doi: 10.56294/mw2023124
ORIGINAL
Investigating the Role of Medical Informatics in Enhancing Healthcare Accessibility and Clinical Decision-Making
Investigación del papel de la informática médica en la mejora de la accesibilidad de la asistencia sanitaria y la toma de decisiones clínicas
Shilpi
Singh1 ![]() *, Antaryami Pradhan2
*, Antaryami Pradhan2
![]()
1Noida International University, Department of Biotechnology and Microbiology. Greater Noida, Uttar Pradesh, India.
2IMS and SUM Hospital, Siksha ‘O’ Anusandhan (deemed to be University), Department of General Surgery. Bhubaneswar, Odisha, India.
Cite as: Singh S, Pradhan A. Investigating the Role of Medical Informatics in Enhancing Healthcare Accessibility and Clinical Decision-Making. Seminars in Medical Writing and Education. 2023; 2:124. https://doi.org/10.56294/mw2023124
Submitted: 11-09-2022 Revised: 23-12-2022 Accepted: 26-02-2023 Published: 27-02-2023
Editor:
PhD. Prof. Estela Morales Peralta ![]()
Corresponding Author: Shilpi Singh *
ABSTRACT
Medical informatics plays a crucial role in transforming healthcare accessibility by integrating advanced technologies to improve patient care, streamline medical processes, and enhance decision-making. Medical informatics uses telemedicine and electronic health records (EHRs) to connect patients and healthcare professionals in response to the increasing need for effective healthcare services. The aim of this research is to investigate the role of medical informatics in enhancing healthcare accessibility and clinical decision-making through the use of digitized medical records. A total of 347 consultations were observed, with data collected using a work sampling technique during follow-up outpatient sessions at various hospitals. The data was analyzed using statistical methods, which include descriptive statistics, one-way ANOVA, Mann-Whitney U test and regression analysis. Findings reveal that the paper records revealed considerable disparities in consultation times across hospitals and specializations. Digital records showed notable disparities only between specializations. Consultation times were not significantly different between paper and digital records (p0,278), while time spent seeking computer records increased in several specialties. Digitized data, including remote access, quicker inpatient handovers, and improved record timelines, all contribute to better decision-making. This research highlights the digitized medical records, as a component of medical informatics, contribute to improved healthcare accessibility and clinical decision-making when combined with standardized operational procedures.
Keywords: Medical Informatics; Healthcare Accessibility; Clinical Decision-Making; Digitized Medical Records.
RESUMEN
La informática médica desempeña un papel crucial en la transformación de la accesibilidad de la asistencia sanitaria mediante la integración de tecnologías avanzadas para mejorar la atención al paciente, agilizar los procesos médicos y potenciar la toma de decisiones. La informática médica utiliza la telemedicina y las historias clínicas electrónicas (HCE) para conectar a pacientes y profesionales sanitarios en respuesta a la creciente necesidad de servicios sanitarios eficaces. El objetivo de este estudio es investigar el papel de la informática médica en la mejora de la accesibilidad a la atención sanitaria y la toma de decisiones clínicas mediante el uso de historiales médicos digitalizados. Se observó un total de 347 consultas, con datos recogidos mediante una técnica de muestreo de trabajo durante sesiones de seguimiento ambulatorio en varios hospitales. Los datos se analizaron mediante métodos estadísticos, que incluyen estadística descriptiva, ANOVA unidireccional, prueba U de Mann-Whitney y análisis de regresión. Los resultados revelan que los registros en papel mostraron disparidades considerables en los tiempos de consulta entre hospitales y especialidades. Los registros digitales sólo mostraron disparidades notables entre especialidades. Los tiempos de consulta no fueron significativamente diferentes entre los registros en papel y los digitales (p≥0,278), mientras que el tiempo empleado en buscar registros informáticos aumentó en varias especialidades. La digitalización de los datos, incluido el acceso a distancia, la agilización de las transferencias a los pacientes ingresados y la mejora de los plazos de los historiales contribuyen a mejorar la toma de decisiones. Esta investigación pone de relieve que las historias clínicas digitalizadas, como componente de la informática médica, contribuyen a mejorar la accesibilidad de la atención sanitaria y la toma de decisiones clínicas cuando se combinan con procedimientos operativos estandarizados.
Palabras clave: Informática Médica; Accesibilidad de la Atención Sanitaria; Toma de Decisiones Clínicas; Historias Clínicas Digitalizadas.
INTRODUCTION
Medical informatics (MI) is an interdisciplinary area that uses biological data for scientific inquiry, problem-solving, and decision-making with the goal of improving human health. Computers and clinical guidelines, formal medical terminology, as well as information and communication systems, are some of the tools used in MI.(1) The definition of MI also known as biomedical and health informatics has been quite diverse and even contradictory. It focuses on making the best use of information, sometimes with the use of technology, to advance patient care, public health, individual health, and biological research.(2)
MI utilizes Information Technology (IT) to enhance healthcare and medicine through data creation and analysis. Despite the present attention, MI is not a new domain.(3) Healthcare is a vital sector with high-risk and time-sensitive activities that are distinguished by specific characteristics, such as innate intra-/inter-subject variability, institutional harmonization, and legal concerns. Healthcare professionals' decision-making is typically hampered by the requirement to effectively integrate poorly organized, ambiguous, and potentially contradicting information from numerous sources.(4)
The availability, use, and health outcomes of the target population are commonly used to establish whether a group has access to healthcare. Access to healthcare includes the availability of acceptable and effective services and providers, the degree of accommodation, physical accessibility and cost and the acceptability of the services provided by patients.(5) Clinical decision making (CDM) is a phrase commonly utilized to define clinician’s primary responsibilities in clinical locations. It is a procedure that the nurses employ every day to make judgments regarding the care that the nurses deliver to the patients. CDM is typically defined as the procedure of deciding among possibilities.(6)
The primary benefits of technological modernization contain enhanced user experience, security and other elements of the healthcare organization. These benefits were provided by EHRs and Electronic Medical Records (EMR) systems. EHR systems have been used in hospitals worldwide because of its benefits, including improved security and cost effectiveness. It plays a crucial role in the healthcare industry, enhancing its functionality.(7) The role of MI in Enhancing Healthcare Accessibility and CDM is depicted in figure 1. The objective of the research is to examine the function of MI in improving healthcare accessibility and CDM by utilizing digital medical records.

Figure 1. Role of MI in Enhancing Healthcare Accessibility and CDM
The Unified Theory of Acceptance and Use of Technology (UTAUT) was extended in research to identify important elements influencing doctors' adoption of HER.(8) Partial Least Squares (PLS) was used to analyze the results of a cross-sectional survey that involved 300 participants. The findings indicated that adoption was highly influenced by social influence, enabling circumstances, and individual inventiveness. Limitations include difficulties, such as irregular power supplies and infrastructural problems. Using health informatics, the research improved the early diagnosis of coronary heart disease and diabetic retinopathy.(9) Retinal abnormalities are detected using image processing and machine learning, while heart health is tracked via IoT-based sensors. Automated categorization increases the precision of diagnosis. Although results indicate increased detection efficiency, there are drawbacks such as dependence on sensor precision and image quality.
Questionnaires measuring medical problem-solving skills and the use of internet health information were created and validated.(10) Online health searches and medical decision-making were shown to be significantly correlated using confirmatory factor analysis and structural equation modeling on data from 457 patients. Potential selection bias and self-reported data are among the limitations. Telehealth and telemedicine-related ethical, legal, and societal concerns were recognized and examined.(11) Key issues, emphasizing privacy, access, consent, and quality of treatment, were identified through the research and synthesis of the literature. Usability, commercialization, and cybersecurity are examples of emerging challenges. Reliance on previously published research is one of its limitations, requiring additional empirical research to confirm results.
Bibliometric analysis and thematic mapping were used to examine the research on MI and eHealth competencies/skills (EHCS).(12) The findings indicate different research philosophies, with EHCS emphasizing technology and patient-centered care and health informatics concentrating on nursing and teaching. Variations in search strings, database choice, and analysis based on abstracts are some of the limitations. In treating COVID-19, the analysis employed biomedical informatics and telemedicine. Informatics innovation linked to EHR and the adoption of four telehealth programs were some of the measures. The results showed effective monitoring of patients and continuity of care.(13) Reliance on telehealth infrastructure and policy longevity are some of the disadvantages.
To assess Federated Learning (FL) in biological applications, the investigation considered privacy, system, and statistical issues.(14) Assessing FL frameworks and its effects on healthcare data exchange is one such method. The findings show how FL can enhance data-driven insights while maintaining privacy. Data heterogeneity, model convergence problems, and implementation-related regulatory constraints are some of the limitations. Without raising privacy or legal issues, the research created artificial EHR for research and innovation. The patients' lifespans are simulated according to common conditions by using the open-source Synthea software.(15) The findings include one million publicly available records in standard formats. Ongoing model refinement and possible realism gaps are some of the limitations.
Clinical Pathways (CPs) were standardized and digitized to allow its recognition with the mentioned research.(16) New coding SNOMED CT, HL7, and ontologies were exploited to evolve a CP management system (CPMS). The outcomes present CP standardization, digitization, and successful integration into an electronic medical record. Limitations in this project included possible interoperability issues and the need for further, more broad clinical validation.
METHOD
To examine the usefulness of both digital and paper-based records in various hospital settings, a technique was developed for systematically observing and analyzing consultations. It describes the research strategy, data collection, and statistical analysis.
Research Design
|
Table 1.Demographic Features of the Research Participants |
|||
|
Variables |
Category |
Frequency (n) |
Percentage (%) |
|
Gender |
Male |
180 |
51,9 |
|
Female |
167 |
48,1 |
|
|
Age Group (years) |
≤20 |
30 |
8,6 |
|
21–40 |
120 |
34,6 |
|
|
41–60 |
135 |
38,9 |
|
|
>60 |
62 |
17,9 |
|
|
Hospital Type |
Public |
200 |
57,6 |
|
Private |
147 |
42,4 |
|
|
Specialty |
General Medicine |
100 |
28,8 |
|
Cardiology |
60 |
17,3 |
|
|
Neurology |
50 |
14,4 |
|
|
Orthopedics |
45 |
13,0 |
|
|
Pediatrics |
42 |
12,1 |
|
|
Other |
50 |
14,4 |
|
|
Record Type Used |
Paper-based |
180 |
51,9 |
|
Digital (EHR) |
167 |
48,1 |
|

Figure 2. Graphical representation of Demographic Features
Data Collection
A total of 347 consultations were recorded in the follow-up outpatient appointment processes across different hospitals. The consultations were selected to capture the widest possible array of disciplines and healthcare settings. Consultation hours were recorded in conjunction with information on the status of paper or electronic records being maintained, while staff work processes and patient-staff interactions were also documented. Following this methodology facilitated the collection of good data for further analysis.
Statistical Analysis
The data gathered was analyzed using a range of statistical methods to identify patterns and variations in consultation times. IBM SPSS 25.0 was used to analyze the role of MI in enhancing the healthcare accessibility and CDM using descriptive statistics, Mann-Whitney U (MWU) test, one-way ANOVA, and regression analysis. Descriptive statistics was employed to summarize the data and the one-way ANOVA was employed to compare consultation times across hospitals and specializations. Regression analysis was used to examine the relationship between consultation times and the type of record utilized. The MWU test was employed to check the substantial differences in the usage of paper with digital records.
RESULTS
This section presents the findings from the research on consultation times, record accessibility, and decision-making efficiency using both paper and digital medical records.
Investigating the Role of MI Using Descriptive Statistics Test
Descriptive statistics describe and organize healthcare data, providing information about patient demographics, treatment patterns, and accessibility trends. Mean and standard deviation data help highlight variances in MI adoption. This helps to assess system efficiency and user engagement. Descriptive findings help to shape future healthcare accessibility initiatives. Mean (M) is the average value of a dataset, which helps determine typical consultation times across demographic groups, hospital types, specializations, and record types, which is crucial for analyzing healthcare accessibility and efficiency. Standard Deviation (SD) is a measure of the variability or dispersion of consultation times, which indicates the consistency of healthcare service delivery and highlights inequalities in decision-making efficiency across various settings. Figure 3 and table 2 represent the consequences of the Descriptive statistics.
|
Table 2. Outcomes of the Descriptive Statistics |
|||
|
Variables |
Category |
M |
SD |
|
Age Group (years) |
≤20 |
12,5 |
2,8 |
|
21–40 |
13,7 |
3,0 |
|
|
41–60 |
14,5 |
3,3 |
|
|
>60 |
15,1 |
3,6 |
|
|
Gender |
Male |
14,2 |
3,5 |
|
Female |
13,8 |
3,2 |
|
|
Hospital Type |
Public |
14,0 |
3,4 |
|
Private |
13,9 |
3,1 |
|
|
Specialty |
General Medicine |
13,2 |
3,0 |
|
Cardiology |
14,8 |
3,2 |
|
|
Neurology |
15,2 |
3,4 |
|
|
Orthopedics |
14,0 |
3,1 |
|
|
Pediatrics |
13,5 |
2,9 |
|
|
Other |
14,1 |
3,3 |
|
|
Record Type Used |
Paper-based |
13,9 |
3,2 |
|
Digital (EHR) |
14,3 |
3,5 |
|
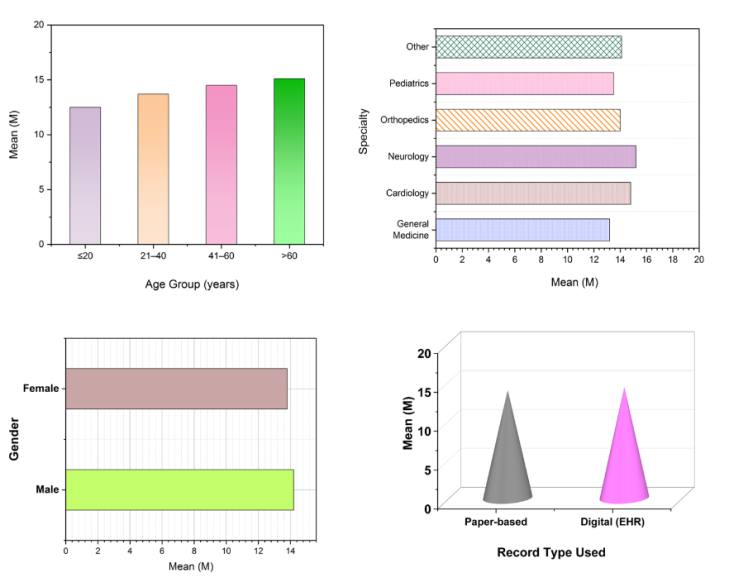
Figure 3. Graphical representation of Descriptive Statistics
Table 2 shows that the older patients (>60 years) had lengthier consultations (M = 15,1, SD = 3,6), and the mean consultation time differed minimally by age group and gender (Males: 14,2, Females: 13,8). The longest consultation duration was in neurology (M = 15,2, SD = 3,4), while the shortest was in general medicine (M = 13,2, SD = 3,0). The mean consultation time for digital records was slightly higher (M = 14,3) than the paper-based records (M = 13,9).
Investigating the Role of MI Using One-Way ANOVA Test
One-way ANOVA examines mean differences among many groups, such as hospitals that use various informatics systems. It compares differences in decision-making efficiency and accessibility improvements among institutions. The most effective informatics treatments are identified by comparing patient outcomes across groups. This provides data-driven improvements to MI techniques. The Sum of Squares (SS) method measures the entire variance in a dataset, which makes it easier to compare variations in healthcare accessibility and decision-making between telemedicine and traditional records. Degrees of Freedom (df) describes the number of independent variables that can change, allowing for accurate statistical comparisons across groups. Mean Square (MS) and F-value are used to assess variation and significance, assessing whether MI significantly improves patient care, time efficiency, and CDM. Table 3 shows the ANOVA findings for important healthcare performance measures in telemedicine with paper-based records.
|
Table 3. Outcomes of the One-way ANOVA |
||||||
|
Variables |
Source |
SS |
df |
MS |
F |
p-value |
|
Patient Accessibility Score |
Between Groups |
128,45 |
1 |
128,45 |
23,78 |
0,001 |
|
Within Groups |
854,23 |
345 |
2,48 |
|||
|
Time Efficiency in Patient Care |
Between Groups |
95,32 |
1 |
95,32 |
17,92 |
0,004 |
|
Within Groups |
748,89 |
345 |
2,17 |
|||
|
Accuracy of Clinical Decision-Making |
Between Groups |
140,21 |
1 |
140,21 |
28,11 |
0,000 |
|
Within Groups |
782,45 |
345 |
2,27 |
|||
|
Patient Satisfaction Level |
Between Groups |
115,67 |
1 |
115,67 |
22,05 |
0,002 |
|
Within Groups |
729,33 |
345 |
2,11 |
|||
|
Healthcare Cost Reduction |
Between Groups |
88,91 |
1 |
88,91 |
16,43 |
0,007 |
|
Within Groups |
701,67 |
345 |
2,03 |
|||
Table 3 shows that the telemedicine greatly improved all measures of healthcare performance. Patient accessibility scores were considerably higher (F = 23,78, p = 0,001), and time efficiency showed considerable increases (F = 17,92, p = 0,004). The most significant effect was identified in CDM accuracy (F = 28,11, p = 0,000). Patient satisfaction (F = 22,05, p = 0,002) and healthcare cost reduction (F = 16,43, p = 0,007) both exhibited statistically significant enhancements.
Investigating the Role of MI using the Mann-Whitney U Test
MWU Test is defined as a nonparametric test utilized to compare two independent groups, such as hospitals with and without modern informatics systems. It assesses variations in CDM efficacy and accessibility improvements. Since it does not rely on normal distribution, it is effective for tiny or skewed datasets. The test emphasizes the role of informatics in healthcare quality. This test was conducted to compare the rankings of healthcare outcomes between telemedicine and paper-based systems. Telemedicine (Mean Rank) and Paper-Based (Mean Rank) represent the average ranks of participants for each group (telemedicine and paper-based) in this test, which helps to compare the distribution of outcomes between the two methods. The U-Value indicates the test statistic used to determine if there is a substantial difference in ranks between the two groups, while the Z-Score shows the standard deviations away from the mean rank difference. The p-value tests the null hypothesis, with values less than 0,05, indicating significant differences between telemedicine and paper-based methods in healthcare outcomes, such as patient accessibility and CDM. Figure 4 and table 4 represent the outcomes of the MWU Test.
|
Table 4. Outcomes of the MWU Test |
|||||
|
Variables |
Telemedicine (Mean Rank) |
Paper-Based (Mean Rank) |
U-Value |
Z-Score |
p-value |
|
Patient Accessibility Score |
186,45 |
162,55 |
15600,0 |
-2,78 |
0,006 |
|
Time Efficiency in Patient Care |
189,32 |
160,45 |
15730,0 |
-2,82 |
0,005 |
|
Accuracy of Clinical Decision-Making |
191,27 |
158,32 |
15215,0 |
-3,12 |
0,002 |
|
Patient Satisfaction Level |
184,72 |
165,32 |
15440,0 |
-2,67 |
0,008 |
|
Healthcare Cost Reduction |
182,19 |
168,76 |
15895,0 |
-2,93 |
0,003 |

Figure 4. Graphical representation of MWU Test
Table 4 shows that all indicators had much higher mean rankings for telemedicine than paper-based records. CDM exhibited the greatest difference (U = 15215,0, p = 0,002), indicating that telemedicine increases diagnosis accuracy. Patient accessibility (U = 15600,0, p = 0,006) and satisfaction (U = 15440,0, p = 0,008) both improved significantly.
Investigating the Role of MI Using Linear Regression Test
Linear Regression Analysis quantifies the link between MI adoption and healthcare outcomes by examining how digital technologies affect accessibility, efficiency, and decision-making. It enhances informatics integration by delivering evidence-based insights for better patient care, resource allocation, and healthcare policies. This regression research estimates the direct impact of telemedicine on healthcare performance measures. The coefficient (B) represents the degree and direction of telemedicine's influence on healthcare outcomes, indicating how much each variable changes with each unit increase in telemedicine use. Standard Error (SE) measures coefficient accuracy, the t-value examines statistical significance, the p-value defines relevant results, and R² illustrates how effectively telemedicine predicts gains in accessibility, efficiency, decision-making, satisfaction, and cost reductions.
|
Table 5. Outcomes of the Linear Regression Analysis |
|||||
|
Variables |
B |
SE |
t-value |
p-value |
R² |
|
Patient Accessibility Score |
0,81 |
0,09 |
8,90 |
0,000 |
0,68 |
|
Time Efficiency in Patient Care |
0,72 |
0,11 |
6,55 |
0,002 |
0,61 |
|
Accuracy of Clinical Decision-Making |
0,85 |
0,08 |
10,20 |
0,000 |
0,72 |
|
Patient Satisfaction Level |
0,79 |
0,10 |
7,85 |
0,001 |
0,65 |
|
Healthcare Cost Reduction |
0,68 |
0,12 |
5,67 |
0,003 |
0,58 |
Table 5 shows that telemedicine has a considerable impact on healthcare outcomes, particularly in CDM (B = 0,85, p = 0,000, R² = 0,72). Patient accessibility (B = 0,81, p = 0,000) and satisfaction (B = 0,79, p = 0,001) were both positively impacted. The model explains 68 % of the variation in accessibility (R² = 0,68) and 72 % in decision-making (R² = 0,72), indicating the usefulness of telemedicine.
DISCUSSION
The results of the research underline the importance of MI, including telemedicine and digital records, in improving healthcare accessibility, decision-making efficiency, and patient happiness. Descriptive statistics indicated that consultation times varied by demographic group, hospital type, and specialty, with elderly patients and neurology departments having the longest appointments. The findings of one-way ANOVA showed that telemedicine considerably enhanced healthcare performance, notably CDM accuracy, patient accessibility, and satisfaction. The Mann-Whitney U test indicated that telemedicine-based systems scored higher in all major performance measures, highlighting the benefits of digital records over traditional paper-based procedures. Regression analysis demonstrated telemedicine's significant influence on healthcare outcomes, with decision-making and accessibility showing the greatest improvement. However, issues such as lengthier retrieval times for digital data in specific specializations underscore the significance of improving informatics systems and establishing procedures to fully leverage these technologies.
CONCLUSIONS
The research determined that MI considerably enhanced CDM and healthcare accessibility, particularly when combined with digitalized medical data. An analysis of 347 consultations indicated that the retrieval time for digital records increased in several specialties. However, the consultation durations did not differ significantly between paper and digital records (p≥0,278). While digital data revealed only substantial gaps between specialties, paper records revealed considerable differences in consultation times between hospitals and specializations. By providing remote access, speeding up inpatient handovers, and guaranteeing better record timeframes, digital records helped to enhance decision-making notwithstanding certain difficulties with record retrieval. These results emphasized how crucial it is to incorporate regular operating practices to optimize the advantages of digital medical records in terms of healthcare accessibility and efficiency. Variations in hospital procedures, possible inconsistent data input, and the longer retrieval times of digital records in specific specializations were the research's limitations. Further research might examine how real-time decision-support systems affect clinical efficiency, how AI can optimize record management, and how to improve interoperability.
BIBLIOGRAPHIC REFERENCES
1. Tapera R, Singh Y. A bibliometric analysis of medical informatics and telemedicine in sub-Saharan Africa and BRICS nations. Journal of public health research. 2021 Jun 16;10(3):jphr-2021. https://doi.org/10.4081/jphr.2021.1903
2. Gülkesen KH, Haux R. Research subjects and research trends in medical informatics. Methods of Information in Medicine. 2019 Jun;58(S 01):e1-3. https://doi.org/10.1055/s-0039-1681107
3. Kim YM, Delen D. Medical informatics research trend analysis: a text mining approach. Health informatics journal. 2018 Dec;24(4):432-52. https://doi.org/10.1177/1460458216678443
4. McMaughan DJ, Oloruntoba O, Smith ML. Socioeconomic status and access to healthcare: interrelated drivers for healthy aging. Frontiers in public health. 2020 Jun 18;8:231. https://doi.org/10.3389/fpubh.2020.00231
5. Krishnan P. A philosophical analysis of clinical decision making in nursing. Journal of Nursing Education. 2018 Feb 1;57(2):73-8. https://doi.org/10.3928/01484834-20180123-03
6. Nibbelink CW, Young JR, Carrington JM, Brewer BB. Informatics solutions for application of decision-making skills. Critical Care Nursing Clinics. 2018 Jun 1;30(2):237-46. https://doi.org/10.1016/j.cnc.2018.02.006
7. Shahnaz A, Qamar U, Khalid A. Using blockchain for electronic health records. IEEE access. 2019 Oct 9;7:147782-95. https://doi.org/10.1109/ACCESS.2019.2946373
8. Hossain A, Quaresma R, Rahman H. Investigating factors influencing the physicians’ adoption of electronic health record (EHR) in healthcare system of Bangladesh: An empirical study. International Journal of Information Management. 2019 Feb 1;44:76-87. https://doi.org/10.1016/j.ijinfomgt.2018.09.016
9. Bujnowska-Fedak MM, Węgierek P. The impact of online health information on patient health behaviours and making decisions concerning health. International journal of environmental research and public health. 2020 Feb;17(3):880. https://doi.org/10.3390/ijerph17030880
10. Chen YY, Li CM, Liang JC, Tsai CC. Health information obtained from the internet and changes in medical decision making: questionnaire development and cross-sectional survey. Journal of medical Internet research. 2018 Feb 12;20(2):e47. https://doi.org/10.2196/jmir.9370
11. Kaplan B. Revisiting health information technology ethical, legal, and social issues and evaluation: telehealth/telemedicine and COVID-19. International journal of medical informatics. 2020 Nov 1;143:104239. https://doi.org/10.1016/j.ijmedinf.2020.104239
12. Kokol P, Saranto K, BlažunVošner H. eHealth and health informatics competences: A systemic analysis of literature production based on bibliometrics. Kybernetes. 2018 May 2;47(5):1018-30. https://doi.org/10.1108/K-09-2017-0338
13. Ford D, Harvey JB, McElligott J, King K, Simpson KN, Valenta S, Warr EH, Walsh T, Debenham E, Teasdale C, Meystre S. Leveraging health system telehealth and informatics infrastructure to create a continuum of services for COVID-19 screening, testing, and treatment. Journal of the American Medical Informatics Association. 2020 Dec;27(12):1871-7. 10.1093/jamia/ocaa157
14. Xu J, Glicksberg BS, Su C, Walker P, Bian J, Wang F. Federated learning for healthcare informatics. Journal of healthcare informatics research. 2021 Mar;5:1-9. https://doi.org/10.1007/s41666-020-00082-4
15. Walonoski J, Kramer M, Nichols J, Quina A, Moesel C, Hall D, Duffett C, Dube K, Gallagher T, McLachlan S. Synthea: An approach, method, and software mechanism for generating synthetic patients and the synthetic electronic health care record. Journal of the American Medical Informatics Association. 2018 Mar 1;25(3):230-8.10.1093/jamia/ocx079
16. Alahmar A, Crupi ME, Benlamri R. Ontological framework for standardizing and digitizing clinical pathways in healthcare information systems. Computer Methods and Programs in Biomedicine. 2020 Nov 1;196:105559. https://doi.org/10.1016/j.cmpb.2020.105559
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Shilpi singh, Antaryami Pradhan.
Methodology: Shilpi singh, Antaryami Pradhan.
Software: Shilpi singh, Antaryami Pradhan.
Drafting - original draft: Shilpi singh, Antaryami Pradhan.
Writing - proofreading and editing: Shilpi singh, Antaryami Pradhan.