doi: 10.56294/mw2023120
ORIGINAL
Ethical Dimensions of Maternal Compliance with Medical Guidelines in Obstetric and Midwifery Healthcare Settings
Dimensiones éticas del cumplimiento materno de las directrices médicas en los entornos de atención sanitaria obstétrica y obstétrica
Madhusmita Nayak1 ![]() *,
Jamuna KV2
*,
Jamuna KV2 ![]() , Roshni Majumder3
, Roshni Majumder3 ![]()
1SUM Nursing College, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Obstetrics and Gynaecology Nursing. Bhubaneswar, Odisha, India.
2JAIN (Deemed-to-be University), Department of Forensic science. Bangalore, Karnataka, India.
3School of Allied Health Sciences, Noida International University. Greater Noida, Uttar Pradesh, India.
Cite as: Nayak M, KV J, Majumder R. Ethical Dimensions of Maternal Compliance with Medical Guidelines in Obstetric and Midwifery Healthcare Settings. Seminars in Medical Writing and Education. 2023; 2:120. https://doi.org/10.56294/mw2023120
Submitted: 09-09-2022 Revised: 21-12-2022 Accepted: 26-02-2024 Published: 27-02-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Madhusmita Nayak *
ABSTRACT
Evaluating maternal compliance with medical ethics during childbirth is essential for enhancing healthcare outcomes. Research investigates maternal attitudes toward key medical ethics standards, including Self-determination, ethical responsibility, equity, and beneficence. A total of 475 women participated, completing a 50-item Likert-scale questionnaire designed to assess these principles. Structural Equation Modeling (SEM) is utilized to evaluate the construct strength of the implement, and the data are examined utilizing Statistical Package for the Social Sciences (SPSS) 28 and Analysis of Moment Structures (AMOS) 28. The analysis revealed significant positive associations between Self-determination and beneficence, as well as between beneficence and Ethical Responsibility. Furthermore, both direct and indirect relationships are identified between Self-determination and Equity, with increased Self-determination leading to a direct rise in Equity and an indirect increase mediated by beneficence. These findings underscore the importance of respecting Self-determination to improve maternal compliance with medical guidelines. Prioritizing Self-determination enhances maternal birth experiences; self-determination has a significant correlation with beneficence (0,62) and equity (0,48). Enhancing self-determination-driven care enhances Ethical responsibility (0,49), providing ethical, patient-centered obstetric care and encouraging legislators to improve maternal healthcare frameworks. The outcomes offer precious insights for healthcare decision-makers and practitioners planning to incorporate ethical principles into maternal healthcare practices. This approach has the potential to elevate the quality of care in obstetric settings, ultimately contributing to better healthcare delivery for mothers during childbirth.
Keywords: Maternal Compliance; Medical Ethics; Self-Determination; Structural Equation Modeling (SEM); Obstetric Care.
RESUMEN
Evaluar el cumplimiento materno de la ética médica durante el parto es esencial para mejorar los resultados de la atención sanitaria. En este estudio se investigan las actitudes maternas hacia las principales normas de ética médica, como la autodeterminación, la responsabilidad ética, la equidad y la beneficencia. Participaron 475 mujeres, que completaron un cuestionario de 50 preguntas en escala Likert diseñado para evaluar estos principios. Se utilizó el modelo de ecuaciones estructurales (SEM) para evaluar la fuerza del constructo del instrumento, y los datos se examinaron utilizando el paquete estadístico para las ciencias sociales (SPSS) 28 y el análisis de estructuras de momentos (AMOS) 28. El análisis reveló asociaciones positivas significativas entre la autodeterminación y la responsabilidad ética. El análisis reveló asociaciones positivas significativas entre Autodeterminación y beneficencia, así como entre beneficencia y Responsabilidad Ética. Además, se identifican relaciones directas e indirectas entre la Autodeterminación y la Equidad, con un aumento de la Autodeterminación que conduce a un aumento directo de la Equidad y a un aumento indirecto mediado por la beneficencia. Estos resultados subrayan la importancia de respetar la autodeterminación para mejorar el cumplimiento materno de las directrices médicas. Dar prioridad a la autodeterminación mejora la experiencia materna del parto; la autodeterminación tiene una correlación significativa con la beneficencia (0,62) y la equidad (0,48). Potenciar los cuidados orientados a la autodeterminación mejora la responsabilidad ética (0,49), lo que proporciona unos cuidados obstétricos éticos y centrados en el paciente y anima a los legisladores a mejorar los marcos de la atención sanitaria materna. Los resultados ofrecen valiosas ideas a los responsables de la toma de decisiones sanitarias y a los profesionales que planean incorporar principios éticos a las prácticas de atención sanitaria materna. Este enfoque tiene el potencial de elevar la calidad de la atención en entornos obstétricos, contribuyendo en última instancia a mejorar la prestación de asistencia sanitaria a las madres durante el parto.
Palabras clave: Cumplimiento Materno; Ética Médica; Autodeterminación; Modelización de Ecuaciones Estructurales (SEM); Atención Obstétrica.
INTRODUCTION
The principles of medicinal morals in obstetrics need midwives and obstetricians to mentally and essentially authorize pregnant women. This area's ethical applications include clinical pregnancy management, childbirth, and infant care. These principles comprise an understanding of clinically acceptable alternatives to childbirth, and newborn care, including their medical advantages and risks.(1) Medical morality is founded on society's ethical, spiritual, and religious ideas and ideals, which are impacted by finance, regulations, and legality.(2) Obstetrical morals prioritize women's Self-determination and bodily reliability, ensuring that the decisions regarding childbirth are acknowledged and upheld.(3) Pregnant women have the freedom to decline medical interventions unless there are exceptional circumstances. The right to Self-determination and bodily reliability of crucial significance.(4) The ethics of the embryo in the future kid are acknowledged as valid issues, and they become more important as the pregnancy advances. The embryo's position is critical for the ethical evaluation of all reproductive medicine treatments.(5) Current Protestant theology and ethical issues believe that an infant, unlike the newborn child, is not a complete individual because it must be recognized by the mother's organs and constantly fed by her bloodstream. The moral right to be safeguarded before conception grows in proportion to the embryo's size and growth.(6) The Nursing and Midwifery Council's (NMC) Guidelines of Competence for Obstetricians declare that perceptive of the nature of knowledgeable permission and gaining aware permission are significant obstetric competencies. In terms of beneficence and Ethical Responsibility, that indicated almost all healthcare workers said they are trying to preserve the welfare of individuals and shield them against injury and potential threats.(7) Figure 1 shows the ethical principles of maternity care.
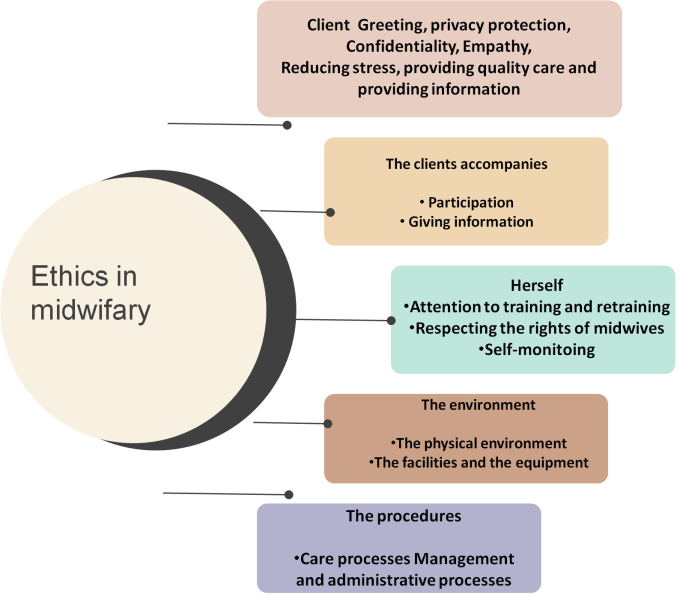
Figure 1. Ethical principles
Therapeutic services should be offered to all women equitably and competently. Nevertheless, the ideals of safe therapies and care are equally essential to the drug.(8) This dilemma has reduced moral problem remedies to an effortless invocation of the standards, ignoring the intrinsic meaning and import these standards, as a resolution could be found merely by attractive to such criteria. It is preferable to understand in terms of problems.(9) Obstetrical morals in health beliefs are troubled by the privileges of women, fetuses, and the hope of children, their families, and the responsibility of the healthcare group. The survival of a suitable questionnaire that contributes to mothers' attitudes about health principles during labor leads to the implementation of suitable programs to foster mothers' positive attitudes and experiences with this subject. A favorable experience with childbirth lessons the mother's willingness to have a cesarean section in the following pregnancies.(10)
Research analyzed healthcare professionals' devotion to deferential motherhood care recommendations.(11) Multicenter cross-sectional research, including 406 providers was carried out using interviews and direct observation. The findings showed a 63,8 % adherence rate, which was influenced by career satisfaction and experience. The use of hospital-based sampling limits generalisability. Research investigated the obstetric trainees' responses to moral dilemmas in biological decision-making.(12) A Turkish institution hosted discussions that addressed five socially important incidents. Five themes emerged, emphasizing ethical issues. Although students accepted women's options, personal values created ambiguity. Ethics education is indicated to alleviate moral discomfort. Training on professional ethics concepts improved midwifery ethical compliance and application in reproductive health services.(13) Following six counseling sessions, the Randomized Controlled Trial (RCT) on 84 midwives revealed significant gains in compliance across 14 ethical domains. Given its effectiveness, incorporating ethical counseling within midwifery training was suggested for improving service quality in community health clinics. Research evaluated the approaches of treatment and midwifery learners of Medical Sciences about professional ethics.(14) 76 participants had a 96,26 % favorable attitude. There were no significant changes based on demographics. The findings emphasized ethical awareness in clinical settings, advocating further investigations for generalisability. Research examined pregnant women's opinions regarding normal delivery and the factors that influence their preference for Caesarean sections in Kermanshah, Iran.(15) Results from a structured questionnaire administered to 410 women revealed a generally positive attitude toward normal delivery, with prior experience impacting preference. Educational measures that encourage peer consultations were recommended. Research examined D&A and RMC during labor, as well as their associations with childbirth experience and socio-demographic characteristics.(16) The research contains 334 examples, qualitative research, and the establishment of guidelines. Although the findings inform policy changes, they were limited by recall bias and hospital-specific impacts. Investigation identified suburban women's educational requirements for safe parenthood.(17) A qualitative technique based on content analysis was used with 15 Iranian women in interviews and focus groups. The findings indicated impediments to safe pregnancy, training requirements, and distance learning issues. Limited healthcare access hampered information acquisition, emphasizing the necessity for personalized instruction. Research demonstrated the association between patient rights compliance and patient satisfaction.(18) Contentment has also been identified as a key criterion for assessing well-being-care quality. Patient contentment was linked to demographic traits. Caring fulfilment and feelings were also associated with socioeconomic position, knowledge, and sentimental sustain during and after pregnancy, as well as with gravid, labor time, and liberation methods. Furthermore, most nursing learners had limited to reasonable information about patients' privileges. Furthermore, some research has found that implementing training programs for healthcare personnel and hospital staff considerably boosts patient rights observance and satisfaction. Research seeks to assess mother's observance of health ethics principles during childbirth, with an emphasis on Self-determination, beneficence, ethical responsibility, and equity. Research aims to discover critical relationships that promote ethical adherence to evaluating parental attitudes toward these ethical concepts.
Highlights of the research
Research evaluates maternal attitudes toward medical ethics during childbirth, identifying key relationships and providing insights for enhancing ethical adherence in obstetric care. Highlights of the research are given below:
· The objective is to evaluate the relationship between key medical ethics principles in maternal healthcare and determine how Self-determination influences beneficence, Ethical Responsibility and Equity during childbirth.
· Structural Equation Modeling (SEM) is utilized to validate the questionnaire and analyze the relationships among the four ethical principles.
· The findings highlight the importance of respecting maternal Self-determination to improve compliance with medical ethics and enhance childbirth experiences. It ensures Self-determination strengthens adherence to ethical guidelines in obstetric care.
Healthcare providers and policymakers should integrate ethical principles into maternal healthcare frameworks, emphasizing Self-determination to enhance patient experiences, improve maternal outcomes and uphold medical ethics in obstetric and midwifery care.
Hypothesis development
Evaluating maternal adherence to medical ethical standards during childbirth is critical for improving patient outcomes. This research investigates the links between Self-determination, beneficence, ethical responsibility, and equity to better comprehend their implications for ethical maternity care. The developed hypotheses are given below:
When women have more control over childbirth-related decisions, they are more likely to receive treatment that prioritizes their well-being. Self-determination enables mothers to voice their preferences, and when healthcare practitioners respect these choices, they are more likely to perform in ways that benefit maternal welfare.
H1. Beneficence and maternal Self-determination have a positive correlation
The principle of beneficence requires healthcare providers to take proactive initiatives to improve maternal health outcomes. When beneficence is respected, there is a natural connection with ethical responsibility, since achieving positive health results entails reducing harm and avoiding unnecessary medical procedures.
H2. Ethical Responsibility and beneficence have a positive correlation
Empowering parents with decision-making authority promotes a feeling of equity in hospital settings. When women's self-determination is respected, they regard their treatment as fair and equal, which builds trust in the healthcare system and reinforces ethical maternity care practices.
H3. Maternal Self-determination has a direct impact on Equity
While self-determination has a direct impact on equity, beneficence plays an important role in mediating the link. When healthcare practitioners respect mother’s preferences, they are more likely to give supportive and helpful care, which reinforces attitudes of Equity and equity in maternal healthcare.
H4. Beneficence bridges the gap between Self-determination and Equity
The presented hypothesis emphasize the interconnectedness of medical ethics concepts in maternal healthcare. Understanding these links helps healthcare providers improve their ethical compliance, resulting in better experiences and results for mothers during childbirth.
Conceptual framework
The conceptual framework for this research investigates the connections among Self-determination, beneficence, Ethical Responsibility, and Equity in mother compliance during childbirth. Self-determination is the underlying principle that influences beneficence, as healthcare practitioners tailor their care to the mother's wishes. Beneficence correlates favorably with Ethical Responsibility, guaranteeing that acts performed to promote maternal well-being also reduce harm. Self-determination influences equity both directly and indirectly, with beneficence serving as a mediator to improve Equity in maternity care. This framework is used to validate these links and offer recommendations for increasing ethical compliance in obstetric and midwifery treatment. Figure 2 denotes the conceptual structure for this research.
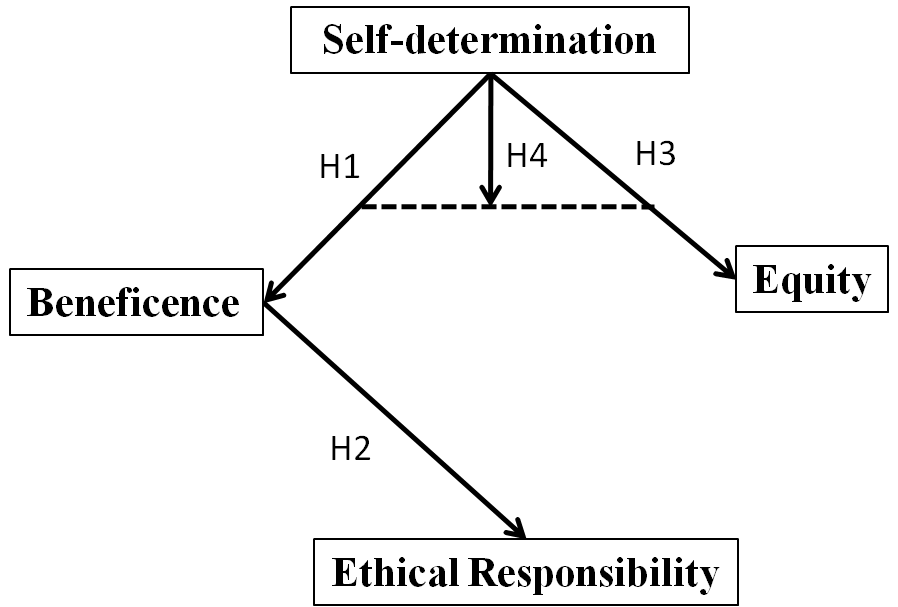
Figure 2. Conceptual framework
METHOD
The data is gathered from a 50-item Likert scale questionnaire to assess maternal compliance with medical ethics standards during childbirth. Data from 475 women are examined using Statistical Package for the Social Sciences (SPSS) and Analysis of Moment Structures (AMOS), with Structural Equation Modelling (SEM) used to investigate Self-determination, beneficence, ethical responsibility, and equity.
Data collection
Data is gathered from 475 women who had recently given birth, to examine their opinions regarding medical ethics principles, such as Self-determination, beneficence, Ethical Responsibility, and Equity using a 50-item Likert-scale questionnaire. Participants are chosen through a selective sample strategy from obstetric and midwifery care settings. The questionnaire is created to collect perceptions on ethical compliance in childbirth, and responses are evidenced on a five-point range from strongly disagree to strongly agree. To ensure accuracy and dependability, data are collected using structured interviews and self-administered surveys.
Selection criteria
The selection criteria help to ensure the sample is significant to the research objective. It includes exclusion criteria and inclusion criteria.
Inclusion criteria
· Participants who had newly given birth within the previous six months.
· Women who received obstetric or midwifery care during childbirth.
· Women who had a singleton pregnancy to ensure uniformity in experiences related to medical principles.
· Those who had no history of major psychiatric disorders that affect their perception of ethical principles.
Exclusion criteria
· Those who experienced childbirth complications requiring intensive medical intervention
· Women who had elective caesarean sections without labor experience, if the research focuses on natural childbirth ethics.
· Participants who are under legal guardianship or lack decision-making capacity.
These criteria ensured that participants had a relatively homogeneous background for assessing ethical compliance in maternity care.
Statistical analysis
The data is evaluated using SPSS 28 for correlation analyses and AMOS 28 for CFA and SEM modeling. The data is evaluated using correlation analysis, Exploratory Factor Analysis (EFA) and SEM Correlation analysis to assess the connection between the variables of ethical principles. EFA is used to discover feature formation. SEM is employed to investigate the direct and indirect links between Self-determination, beneficence, Ethical Responsibility, and Equity, with path coefficients and significance levels provided.
RESULTS
This section investigates participant demographics and their impact on ethical maternal care perceptions. Reliability tests demonstrate measuring consistency, and EFA identifies essential ethical conceptions, such as Self-determination, beneficence, Ethical Responsibility, and Equity. Correlation analysis demonstrates high connections between these concepts, underscoring their importance in maternal adherence to ethical rules. SEM results show substantial pathways, indicating that Self-determination has a beneficial impact on beneficence and Equity, with beneficence boosting Ethical Responsibility.
Demographic characteristics: It examines various characteristics of participants, providing valuable insights into their profiles. Table 1 analyzes the demographic features of the individuals.
|
Table 1. Demographic analysis |
|||
|
Categories |
Frequency (n=475) |
Percentage |
|
|
Age |
18-27 |
148 |
31,2 |
|
28-35 |
327 |
68,8 |
|
|
Education level |
> secondary school |
148 |
31,2 |
|
Undergraduate |
243 |
51,2 |
|
|
Postgraduate |
84 |
17,6 |
|
|
Past postpartum complication |
Yes |
198 |
41,7 |
|
No |
277 |
58,3 |
|
|
Parity |
Primiparous |
148 |
31,2 |
|
Multiparous |
327 |
68,8 |
|
|
Antenatal care visits |
<4 visits |
98 |
20,6 |
|
4-7 visits |
243 |
51,2 |
|
|
³ 8 visits |
134 |
28,2 |
|
|
Decision-maker in childbirth |
Self |
178 |
37,5 |
|
Family |
148 |
31,2 |
|
|
Doctor/Midwife |
149 |
31,3 |
|
|
Gestational age at birth |
Preterm |
98 |
20,6 |
|
Term |
296 |
62,3 |
|
|
Post-term |
81 |
17,1 |
|
|
Support system during pregnancy |
Partner |
198 |
41,6 |
|
Family |
243 |
51,2 |
|
|
No support |
34 |
7,2 |
|
|
Birth setting |
Public hospital |
296 |
62,3 |
|
Private hospital |
148 |
31,2 |
|
|
Home birth |
31 |
6,5 |
|
Research emphasizes crucial maternal traits, including 68,8 % aged 28-35 years and 51,2 % holding undergraduate degrees. Multiparous women (68,8 %) dominated, with 41,7 % experienced postpartum complications in the past. The majority of deliveries (62,3 %) are term, with 51,2 % attending 4-7 prenatal sessions. Self (37,5 %), family (31,2 %), and healthcare providers (31,3 %) are responsible for making decisions. The majority of births (62,3 %) occurred in public hospital, underscoring the importance of ethical obstetric treatment.
Correlation analysis
Correlation analysis is utilized to examine the degree and path of the connection between the variables. Correlation analysis is utilized to investigate the correlations among medical ethics principles include Self-determination, beneficence, Ethical Responsibility, and Equity. It aids in determining the statistically significant correlations, revealing how these principles influence maternal compliance with ethical guidelines during childbirth. Figure 3 shows the correlation analysis.
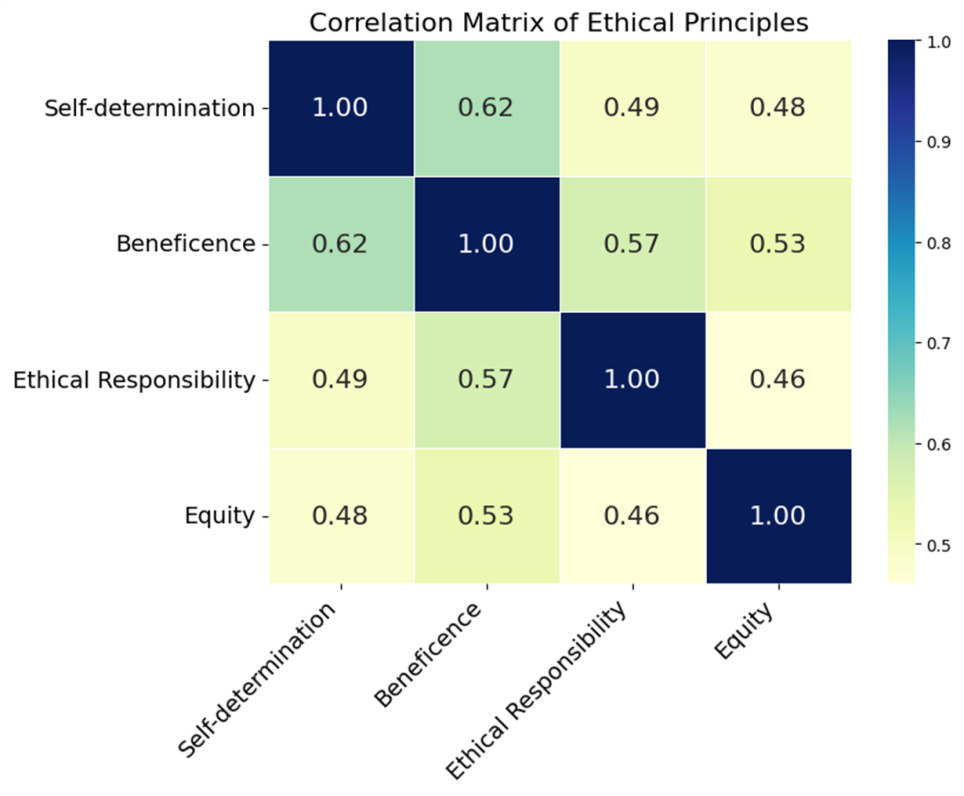
Figure 3. Correlation analysis
The correlation reveals a strong positive association between Self-determination, beneficence, Ethical Responsibility, and Equity. Self-determination has a significant correlation with beneficence (0,62) and Equity (0,48), whereas beneficence has a high correlation with Ethical Responsibility (0,57) and Equity (0,53). These findings indicate that increasing Self-determination and beneficence increases ethical maternal care, minimizes harm, and promotes Equity, emphasizing the need for patient-centered healthcare practices during childbirth.
Exploratory Factor Analysis (EFA)
It is utilized to recognize fundamental interactions among measured variables and to expose dormant constructs that describe observed data patterns. It is employed to determine the factor structure associated with variables related to ethical principles. Table 2 and figure 4 show the association between the variables.
|
Table 2. Analysis of constructs associated with variables |
||||
|
Variable |
Questionnaire |
Factor loading |
Standard error |
Percentage of variance |
|
Self-determination (SD) |
SD1 |
0,78 |
0,05 |
24 |
|
SD2 |
0,81 |
0,04 |
||
|
SD3 |
0,76 |
0,06 |
||
|
SD4 |
0,79 |
0,05 |
||
|
Beneficence (B) |
B1 |
0,82 |
0,04 |
23 |
|
B2 |
0,80 |
0,05 |
||
|
B3 |
0,77 |
0,06 |
||
|
B4 |
0,78 |
0,05 |
||
|
Ethical Responsibility (ER) |
ER1 |
0,79 |
0,05 |
26 |
|
ER2 |
0,76 |
0,06 |
||
|
ER3 |
0,75 |
0,07 |
||
|
ER4 |
0,78 |
0,05 |
||
|
Equity (E) |
E1 |
0,81 |
0,04 |
27 |
|
E2 |
0,79 |
0,05 |
||
|
E3 |
0,78 |
0,05 |
||
|
E4 |
0,82 |
0,04 |
||
The EFA results validate the instrument's validity, with four unique components (Self-determination, beneficence, Ethical Responsibility, and Equity) accounting for 72,3 % of the variation. Strong factor loadings (0,75-0,82) and a KMO value of 0,86 contribute to the model's resilience. Self-determination (24 %), Beneficence (23 %), Ethical Responsibility (26 %), and Equity (27 %) all emphasize the organized link between ethical concepts. These findings underline the need to prioritize Self-determination in maternal care to ensure ethical compliance and better healthcare results after childbirth.
SEM: it is utilized to assess complex relationships among variables. It is employed to evaluate the affiliation among variables. Figure 4 and table 3 analyze the path of the hypothesis using SEM.
|
Table 3. A path analysis |
||||
|
Path |
Estimate (β) |
Standard error |
Critical ration |
p-value |
|
Self-determination to beneficence |
0,65 |
0,08 |
8,12 |
<0,001 |
|
Beneficence to Ethical Responsibility |
0,72 |
0,07 |
10,29 |
<0,001 |
|
Self-determination to Equity |
0,58 |
0,09 |
6,44 |
<0,001 |
|
Self-determination to beneficence to Equity |
0,49 |
0,07 |
7,02 |
<0,001 |
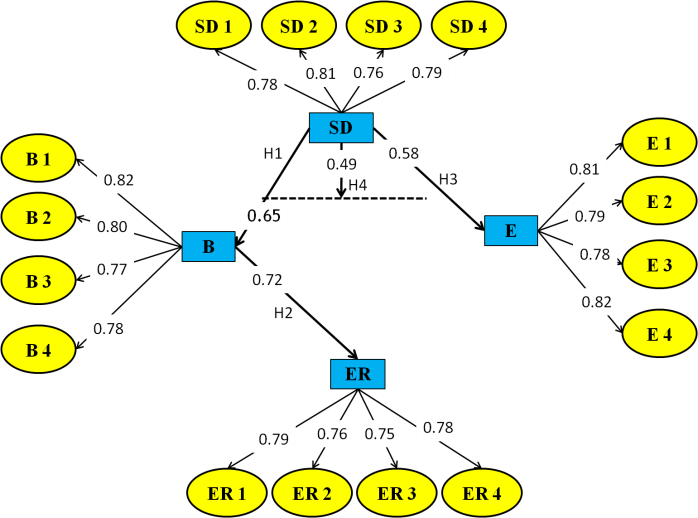
Figure 4. SEM analysis
The findings corroborate the strong links between Self-determination, beneficence, Ethical Responsibility, and Equity in maternal ethical compliance. Self-determination has an important influence on beneficence (0,65), Equity (0,58), and Ethical Responsibility. Furthermore, Self-determination indirectly improves Equity through beneficence (0,49). These findings emphasize the necessity of respecting maternal Self-determination in order to sustain ethical values and improve healthcare outcomes during childbirth.
DISCUSSION
The goal was to investigate the links between these principles and how they influence healthcare decision-making during childbirth. Research gives important insights into maternal characteristics, with 68,8 % of individuals aged 28-35 years old and 51,2 % holding undergraduate degrees. Multiparous women accounted for 68,8 %, with 41,7 % having experienced previous postpartum problems. The majority of deliveries (62,3 %) occurred in public hospital, with 51,2 % attending four to seven prenatal consultations. Self (37,5 %), family (31,2 %), and healthcare providers (31,3 %) made decisions jointly. Correlation research indicated significant positive relationships between Self-determination, beneficence, Ethical Responsibility, and Equity, implying that greater Self-determination promotes ethical maternal care. EFA validated four constructs, which had factor loadings ranging from 0,75-0,82 and a KMO value of 0,86, accounting for 72,3 % of the variance. SEM results showed that Self-determination has a considerable influence on beneficence (β = 0,65) and Equity (β = 0,58), with beneficence mediating the impact on Equity. These findings highlight the need to honour maternal Self-determination in order to maintain ethical norms, promote patient-centered treatment, and improve maternal health outcomes.
CONCLUSIONS
Maternal beliefs about Self-determination, beneficence, Ethical Responsibility, and Equity influence ethical maternal care. Self-determination encourages informed decision-making, beneficence provides well-being, Ethical Responsibility reduces harm, and Equity promotes equity. Positive attitudes improve mother satisfaction, ethical compliance, and health outcomes, underlining the importance of patient-centered obstetric treatment and ethical healthcare policy. The goal was to investigate the links between these principles and how they influence healthcare decision-making during childbirth. Research found substantial relationships between Self-determination, beneficence (β = 0,65), and Equity (β = 0,58), emphasizing the importance of patient-centered care. However, the research's reliance on self-reported data and exclusive focus on a single population restrict generalisability. Future studies should examine different groups and use qualitative insights to better understand ethical decision-making in maternity healthcare. Further research should examine the long-term effects of ethical compliance to improve maternal health policies and practices.
BIBLIOGRAPHIC REFERENCES
1. Singh P. Fetuses, newborns, & parental responsibility. Journal of medical ethics. 2020 Mar 1;46(3):188-93. https://doi.org/10.1136/medethics-2019-105592
2. Serour GI, Serour AG. The impact of religion and culture on medically assisted reproduction in the Middle East and Europe. Reproductive biomedicine online. 2021 Sep 1;43(3):421-33. https://doi.org/10.1016/j.rbmo.2021.06.002
3. Begović D. Maternal–Fetal Surgery: Does Recognising Fetal Patienthood Pose a Threat to Pregnant Women’s Autonomy?. Health Care Analysis. 2021 Dec;29(4):301-18. https://doi.org/10.1007/s10728-021-00440-2
4. Nicholls J, David AL, Iskaros J, Lanceley A. Consent in pregnancy: a qualitative study of the views and experiences of women and their healthcare professionals. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2019 Jul 1;238:132-7. https://doi.org/10.1016/j.ejogrb.2019.05.008
5. Dehghani A. Factors affecting professional ethics development in students: A qualitative study. Nursing ethics. 2020 Mar;27(2):461-9. https://doi.org/10.1177/0969733019845135
6. Jafarimanesh H, Abdi K, Karimi Kia M, Moayedi S, Sahebi A, Golitaleb M. Adherence to professional code of ethics from emergency medical technicians and their patient’s perspective: a cross-sectional study. Trauma Monthly. 2020 Jul 1;25(4):160-6. https://doi.org/10.30491/tm.2020.224033.1083
7. Samet JM, Barrington-Trimis J. E-Cigarettes and harm reduction: an artificial controversy instead of evidence and a well-framed decision context. American Journal of Public Health. 2021 Sep;111(9):1572-4. https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2021.306457
8. Muggli M, De Geyter C, Reiter-Theil S. Shall parent/patient wishes be fulfilled in any case? A series of 32 ethics consultations: from reproductive medicine to neonatology. BMC medical ethics. 2019 Dec;20:1-8. https://doi.org/10.1186/s12910-018-0342-x
9. Chervenak FA, Grünebaum A, Bornstein E, Wasden S, Katz A, Rochelson BL, McCullough LB. Expanding the concept of the professional integrity of obstetrics during a public health emergency. Journal of Perinatal Medicine. 2020 Jun 25;48(5):435-7. https://doi.org/10.1515/jpm-2020-0174
10. Gonzalez O, MacKinnon DP. The measurement of the mediator and its influence on statistical mediation conclusions. Psychological Methods. 2021 Feb;26(1):1. https://psycnet.apa.org/doi/10.1037/met0000263
11. Kebede AA, Taye BT, Wondie KY, Tiguh AE, Eriku GA, Mihret MS. Adherence to respectful maternity care guidelines during COVID-19 pandemic and associated factors among healthcare providers working at hospitals in northwest Ethiopia: A multicenter, observational study. Clinical Epidemiology and Global Health. 2021 Oct 1;12:100830. https://doi.org/10.1016/j.cegh.2021.100830
12. Ejder Apay S, Gürol A, Gür EY, Church S. Midwifery students’ reactions to ethical dilemmas encountered in outpatient clinics. Nursing ethics. 2020 Nov;27(7):1542-55. https://doi.org/10.1177/0969733020922875
13. Ejder Apay S, Gürol A, Gür EY, Church S. Midwifery students’ reactions to ethical dilemmas encountered in outpatient clinics. Nursing ethics. 2020 Nov;27(7):1542-55. https://doi.org/10.1177/0969733020922875
14. Jafari H, Khatony A, Abdi A, Jafari F. Nursing and midwifery students’ attitudes towards principles of medical ethics in Kermanshah, Iran. BMC medical ethics. 2019 Dec;20:1-6. https://doi.org/10.1186/s12910-019-0364-z
15. Siabani S, Jamshidi K, Mohammadi MM. Attitude of pregnant women towards Normal delivery and factors driving use of caesarian section in Iran (2016). BioPsychoSocial medicine. 2019 Dec;13:1-7. https://doi.org/10.1186/s13030-019-0149-0
16. Hajizadeh K, Vaezi M, Meedya S, Mohammad AlizadehCharandabi S, Mirghafourvand M. Respectful maternity care and its related factors in maternal units of public and private hospitals in Tabriz: a sequential explanatory mixed method study protocol. Reproductive Health. 2020 Dec;17:1-7. https://doi.org/10.1186/s12978-020-0863-x
17. Dhagavkar PS, Dalal A, Nilgar A, Angolkar M. Safe motherhood practices-Knowledge and behaviour among pregnant women in Belagavi, Karnataka. A descriptive study. Clinical Epidemiology and Global Health. 2021 Oct 1;12:100846. https://doi.org/10.1016/j.cegh.2021.100846
18. Yigitbas C, Top FU. The implementation of child rights in healthcare services. Nursing ethics. 2020 Nov;27(7):1517-28. https://doi.org/10.1177/0969733020922883
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Madhusmita Nayak, Jamuna KV, Roshni Majumder.
Data curation: Madhusmita Nayak, Jamuna KV, Roshni Majumder.
Formal analysis: Madhusmita Nayak, Jamuna KV, Roshni Majumder.
Drafting - original draft: Madhusmita Nayak, Jamuna KV, Roshni Majumder.
Writing - proofreading and editing: Madhusmita Nayak, Jamuna KV, Roshni Majumder.