doi: 10.56294/mw2023121
ORIGINAL
Ethical Considerations in Critical Care Nursing and Their Impact on Professional Conduct in Intensive Care Units
Consideraciones éticas en enfermería de cuidados críticos y su impacto en la conducta profesional en las unidades de cuidados intensivos
Sachet Dawar1 ![]() *, Ritarani Nayak2
*, Ritarani Nayak2 ![]() , RenukaJyothi S3
, RenukaJyothi S3 ![]()
1Noida International University, Department of Medicine. Greater Noida, Uttar Pradesh, India.
2SUM Nursing College, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Mental Health Nursing. Bhubaneswar, Odisha, India.
3JAIN (Deemed-to-be University), Department of Biotechnology and Genetics. Bangalore, Karnataka, India.
Cite as: Dawar S, Nayak R, S RJ. Ethical Considerations in Critical Care Nursing and Their Impact on Professional Conduct in Intensive Care Units. Seminars in Medical Writing and Education. 2023; 2:121. https://doi.org/10.56294/mw2023121
Submitted: 10-09-2022 Revised: 22-12-2022 Accepted: 26-02-2023 Published: 27-02-2023
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Sachet Dawar *
ABSTRACT
Making moral decisions is a crucial part of nursing practice since intensive care units (ICUs) commonly provides moral conundrums pertaining to patient autonomy, informed consent, and resource allocation. Critical care nursing requires intricate decision-making in high-pressure environments in shaping patient care and professional conduct. Despite their importance in ICUs, ethical considerations often cause moral distress and uncertainty for nurses. The absence of standardized training and institutional support leads to inconsistencies in professional conduct, affecting patient care quality and teamwork. Research involved ICU nurses from multiple hospitals, with a sample size of 150 participants selected through stratified random sampling. Both descriptive and inferential statistical analysis were performed, such as logistic regression models to examine the impact of ethical training on critical care decision-making and chi-square tests to investigate associations between professional behaviour and ethical awareness. The findings revealed a significant correlation between ethical awareness and professional conduct, with nurses who received formal ethical training demonstrating higher adherence to ethical principles. Ethical challenges related to appropriate care and resource allocation were the most frequently reported dilemmas. Additionally, nurses with institutional support and ethical guidelines exhibited lower levels of moral distress and improved interdisciplinary collaboration. Resolving these moral dilemmas improves decision-making, lessens moral suffering, and creates a more moral and professional intensive care unit, all of which contribute to better patient care.
Keywords: Intensive Care Units (ICU); Ethical Considerations; Critical Care Nursing; Professional Conduct.
RESUMEN
La toma de decisiones morales es una parte crucial de la práctica enfermera, ya que las unidades de cuidados intensivos (UCI) suelen plantear dilemas morales relacionados con la autonomía del paciente, el consentimiento informado y la asignación de recursos. La enfermería de cuidados intensivos requiere una toma de decisiones compleja en entornos de alta presión para dar forma a la atención al paciente y a la conducta profesional. A pesar de su importancia en las UCI, las consideraciones éticas a menudo causan angustia moral e incertidumbre a las enfermeras. La ausencia de una formación estandarizada y de apoyo institucional provoca incoherencias en la conducta profesional, lo que afecta a la calidad de la atención al paciente y al trabajo en equipo. En la investigación participaron enfermeras de UCI de varios hospitales, con una muestra de 150 participantes seleccionadas mediante muestreo aleatorio estratificado. Se realizaron análisis estadísticos descriptivos e inferenciales, como modelos de regresión logística para examinar el impacto de la formación ética en la toma de decisiones en cuidados críticos y pruebas de chi-cuadrado para investigar las asociaciones entre el comportamiento profesional y la conciencia ética. Los resultados revelaron una correlación significativa entre la conciencia ética y la conducta profesional, y las enfermeras que recibieron formación ética formal demostraron una mayor adhesión a los principios éticos. Los dilemas éticos más frecuentes fueron los relacionados con los cuidados adecuados y la asignación de recursos. Además, las enfermeras con apoyo institucional y directrices éticas mostraron niveles más bajos de angustia moral y una mejor colaboración interdisciplinar. La resolución de estos dilemas morales mejora la toma de decisiones, disminuye el sufrimiento moral y crea una unidad de cuidados intensivos más moral y profesional, todo lo cual contribuye a mejorar la atención al paciente.
Palabras clave: Unidades de Cuidados Intensivos (UCI); Consideraciones Éticas; Enfermería de Cuidados Críticos; Conducta Profesional.
INTRODUCTION
The needs of nursing and healthcare have increased in recent years, particularly during the pandemic. More individuals need critical care as a result of the epidemic. Critically sick patients were putting increased strain on nurses in Intensive Care Units (ICUs). Nurses experienced ethical stress as a result of an increased workload and a worsening work environment. The primary way that patient safety and care quality were jeopardized was regarded as an ethical concern.(1) Several hundred nurses have died from COVID-19, and the virus's consequences on nurses' health and wellbeing have also drawn attention. In the midst of the global pandemic, nurses are tackling the most challenging ethical conundrums of the moment.(2)
Critical care nurses took on a significant amount of responsibility for patients who were in critical condition, particularly during the COVID-19 pandemic. Their training with expertise was the cause of this. Responding to moral distress has a negative emotional impact on healthcare workers, which affects patient care.(3) Many nurses in critical care are thinking about quitting their current jobs due to moral discomfort. The professional code of conduct that directs nurses in their everyday work and helps them decide what is right and wrong in certain clinical settings is known as ethics. When someone asks themselves what they should and shouldn't do, or what constitutes appropriate behavior and action, they are posing an ethical dilemma.(4)
Ethical problems are stressful, have detrimental effects, and have the potential to lower the caliber and moral standards of the nursing profession. Compared to nurses in other clinical practice areas, ICU nurses are more likely to encounter ethical dilemmas. The ability to comprehend ethical concerns more deeply enables nurses to identify circumstances in their day-to-day clinical practice.(5) Being able to solve ethical problems and having ethical competence are regarded as essential skills for a professional nurse. The ability to handle ethical dilemmas and behaviors is correlated with moral well-being. The ability of nurses to make moral decisions can impact patients' recuperation and lower medical expenses.(6)
Nursing ethics is the field that analyzes the moral implications of nursing practice. This subfield of healthcare ethics is sometimes called bioethics. The three primary facets of nursing ethics are outlining the ethical components of nursing, developing ethical guidelines, and prescribing ethical norms. Understanding ethical and unethical nursing practice is guided by empirical research in the field of nursing ethics. The fundamental ideas that nurses need to comprehend ethical notions are provided by philosophical nursing ethics. Adopting and comprehending a critical attitude to ethical frameworks directed by regulatory bodies and experts constitutes the third aspect of nursing ethics.(7)
The ethical functions that nurse carry on with care give rise to ethical conflict, which impedes the decision-making process. Nurses working in ICUs could encounter this occurrence. A thorough investigation of the phenomena can aid in its treatment and prevention. The purpose of this investigation was to determine the prevalence, seriousness, level of revelation, and kind of ethical issues among nurses employed in intensive care units.(8)
To improve the quality of treatment and reduce ethical suffering among nurses, this analysis sought to provide hospital administrators, nursing directors, and nursing schools with a moral empowerment program.(9) According to this analysis, moral empowerment programs have been successful in lowering the average moral distress score. Thus, it is advised that hospital administrators and nursing management put in place an empowerment program to lessen nurses' moral suffering and raise the standard of care.
Investigation presents the findings of descriptive research conducted with nurses who work in hospital ICUs.(10) Data was gathered using a personal information form and the Moral Sensitivity Questionnaire, which were created by researchers in compliance with the pertinent literature. The findings showed that ethical dilemmas are common for intensive care nurses and that moral awareness was necessary to help them deal with them. When compared to nurses who were unhappy with their jobs, it was found that those who were extremely happy with their jobs were more sensitive to ethical issues.
The research evaluated critical care nurses' communication experiences, with consideration for patients in the ICU.(11) Three themes emerged from nurses' communication experiences: overcoming unforeseen communication obstacles, learning from mistakes, and realizing that communication was crucial to patient care. Nurses understood the importance of using communication to deliver high-quality healthcare.
The connections between a nationwide sample of critical care nurses' levels of ethical suffering, their patient security and their clinical environments, were examined.(12) Negative opinions of the clinical setting and patient safety were slightly associated to moral discomfort. Age, practice setting, and job satisfaction were all statistically significant predictors of ethical discomfort in this population.
The purpose of this examination was to define and investigate the causes of ethical suffering in the ICU, with a focus on ethically challenging circumstances such as pre-viable resuscitation and end-of-life care.(13) It examined that ethical suffering affects decision-making and the provision of treatment and that different healthcare workers perceive it differently. The research also emphasized that moral anguish was shaped by team dynamics, parental discretion, and collaborative decision-making.
The determination of this research investigated that moral anguish and perceived organizational fairness relate to ICU nurses.(14) The results of the investigation demonstrated a strong negative correlation between perceived organizational justice and moral anguish; consequently, head nurses are supposed to assist nurses in feeling less morally distressed and more connected to the organization.
Research two primary objectives were to (I) assess that formalizing nurses' participation in rounds through an interdisciplinary rounding format affected the efficacy of interprofessional cooperation, particularly with nurses and physicians; and (II) assess whether adopting these rounds could affect quantifiable patient care outcomes.(15) Its conclusions reinforce the mounting data, showing that interdisciplinary rounds enhance teamwork and raise the typical of patient care.
Compared to nurses employed in other hospital departments, critical care nurses are subjected to elevated levels of emotional, bodily, and occupational stress. The purpose of this investigation was to ascertain that resilience training affected the extent of resilience and stress while employed of the ICU nurses.(16)
To assess how ethical awareness affects ICU nurses' professional behavior was the main purpose of this research. It proposes to evaluate that ethical training enhances nurses' ability to make decisions, uphold moral standards, and collaborate across disciplines. It establishes that nursing practice is impacted by ethical dilemmas that commonly occur in critical care settings, such as resource allocation and end-of-life care. It also examines that institutional support could improve ethical competency and lessen moral discomfort.
METHOD
Key ethical challenges in ICU, such as Informed consent, resource allocation, patient autonomy, and the final stages of life, were the focus of this research, which used a pre-and post-assessment design to evaluate the impression of ethical awareness training on ICU nurses across three hospitals. Data were gathered using the Ethical Awareness Scale (EAS) to assess nurses' knowledge, confidence, and adherence to ethical principles.
Data collection
ICU nurses from three separate hospitals provided the data for this research, ensuring a varied representation of experiences and moral dilemmas in critical care environments. Stratified random sampling was used to choose 150 participants to ensure equitable representation throughout hospitals and nursing experience categories. An overview of the attributes of ICU nurses, such as gender, age, work experience, hospital type, and ICU sections, is presented in table 1. It emphasizes attention to the distribution of nurses in different ICUs and public and private hospitals. The percentage of nurses with previous ethical training is also shown, along with typical ethical dilemmas encountered in critical care environments. These revelations aid in comprehending the ethical environment of ICU nursing and that it affects professional behavior.
|
Table 1. ICU nurses' demographic characteristics |
||
|
Variables |
Categories |
Participants (n=150) |
|
Gender |
Male |
45 (30 %) |
|
Female |
105 (70 %) |
|
|
Age group |
20-30 |
60 (40 %) |
|
31-35 |
50 (33,3 %) |
|
|
36-39 |
40 (26,7 %) |
|
|
Work experience |
<5 years |
40 (26,7 %) |
|
5-10 years |
55 (36,7 %) |
|
|
11-15 years |
55 (36,6 %) |
|
|
ICU section |
Medical ICU (MICU) |
50 (33,3 %) |
|
Surgical ICU (SICU) |
40 (26,7 %) |
|
|
Pediatric ICU (PICU) |
25 (16,7 %) |
|
|
Neonatal ICU (NICU) |
20 (13,3 %) |
|
|
Cardiac ICU (CICU) |
15 (10 %) |
|
|
No. of hospitals |
Hospital 1 (H1) |
60 (40 %) |
|
Hospital 2 (H2) |
50 (33,3 %) |
|
|
Hospital 3 (H3) |
40 (26,7 %) |
|
|
Exposure to Ethical training |
Yes |
100 (66,6 %) |
|
No |
50 (33,3 %) |
|
|
Common Ethical challenges faced |
End-of-life-care |
30 (20 %) |
|
Patient autonomy |
40 (26,7 %) |
|
|
Resource allocation |
45 (30 %) |
|
|
Informed consent |
35 (23,3 %) |
|
Selection Criteria
The selection criteria ensured that only registered ICU nurses with direct patient care duties and at least 1 year of experience were included. The research was exposed to nurses who agreed to participate from both public and private institutions. Those who were working in non-ICU roles, temporarily assigned, or unable to participate in assessments were excluded (figure 1).
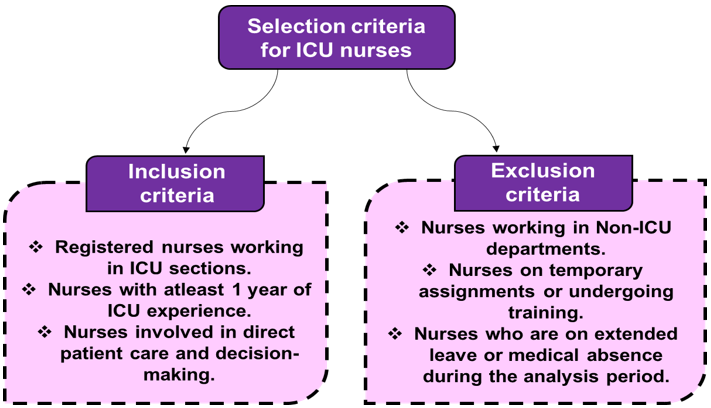
Figure 1. Criteria for ICU nurses
Critical Care Nursing's Application of the Ethical Awareness Scale (EAS)
Nurses undergo evaluation of their ethical principal practice understanding and implementation skills through the standardized EAS assessment scale. This evaluation tool examines four vital areas, which include resource management, patient self-determination and ethical decision-making as well as professional ethics standards. The Likert-type items measure nurse responses through agreement frequency and observation frequency of ethical situations. Both pre and post-assessments of ethical awareness changes used the EAS to measure results. EAS served as the research tool to track ethical awareness levels in nurses, identify their knowledge deficiencies and test how nursing practice changed after ethical training in ICUs.
Training and Assessment for Ethical Awareness
A description appears regarding the assessment procedures applied to ICU nurses during pre-test and post-test alongside their ethical awareness instruction. The research focuses on the organized training program together with evaluations of ethical concepts and the behavioral and judgmental changes that result from training in critical care teams.
Pre-Assessment of Ethical Awareness in ICU Nurses
A pre-assessment evaluated ICU nurses regarding their current knowledge base together with their ethical frameworks and their choices when facing critical care ethical dilemmas. The participants underwent EAS testing to validate their ethical concept understanding together with their problem-solving abilities and assurances about moral decisions. The assessment targeted essential ethical matters, including end-of-life care with patient autonomy along with resource distribution and informed consent and evaluated nurses operating in different ICU environments and hospital facilities. The results from the assessment created the basis for recognizing professional conduct and ethical knowledge deficiencies that training sessions helped address systematically.
Training in Ethical Awareness for ICU Nurses
The main objective of the ethical awareness program was to improve ICU nurses' understanding of critical care ethics together with their actions and professional standards. Through real healthcare situations combined with live dialogue sessions, the course addressed significant elements, which included patient self-determination together with voluntary permission granting as well as end-of-life care and medical resource distribution. The presentation of ethical frameworks to nurses was intended to increase their abilities to address tough moral decisions. The seminars provided essential guidance on how nurses should handle ethical dilemmas, reduce their ethical discomfort and build solid professional relationships between fields. The nurses acquired improved ethical knowledge and practical moral decision-making expertise for ICU environments through this training.
Post-Assessment of Professional Conduct and Ethical Awareness
The post-assessment evaluated whether the ethical awareness training programs changed ICU nurses' ethical decision-making while also affecting their professional behavior. The assessment evaluated three dimensions of nursing practice using the EAS: ethical concept knowledge, ethical situation resolution ability, and ethical rule compliance. The evaluation used three assessment methods, which included self-assessments of ethical confidence measures alongside direct observations of clinicians' behaviors in real situations combined with ethical scenarios that applied to diverse situations. The results obtained ethical competency improvements as well as interdisciplinary teamwork growth through assessment comparisons between pre-education tests and post-education tests. The results helped evaluate that ethical training improves intensive care patient care while decreasing moral suffering.
Statistical analysis
The evaluation of ethical awareness training effects on ICU nurse professional conduct and decision-making was preceded through SPSS version 27 data analysis. They conducted a chi-square analysis to understand whether nurses demonstrated better ethical conduct and displayed greater ethical knowledge. Logistic regression models revealed the main factors affecting ethical competence through the evaluation of ethical training outcomes on critical care decision-making by nurses. The research based its findings on paired t-tests, which examined the statistical significance of ethical perception changes, enhanced professional competence and enhanced teamwork after residency programs. The research confirmed that ICU practitioner ethical training effectively enhances professional conduct. Research evaluators examined changes in pre- and post assessment ratings to determine training effects on participant interdisciplinary cooperation, confidence, and ethical awareness.
RESULTS AND DISCUSSION
Ethical training programs produced substantial improvements in ICU nursing professional standards as all survey metrics obtained higher scores following implementation. Nurses gained better capabilities to deal with ethical situations involving patient autonomy and end-of-life care and demonstrated increased self-assurance about their moral judgments and ethical practice.
Chi-Square Test Analysis of the Effects of Ethical Awareness Training on ICU Nurses
The Chi-Square technique examined the relationship between the professional conduct of ICU nurses at three hospitals with their ethical awareness training (H1, H2, and H3). Measures of interdisciplinary collaboration, ethical awareness, decision-making confidence, and ethical principal adherence were provided by the assessment both before and after the training time. Results from table 2 and figure 2 reveal statistical significance through p-values below 0,001 for all variables after ethical training, indicating its effectiveness on nurse behavior. After receiving training, nurses developed improved teamwork skills and felt more capable when handling ethical issues while demonstrating increased dedication to ethical standards. The organized ethical training showed effectiveness through progressive increases in post-assessment results compared to pre-assessment results. Nurses who receive professional training demonstrate both high levels of ethical awareness and professional conduct in ICUs according to assessment results.
|
Table 2. Analysis of ICU nurses' professional conduct and ethical awareness |
|||||||
|
Variable |
Hospital |
Pre-assessment score (%) |
Post-assessment score (%) |
X2 value |
df |
p-value |
Significance |
|
Ethical awareness |
H1 |
54,6 |
86,3 |
41,87 |
1 |
<0,001 |
Significant |
|
H2 |
51,2 |
83,8 |
39,42 |
1 |
<0,001 |
Significant |
|
|
H3 |
52,9 |
85,4 |
40,78 |
1 |
<0,001 |
Significant |
|
|
Adherence to Ethical guidelines |
H1 |
49,5 |
82,7 |
44,21 |
1 |
<0,001 |
Significant |
|
H2 |
47,3 |
81,1 |
42,38 |
1 |
<0,001 |
Significant |
|
|
H3 |
48,6 |
83,2 |
43,89 |
1 |
<0,001 |
Significant |
|
|
Confidence in Ethical decision-making |
H1 |
50,8 |
87,1 |
47,53 |
1 |
<0,001 |
Significant |
|
H2 |
48,6 |
84,2 |
45,12 |
1 |
<0,001 |
Significant |
|
|
H3 |
49,9 |
85,9 |
46,75 |
1 |
<0,001 |
Significant |
|
|
Interdisciplinary collaboration |
H1 |
52,7 |
88,5 |
51,64 |
1 |
<0,001 |
Significant |
|
H2 |
50,9 |
86,4 |
48,73 |
1 |
<0,001 |
Significant |
|
|
H3 |
52,1 |
87,8 |
50,21 |
1 |
<0,001 |
Significant |
|
|
Ethical conflict resolution skills |
H1 |
48,3 |
85,2 |
46,89 |
1 |
<0,001 |
Significant |
|
H2 |
46,1 |
82,9 |
44,76 |
1 |
<0,001 |
Significant |
|
|
H3 |
47,4 |
84,5 |
45,98 |
1 |
<0,001 |
Significant |
|
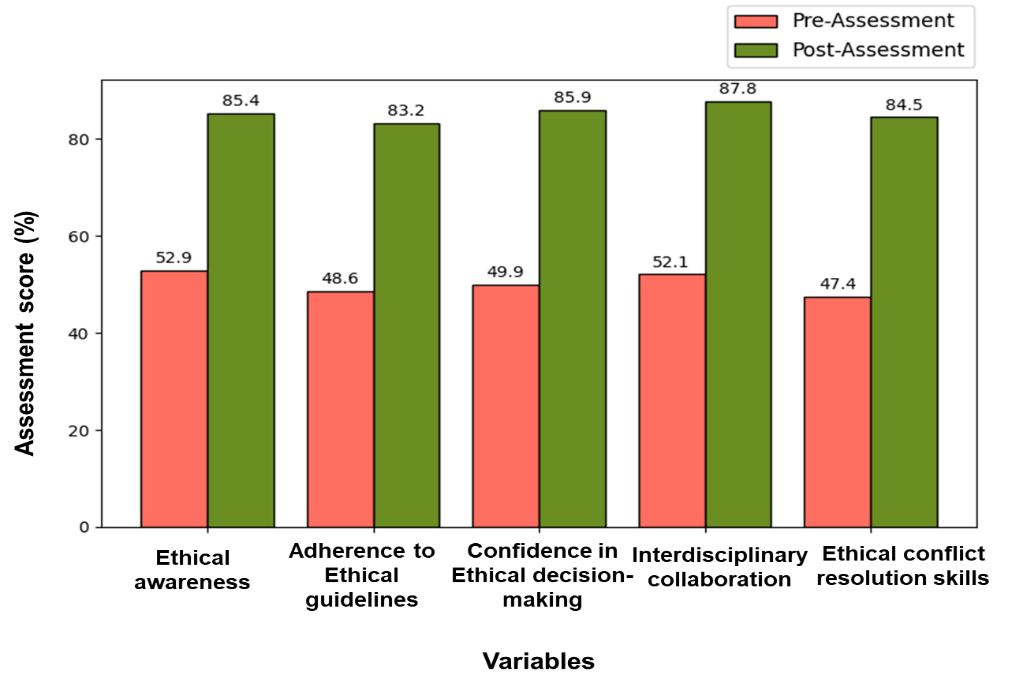
Figure 2. Comparison of pre-and post-assessment scores for ICU nurses
A Logistic Regression Analysis of the Impact of Ethical Training on Nurses' Ethical Decision-Making
The effect of ethical training on ICU nurses' capacity to manage moral dilemmas was assessed using logistic regression analysis. With a high Exp(B) = 6,36 (p < 0,001), the model demonstrated that ethical training had a considerable impact on professional conduct, showing that trained nurses were more than six times more likely to follow ethical rules (table 3 and figure 3). Additionally, the analysis revealed that, in contrast to lower pre-assessment scores, post-assessment ratings improved significantly across all ethical issues, surpassing 80 %. This suggests that nurses' capacity to handle moral conundrums was enhanced by ethical training. The results showed that professional behavior and ethical awareness were strongly correlated, with trained nurses exhibiting superior ethical decision-making and adherence to ethical norms. Increased ethical competency reinforces the value of organized ethical training programs in ICUs by lowering moral anguish and improving patient care.
|
Table 3. Evaluation of the Effects of Ethical Training on ICU Nurses |
|||||
|
Variable |
Ethical Training |
End-of-Life Care Challenges |
Patient Autonomy Issues |
Resource Allocation Concerns |
Informed Consent Challenges |
|
Responses |
Yes vs. No |
Handled Well vs. Poorly |
Respected vs. Overlooked |
Fairly Managed vs. Unfairly |
Properly Obtained vs. Lacking |
|
Beta coefficient (B) |
1,85 |
1,72 |
1,65 |
1,59 |
-1,24 |
|
Standard error (SE) |
0,42 |
0,38 |
0,35 |
0,33 |
0,40 |
|
Wald χ² |
19,48 |
20,91 |
22,32 |
21,78 |
9,56 |
|
df |
1 |
1 |
1 |
1 |
1 |
|
p-value |
<0,001 |
<0,001 |
<0,001 |
<0,001 |
0,002 |
|
Exponentiated Beta (Exp (B)) |
6,36 |
5,58 |
5,21 |
4,90 |
0,29 |
|
Pre-Assessment (%) |
52,4 |
60,3 |
58,2 |
56,7 |
46,7 |
|
Post-Assessment (%) |
85,2 |
83,8 |
85,1 |
82,9 |
81,4 |
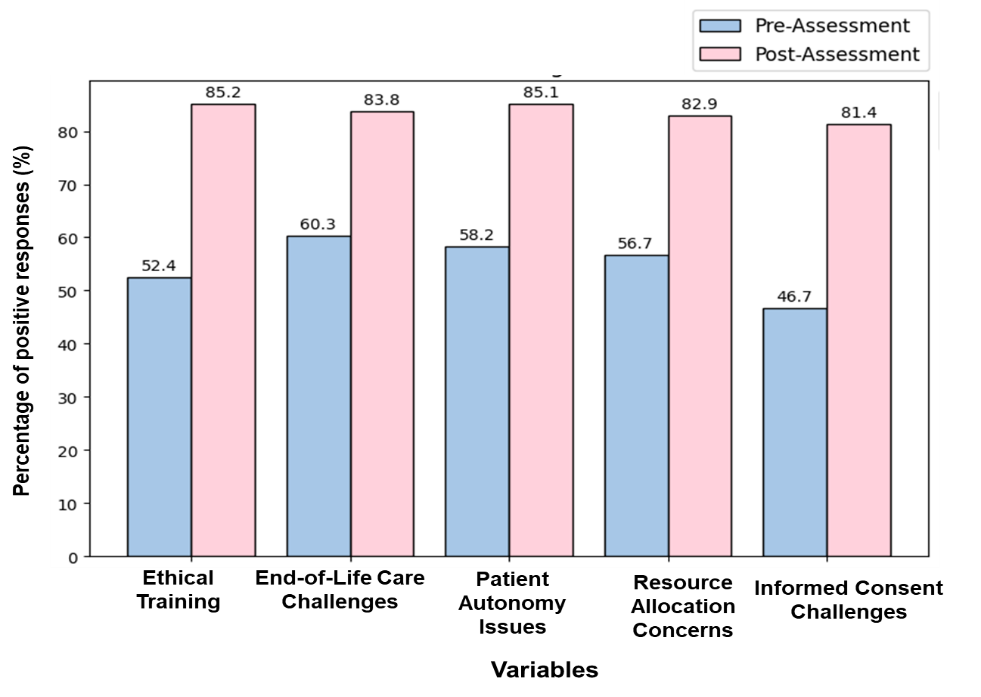
Figure 3. Effect of Ethical training on ICU nurses
Analysis of the paired T-test on the Effect of Ethical Training on ICU Nurses
By comparing pre- and post-assessment ratings across various ICU sections, the paired t-test was used to evaluate the efficacy of ethical instruction. The assessment evaluated whether training led to a statistically significant alteration in nurses' ethical awareness measures. Table 4 and figure 4 revealed that ethical training produced a very significant effect (p < 0,001) on all ICU sections by enhancing professional conduct among nurses. Training at the cardiac ICU generated the most noticeable improvement (Mean Difference = 32,6) and subsequent sections also registered improved results as nursing employees demonstrated substantial ethical understanding following their training sessions. Research evidence revealed that professional conduct and ethical consciousness maintained a direct relationship since nurses who received ethics education followed ethical norms better. The results demonstrate that essential structured ethical training should be implemented in critical care scenarios because it improves healthcare decisions and builds ethical expertise to enhance patient care quality.
|
Table 4. Comparing Ethical Awareness Scores in Different ICU Sections |
|||||||
|
Variable (ICU section) |
Ethical awareness of Pre-Assessment Mean (SD) |
Ethical awareness of Post-Assessment Mean (SD) |
Mean Difference |
t-value |
df |
p-value |
Significance |
|
Medical ICU (MICU) |
53,2 (8,4) |
84,3 (7,1) |
31,1 |
12,45 |
149 |
<0,001 |
Significant |
|
Surgical ICU (SICU) |
50,8 (7,7) |
82,1 (6,9) |
31,3 |
11,89 |
149 |
<0,001 |
Significant |
|
Pediatric ICU (PICU) |
50,8 (7,7) |
80,8 (7,2) |
31,3 |
11,62 |
149 |
<0,001 |
Significant |
|
Neonatal ICU (NICU) |
51,2 (8,3) |
81,9 (7,4) |
30,7 |
12,21 |
149 |
<0,001 |
Significant |
|
Cardiac ICU (CICU) |
50,1 (7,6) |
82,7 (6,7) |
32,6 |
12,83 |
149 |
<0,001 |
Significant |
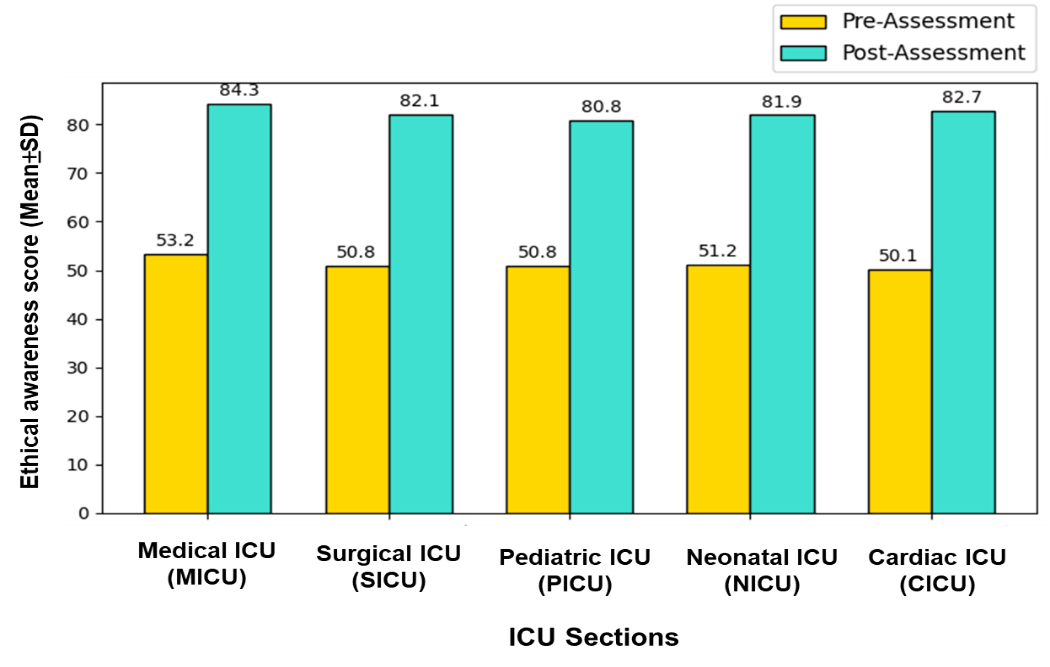
Figure 4. Ethical awareness in different ICU sections
By conducting structured ethical training, researchers measured ICU nurse's ethical performance and ethical consciousness through an assessment of their progress in confronting dilemmas, their assurance in decision-making and their commitment to ethical principles. The assessment scores indicated that nurses displayed greater ethical capability after the program while their patient autonomy management and end-of-life care and resource distribution quality improved. The professional competence of nurses increased alongside their confidence in ethical decisions and their ability to follow ethical guidelines. Ethical training programs produced clear evidence that morality improved along with better ethical awareness, thus demonstrating the necessity for sustaining ethical training initiatives that enhance both critical reasoning abilities and help reduce behavioral conflicts and better patient-centered care in ICUs.
CONCLUSIONS
Professional ethical training programs led to improved ethical awareness levels and better decision-making abilities along with enhanced professional behavior among ICU nurses, according to this research. The research aimed to evaluate whether nurses receive improved moral dilemma management skills through structured training programs in critical care settings. After the training, the ethical awareness of participants improved significantly and their ratings in post-assessment showed statistically notable changes across all variables (p < 0,001). The training increased the probability of ethical principal compliance by trained nurses by 6,36 percent (Exp(B) = 6,36 p < 0,001). The paired t-test showed substantial improvements in every ICU area with cardiac units, demonstrating maximum mean enhancement. Organized ethical training emerges as a crucial factor for developing ICU nurses' moral judgment and decreasing ethical problems, which leads to better patient care. One major weakness of the research stems from its narrow focus on ICU nurses working at three specific hospitals, leading to minimal external validity. Future research must investigate how ethical training influences employee retention across a long period as well as its influence on patient outcomes in multiple healthcare environments.
BIBLIOGRAPHIC REFERENCES
1. McAndrew NS, Leske J, Schroeter K. Moral distress in critical care nursing: the state of the science. Nursing ethics. 2018 Aug;25(5):552-70. https://doi.org/10.1177/0969733016664975
2. Fukuda T, Sakurai H, Kashiwagi M. Impact of having a certified nurse specialist in critical care nursing as head nurse on ICU patient outcomes. PloS one. 2020 Feb 5;15(2):e0228458. https://doi.org/10.1371/journal.pone.0228458
3. Social LD. Resilience as an Incomplete Strategy for Coping With Moral Distress in Critical Care Nurses. Critical Care Nurse. 2020 Dec 1;40(6). 10.4037/ccn2020873
4. Bergman L, Falk AC, Wolf A, Larsson IM. Registered nurses' experiences of working in the intensive care unit during the COVID‐19 pandemic. Nursing in critical care. 2021 Nov;26(6):467-75. https://doi.org/10.1111/nicc.12649
5. Crowe S, Howard AF, Vanderspank-Wright B, Gillis P, McLeod F, Penner C, Haljan G. The effect of COVID-19 pandemic on the mental health of Canadian critical care nurses providing patient care during the early phase pandemic: A mixed method study. Intensive and Critical Care Nursing. 2021 Apr 1;63:102999. https://doi.org/10.1016/j.iccn.2020.102999
6. Khan N, Jackson D, Stayt L, Walthall H. Factors influencing nurses' intentions to leave adult critical care settings. Nursing in critical care. 2019 Jan;24(1):24-32. https://doi.org/10.1111/nicc.12348
7. Akdeniz M, Yardımcı B, Kavukcu E. Ethical considerations at the end-of-life care. SAGE open medicine. 2021 Mar;9:20503121211000918. https://doi.org/10.1177/20503121211000918
8. Pishgooie AH, Barkhordari-Sharifabad M, Atashzadeh-Shoorideh F, Falcó-Pegueroles A. Ethical conflict among nurses working in the intensive care units. Nursing ethics. 2019 Nov;26(7-8):2225-38. https://doi.org/10.1177/0969733018796686
9. Abbasi S, Ghafari S, Shahriari M, Shahgholian N. Effect of moral empowerment program on moral distress in intensive care unit nurses. Nursing ethics. 2019 Aug;26(5):1494-504. https://doi.org/10.1177/0969733018766576
10. Kavurmacı M, Tan M. Determining the moral sensitivities of intensive care nurses. Critical care nursing quarterly. 2019 Jul 1;42(3):278-84. 10.1097/CNQ.0000000000000270
11. Yoo HJ, Lim OB, Shim JL. Critical care nurses’ communication experiences with patients and families in an intensive care unit: A qualitative study. Plos one. 2020 Jul 9;15(7):e0235694. https://doi.org/10.1371/journal.pone.0235694
12. Hiler CA, Hickman Jr RL, Reimer AP, Wilson K. Predictors of moral distress in a US sample of critical care nurses. American Journal of Critical Care. 2018 Jan 1;27(1):59-66. https://doi.org/10.4037/ajcc2018968
13. Mills M, Cortezzo DE. Moral distress in the neonatal intensive care unit: what is it, why it happens, and how we can address it. Frontiers in pediatrics. 2020 Sep 10;8:581. https://doi.org/10.3389/fped.2020.00581
14. Haghighinezhad G, Atashzadeh-Shoorideh F, Ashktorab T, Mohtashami J, Barkhordari-Sharifabad M. Relationship between perceived organizational justice and moral distress in intensive care unit nurses. Nursing ethics. 2019 Mar;26(2):460-70. https://doi.org/10.1177/0969733017712082
15. Urisman T, Garcia A, Harris HW. Impact of surgical intensive care unit interdisciplinary rounds on interprofessional collaboration and quality of care: Mixed qualitative-quantitative study. Intensive and Critical Care Nursing. 2018 Feb 1;44:18-23. https://doi.org/10.1016/j.iccn.2017.07.001
16. Babanataj R, Mazdarani S, Hesamzadeh A, Gorji MH, Cherati JY. Resilience training: Effects on occupational stress and resilience of critical care nurses. International journal of nursing practice. 2019 Feb;25(1):e12697. https://doi.org/10.1111/ijn.12697
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Sachet Dawar, Ritarani Nayak, RenukaJyothi S.
Methodology: Sachet Dawar, Ritarani Nayak, RenukaJyothi S.
Software: Sachet Dawar, Ritarani Nayak, RenukaJyothi S.
Drafting - original draft: Sachet Dawar, Ritarani Nayak, RenukaJyothi S.
Writing - proofreading and editing: Sachet Dawar, Ritarani Nayak, RenukaJyothi S.