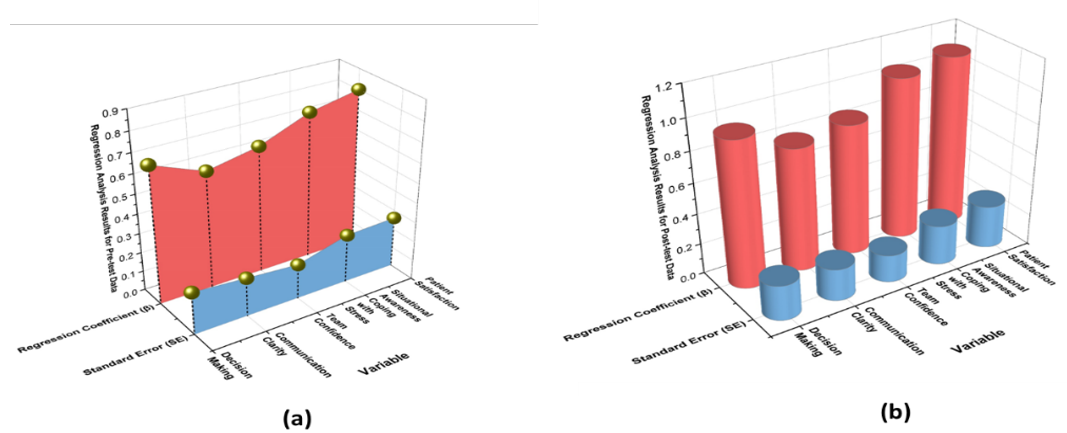
Figure 3. Regression analysis of results for (a) Pre-test data; (b) Post-test data
DISCUSSION
The performance evaluation of the patient-centered communication training reveals significant improvements in communications-related skills, as assessed through both one-way ANOVA with post-hoc Tukey's test and regression analysis. The analysis results, with p-values consistently below 0,05, indicate that training had a statistically significant effect on variables, such as decision-making, communication clarity, team confidence, situational awareness, coping with stress, and patient satisfaction, confirming the effectiveness of the training. The post-hoc Tukey's test further supports these findings, showing significant relationships between the training and the outcome variables, with p-values under 0,05. The R2 values for post-test data (ranging from 0,38 to 0,45) suggest a moderate to strong and sustainable effect of the training, explaining a significant portion of the variance in the assessed variables, reinforcing the lasting impact of the intervention on clinical performance.
CONCLUSIONS
Research aimed to assess the effectiveness of a patient-centered communications training program for trauma care terms to improve patient engagement and clinical efficiency. The research involved 126 medical staff members from trauma teams who underwent training focused on enhancing communications and engagement during trauma encounters. Participants completed simulated trauma scenarios before and after the training, followed by a 6-week follow-up to assess the sustainability of communications improvements. Statistical analysis, including one-way ANOVA and regression analysis, was used to evaluate the impact of the training. The results indicated significant improvements in communications and patient engagement behaviors (p<0,05), which were sustained at the 6-week follow-up, though some retention loss was observed (p>0,05). Regression analysis identified prior communications experience and training intensity as key factors influencing long term retention of improved communications behaviors. Participants expressed high satisfaction with the training and a strong intent to incorporate the learned communication strategies into their practice. Despite some limitations, including potential biases in self-reported satisfaction and the retention loss observed, the research demonstrates that brief, targeted training interventions can lead to significant improvements in trauma team communications. Future research could explore longer follow-up periods and expanded training modules to further refine and assess the long-term impact of patient-centered communications in high-stress emergency settings.
BIBLIOGRAPHIC REFERENCES
1. Marler H, Ditton A. “I'm smiling back at you”: exploring the impact of mask wearing on communication in healthcare. International journal of language & communication disorders. 2021 Jan;56(1):205-14.Doi: https://doi.org/10.1111/1460-6984.12578.
2. Veilleux S, Noiseux I, Lachapelle N, Kohen R, Vachon L, Guay BW, Bitton A, Rioux JD, iGenoMed Consortium. Patients’ perception of their involvement in shared treatment decision making: key factors in the treatment of inflammatory bowel disease. Patient education and counseling. 2018 Feb 1;101(2):331-9.Doi: https://doi.org/10.1016/j.pec.2017.07.028.
3. Kwame A, Petrucka PM. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC nursing. 2021 Sep 3;20(1):158.Doi: https://doi.org/10.1186/s12912-021-00684-2.
4. Fu R, Shen Y, Noguchi H. The best of both worlds? The economic effects of a hybrid fee‐for‐service and prospective payment reimbursement system. Health Economics. 2021 Mar;30(3):505-24.Doi: https://doi.org/10.1002/hec.4205.
5. Muscat DM, Shepherd HL, Nutbeam D, Trevena L, McCaffery KJ. Health literacy and shared decision-making: exploring the relationship to enable meaningful patient engagement in healthcare. Journal of general internal medicine. 2021 Feb;36:521-4.Doi: https://doi.org/10.1007/s11606-020-05912-0.
6. Mead KH, Wang Y, Cleary S, Arem H, Pratt-Chapman ML. Defining a patient-centered approach to cancer survivorship care: development of the patient centered survivorship care index (PC-SCI). BMC health services research. 2021 Dec 18;21(1):1353.Doi: https://doi.org/10.1186/s12913-021-07356-6.
7. Agha AZ, Werner RM, Keddem S, Huseman TL, Long JA, Shea JA. Improving patient-centered care: how clinical staff overcome barriers to patient engagement at the VHA. Medical care. 2018 Dec 1;56(12):1009-17.Doi: https://doi.org/10.1097/MLR.0000000000001007.
8. Tran BQ. Strategies for effective patient care: Integrating quality communication with the patient‐centered approach. Social and Personality Psychology Compass. 2021 Jan;15(1):e12574.Doi: https://doi.org/10.1111/spc3.12574.
9. Naughton CA. Patient-centered communication. Pharmacy. 2018 Feb 13;6(1):18.Doi: https://doi.org/10.3390/pharmacy6010018.
10. Akseer R, Connolly M, Cosby J, Frost G, Kanagarajah RR, Lim SH. Clinician–patient relationships after two decades of a paradigm of patient-centered care. International Journal of Healthcare Management. 2021 Jul 3;14(3):888-97.Doi: https://doi.org/10.1080/20479700.2020.1713535.
11. Kwon SC, Tandon SD, Islam N, Riley L, Trinh-Shevrin C. Applying a community-based participatory research framework to patient and family engagement in the development of patient-centered outcomes research and practice. Translational behavioral medicine. 2018 Oct;8(5):683-91.Doi: https://doi.org/10.1093/tbm/ibx026.
12. Stergiopoulos S, Michaels DL, Kunz BL, Getz KA. Measuring the impact of patient engagement and patient centricity in clinical research and development. Therapeutic innovation & regulatory science. 2020 Jan;54:103-16.Doi: https://doi.org/10.1007/s43441-019-00034-0.
13. Forsythe L, Heckert A, Margolis MK, Schrandt S, Frank L. Methods and impact of engagement in research, from theory to practice and back again: early findings from the Patient-Centered Outcomes Research Institute. Quality of Life Research. 2018 Jan;27:17-31.Doi: https://doi.org/10.1007/s11136-017-1581-x.
14. Mohiuddin SI, Thorakkattil SA, Abushoumi F, Nemr HS, Jabbour R, Al-Ghamdi F. Implementation of pharmacist-led tele medication management clinic in ambulatory care settings: a patient-centered care model in COVID-19 era. Exploratory Research in Clinical and Social Pharmacy. 2021 Dec 1;4:100083.Doi: https://doi.org/10.1016/j.rcsop.2021.100083.
15. Al-Khawaga S, Abdelalim EM. Potential application of mesenchymal stem cells and their exosomes in lung injury: an emerging therapeutic option for COVID-19 patients. Stem cell research & therapy. 2020 Dec;11:1-33.Doi: https://doi.org/10.1186/s13287-020-01963-6
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Debasmita Tripathy, Malathi H, Pallavi Prakash Chandra.
Methodology: Debasmita Tripathy, Malathi H, Pallavi Prakash Chandra.
Software: Debasmita Tripathy, Malathi H, Pallavi Prakash Chandra.
Drafting - original draft: Debasmita Tripathy, Malathi H, Pallavi Prakash Chandra.
Writing - proofreading and editing: Debasmita Tripathy, Malathi H, Pallavi Prakash Chandra.