doi: 10.56294/mw2023130
ORIGINAL
Exploring Health Professionals’ Preparedness and Knowledge for Electronic Medical Record System Implementation in Hospitals
Exploración de la preparación y los conocimientos de los profesionales sanitarios para la implantación del sistema de historia clínica electrónica en los hospitales
Vishal Biswas1
![]() *, Satya Sundar Gajendra Mohapatra2
*, Satya Sundar Gajendra Mohapatra2
![]() , Pooja Varma3
, Pooja Varma3
![]()
1School of Allied Health Sciences, Noida International University. Greater Noida, Uttar Pradesh, India.
2IMS and SUM Hospital, Siksha ‘O’ Anusandhan (deemed to be University), Department of Radiology. Bhubaneswar, Odisha, India.
3JAIN (Deemed-to-be University), Department of Psychology. Bangalore, Karnataka, India.
Cite as: Biswas V, Gajendra Mohapatra SS, Varma P. Exploring Health Professionals’ Preparedness and Knowledge for Electronic Medical Record System Implementation in Hospitals. Seminars in Medical Writing and Education. 2023; 2:130. https://doi.org/10,56294/mw2023130
Submitted: 13-09-2022 Revised: 25-12-2022 Accepted: 28-02-2023 Published: 01-03-2023
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Vishal Biswas *
ABSTRACT
Health professionals use Electronic Medical Record (EMR) systems better to deliver healthcare services and enhance operational efficiency and patient safety as well as data management capabilities. EMR system implementation success depends mostly on health professional readiness and expertise because these professionals remain as the critical users of the system. The research evaluates how health personnel prepare and understand EMR hospital implementations. A total of 167 health professionals participated, and the questionnaire was pretested on a small sample to ensure clarity, reliability, and validity before full-scale implementation. IBM SPSS version 26.0 was used to examine the data and statistical techniques such as regression analysis, T-tests, and descriptive statistics were used. These methods were used to assess important elements influencing the adoption of EMRs, such as the readiness of healthcare professionals for system integration, their understanding of EMRs, their attitudes and perspectives, implementation obstacles, and their general level of preparedness. Findings revealed that only 25,3 % of health professionals demonstrated high preparedness, while 26,6 % had good knowledge of EMRs. Although 58,2 % viewed EMRs positively, 40,7 % expressed concerns, with 28,4 % citing increased workload and 24,1 % highlighting data security risks. Key barriers to EMR adoption included limited Information and Communication Technology (ICT) training, poor infrastructure, and resistance to change. The research found that readiness for EMR adoption was 54,2 %, significantly influenced by postgraduate education (p < 0,01) and EMR knowledge. Hospital staff needs developed organizational strategies and consistent technical assistance along with well-designed training programs to correctly adopt EMR systems.
Keywords: Health Professionals; Electronic Medical Record (EMR); Hospitals; Preparedness and Knowledge; Training Programs.
RESUMEN
Los profesionales sanitarios utilizan mejor los sistemas de historia clínica electrónica (HCE) para prestar servicios sanitarios y mejorar la eficiencia operativa y la seguridad de los pacientes, así como la capacidad de gestión de datos. El éxito de la implantación de sistemas de RME depende sobre todo de la preparación y los conocimientos de los profesionales sanitarios, ya que éstos siguen siendo los usuarios fundamentales del sistema. La investigación evalúa cómo se prepara y comprende el personal sanitario las implantaciones hospitalarias de RME. Participaron 167 profesionales sanitarios, y el cuestionario se sometió a una prueba previa en una pequeña muestra para garantizar su claridad, fiabilidad y validez antes de la implantación a gran escala. Para examinar los datos se utilizó la versión 26.0 de IBM SPSS y se emplearon técnicas estadísticas como el análisis de regresión, las pruebas T y la estadística descriptiva. Estos métodos se utilizaron para evaluar elementos importantes que influyen en la adopción de los RME, como la preparación de los profesionales sanitarios para la integración de sistemas, su comprensión de los RME, sus actitudes y perspectivas, los obstáculos a la implantación y su nivel general de preparación. Los resultados revelaron que sólo el 25,3 % de los profesionales sanitarios mostraba un alto grado de preparación, mientras que el 26,6 % tenía un buen conocimiento de los RME. Aunque el 58,2 % valoraba positivamente los RME, el 40,7 % expresaba su preocupación al respecto: el 28,4 % mencionaba el aumento de la carga de trabajo y el 24,1 %, los riesgos para la seguridad de los datos. Entre los principales obstáculos a la adopción de los RME se encuentran la escasa formación en tecnologías de la información y la comunicación (TIC), las deficiencias de las infraestructuras y la resistencia al cambio. El 54,2 % de los encuestados estaba dispuesto a adoptar los RME, lo que dependía en gran medida de la formación de posgrado (p < 0,01) y de los conocimientos sobre RME. El personal hospitalario necesita estrategias organizativas desarrolladas y una asistencia técnica constante, junto con programas de formación bien diseñados, para adoptar correctamente los sistemas de RME.
Palabras clave: Profesionales de la Salud; Historia Clínica Electrónica (HCE); Hospitales; Preparación y Conocimientos; Programas de Formación.
INTRODUCTION
Today's healthcare sector achieves greater operational success due to Electronic Medical Record (EMR) systems, which have converted paper medical records into digital formats. A complete electronic version of patient paper records, known as EMR, assists in recording patient data electronically for management purposes.(1) EMRs contain all crucial patient information, which includes medical records along with diagnosis procedures and medication profiles together with test outcomes. The efficient sharing of patient data between healthcare providers through EMRs helps medical staff improve their delivery quality and speed of operations.(2,3) The move toward electronic healthcare documentation has become a fundamental driver for healthcare quality improvements because it cuts down errors while enhancing clinical results and enhancing office management work processes. The original goal behind EMR system implementations involved ensuring healthcare data can be accessed simultaneously between hospital care facilities and outpatient clinics. EMR systems have developed new functional capabilities throughout the years to offer decision support tools to providers while providing data analysis functions for monitoring treatment results.(4) Authorities and healthcare organizations at present acknowledge EMR systems' significance, providing benefits and setting rules for entities. EMR system success demands substantial training and preparedness of healthcare providers to operate these systems competently because it remains the main focus in healthcare technology integration. The introduction of EMR systems serves healthcare by advancing patient care quality and operational effectiveness as well as provider-to-provider communication.(5) Healthcare facilities use EMRs as digital record systems to store patient data instead of relying on error-prone manual records that are subject to loss and extended delays in access time. Healthcare professionals can obtain complete patient histories from EMR systems, which helps in creating better treatment decisions. EMR systems enhance patient safety because it generates real-time alerts about medication dangers and other critical health issues involving allergies.(6,7) The implementation of EMR systems promotes administrative efficiency through streamlined operations and decreases costs as well as maximizes resource utilization beyond patient-oriented benefits. These systems help medical organizations meet health legislation requirements for maintaining data privacy and security standards. Medical facilities can utilize EMRs to perform data analysis for research and policymaking purposes, which drives healthcare improvements that benefit public health results.(8,9) The execution of EMR systems with hospitals for successful implementation depends entirely on healthcare professionals who actively participate and show readiness for use. Medical staff and nurses alongside administrative personnel hold essential roles in achieving flawless implementation of EMR systems and optimal workflow in healthcare facilities.(10) Health professionals need to actively participate as system interactions determine the effectiveness of EMRs for improving patient care quality and error reduction while streamlining administrative processes. Health professionals need both technical skills to manage the EMR system and complete understanding of how it enhances patient care management along with clinical decision-support capabilities. Healthcare providers successfully operate EMR tools by receiving the right training and supportive practices.(11) The effectiveness of EMR integration requires a positive mindset toward technology adoption, as refusal of change acts as a barrier to system integration success. Medical personnel can view EMRs as practice-assisting technological tools instead of practice-disrupting systems. EMR system implementation success depends directly on the preparedness along with the knowledge levels of health professionals. The long-term achievement of digital health initiatives depends heavily on providing healthcare workers with enough education, practical training, and continuous support.(12)
Healthcare organizations encounter multiple difficulties when integrating and using Electronic Medical Record systems in hospitals. Several barriers hinder EMR system adoption by healthcare professionals including staff reluctance to change, doubts about user-interface, underprepared staff, and insufficient support staffs. Hospitals avoid complete EMR system adoption mostly because of implementation expenses, privacy and security concerns regarding data while simultaneously facing resistance from healthcare staff. To tackle the above-mentioned concerns, the research considered descriptive statistics, T-tests, and regression analysis that were performed to assess key factors influencing EMR adoption, including preparedness, knowledge of EMRs, attitudes, and perceptions, barriers to implementation, and overall readiness.
The standard of medical treatment provided by two state hospitals in Jordan used paper-based and EMR. The results indicate that hospitals that have used EMRs have improved efficiency, availability, fulfillment, and privacy.(13) In Bangladesh's healthcare system, doctors' use of Electronic Health Records (EHR) is greatly influenced by societal impact, enabling circumstances, and individual information technology (IT) innovation. It recommends politicians create plans, guarantee technical adequacy, and offer instruction.(14) Physicians and nurses in Finland report better technical performance, but less work support and poorer usability. Reactive problem-solving instead of proactive benefit realization results from post-implementation events that defy pre-implementation expectations.(15) Most people’s health information can be accessed by a third party and that can face prejudice. The majority of doctors were concerned about patient safety but disagreed that EHRs can ruin the doctor-patient relationship.(16) Norway plans to introduce Epic, which was anticipated to provide better care more effectively while taking inspiration from Denmark's experiences. However, there was a lot of uncertainty around the implementation in Norway.(17) Decentralized computationally scalable solutions are being used more and more in the healthcare industry to address complex issues. The findings demonstrate that it converges more quickly than centralized techniques and has less communication overhead than other distributed algorithms while producing predictions with comparable accuracy.(18) Privacy, security, and quality enhancement are the main concerns of health information technology, mobile health, and electronic health records. Scholars in healthcare informatics can use this thorough knowledge structure to pinpoint research areas and select initiatives in the expanding field of e-health.(19) Cultural, financial, organizational, personal, technological, legal, and regulatory concerns are among the main obstacles. Health initiatives can concentrate on including the lack of money, poor system quality, resistance from doctors and patients, insufficient infrastructure, and a lack of information technology training to increase access to health information, services, and training.(20)
METHOD
EMR investigates the readiness and information level of medical workers when handling hospital EMR system implementation practices. The analysis investigates factors that influence the user acceptability of these systems together with obstacles encountered in system implementation. The investigation targets two main approaches for better-involving healthcare staff and better managing EMR system deployment to achieve superior clinical results and operational effectiveness. Figure 1 presents the schematic diagram of the methodology flow.
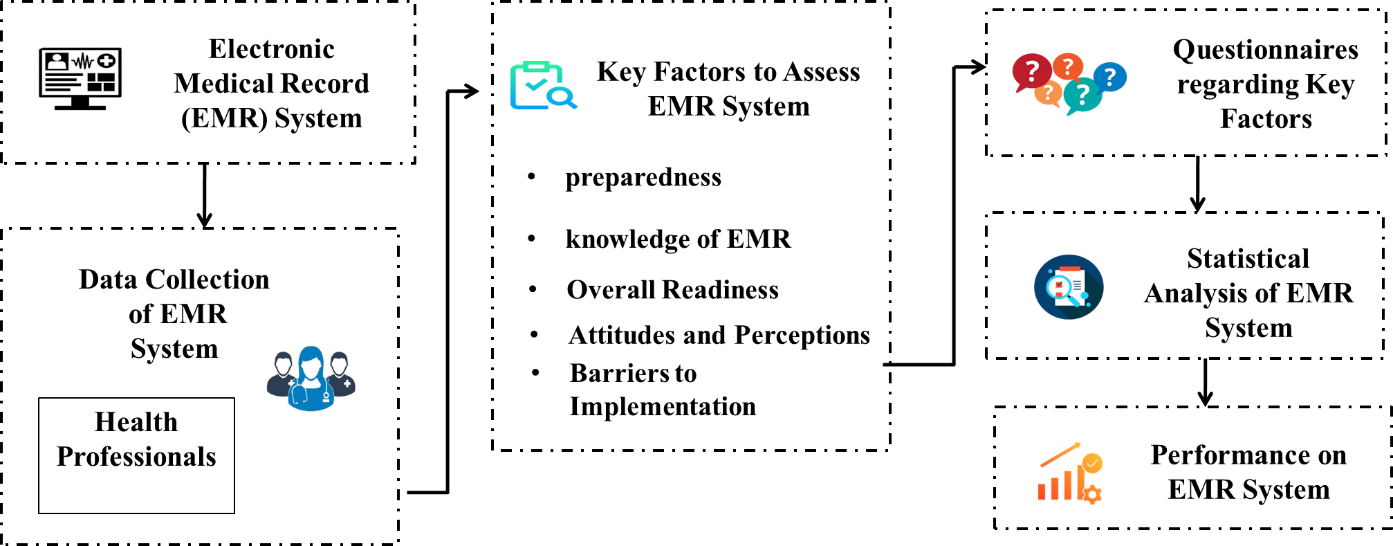
Figure 1. Schematic diagram of methodology flow
Data collection
The 167 medical professionals participated in the research, offering insightful information about readiness and expertise for the deployment of EMR systems in hospitals. The research focuses on important elements that impact the adoption of EMRs, such as preparedness, knowledge of EMRs, attitudes, and perceptions, barriers to implementation, overall readiness, comprehension of EMR features, and readiness to use the system. It also evaluates healthcare professionals' general preparedness to interact with EMR systems and tackles obstacles to successful EMR adoption, such as reluctance to change and a lack of training.
Key factors to assess EMR system
The assessment of EMR implementation requires evaluations to determine the preparedness of healthcare workers as well as technological proficiency and system operation effectiveness. The assessment process requires data collection on how new technological adoption affects care quality and how it impacts healthcare services. EMR integration requires identifying key obstacles, which include problems with infrastructure time limitations and staff resistance to change.
Preparedness
All hospitals need proper preparedness to implement EMR systems successfully throughout facilities. The factor demonstrates how well employees accept and effectively utilize new technology in work processes. The ability to successfully implement an EMR system requires staff members to understand system functionality, and learn how to use the interface. Complete training along with simple communication about system benefits is required to develop readiness within healthcare staff. The successful implementation of EMR systems depends on completing thorough training for healthcare professionals before launch because trained staff adopts systems better while reducing an error, which leads to better operational output and better health system performance.
Knowledge of EMR
Healthcare workers need appropriate implementation experience in hospital environment to use EMR systems effectively. Better system operation and improved patient care are made possible by the efficient use of patient data management along with an understanding of documentation and decision support tools. While unskilled users tend to ignore the system, which causes operational setbacks, EMR users with extensive system knowledge prevent error during practice. Employers can give employees ongoing support since it improves training results and facilitates transitions, which fosters a favorable opinion of EMRs and determines preparedness for a successful rollout of these systems.
Attitudes and perceptions
Healthcare professionals' preparedness for EMR implementation and technology knowledge follow directly from attitudes regarding the system. Positive thinking helps medical staff exceed resistance barriers and participate actively. The acceptance of EMRs alongside patient welfare and improved work processes leads healthcare staff to adopt the system through proper education. The obstacles that emerge from negative views, including system problems and increased workload, challenge healthcare professionals, together with effective communication strategies coupled with organizational support, the basis to change staff perspectives was created and competence in the daily operational use of EMRs was provided.
Barriers to implementation
The barriers that emerge during implementation deeply influence the extent to which health professionals develop readiness for participating with EMR systems. The implementation of new systems is hindered by three main barriers, which consist of insufficient training the absence of technical support and resistance to system change. The lack of proper education and limited practical exposure causes health professionals to lose confidence in using electronic medical records systems, which results in inefficient patient care and error. Implementation becomes difficult when users show negative attitudes toward the system due to skepticism about its adoption. Health professionals need complete training with clear communication and ongoing assistance to achieve full readiness and implement EMR systems effectively in hospital environment.
Overall readiness
Health professionals require overall readiness as fundamental benchmark to obtain sufficient EMR system implementation preparation and knowledge for hospitals. The implementation of digital tools requires an assessment of training options and staff knowledge about technology together with reception of modern systems. The organizational support for EMR integration includes all necessary infrastructure, designed systems, and sufficient resources. Health professionals demonstrate readiness when successfully adapting to system features for efficient performance and daily integration of EMR in clinical work. The way healthcare professionals approach change together with their perception of EMR advantages significantly impacts system usage. Sophisticated EMR systems encounter difficulties when users do not receive proper preparation, which results in inadequate system implementation and negative reception by users.
Questionnaires regarding key factors
Health professionals undergo questionnaire assessments to determine system implementation readiness by testing preparedness together with knowledge and attitudes as well as perceptions of the system as shown in table 1. These factors focus on technological skills, training backgrounds as well as the benefits, adoption challenges and organizational preparedness.
|
Table 1. Questionnaires regarding key factors |
||
|
Factors |
Questionnaires (Q) number |
Question’s |
|
Preparedness |
Q1 |
How confident are using the EMR system effectively in daily tasks? |
|
Q2 |
Whether receive adequate training on the EMR system before implementation? |
|
|
Knowledge of EMR |
Q3 |
How well do health professionals understand the features and functions of the EMR system? |
|
Q4 |
To what extent are health professionals prepared to troubleshoot or resolve the EMR system? |
|
|
Attitudes and perceptions |
Q5 |
How do health professionals perceive the impact of EMR on patient care and workflow efficiency? |
|
Q6 |
What is the general attitude toward adopting digital health solutions, such as the EMR system, among health professionals? |
|
|
Barriers to implementation |
Q7 |
What challenges or obstacles do health professionals face in using the EMR system daily? |
|
Q8 |
How satisfied are health professionals with the infrastructure and support provided for the EMR system in the hospital? |
|
|
Overall readiness |
Q9 |
How prepared are health professionals to fully integrate EMR into work processes? |
|
Q10 |
Does the current hospital environment support successful EMR implementation according to health professionals? |
|
Statistical analysis
The IBM SPSS software version of 26.0 has been utilized in the research. The evaluation used descriptive statistics and t-tests alongside regression analysis to determine the main factors that drive EMR adoption. The survey data was presented through descriptive statistics models followed by t-tests, which evaluated differences in the factors. The relationships between variables were analyzed through regression analysis because it examined both knowledge of EMRs and barriers to implementation and readiness status for predictive effects on hospital EMR adoption success.
Performance Analysis of The EMR System
Evaluation of EMR system performance was assessed through dimensions involving system efficiency and usability and health care outcome effectiveness. The EMR system evaluation depends on five essential elements: preparedness, knowledge of EMRs, attitudes and perceptions, barriers to implementation, and overall readiness for health professionals. Well-functioning EMR technology enables enhanced workflows combined with reduced error that result in better patient care, thus leading to more efficient hospital operations.
Demographic characteristics of health professionals
Diverse professionals from doctors to nurses and administrative staff who show different levels of experience in healthcare made up the health professional participants. A diverse range of clinical and non-clinical hospital personnel participated to acquire a comprehensive understanding of EMR system implementation. The research used a sample that combined participants from different age groups with both male and female members and professionals at various educational stages to create an extensive understanding of demographic characteristics affecting preparedness along with EMR implementation knowledge and attitudes. Table 2 depicts the demographic characteristics of health professionals. Figure 2 presents demographic characteristics of health professionals: (a) age range and (b) years of experience.
|
Table 2. Demographic characteristics of health professionals |
|||
|
Categories |
n=167 |
Percentage (%) |
|
|
Gender |
Male |
92 |
55,1 |
|
Female |
75 |
44,9 |
|
|
Age Range |
18-25 |
98 |
58,7 |
|
26-35 |
43 |
25,7 |
|
|
36+ |
26 |
15,6 |
|
|
Years of Experience |
1-3 Years |
105 |
62,9 |
|
4-6 Years |
40 |
23,9 |
|
|
7+ Years |
22 |
13,2 |
|
|
Professional Role |
Doctors |
60 |
35,9 |
|
Nurses |
57 |
34,1 |
|
|
Administrative Staff |
50 |
30,0 |
|
|
ICT Training |
Yes |
85 |
50,9 |
|
No |
82 |
49,1 |
|
|
Hospital Type |
Public |
107 |
64,1 |
|
Private |
60 |
35,9 |
|
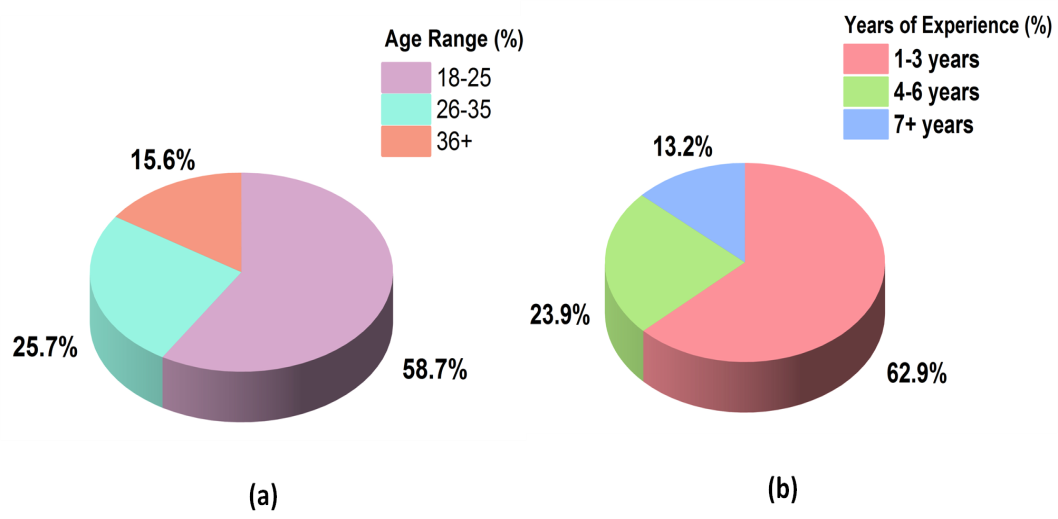
Figure 2. Demographic characteristics of health professionals (a) age range and (b) years of experience
Descriptive statistics
The collected data from health professionals regarding EMR system preparation and understanding was summarized through descriptive statistics analysis. Descriptive analysis measures, including means, standard deviations, frequencies, and percentages, served to understand the distribution of survey responses. The analysis revealed statistical insights regarding how many health professionals showed readiness or had good attitudes toward electronic medical records systems. As shown in equation (1), the initial analysis through descriptive statistics enabled researchers to obtain a better understanding of hospital health professional readiness and knowledge and concerns about EMR system implementation. Table 3 illustrates the quantitative values of descriptive statistics.
![]()
|
Table 3. Quantitative values of descriptive statistics |
||||
|
Factors |
Minimum |
Maximum |
Mean |
SD |
|
Preparedness |
1 |
5 |
2,4 |
1,1 |
|
Knowledge of EMRs |
1 |
5 |
2,6 |
1,0 |
|
Attitude and Perceptions |
1 |
5 |
3,4 |
0,9 |
|
Barriers to Implementation |
1 |
5 |
3,1 |
1,2 |
|
Overall Readiness |
1 |
5 |
29 |
1,0 |
|
Note: Standard Deviation (SD) |
||||
T- Test
The T-test serves as a statistical procedure that helps to identify major mean discrepancies between factors. Determining significant mean variations between health professional groups regarding EMR-related preparedness and knowledge levels and attitude stands utilizes the t-test in EMR system implementation environments. The t-test assessment method examines how statistically important the observed differences in factors appear or random occurrences. The analysis uncovers critical information about weak points that direct training activities and EMR system implementation strategies as well as healthcare delivery improvements. Table 4 shows the quantitative values of the T-test. The mean of the T-test is calculated based on equation (2).
|
Table 4. Quantitative values of T-test |
||||||
|
Factors |
n=167 |
Mean |
t-Statistic |
df |
p-value |
Interpretation |
|
Preparedness |
167 |
2,4 |
-8,56 |
166 |
0,0001 |
Significant |
|
Knowledge of EMRs |
167 |
2,6 |
-5,45 |
166 |
0,00001 |
Significant |
|
Attitude and Perceptions |
167 |
3,4 |
3,23 |
166 |
0,0015 |
Significant |
|
Barriers to Implementation |
167 |
3,1 |
1,81 |
166 |
0,073 |
Not Significant |
|
Overall Readiness |
167 |
2,9 |
-3,23 |
166 |
0,0015 |
Significant |
|
Note: Degrees of Freedom (df) |
||||||
Regression analysis
Regression analysis techniques are investigating the connection between EMR implementation readiness factors consisting of preparedness alongside knowledge and attitudes and barriers to implementation. Through analysis of these variables, the research aimed to determine what factors most influenced health professional readiness levels regarding EMR system usage. Adequate training combined with positive technological attitudes proved to be substantial indicators that directly enhanced preparedness and knowledge. Analysis through regression determined both higher workload expectations and lack of assistance as key factors that diminished general readiness levels. The research discovered essential variables that healthcare organizers can focus on to enhance the implementation of EMR systems. Table 5 depicts the quantitative values of regression analysis. The mathematical regression analysis is as shown in equation (3).
![]()
|
Table 5. Quantitative values of regression analysis |
|||||
|
Factors |
Coefficient |
SE |
t-value |
p-Value |
R-Squared Contribution (%) |
|
Preparedness |
0,350 |
0,100 |
3,50 |
<0,01 |
14,3 |
|
Knowledge of EMRs |
0,250 |
0,080 |
3,13 |
<0,01 |
12,5 |
|
Attitude and Perceptions |
0,150 |
0,070 |
2,14 |
0,03 |
7,5 |
|
Barriers to Implementation |
-0,200 |
0,090 |
-2,22 |
0,02 |
-6,0 |
|
Overall Readiness |
0,450 |
0,110 |
4,09 |
<0,01 |
54,2 |
|
Note: Standard Error (SE) |
|||||
Impact of EMR adoption
Health professionals reacted differently to the implementation of EMRs. The survey participants indicated that 25,3 % of health professionals were well-prepared for system use, yet 26,6 % possessed a satisfactory level of understanding about EMR functionalities. 58,2 % of the respondents saw advantages in EMRs because it improved both clinical processes and patient treatment, but 40,7 % had negative opinions. Increased workload stood out to 28,4 % of the health professionals who criticized the EMR system because many reported being inundated by the administrative tasks associated with it. The concerns about data security risks were identified by 24,1 % of respondents who showcased worries regarding patient privacy and information protection. The research outcomes show that healthcare professionals need specific training together with support because these measures can boost EMR adoption success in medical facilities. Table 6 and figure 3 presents the numerical outcomes of the impact of EMR adoption.
|
Table 6. Numerical outcomes in the impact of EMR adoption |
|
|
Factors |
Percentage of EMR adoption (%) |
|
High Preparedness |
25,3 |
|
Good Knowledge of EMRs |
26,6 |
|
Positive View of EMRs |
58,2 |
|
Concerns About EMRs |
40,7 |
|
Increased Workload |
28,4 |
|
Data Security Risks |
24,1 |
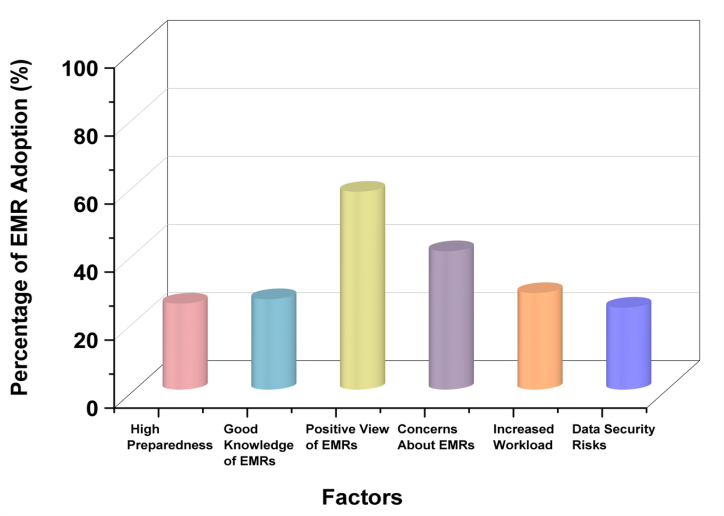
Figure 3. Graphical representation in the impact of EMR adoption
CONCLUSIONS
The health professional’s preparedness and knowledge stands were considered essential for the effective EMR system implementation success demonstrated in the research. The implementation of EMR systems received generally positive feedback from most health professionals, but it faced difficulties because of insufficient ICT education along with insufficient infrastructure and resistance to change. The research found that readiness for EMR adoption was 54,2 %, significantly influenced by postgraduate education (p < 0,01) and EMR knowledge. Postgraduate education and EMR understanding are crucial to developing readiness to research findings because hospital staff needs well-designed training alongside technical assistance to successfully implement these systems. Self-reported data collection with the research presents a limitation because it contains unfair responses. Future research can extend the effects of ongoing training methods while investigating hospital administration strategies in developing positive working conditions for EMR system acceptance.
BIBLIOGRAPHIC REFERENCES
1. Van Velthoven MH, Cordon C, Challagalla G. Digitization of healthcare organizations: The digital health landscape and information theory. International journal of medical informatics. 2019 Apr 1;124:49-57. https://doi.org/10,1016/j.ijmedinf.2019,01.007
2. Ahmad RW, Salah K, Jayaraman R, Yaqoob I, Ellahham S, Omar M. The role of blockchain technology in telehealth and telemedicine. International journal of medical informatics. 2021 Apr 1;148:104399. https://doi.org/10,1016/j.ijmedinf.2021,104399
3. Asi YM, Williams C. The role of digital health in making progress toward Sustainable Development Goal (SDG) 3 in conflict-affected populations. International journal of medical informatics. 2018 Jun 1;114:114-20. https://doi.org/10,1016/j.ijmedinf.2017,11.003
4. Goss FR, Blackley SV, Ortega CA, Kowalski LT, Landman AB, Lin CT, Meteer M, Bakes S, Gradwohl SC, Bates DW, Zhou L. A clinician survey of using speech recognition for clinical documentation in the electronic health record. International journal of medical informatics. 2019 Oct 1;130:103938. https://doi.org/10,1016/j.ijmedinf.2019,07.017
5. Walsh KE, Secor JL, Matsumura JS, Schwarze ML, Potter BE, Newcomer P, Kim MK, Bartels CM. Secure provider-to-provider communication with electronic health record messaging: an educational outreach study. Journal for Healthcare Quality. 2018 Sep 1;40(5):283-91. https://doi.org/10,1016/j.imu.2019,100182
6. Cabitza F, Campagner A. The need to separate the wheat from the chaff in medical informatics: Introducing a comprehensive checklist for the (self)-assessment of medical AI studies. International Journal of Medical Informatics. 2021 Sep 1;153:104510. https://doi.org/10,1016/j.ijmedinf.2021,104510
7. Sanchez-Pinto LN, Venable LR, Fahrenbach J, Churpek MM. Comparison of variable selection methods for clinical predictive modeling. International journal of medical informatics. 2018 Aug 1;116:10-7. https://doi.org/10,1016/j.ijmedinf.2018,05.006
8. Chen Y, Yang L, Zhang M, Yang J. Central or peripheral? Cognition elaboration cues’ effect on users’ continuance intention of mobile health applications in the developing markets. International journal of medical informatics. 2018 Aug 1;116:33-45. https://doi.org/10,1016/j.ijmedinf.2018,04.008
9. Chen PT, Lin CL, Wu WN. Big data management in healthcare: Adoption challenges and implications. International Journal of Information Management. 2020 Aug 1;53:102078. https://doi.org/10,1016/j.ijinfomgt.2020,102078
10. Wang H, Tao D, Yu N, Qu X. Understanding consumer acceptance of healthcare wearable devices: An integrated model of UTAUT and TTF. International journal of medical informatics. 2020 Jul 1;139:104156. https://doi.org/10,1016/j.ijmedinf.2020,104156
11. Tajirian T, Stergiopoulos V, Strudwick G, Sequeira L, Sanches M, Kemp J, Ramamoorthi K, Zhang T, Jankowicz D. The influence of electronic health record use on physician burnout: cross-sectional survey. Journal of medical Internet research. 2020 Jul 15;22(7):e19274. https://doi.org/10,2196/19274
12. Rajabion L, Shaltooki AA, Taghikhah M, Ghasemi A, Badfar A. Healthcare big data processing mechanisms: The role of cloud computing. International Journal of Information Management. 2019 Dec 1;49:271-89. https://doi.org/10,1016/j.ijinfomgt.2019,05.017
13. Ayaad O, Alloubani A, ALhajaa EA, Farhan M, Abuseif S, Al Hroub A, Akhu-Zaheya L. The role of electronic medical records in improving the quality of health care services: Comparative study. International journal of medical informatics. 2019 Jul 1;127:63-7. https://doi.org/10,1016/j.ijmedinf.2019,04.014
14. Hossain A, Quaresma R, Rahman H. Investigating factors influencing the physicians’ adoption of electronic health record (EHR) in healthcare system of Bangladesh: An empirical study. International Journal of Information Management. 2019 Feb 1;44:76-87. https://doi.org/10,1016/j.ijinfomgt.2018,09.016
15. Rajaram A, Hickey Z, Patel N, Newbigging J, Wolfrom B. Training medical students and residents in the use of electronic health records: a systematic review of the literature. Journal of the american medical informatics association. 2020 Jan;27(1):175-80. https://doi.org/10,1093/jamia/ocz178
16. Entzeridou E, Markopoulou E, Mollaki V. Public and physician’s expectations and ethical concerns about electronic health record: Benefits outweigh risks except for information security. International journal of medical informatics. 2018 Feb 1;110:98-107. https://doi.org/10,1016/j.ijmedinf.2017,12.004
17. Hertzum M, Ellingsen G. The implementation of an electronic health record: Comparing preparations for Epic in Norway with experiences from the UK and Denmark. International journal of medical informatics. 2019 Sep 1;129:312-7. https://doi.org/10,1016/j.ijmedinf.2019,06.026
18. Brisimi TS, Chen R, Mela T, Olshevsky A, Paschalidis IC, Shi W. Federated learning of predictive models from federated electronic health records. International journal of medical informatics. 2018 Apr 1;112:59-67. https://doi.org/10,1016/j.ijmedinf.2018,01.007
19. Gu D, Li T, Wang X, Yang X, Yu Z. Visualizing the intellectual structure and evolution of electronic health and telemedicine research. International journal of medical informatics. 2019 Oct 1;130:103947. https://doi.org/10,1016/j.ijmedinf.2019,08.007
20. Al-Samarraie H, Ghazal S, Alzahrani AI, Moody L. Telemedicine in Middle Eastern countries: Progress, barriers, and policy recommendations. International journal of medical informatics. 2020 Sep 1;141:104232. https://doi.org/10,1016/j.ijmedinf.2020,104232
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Vishal Biswas, Satya Sundar Gajendra Mohapatra, Pooja Varma.
Methodology: Vishal Biswas, Satya Sundar Gajendra Mohapatra, Pooja Varma.
Software: Vishal Biswas, Satya Sundar Gajendra Mohapatra, Pooja Varma.
Drafting - original draft: Vishal Biswas, Satya Sundar Gajendra Mohapatra, Pooja Varma.
Writing - proofreading and editing: Vishal Biswas, Satya Sundar Gajendra Mohapatra, Pooja Varma.