doi: 10.56294/mw2023117
ORIGINAL
Analyzing the Ethical Implications of Resource Allocation and Patient Autonomy in Rehabilitation Medicine
Análisis de las implicaciones éticas de la asignación de recursos y la autonomía del paciente en medicina de rehabilitación
Pradeepta Sekhar Patro1
![]() *,
Jamuna KV2
*,
Jamuna KV2 ![]() , Rama Sankar3
, Rama Sankar3
![]()
1IMS and SUM Hospital, Siksha ‘O’ Anusandhan (deemed to be University), Department of Immunology. Bhubaneswar, Odisha, India.
2JAIN (Deemed-to-be University), Department of Forensic science. Bangalore, Karnataka, India.
3Noida International University, Department of Community Medicine. Greater Noida, Uttar Pradesh, India.
Cite as: Sekhar Patro P, KV J, Sankar R. Analyzing the Ethical Implications of Resource Allocation and Patient Autonomy in Rehabilitation Medicine. Seminars in Medical Writing and Education. 2023; 2:117. https://doi.org/10.56294/mw2023117
Submitted: 08-09-2022 Revised: 20-12-2022 Accepted: 25-02-2023 Published: 26-02-2023
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Sekhar Patro P *
ABSTRACT
Ethical dilemmas in rehabilitation medicine, especially around resource allocation and patient autonomy, play a critical role in clinical decision-making. The challenge of limited resources makes it essential to understand how physicians navigate these issues in their daily practice. The objective is to analyze how resource constraints affect ethical decision-making in rehabilitation, focusing on balancing patient autonomy with the allocation of limited resources. A survey was conducted with 73 rehabilitation doctors, assessing their views on key ethical issues in resource-limited settings. Chi-square tests were used to identify associations among demographic factors and ethical attitudes, Correlation Analysis examined the relationship between views on resource allocation and patient autonomy. Regression Analysis was employed to identify significant predictors of ethical decision-making, with an emphasis on experience and professional background. Chi-Square Tests showed that Patient Autonomy Priority (χ² = 5,12) were more likely to prioritize patient autonomy, while Resource Allocation Efficiency (χ² = 6,21), more experienced doctors leaned toward resource efficiency. Correlation Analysis revealed a moderate relationship between attitudes toward resource allocation and patient autonomy, suggesting potential conflicts in decision-making. The findings underscore the influence of demographic factors on ethical decision-making in rehabilitation medicine. Understanding these influences can guide interventions aimed at fostering a more balanced, patient-centered approach to care in resource-limited environments, offering valuable insights for improving ethical practices in clinical settings.
Keywords: Rehabilitation Medicine; Resource Allocation; Patient Autonomy; Chi-Square Tests; Correlation Analysis; Regression Analysis; Clinical Practice.
RESUMEN
Los dilemas éticos en la medicina de rehabilitación, especialmente en torno a la asignación de recursos y la autonomía del paciente, desempeñan un papel fundamental en la toma de decisiones clínicas. El reto de los recursos limitados hace que sea esencial entender cómo los médicos se enfrentan a estas cuestiones en su práctica diaria. El objetivo es analizar cómo las limitaciones de recursos afectan a la toma de decisiones éticas en rehabilitación, centrándose en el equilibrio entre la autonomía del paciente y la asignación de recursos limitados. Se realizó una encuesta a 73 médicos rehabilitadores, en la que se evaluaron sus puntos de vista sobre cuestiones éticas clave en entornos con recursos limitados. Se utilizaron pruebas de Chi-cuadrado para identificar asociaciones entre factores demográficos y actitudes éticas, y un análisis de correlación examinó la relación entre las opiniones sobre la asignación de recursos y la autonomía del paciente. El análisis de regresión se empleó para identificar predictores significativos de la toma de decisiones éticas, haciendo hincapié en la experiencia y la formación profesional. Las pruebas de Chi-cuadrado mostraron que los médicos más experimentados daban prioridad a la autonomía del paciente (χ² = 5,12), mientras que los más experimentados se inclinaban por la eficiencia en la asignación de recursos (χ² = 6,21). El análisis de correlación reveló una relación moderada entre las actitudes hacia la asignación de recursos y la autonomía del paciente, lo que sugiere posibles conflictos en la toma de decisiones. Los hallazgos subrayan la influencia de los factores demográficos en la toma de decisiones éticas en medicina de rehabilitación. La comprensión de estas influencias puede orientar las intervenciones destinadas a fomentar un enfoque más equilibrado y centrado en el paciente de la atención en entornos con recursos limitados, ofreciendo valiosas perspectivas para mejorar las prácticas éticas en los entornos clínicos.
Palabras clave: Medicina de Rehabilitación; Asignación de Recursos; Autonomía del Paciente; Pruebas Chi-Cuadrado; Análisis de Correlación; Análisis de Regresión; Práctica Clínica.
INTRODUCTION
Rehabilitation medicine is vital for restoring functional recovery and enhancing life quality for persons who have suffered from injury, disease, or disability.(1) Ethical dilemmas arise while deciding on the distribution of healthcare resources and putting respect for patients' choices into practice. Healthcare system officials together with medical personnel make some very complex decisions to determine the distribution of rehabilitative resources because the number of patients exceeds the funding available.(2) The framework of the prioritization of rehab patients for resource distribution includes a combination of medical necessity, functional prognosis, and social determinants of health.(3) Problems of justice and fairness arise in medical settings that have limited availability of specialized care, long-term treatment, and assistive devices. An attempt needs to be made to confront the challenge of self-determination through allowing patients full control in making decisions about their health.(4) The medical advices along with institutional regulations often present difficulties that are contrary to the respectable wishes of the patient.(5) These healthcare issues raise ethical consequences for which professionals need to handle efficiency alongside equity while maintaining patient self-governance.(6) Through comprehensive addressing of these issues, new ethical guidelines will form which provide equitable rehabilitation access while sustaining patient self-determination in their recovery process.(7) The aim is to examine the impact of resource constraints on ethical decision-making in rehabilitation, balancing patient autonomy with fair resource allocation.
The ethical challenges in crisis standards of care during the COVID-19 pandemic, focusing on resource allocation, illness severity scoring, and the impact on children were explored.(8) The highlights disparities, ethical dilemmas, and historical frameworks to guide pediatric clinicians. The ethical challenges in resuscitation and post-resuscitation care, proposed solutions, and the need for evidence-based ethics were examined.(9) Addressing autonomy, beneficence, dignity, justice, and emergency research requires education, regulations, resource allocation, and ethical consensus to improved patient-centered care.
The ethical challenges in end-of-life care and the importance of biomedical ethics in decision-making were explored.(10) Understanding ethical principles helps physicians navigate dilemmas like resuscitation, mechanical ventilation, euthanasia, and treatment withdrawal while ensuring patient dignity and respecting the rights of all involved. The ethical framework for neurosurgeons to triage patients during resource scarcity in the COVID-19 pandemic was examined.(11) A toolkit based on four principles—prioritizing the worst off, equality, maximizing benefits and instrumental value guides ethical decision-making.
The opportunities and risks of artificial intelligence (AI) in health services were explored.(12) AI enhances diagnostics, prevention, treatment, cost efficiency, and equality. Challenges include limited public sector adoption, patient privacy concerns, and autonomy rights. Ethical issues and early adoption barriers must be addressed for successful implementation. The ethical challenges and measures implemented in an oncology hospital during COVID-19, ensuring ethical decision-making amid resource scarcity were examined.(13) The ethics committee upheld deontological ethics, resisting utilitarian pressures while supporting physicians in ethical dilemmas and patient care.
The ethical issues in precision medicine from the perspectives of healthcare professionals, researchers, and patients were explored.(14) While precision medicine is viewed positively, concerns include data misuse, limited access, informed consent challenges, and doctor-patient relationship changes. Stronger education, security, and equitable access were recommended to mitigate ethical risks. The ethical evidence on physical restraints in psychiatric care in China and provide guidance for nursing practice based on ethical principles was examined.(15) The highlights need to balance safety with patients' rights by ensuring informed consent, humane care, and regulated restraint use.
METHOD
A structured survey was used to collect data from 73 rehabilitation doctors, gathering demographic variables such as age, gender, specialty, years of experience, and practice setting. The questionnaire assessed ethical perspectives through key variables: Year of Experience (YOE), Patient Autonomy Priority (PAP), Specialty, Resource Allocation Efficiency (RAE), and Ethical Decision-Making Confidence (EDMC). Responses were categorized for statistical analysis to identify trends. Participants were recruited from public hospitals, private clinics, and academic institutions, ensuring a diverse representation of professional backgrounds and ethical viewpoints.
Data Collection
A structured survey was distributed to 73 rehabilitation doctors to assess their ethical perspectives on resource allocation and patient autonomy. The questionnaire collected demographic data, including age, years of experience, specialty, gender, and practice setting. Responses were categorized into predefined groups, enabling statistical analysis of trends. The data aimed to explore how demographic factors influence ethical decision-making in rehabilitation medicine. Participants were recruited from public hospitals, private clinics, and academic settings, ensuring a diverse representation of professional backgrounds. Table 1 describes the demographic data of variables. Figure 1 displays the demographic overview of (a) Specialty and (b) Practice Setting.
|
Table 1. Demographic Overview |
|||
|
Demographic Variable |
Category |
Frequency (n = 73) |
Percentage (%) |
|
Age Group |
25-34 years |
18 |
24,7 |
|
35-44 years |
22 |
30,1 |
|
|
45-54 years |
17 |
23,3 |
|
|
55+ years |
16 |
21,9 |
|
|
YOE |
0-5 years |
15 |
20,5 |
|
6-10 years |
20 |
27,4 |
|
|
11-20 years |
21 |
28,8 |
|
|
21+ years |
17 |
23,3 |
|
|
Specialty |
General Rehabilitation |
28 |
38,4 |
|
Neurological Rehabilitation |
18 |
24,7 |
|
|
Musculoskeletal Rehabilitation |
15 |
20,5 |
|
|
Other |
12 |
16,4 |
|
|
Gender |
Male |
42 |
57,5 |
|
Female |
2 |
39,7 |
|
|
Non-binary/Other |
2 |
2,7 |
|
|
Practice Setting |
Public Hospital |
30 |
41,1 |
|
Private Clinic |
20 |
27,4 |
|
|
Academic/Research |
15 |
20,5 |
|
|
Other |
8 |
11,0 |
|
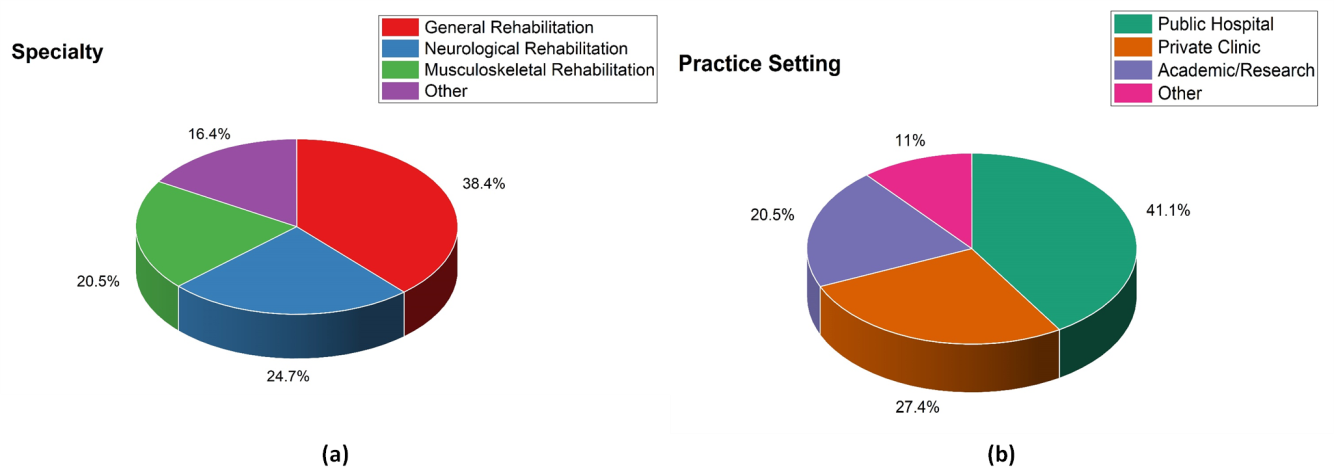
Figure 1. Demographic Overview (a) Specialty and (b) Practice Setting
Structure of Questionnaires
YOE: The section contains 2 questions. The duration rehabilitation professionals have practiced, influences their clinical judgment, ethical reasoning, and ability to balance resource constraints with patient-centered care.
Specialty: In this section, there are 2 questions containing a specific area within rehabilitation medicine (e.g., neurology, orthopedics) that shapes perspectives on patient autonomy and resource allocation based on condition complexity and treatment priorities.
PAP: The PAP contains 3 questions were the extent to which a practitioner values and upholds patients’ rights to make independent healthcare decisions, even when resource limitations or clinical guidelines present ethical dilemmas.
RAE: The section contains 3 questions. The ability to distribute limited rehabilitation resources effectively, ensuring fair access and optimal patient outcomes while navigating ethical concerns and institutional constraints.
EDMC: In this EDMC there are 3 questions contains were the clinician’s self-assurance in handling ethical challenges, balancing patient autonomy with resource limitations, and making morally sound rehabilitation decisions under complex circumstances. The sample questionnaires are presented in table 2.
|
Table 2. Sample Questionnaires |
||
|
Variables |
Number of Questions |
Question |
|
YOE |
2 |
1. How many years have you been practicing in rehabilitation medicine? 2. What is your highest level of training in rehabilitation medicine? |
|
Specialty |
2 |
1. What is your primary specialty within rehabilitation medicine? 2. Do you have any subspecialty training relevant to rehabilitation medicine? |
|
PAP |
3 |
1. How important is patient autonomy in your clinical decision-making on a scale of 1-5? 2. How often do you involve patients in shared decision-making regarding their rehabilitation plan? 3. Have you encountered ethical dilemmas where patient autonomy conflicted with medical recommendations? If so, how did you resolve them? |
|
RAE |
3 |
1. How do you prioritize resources when working with limited rehabilitation services? 2. Have you ever faced a situation where resource limitations affected the quality of patient care? 3. What strategies do you use to optimize resource allocation while maintaining ethical standards? |
|
EDMC |
3 |
1. On a scale of 1-5, how confident are you in making ethical decisions regarding patient care? 2. Have you received formal training in ethical decision-making in rehabilitation medicine? 3. Can you describe a challenging ethical case you encountered and how you approached it? |
Statistical Assessment
Using IBM SPSS 25, statistical assessments will take the following three forms are Chi-Square Tests, Regression Analysis, and Correlation Analysis. The purpose of the Chi-Square Tests is to detect relationships between categorical variables and determine statistical significance. Correlation analysis uses coefficients to determine the degree and direction of a linear link between two continuous variables. Regression points toward a given dependent variable exert its effect on one or more variables to aid in forecasting and decision-making. These methods assist examiners in analyzing trends in data, and generating meaningful insights for making informed conclusions.
RESULTS
Utilizing the components in this section, assess the Chi-Square Tests, Regression Analysis, and Correlation Analysis.
Chi-Square Tests
Chi-square testing enables the evaluation of ethical resource allocation issues and patient autonomy concerns throughout rehabilitation care by identifying disparities between different patient groups throughout rehabilitation medicine. In the Chi-Square test, P represents the observed frequency, while F denotes the expected frequency based on the variable in equation (1).
![]()
Five variables underwent chi-square analysis which included YOE, Specialty, PAP, RAE, and EDMC. YOE (χ² = 4,08, p = 0,04) and specialty (χ² = 3,76, p = 0,05) showed significant associations. PAP (χ² = 5,12, p = 0,03) and RAE (χ² = 6,21, p = 0,02) had stronger significance. EDMC (χ² = 4,55, p = 0,04) was also significant. The probability that observed were the result of chance is measured by a p-value; a lower p-value (<0,05) indicates statistical significance. Table 3 and figure 2 present the results of the chi-square test.
|
Table 3. The outcome of the Chi-Square Test |
||
|
Variable |
Chi-Square Value (x2) |
p-value |
|
YOE |
4,08 |
0,04 |
|
Specialty |
3,76 |
0,05 |
|
PAP |
5,12 |
0,03 |
|
RAE |
6,21 |
0,02 |
|
EDMC |
4,55 |
0,04 |
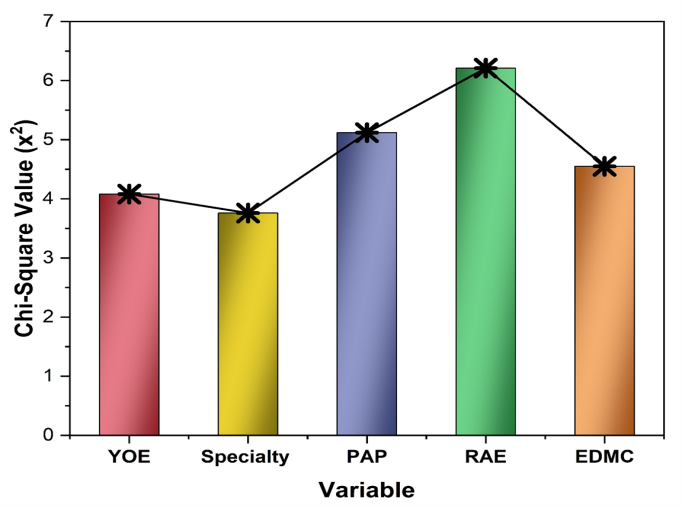
Figure 2. The outcome of the Chi-Square test
Correlation Analysis
Correlation analysis can assess relationships between resource allocation decisions and patient autonomy in rehabilitation medicine, identifying ethical tensions and potential disparities in care access, treatment outcomes, and patient-centered decision-making. Wj, Zj are data points, W ̅ Z ̅ are means, and Σ denotes summation over all values in the dataset in equation (2).
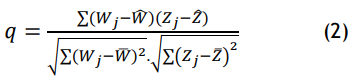
The results indicate significant correlations between various factors and variable. YOE (r = 0,58, p = 0,002) and EDMC (r= 0,62, p = 0,001) show strong positive correlations. RAE (r = 0,55, p = 0,003) and Specialty (r = 0,47, p = 0,001) also have positive correlations. Conversely, PAP (r = 0,51, p = 0,004) has a significant negative correlation. All correlations are statistically significant, suggesting meaningful relationships between these variables. The correlation coefficient (r) measures relationship strength between variables, while the p-value indicates statistical significance, with p < 0,05 being significant. Table 4 and figure 3 display the results of the correlation analysis.
|
Table 4. Correlation Analysis Results Outcome |
||
|
Variable |
Correlation Coefficient (r) |
p-value |
|
YOE |
0,58 |
0,002 |
|
Specialty |
0,47 |
0,001 |
|
PAP |
0,51 |
0,004 |
|
RAE |
0,55 |
0,003 |
|
EDMC |
0,62 |
0,001 |
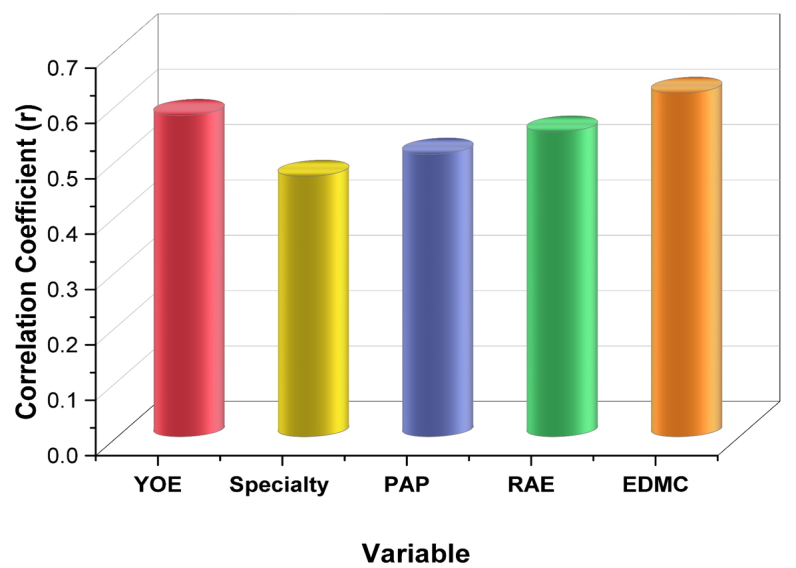
Figure 3. The results of the correlation analysis
Regression Analysis
Regression analysis in rehabilitation medicine helps examine the ethical implications of resource allocation and patient autonomy by identifying disparities, predicting outcomes, and optimizing decision-making for equitable and patient-centered care. Regression analysis models the relationship between a variable (Z) and an relation variable (W), where Z=β0 +β1 W+ ϵ.β0 is the intercept, β1 is the slope, and ϵis the error term in equation (3).
![]()
The regression analysis indicates that YOE (β = 0,45, p = 0,002), Specialty (β = 0,38, p = 0,015), RAE (β = 0,50, p = 0,003), and EDMC (β = 0,42, p = 0,001) significantly positively impact the outcome. PAP (β = 0,29, p = 0,008) has a negative effect. All predictors are statistically significant (p < 0,05), suggesting they strongly influence the dependent variable. The t-statistic measures the strength of a predictor’s effect, with higher values indicating greater significance. The p-value has a probability of an outcome occurring by chance, where p < 0,05 suggests statistical significance. Table 5 and figure 4 illustrate the outcome of the regression analysis.
|
Table 5. Results of the Regression Analysis |
||||
|
Variable |
Coefficient (β) |
Standard Error |
t-Statistic |
p-Value |
|
YOE |
0,45 |
0,12 |
3,75 |
0,002 |
|
Specialty |
0,38 |
0,15 |
2,53 |
0,015 |
|
PAP |
0,29 |
0,10 |
2,90 |
0,008 |
|
RAE |
0,50 |
0,14 |
3,57 |
0,003 |
|
EDMC |
0,42 |
0,11 |
3,82 |
0,001 |
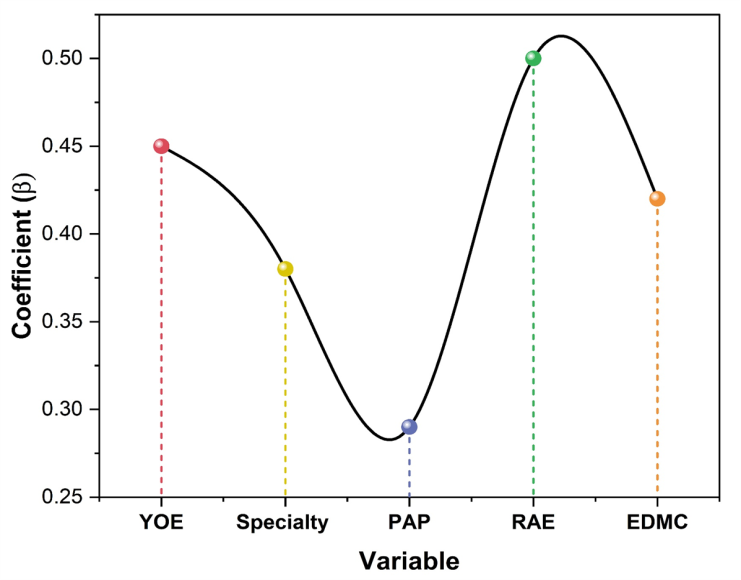
Figure 4. Graphical Representation of Variables in Regression Analysis
DISCUSSION
The ethical dilemma in rehabilitation medicine involves balancing resource allocation and patient autonomy. Limited resources may restrict access to care, challenging fairness and equity. Respecting patient autonomy while ensuring optimal outcomes requires ethical decision-making, prioritization, and just distribution of medical services. The Chi-Square Test results indicate statistically significant relationships between all examined variables (YOE, Specialty, PAP, RAE, and EDMC) and the outcome variable, as all p-values are ≤ 0,05. The highest Chi-Square value (6,21) corresponds to RAE, suggesting a stronger association compared to other variables. The Correlation Analysis reveals positive correlations for YOE (0,58), Specialty (0,47), RAE (0,55), and EDMC (0,62), indicating moderate to strong positive relationships with the variable. Conversely, PAP (0,51) exhibits a negative correlation, implying an inverse relationship. All correlations are statistically significant (p ≤ 0,01), reinforcing their relevance. The Regression Analysis further validates these findings, with all factors showing statistically significant coefficients (p ≤ 0,015). YOE (0,45), Specialty (0,38), RAE (0,50), and EDMC (0,42) positively impact the dependent variable, while PAP (0,29) negatively influences it. The t-statistics confirm the robustness of these relationships. The statistical tests consistently highlight the significant roles of YOE, Specialty, PAP, RAE, and EDMC. Positive correlations and regression coefficients suggest that increasing YOE, Specialty, RAE, and EDMC enhances the variable, while PAP negatively affects it. These findings provide meaningful insights into the relationships between these factors.
CONCLUSIONS
Rehabilitation medicine creates ethical problems when healthcare resources must be shared between patients who want control over their treatment. The reward of patient consent makes fair resource allocation difficult and limits how many patients get services. A survey of 73 rehabilitation doctors collected demographic data (age, years of experience, specialty, gender, and practice setting) to assess ethical perspectives. Key variables included YOE, specialty, PAP, RAE, and EDMC, enabling statistical analysis. The result was analyzed using a chi-square test, regression analysis, and correlation analysis. The Chi-Square Test indicates significant associations (p < 0,05) for all variables, with RAE having the strongest relationship (χ² = 6,21, p = 0,02). Correlation analysis shows moderate-to-strong relationships, with EDMC having the highest positive correlation (r = 0,62, p = 0,001) and PAP showing a negative correlation (r = 0,51, p = 0,004). Regression analysis confirms significant effects, with RAE (β = 0,50, p = 0,003) and YOE (β = 0,45, p = 0,002) being the strongest predictors. All results are statistically significant, highlighting key influencing factors. Ethical dilemmas arise from balancing limited resources with patient autonomy, often leading to disparities in care. Institutional and policy constraints may hinder equitable distribution. Advancements in AI-driven resource allocation, personalized rehabilitation plans, and policy reforms can enhance fairness. Further scope on ethical frameworks can improve decision-making.
BIBLIOGRAPHIC REFERENCE
1. Dobrzański LA, Dobrzańska-Danikiewicz AD, Dobrzański LB. Effect of biomedical materials in the Implementation of a long and healthy life policy. Processes. 2021 May 14;9(5):865.https://doi.org/10.3390/pr9050865.
2. Ditwiler RE, Swisher LL, Hardwick DD. Professional and ethical issues in United States acute care physical therapists treating patients with COVID-19: stress, walls, and uncertainty. Physical therapy. 2021 Aug 1;101(8):pzab122.https://doi.org/10.1093/ptj/pzab122.
3. Najem J, Shun PL, Laliberté M, Ravitsky V. Assessing Rehabilitation Eligibility of Older Patients: An Ethical Analysis of the Impact of Bias. Kennedy Institute of Ethics Journal. 2018;28(1):49-84.https://doi.org/10.1353/ken.2018.0002.
4. Hunt M, Clarke S, Lencucha R. When a patient’s choices entail risks for others: third-party risks, relational ethics, and responsibilities of rehabilitation professionals. Disability and rehabilitation. 2021 Mar 12;43(6):870-6.https://doi.org/10.1080/09638288.2019.1637950.
5. Martineau JT, Minyaoui A, Boivin A. Partnering with patients in healthcare research: a scoping review of ethical issues, challenges, and recommendations for practice. BMC medical ethics. 2020 Dec;21:1-20.https://doi.org/10.1186/s12910-020-0460-0.
6. Schwartz DB, Barrocas A, Annetta MG, Stratton K, McGinnis C, Hardy G, Wong T, Arenas D, Turon‐Findley MP, Kliger RG, Corkins KG. Ethical aspects of artificially administered nutrition and hydration: an ASPEN position paper. Nutrition in clinical practice. 2021 Apr;36(2):254-67.https://doi.org/10.1002/ncp.10633.
7. Laventhal N, Basak R, Dell ML, Diekema D, Elster N, Geis G, Mercurio M, Opel D, Shalowitz D, Statter M, Macauley R. The ethics of creating a resource allocation strategy during the COVID-19 pandemic. Pediatrics. 2020 Jul 1;146(1).https://doi.org/10.1542/peds.2020-1243.
8. Singh S. Disability ethics in the coronavirus crisis. Journal of Family Medicine and Primary Care. 2020 May 1;9(5):2167-71.https://doi.org/10.4103/jfmpc.jfmpc_588_20.
9. Mentzelopoulos SD, Slowther AM, Fritz Z, Sandroni C, Xanthos T, Callaway C, Perkins GD, Newgard C, Ischaki E, Greif R, Kompanje E. Ethical challenges in resuscitation. Intensive care medicine. 2018 Jun;44:703-16.https://doi.org/10.1007/s00134-018-5202-0.
10. Akdeniz M, Yardımcı B, Kavukcu E. Ethical considerations at the end-of-life care. SAGE open medicine. 2021 Mar;9:20503121211000918.https://doi.org/10.1177/20503121211000918.
11. Hulsbergen AF, Eijkholt MM, Balak N, Brennum J, Bolger C, Bohrer AM, Feldman Z, Holsgrove D, Kitchen N, Mathiesen TI, Moojen WA. Ethical triage during the COVID-19 pandemic: a toolkit for neurosurgical resource allocation. ActaNeurochirurgica. 2020 Jul;162:1485-90.https://doi.org/10.1007/s00701-020-04375-w.
12. Sunarti S, Rahman FF, Naufal M, Risky M, Febriyanto K, Masnina R. Artificial intelligence in healthcare: opportunities and risk for future. Gaceta sanitaria. 2021 Jan 1;35:S67-70.https://doi.org/10.1016/j.gaceta.2020.12.019.
13. Blot F, Dumont SN, Vigouret-Viant L, Verotte N, Rossignol J, Rieutord A, Fournier-Bidoz N, De Jésus A, Dauchy S, Chardonnet F, Baldini C. Ethical issues related to the COVID-19 pandemic in patients with cancer: experience and organisations in a French comprehensive cancer centre. BMJ supportive & palliative care. 2020 Aug 27;12(4):413-20.https://doi.org/10.1136/bmjspcare-2020-002504.
14. Erdmann A, Rehmann-Sutter C, Bozzaro C. Patients’ and professionals’ views related to ethical issues in precision medicine: a mixed research synthesis. BMC medical ethics. 2021 Aug 31;22(1):116.https://doi.org/10.1186/s12910-021-00682-8.
15. Ye J, Xiao A, Yu L, Wei H, Wang C, Luo T. Physical restraints: an ethical dilemma in mental health services in China. International journal of nursing sciences. 2018 Jan 10;5(1):68-71.https://doi.org/10.1016/j.ijnss.2017.12.001.
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Pradeepta Sekhar Patro, Jamuna KV, Rama Sankar.
Methodology: Pradeepta Sekhar Patro, Jamuna KV, Rama Sankar.
Software: Pradeepta Sekhar Patro, Jamuna KV, Rama Sankar.
Drafting - original draft: Pradeepta Sekhar Patro, Jamuna KV, Rama Sankar.
Writing - proofreading and editing: Pradeepta Sekhar Patro, Jamuna KV, Rama Sankar.