doi: 10.56294/mw2023122
ORIGINAL
Assessing the Integration of Health Information Technology Competencies into Critical Care Nursing Practices
Evaluación de la integración de las competencias en tecnologías de la información sanitaria en las prácticas de enfermería de cuidados críticos
Malathi H1 ![]() *, Sameer
Rastogi2
*, Sameer
Rastogi2 ![]() , Nibedita Rout3
, Nibedita Rout3 ![]()
1JAIN (Deemed-to-be University), Department of Biotechnology and Genetics. Bangalore, Karnataka, India.
2School of Pharmacy, Noida International University. Greater Noida, Uttar Pradesh, India.
3SUM Nursing College, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Medical Surgical Nursing. Bhubaneswar, Odisha, India.
Cite as: H M, Rastogi S, Rout N. Assessing the Integration of Health Information Technology Competencies into Critical Care Nursing Practices. Seminars in Medical Writing and Education. 2023; 2:122. https://doi.org/10.56294/mw2023122
Submitted: 10-09-2022 Revised: 22-12-2022 Accepted: 26-02-2023 Published: 27-02-2023
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Malathi H *
ABSTRACT
Health Information Technology (HIT) is crucial in enhancing critical care nursing by improving efficiency, patient safety, and decision-making. Despite its benefits, integrating HIT competencies into nursing practice remains inconsistent due to training gaps and system usability issues. Understanding these challenges is essential for optimizing HIT adoption in critical care settings. Research aims to assess the integration of HIT competencies into critical care nursing, identifying competency levels, barriers to adoption, and the impact on clinical performance. 250 critical care nurses from multiple healthcare institutions participated in the investigation. Participants were selected using a stratified random sampling technique. A mixed-methods approach was used, including quantitative surveys and qualitative interviews. Descriptive statistics, t-tests, and regression analysis were employed to assess HIT competency levels and identify significant barriers to adoption. The best-performing factors were perceived proficiency in patient care and HIT usage frequency, which demonstrated important levels of engagement and a favorable consequence on patient results. Regression analysis revealed a significant positive correlation between HIT competency levels and perceived efficiency in patient care (p < 0,05). Addressing these issues through targeted education programs, improved system design, and institutional support is essential for enhancing patient care and nursing efficiency.
Keywords: Health Information Technology (HIT); Critical Care; Nursing Practice; Electronic Health Records (EHR); Decision-Making.
RESUMEN
La tecnología de la información sanitaria (HIT, por sus siglas en inglés) es crucial para mejorar la enfermería de cuidados críticos al mejorar la eficiencia, la seguridad del paciente y la toma de decisiones. A pesar de sus beneficios, la integración de las competencias de la HIT en la práctica de enfermería sigue siendo inconsistente debido a las lagunas en la formación y a los problemas de usabilidad del sistema. Comprender estos retos es esencial para optimizar la adopción de la HIT en los entornos de cuidados críticos. El objetivo de la investigación es evaluar la integración de las competencias de HIT en la enfermería de cuidados críticos, identificando los niveles de competencia, las barreras para la adopción y el impacto en el rendimiento clínico. Participaron en la investigación 250 enfermeras de cuidados críticos de múltiples instituciones sanitarias. Los participantes fueron seleccionados mediante una técnica de muestreo aleatorio estratificado. Se utilizó un método mixto que incluía encuestas cuantitativas y entrevistas cualitativas. Se emplearon estadísticas descriptivas, pruebas t y análisis de regresión para evaluar los niveles de competencia en HIT e identificar las barreras significativas para su adopción. Los factores con mejores resultados fueron la competencia percibida en la atención al paciente y la frecuencia de uso de la HIT, que demostraron importantes niveles de compromiso y una consecuencia favorable en los resultados del paciente. El análisis de regresión reveló una correlación positiva significativa entre los niveles de competencia en HIT y la eficiencia percibida en la atención al paciente (p < 0,05). Abordar estas cuestiones mediante programas de formación específicos, un mejor diseño del sistema y el apoyo institucional es esencial para mejorar la atención al paciente y la eficiencia de la enfermería.
Palabras clave: Tecnología de la Información en Salud (HIT); Cuidados Críticos; Práctica de Enfermería; Historia Clínica Electrónica (HCE); Toma de Decisiones.
INTRODUCTION
Nurses are essential to healthcare by providing complete patient care and building strong patient associations. Superior clinical treatment requires difficult evaluation and education techniques. Adequate nursing education is crucial for preparing competent professionals. To assess the clinical competencies and skills of graduating nursing students, the Objective Structured Clinical Examination (OSCE), originally designed for medical students, has been adapted for use with nursing students. The modification ensures a comprehensive evaluation of nursing students’ practical abilities and clinical proficiency, ensuring well-prepared practice.(1) Nursing graduates need to be thoroughly prepared to apply nursing informatics (NI) to ensure the delivery of safe high-quality and economical patient care within rapidly advancing healthcare environments. NI integrates information and communication technology with nursing practice and knowledge to enhance patient care. By leveraging data and technology, NI supports evidence-based decision-making, improves patient outcomes, and fosters effective communication within healthcare teams. The integration not only elevates patient care but also promotes the healthcare of families and communities, advancing global health in the process.(2)
Critical care nurses need to know how to use a variety of Health Information Technology (HIT) technologies. This entails being able to use telemedicine platforms, patient monitoring equipment, and electronic health records. To certify the patient data is correct and current, nurses should be able to enter, retrieve, and update it in electronic health records. Additionally, they should be skilled at interpreting data from automated patient monitoring devices, which frequently show a quantity of factors at once. The technological ability and the capacity understand the physiological implications of the data being presented. This adaptation is critical for growing patient care, enhancing operational efficiency, and ensuring that healthcare systems remain valuable and combative in a digital world.(3) Critical care nurses need to be proficient communicators who can fast and efficiently convey important information with other medical professionals using HIT tools. This might assume apprising a respiratory therapist of a shift in a patient's oxygen saturation levels or communicating the patient's condition to a doctor through telemedicine. Additionally, nurses need to be able to impose on patients and their families on how to deploy HIT systems, mostly when it comes to using remote monitoring equipment or telemedicine deliberation.(4) A convoluted and increasingly common disorder, delirium poses serious complications for nursing staff, particularly in critical care establishment and Intensive Care Units (ICUs). Delirium can foremost to significant complications, as well as extended hospital stays, long-time cognitive deficiencies, and amplified mortality rates. Numerous factors are extant to its onset, including sleep disturbances, which are common in ICU environments due to noise, bright lights, and persistent monitoring. Pain management is another key factor, as imperfectly controlled pain can amplify cognitive dysfunction. Emotional support, empathy, and clear communication are crucial in critical care settings since patients are generally at their most unprotected. HIT must be used by nurses to improve these aspects of care, ensuring that technology develops rather than detracts from the patient experience. Healthcare organizations need to make investments in thorough training programs that provide nurses the clinical and technical know-how required to use HIT tools efficiently.(5) Research proposes to evaluate the critical care nursing that incorporates HIT capabilities. It evaluates the effect of HIT on clinical performance, evaluates obstacles to HIT adoption, and estimates the skill levels of critical care nurses. It aims to promote HIT adoption for improved patient care and nursing efficiency by highlighting training, system usability, and workload constraints.
A conceptual framework for ICU nursing competencies was generated in the research using the experiences of nurses, patients, and families.(6) Meta-ethnography was used to synthesize 19 research into the main subject of concern safe and being safe, with subthemes such as motivation and improving confidence. Technical proficiency, collaboration, interpersonal skills, communication, bedside presence, participatory care, and cooperation are all important. Sample heterogeneity, cultural variations, and changing intensive care unit methods are some of the difficulties. The outcomes showed that to improve patient safety, trust, and the general standard of care in critical care settings, these capabilities must be incorporated into nursing education and practice.
Research developed a psychometric tool to assess the quality of technology abilities of hired nurses providing academic care facilities because of the necessity for the skills in information technology in the nursing field.(7) The measurement model approach was used for structural equation modeling, and the mean-variance was computed. The model's suppositions and connections were tested using linear structural relations (LISREL) software. Results indicated that the lower part of the first-order measurement model had quite an accurate estimation. The limited ability to generalize findings to larger healthcare populations, constraints on personal information, absence of longitudinal analysis, measurement errors, subjective assessments, potential variations across regions or institutions, small sample size, possible response bias, reliance on LISREL, and lack of external validation. The competency-based education (CBE) programs' new graduate nurses (NGNs) use learned skills in actual healthcare environments was investigated.(8) It addressed that ethnography was carried out on three university hospital acute-care wards. Individual semi-structured interviews or focus groups were conducted with participants from four subgroups: general practice nurses, preceptors, and clinical nurse specialists. According to the data, seven of the eight skills taught to new graduate nurses (NGNs) are successfully applied. The deployment of competencies could be divided into three main ones, such as scientific practice, interprofessional collaboration, and role adaptability. A small sample size, the possibility of participant bias, the single-setting focus, the use of self-reported data, the absence of longitudinal analysis, the limited generalizability, the subjective interpretations, the unexamined external factors, and the absence of an evaluation of long-term competency retention in HIT.
An evaluation of the effects of scenario-based instruction in the medical performance of critical care nursing students was developed.(9) It attempts to present quantifiable data on postgraduate nursing training benefits from simulation-based learning in terms of critical thinking, decision-making, and practical skills. A randomized controlled trial (RCT) design was used. The control and test groups were assigned at random to postgraduate nursing students. Before evaluation, the test group received simulation training, whereas the control group did not allow the comparison of effectiveness. Using the particularly designed instrument, an impartial evaluator gathered performance data. The test group performed significantly better than the control group in two clinical areas, as per the results. However, only targeted patient evaluated and emergency intervention skills observed this improvement. Short-term assessment, lack of long-term follow-up, unmeasured psychological influences, limited participant diversity, potential evaluator bias, single-institution focus, simulation quality variability, reliance on a single evaluation tool, and limited applicability to larger critical care nursing settings are some of the limits.
Research determined the consequences of three-day Nursing Informatics (NI) training course on the competency of critical care nurses were introduced. Three hospitals in southeast Iran provided sixty nurses, who were randomized to either the intervention or control group. Before and one month after the training, data were gathered utilizing the modified Nursing Informatics Competency Assessment Tool (NICAT) and a demographic questionnaire. The results showed that the intervention group's NI competency had significantly increased, especially in informatics literacy. The drawbacks, such as an insufficient number of participants and the possibility of bias, require further research on benefits over time and greater use.(10)
METHOD
To evaluate the integration of HIT accomplishment into critical care nursing practices, research utilizes mixed-methods techniques. To gather a wide range of data from critical care nursing staff, the method is conducted in a lot of hospital establishments. The HIT skill levels, adoption hurdles, and their consequences on clinical performance; the method used both quantitative and qualitative data congregating techniques.
Data collection
To manage an evaluation of HIT skill levels across several clinical contexts, 250 critical care nurses were enlisted from healthcare benefits. A stratified random sampling method is used to create a representative sample, organizing participants according to hospital size, unit specialization, and years of experience. The method reduced the probability of biases and made results could be applied to a larger group of critical care nurses. Calculate to provide sufficient statistical power for in-depth analysis, the sample size selected enables the detection of significant trends in the adoption of HIT, integration challenges, and their overall effects on clinical performance. By integrating nurses from varied backgrounds to provide actionable exhortations for enhancing HIT training and implementation approaches in critical care environments. Table 1 shows that the demographic details of Nurses.
|
Table 1. Demographic Details of Nurses |
|||
|
Demographic Variables |
Category |
Frequency (n) |
Percentage (%) |
|
Age (years) |
61+ |
15 |
6,0 |
|
51-60 |
40 |
16,0 |
|
|
41-50 |
55 |
22,0 |
|
|
31-40 |
80 |
32,0 |
|
|
18-30 |
60 |
24,0 |
|
|
Gender |
Male |
90 |
36,0 |
|
Female |
150 |
60,0 |
|
|
Non-binary/Other |
10 |
4,0 |
|
|
Years of Nursing Experience |
0-5 years |
55 |
22,0 |
|
6-10 years |
70 |
28,0 |
|
|
11-15 years |
65 |
26,0 |
|
|
16+ years |
60 |
24,0 |
|
|
Hospital Type |
Community Hospital |
140 |
56,0 |
|
Private/Other |
110 |
44,0 |
|
|
Experience with HIT |
No experience |
30 |
12,0 |
|
1-2 years |
70 |
28,0 |
|
|
3-5 years |
90 |
36,0 |
|
|
6+ years |
60 |
24,0 |
|
Statistical Analysis
Regression analysis was used to find correlations among competence and perceived patient care efficiency, t-tests were used to compare capability with groups, and descriptive statistics were used to evaluate HIT competency levels. The findings demonstrated the importance of instruction and system usability by showing a strong positive connection between increased HIT levels of proficiency and enhanced healthcare efficiency.
Descriptive statistics
Descriptive statistics were utilized to analyze the quantitative data to extend the recognized competencies and specifics of HIT tool usage. It provides for the research's desire to regulate adoption obstacles, gauge HIT skill levels, and analyze how these affect clinical performance. By recognizing important areas for enhancement in HIT integration, measuring variability guaranteed an accurate depiction of critical care nurses' opinions of competency and use patterns.
![]()
To measure data variability, the formula computes the sample standard deviation (SD). Individual values (w), the number of data points (m), and their deviation from the mean (w ̅) are all taken into account. To present an attached depiction of HIT skill levels and usage patterns, the denominator accounts for sample size.
T-tests
To modulate variations in HIT benefit between subgroups (e.g., nurses with varied degrees of experience or training), t-tests were used. To appraise variability in HIT quantifying among subgroups, such as nurses with deviating degrees of training or experience, t-tests were utilized. To help estimate the combination of HIT competencies in critical care nursing, this analysis organizes competency levels, adoption obstacles, and their consequence on clinical appearance.
The sample standard deviation (s), which demarcate the deviation in HIT competency and adoption obstacles among critical care nurses, is premeditated using the formula. The total amount of declarations is represented by m, whereas c stands for individual data points. All data points are added together in the numerator, while sample size and squared values are regulated for in the denominator. It facilitates an approximation of HIT integration, stimulating skill levels, and apprehending obstacles that impacts the productiveness of critical care nurses and the excellence of patient care.
Regression analysis
The relationship between perceived healthcare productivity and HIT skill levels was evaluated utilizing regression models, with a foreground on detecting important drivers of clinical performance. By organizing adoption obstacles, assessing their enforcements on clinical performance, and measuring skill levels, this research aims to evaluate the integration of HIT achievement into critical care nursing.
![]()
The dependent variable, Y, stands for the evaluated result. The value of Y when x is 0 is signified by the y-intercept, or b. It advances the research’s analysis of the interrelation between nurse coherence and HIT specialty.
RESULTS AND DISCUSSION
This section presents the statistical analysis results on factors modifying HIT ability and incorporation in critical care nursing, using SPSS Version for data analysis. It estimates variations in skill levels, classifies barriers to adoption, and calculates the influence on clinical performance and patient care efficiency. Descriptive statistics, t-tests, and regression analyses were working to appraise HIT ability levels and recognize important barriers to adoption, with a focus on training gaps, system usability issues, and workload concerns.
Descriptive statistics
Descriptive information about critical care nursing's HIT ability and obstacles is shown in table 2. It incorporates perceived efficiency, organizational workload, system usability, training adequacy, usage frequency, and skill levels. The results emphasize the regular usage of HIT but also point to problems including inadequate training, usability problems, and workload issues. A substantial proportion with the technology and an increased workload related to further hinder effective integration. These issues, although not universal, point to the need for targeted improvements in training programs and system design to optimize the use of HIT and improve its possible benefits in critical care surroundings.
|
Table 2. Descriptive Analysis of HIT Competency and Barriers to Integration |
|||||
|
Variable |
Mean |
Standard Deviation (SD) |
Minimum |
Maximum |
Percentage (%) |
|
HIT Competency Level |
3,2 |
0,85 |
1 |
5 |
52 fully competent |
|
HIT Usage Frequency |
4,2 |
0,75 |
1 |
5 |
78 frequent use |
|
Training Sufficiency |
2,8 |
1,1 |
1 |
5 |
64 insufficient training |
|
System Usability Issues |
2,7 |
1,0 |
1 |
5 |
47 usability issues |
|
Documentation Workload |
3,0 |
1,2 |
1 |
5 |
39 increased workload |
|
Perceived Efficiency in Patient Care |
4,1 |
0,68 |
2 |
5 |
75 perceive increased efficiency |
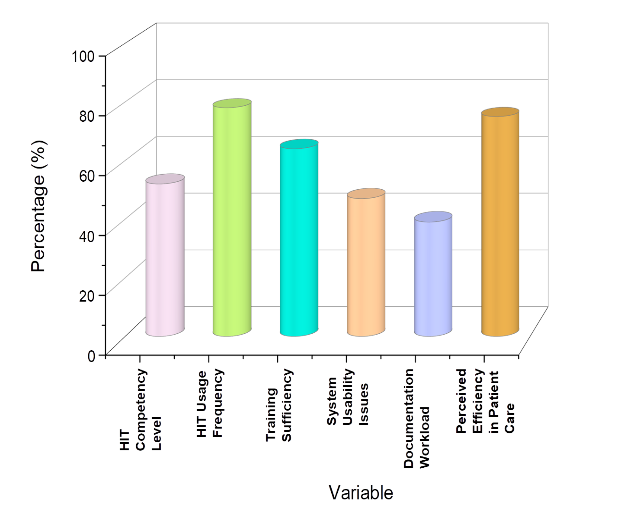
Figure 1. Frequency distribution (%) of different variables
A descriptive assessment of HIT competency and the obstacles to its incorporation in critical care nursing is shown in table 2 and figure 1. According to the data, 52 % of nurses believe they are competent in HIT, with a mean competency level of 3,2 (SD = 0,85). 78 % of respondents indicate regular use of HIT, indicating a high frequency of use (M = 4,2, SD = 0,75). These obstacles hinder optimal use of HIT IN critical care settings. Nevertheless, 75 % of respondents affirm that HIT improves the effectiveness of patient care, importance its perceived value despite the challenges. Addressing the barriers could improve both nurse competency and overall patient care outcomes in critical care environments.
T-tests
The t-test findings evaluating HIT skills and hurdles in critical care nursing are shown in table 3. It evaluates observed efficiency, documentation workload, technology usability, learning adequacy, competency levels, and usage frequency. The results show notable variations in the majority of factors, emphasizing issues with patient records burden, usability, and training deficiencies. These variations highlight the critical barriers that nurses face in effectively utilizing HIT, which might impact both their performance and the quality of patient care.
|
Table 3. T-test Results for HIT Competency and Barriers to Integration |
||||
|
Variable |
t-statistic |
Degrees of Freedom (DF) |
p-value |
Interpretation |
|
HIT Competency Level |
2,25 |
248 |
0,025 |
Statistically significant |
|
HIT Usage Frequency |
3,45 |
248 |
0,001 |
Statistically significant |
|
Training Sufficiency |
1,95 |
248 |
0,055 |
Marginally significant |
|
System Usability Issues |
3,10 |
248 |
0,002 |
Statistically significant |
|
Documentation Workload |
2,35 |
248 |
0,020 |
Statistically significant |
|
Perceived Efficiency in Patient Care |
1,85 |
248 |
0,065 |
Marginally significant |
Table 3 displays the outcomes of a t-test that examined integration obstacles and HIT competency. The following are statistically significant: system usability problems (t = 3,10, p = 0,002), documentation workload (t = 2,35, p = 0,020), HIT competency level (t = 2,25, p = 0,025), and HIT usage frequency (t = 3,45, p = 0,001). The results emphasize the substantial barriers nurses face in effectively using HIT, particularly in terms of system usability and the added burden of documentation. The analysis shows that the competency levels of nurses and their frequency of HIT use are significantly correlated with the integration challenges, perceived efficiency (t=1,85, p = 0,065) and training sufficiency (t= 1,95, p= 0,055) show marginal statistical significance, suggesting that while the factors are important, the overall integration might be moderate.
Regression analysis
Regression analysis results regarding adoption barriers and HIT competency in critical care nursing are shown in table 4. It focuses on the effects on estimated efficiency, machine accessibility, document load, training sufficiency, ability, and usage frequency. The results provide light on important aspects influencing the uptake and efficacy of HIT, both positive and negative. By determining these variables, the outcomes offer insights into the elements that contribute to successful HIT integration, as well as the challenges that hinder its full utilization. The results emphasize the importance of addressing both technical and training barriers to improve overall HIT outcomes.
|
Table 4. Regression Analysis for HIT Competency and Adoption Barriers |
|||||
|
Variable |
Coefficient (β) |
Standard Error (SE) |
t-Statistic |
p-value |
95 % Confidence Interval |
|
HIT Competency Level |
0,45 |
0,12 |
3,75 |
0,000 |
[0,21, 0,69] |
|
HIT Usage Frequency |
0,36 |
0,11 |
3,27 |
0,001 |
[0,15, 0,57] |
|
Training Sufficiency |
0,52 |
0,14 |
3,71 |
0,000 |
[0,25, 0,79] |
|
System Usability Issues |
-0,28 |
0,13 |
-2,15 |
0,033 |
[-0,53, -0,03] |
|
Documentation Workload |
-0,24 |
0,11 |
-2,18 |
0,031 |
[-0,46, -0,02] |
|
Perceived Efficiency in Patient Care |
0,60 |
0,15 |
4,00 |
0,000 |
[0,30, 0,90] |
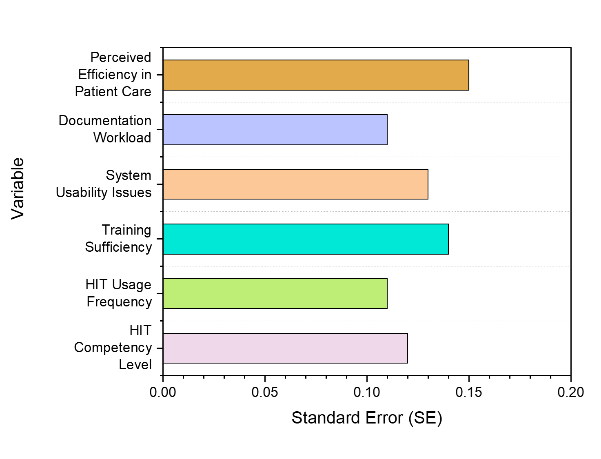
Figure 2. Percentage distribution of research variables
The results of regression analysis evaluating HIT adoption hurdles and skills in critical care nursing are shown in table 4 and figure 2. HIT usage frequency (β = 0,36, p = 0,001) and HIT Competency Level (β = 0,45, p = 0,000) had a beneficial effect on integration. Perceived efficiency (β = 0,60, p = 0,000) and training sufficiency (β = 0,52, p = 0,000) both considerably increase adoption. Nevertheless, implementation is adversely affected by problems with system usability (β = -0,28, p = 0,033) and documentation workload (β = -0,24, p = 0,031) have a detrimental effect on the successful implementation of HIT, indicating that they need to be addressed for improved acceptance. The outcomes highlight the critical role of user competence and adequate resources in overcoming adoption challenges.
DISCUSSION
The research aimed to evaluate clinical performance, identify integration hurdles, and gauge HIT competency. Using descriptive data, the majority of critical care nurses regularly utilize HIT; nonetheless, adoption is challenged by problems including insufficient training, usability challenges, and records burden. Significant differences in competency, workload, and system usability were validated by the findings of the t-test. According to regression research, adoption is positively impacted by HIT expertise, usage frequency, training adequacy, and perceived efficiency, while it is negatively impacted by usability problems and documentation effort. For HIT adoption in clinical settings to be additionally successful, the results emphasize the necessity of better training, system usability improvements, and workload management techniques. The use of technology in patient care can be improved by removing obstacles to its adoption. Improving system usability through user-centered design and intuitive interfaces makes it easier for nurses to use tools, which lowers faults and troubleshooting time. By addressing knowledge gaps and continuously promoting education and support, nurses' confidence and proficiency with HIT can be enhanced. Workload management techniques can also lessen managerial strain and free up more time for patient care, such as automating unchanging duties. When combined, these upgrades have the potential to increase patient outcomes and nurse satisfaction while also creating a more productive healthcare environment. The result accentuates that maximizing HIT uptake and making sure it fits with clinical processes would need fixing usability concerns and presenting concentrated training. A more constructive healthcare environment can eventually help patients and healthcare providers by enhancing nurses' technical skills and utilizing technology.
CONCLUSIONS
HIT is modifying critical care nursing by improving efficiency, patient safety, and clinical decision-making. The research aimed to assess the integration of HIT competencies in critical care nursing, identifying competency levels, barriers to adoption, and the impact on clinical performance. 250 critical care nurses participated in a mixed-methods that included questionnaires and interviews to gather data. The data was analyzed using regression analysis, t-tests, and descriptive statistics. The findings showed that just 52 % of nurses felt completely competent, even though 78 % regularly utilize HIT technologies. Insufficient instruction (64 %) and problems with system use (47 %) are major obstacles. Nurses' self-reported proficiency levels might not entirely represent their real skills with HIT. In addition, the sample size, albeit essential, is confined to a specific medical context, which can impair generalizability. Future investigations should examine how nursing performance is affected over the long run by the implementation of HIT, with a concentration on consistent gains in clinical consequences and competency. Additionally, research ought to look into the creation of intuitive HIT systems and efficient training curricula suited to a range of nursing positions.
BIBLIOGRAPHIC REFERENCES
1. Tseng LP, Hou TH, Huang LP, Ou YK. Effectiveness of applying clinical simulation scenarios and integrating information technology in medical-surgical nursing and critical nursing courses. BMC nursing. 2021 Dec; 20:1-4. https://doi.org/10.1186/s12912-021-00744-7
2. Shin EH, Cummings E, Ford K. A qualitative study of new graduates’ readiness to use nursing informatics in acute care settings: clinical nurse educators’ perspectives. Contemporary nurse. 2018 Jan 2;54(1):64-76. https://doi.org/10.1080/10376178.2017.1393317
3. Vehko T, Hyppönen H, Puttonen S, Kujala S, Ketola E, Tuukkanen J, Aalto AM, Heponiemi T. Experienced time pressure and stress: electronic health records usability and information technology competence play a role. BMC medical informatics and decision making. 2019 Dec; 19:1-9. https://doi.org/10.1186/s12911-019-0891-z
4. Hassona MF, Albaqawi H, Laput V. Effect of Saudi nurses' perceived work-life quality on work engagement and organizational commitment. Int J Adv Appl Sci. 2021 Feb 19;8:79-87. https://doi.org/10.21833/ijaas.2021.06.009
5. Ozga D, Krupa S, Witt P, Mędrzycka-Dąbrowska W. Nursing interventions to prevent delirium in critically ill patients in the intensive care unit during the COVID-19 pandemic—narrative overview. In Healthcare 2020 Dec 21 (Vol. 8, No. 4, p. 578). MDPI. https://doi.org/10.3390/healthcare8040578
6. Henriksen KF, Hansen BS, Wøien H, Tønnessen S. The core qualities and competencies of the intensive and critical care nurse, a meta‐ethnography. Journal of advanced nursing. 2021 Dec;77(12):4693-710. https://doi.org/10.1111/jan.15044
7. Farzandipour M, Mohamadian H, Akbari H, Safari S, Sharif R. Designing a national model for assessment of nursing informatics competency. BMC medical informatics and decision making. 2021 Dec; 21:1-2. https://doi.org/10.1186/s12911-021-01405-0
8. Charette M, Goudreau J, Bourbonnais A. How do newly graduated nurses from a competency-based program demonstrate their competencies? A focused ethnography of acute care settings. Nurse Education Today. 2019 Aug 1; 79:161-7. https://doi.org/10.1016/j.nedt.2019.05.031
9. Hardenberg J, Rana I, Tori K. Simulation exposure improves clinical skills for postgraduate critical care nurses. Clinical Simulation in Nursing. 2019 Mar 1;28: 39-45. https://doi.org/10.1016/j.ecns.2018.12.007
10. Jouparinejad S, Foroughameri G, Khajouei R, Farokhzadian J. Improving the informatics competency of critical care nurses: results of an interventional study in the southeast of Iran. BMC Medical Informatics and Decision Making. 2020 Dec; 20:1-2. https://doi.org/10.1186/s12911-020-01244-5
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Malathi H, Sameer Rastogi, Nibedita Rout.
Methodology: Malathi H, Sameer Rastogi, Nibedita Rout.
Software: Malathi H, Sameer Rastogi, Nibedita Rout.
Drafting - original draft: Malathi H, Sameer Rastogi, Nibedita Rout.
Writing - proofreading and editing: Malathi H, Sameer Rastogi, Nibedita Rout.