doi: 10.56294/mw2023132
ORIGINAL
Investigating the Impact of Cloud-Based Technologies on Healthcare Accessibility and Service Efficiency
Investigación del impacto de las tecnologías basadas en la nube en la accesibilidad y la eficiencia de los servicios sanitarios
Snehanshu Dey1 ![]() *,
Suhas Ballal2
*,
Suhas Ballal2 ![]() , Avinash Kumar3
, Avinash Kumar3 ![]()
1IMS and SUM Hospital, Siksha ‘O’ Anusandhan (deemed to be University), Department of Psychiatry. Bhubaneswar, Odisha, India.
2School of Sciences, JAIN (Deemed-to-be University), Department of Biochemistry. Karnataka, India.
3Noida International University, Department of ENT. Greater Noida, Uttar Pradesh, India.
Cite as: Dey S, Ballal S, Kumar A. Investigating the Impact of Cloud-Based Technologies on Healthcare Accessibility and Service Efficiency. Seminars in Medical Writing and Education. 2023; 2:132. https://doi.org/10.56294/mw2023132
Submitted: 13-09-2022 Revised: 25-12-2022 Accepted: 28-02-2023 Published: 01-03-2023
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Snehanshu Dey *
ABSTRACT
Cloud computing has significantly transformed healthcare by providing enhanced remote access and improving service delivery efficiency. Despite its promise, there are indeed obstacles to its general acceptance, especially in developing nations where concerns about data security and underuse of ICTs prevent adoption. Research examines the factors influencing healthcare consumers’ attitudes toward adopting cloud-based health systems, focusing on accessibility and service efficiency. A survey of 530 participants was conducted, and SPSS and factors were employed to examine the data. The results identify eight key factors that significantly impact healthcare consumers’ behavioral intentions to adopt cloud-based healthcare technologies: perceived usefulness, facilitating conditions, performance expectancy, information sharing, social influence, and trust in technology, effort expectancy, and data security. However, Cloud-based health information was shown with no discernible effect. These findings underscore the importance of addressing consumer concerns, particularly related to security and system integration, to ensure the effective deployment of cloud-based medical centers. Such systems have the potential to improve healthcare access, especially in underserved and rural areas, while enhancing the overall efficiency of service delivery. The research suggests that healthcare policymakers and technology developers must prioritize these factors to foster greater adoption of cloud-based technologies within healthcare systems.
Keywords: Cloud Computing; Healthcare Accessibility; Service Efficiency; Adoption Factors; Data Security.
RESUMEN
La computación en nube ha transformado significativamente la atención sanitaria al proporcionar un mayor acceso remoto y mejorar la eficiencia en la prestación de servicios. A pesar de sus promesas, existen obstáculos para su aceptación general, especialmente en los países en desarrollo, donde la preocupación por la seguridad de los datos y la infrautilización de las TIC impiden su adopción. La investigación examina los factores que influyen en la actitud de los consumidores sanitarios hacia la adopción de sistemas sanitarios basados en la nube, centrándose en la accesibilidad y la eficiencia de los servicios. Se realizó una encuesta a 530 participantes y se emplearon SPSS y factores para examinar los datos. Los resultados identifican ocho factores clave que influyen significativamente en la intención de los consumidores sanitarios de adoptar tecnologías sanitarias basadas en la nube: utilidad percibida, condiciones facilitadoras, expectativa de rendimiento, intercambio de información, influencia social y confianza en la tecnología, expectativa de esfuerzo y seguridad de los datos. Sin embargo, la información sanitaria basada en la nube no mostró ningún efecto perceptible. Estos resultados subrayan la importancia de abordar las preocupaciones de los consumidores, en particular las relacionadas con la seguridad y la integración de sistemas, para garantizar la implantación eficaz de los centros médicos basados en la nube. Estos sistemas tienen el potencial de mejorar el acceso a la atención sanitaria, especialmente en zonas rurales y desatendidas, al tiempo que aumentan la eficiencia general de la prestación de servicios. La investigación sugiere que los responsables de las políticas sanitarias y los desarrolladores de tecnología deben dar prioridad a estos factores para fomentar una mayor adopción de las tecnologías basadas en la nube dentro de los sistemas sanitarios.
Palabras clave: Computación en Nube; Accesibilidad Sanitaria; Eficiencia de los Servicios; Factores de Adopción; Seguridad de los Datos.
INTRODUCTION
Modern healthcare services and patient care have been revolutionized by adopting cloud-based technologies.(1) The worldwide medical field needs efficient and accessible solutions because cloud computing enables scalable management of data together with remote healthcare and real-time professional collaboration.(2) The innovations enable remote areas and underserved populations to get quality healthcare immediately by overcoming geographic obstacles. Cloud-based platforms assist with healthcare operation optimization through their essential functions.(3) Incorporating EHRs and telemedicine treatments streamlines administrative processes, reduces redundancy, and improves coordination among healthcare providers.(4) Digital data processing and cloud-based analytics improve clinical decision-making, resulting in more precise diagnoses and faster interventions.(5) Security features of cloud storage protect medical records while making them accessible for swift retrieval, thus preventing errors during patient care delivery. The latest innovations in the industry yet face multiple existing hurdles.(6) Various difficulties indeed need to be addressed. Healthcare organizations using cloud solutions need to protect their data while maintaining reliable systems, which are essential operations.(7) Healthcare accessibility together with service efficiency continues to develop in significance as cloud computing evolves. Cloud technologies will reshape the future of patient-centered care together with medical service delivery at an international level through enhanced connectivity reduced administrative burdens and digital healthcare support.(8) Research uses CP-ABE to present a very fine control of data access approach for wireless IoT.(9) The approach conceals attribute information using an imprecise placement method based on a corrupted Bloom filter, ensuring data security and privacy through a randomized retrieval policy. The suggested approach delivers little data processing and storage expense while effectively protecting decision secrecy. Cloud computing, the IoT, and mechanization are some of the advancements that smart architecture uses for effective administration.(10) Smart health care systems (SMS) make use of devices with sensors and communication networks. For cloud-assisted SMS, an identification infrastructure based on ECC is developed to ensure mutual authentication, efficient computation, and communication while maintaining security and privacy. To address any risks to data security and privacy, research suggests an encrypted access mechanism for storing in the cloud electronic medical facilities.(11) Multiple keys created using the KDF have been employed in the encryption protocol to guard against abuse and guarantee end wise statistics ciphering. To defend anonymity, permission to use cloud services is predicated on the affiliation and identification of the parties involved. The straightforward and reliable plan is the greatest solution for safeguarding data confidentiality and security in cloud-based electronic healthcare services. Scalability, data storage enhancement, and AI-machine learning cooperation are all provided by cloud-based healthcare computing.(12) This research investigates the use of clever strategies in medical facilities, with a focus on concerns regarding security and privacy. It discusses the growing need for cloud computing, who it affects, and the opportunities and difficulties of putting these developments into practice. The research paper examines the literature on several strategies and a system employed to address security and privacy worries, e-Health noting the advantages and disadvantages of each model. Research examines several e-health security and privacy strategies, with an emphasis on cloud-based models.(13) Along with discussing the rules surrounding HIPAA, it offers a common definition of e-health and categorizes cloud-based models. The authors provide a secure framework for digital health records that guarantees effectiveness, dependability, and controlled contact with medical data. A secure, cost-effective cloud-based architecture for the healthcare industry that ensures privacy protection; it focuses on the EHR system, which uses multi-authority ciphertext-policy attribute-based security to enable precise control of access.(14) The system, which incorporates multifaceted application identification, attempts to give residents access to government-provided healthcare and other amenities. Cloud-based computing services have improved patient care by revolutionizing the handling of health information.(15) Advanced cloud services are available from the top three suppliers: Microsoft, Amazon, and Google. For safe data ingestion, storage, and analysis, to make the most of these services, a framework is suggested. The goal of this investigation database is to create a versatile informatics structure for telemedicine, which will improve the healthcare ecosystem by extending interconnection between telemedicine, IoT e-health, and hospital information systems.(16) This examines technological burdens and suggests ways to improve healthcare service levels using Sensor Hub and IoT technology. To enhance customer confidentiality as well as protection, this research proposes a smart service authenticating architecture for Telecommuting Medical Information Systems (TMIS).(17) To improve reciprocal authenticity, the framework cross-examines shared secret session keys between communication entities. The suggested framework's security features were confirmed through both official and informal verification techniques.
METHOD
Data collected from 530 respondents are used to analyze factors that could influence the implementation of cloud-based technologies in healthcare. The hypothesis were tested and the correlations between the concepts were established using modeling with SEM. Mediation and hierarchical regression analysis assessed direct and indirect effects. A correlation matrix was formed to evaluate inter-variable associations. Statistical analysis were used to ensure the reliability and strength of the results.
Data collection
A standardized questionnaire was used to collect data for this investigation from 530 patients in various locations. It was used to measure key determinants affecting cloud-based health systems' adoption, including perceived usefulness, effort expectancy, social influence, data security, and trust in technology. As shown in table 1, the characteristics of the subjects include gender, age, education, employment, localization, and prior knowledge of cloud-based health systems. This information aids in evaluating trends and variations in acceptance across groups. It is through this comprehension that one is enabled to detect the main barriers and facilitators of cloud-based health adoption, which will then allow programmers and technology developers to design targeted interventions for successful implementation and increased adoption.
|
Table 1. Demographic Characteristics of Healthcare Consumers for Cloud Adoption |
|||
|
Demographic Variable |
Category |
Frequency (N = 530) |
Percentage (%) |
|
Gender |
Men |
280 |
52,8 |
|
Women |
250 |
47,2 |
|
|
Age Group |
18–30 years |
180 |
34,0 |
|
31–45 years |
220 |
41,5 |
|
|
46+ years |
130 |
24,5 |
|
|
Education Level |
Secondary School |
160 |
30,2 |
|
Bachelor's Degree |
230 |
43,4 |
|
|
Postgraduate |
140 |
26,4 |
|
|
Employment Status |
Employed |
260 |
49,1 |
|
Unemployed |
140 |
26,4 |
|
|
Self-Employed |
130 |
24,5 |
|
|
Location |
Urban |
310 |
58,5 |
|
Rural |
220 |
41,5 |
|
|
Prior Knowledge of Cloud-Based Health Systems |
Yes |
320 |
60,4 |
|
No |
210 |
39,6 |
|
Enhancing healthcare access and efficiency through cloud-based technologies adoption
Cloud-based technologies have postponed the revolution of access and efficiency in healthcare through remote consultations, electronic health records, and real-time data exchange. These technologies tend to safeguard the way toward greater accessibility to all the citizens because of the pervasive improvement of geographic and economic difficulties in healthcare, especially in poorer areas. This research investigates the main factors affecting adoption by healthcare consumers of cloud-based systems, that is, perceived usefulness, effort expectancy in using the technology, social influence, data security, and trust in technology. Drawing on an analysis of consumer attitudes, barriers towards adoption and ways to enhance implementation are identified. The present findings provide key advice for legislators and technology businesses in the process of optimizing cloud-based healthcare solutions that would ensure seamless integration of the solutions with patient outcomes and operational efficiency. This is most important in reducing the fears relative to security, usability, and lattices to enhance acceptance and realize maximum benefits. This research contributes to the ongoing discourse on digital healthcare transformation by emphasizing consumer trust and system reliability, fostering widespread adoption and sustainable healthcare innovation.
Hypothesis pathway
The hypothesis suggests certain key factors that are presumed to influence the acceptance of cloud-based healthcare systems concerning user perceptions, trust, and security concerns. Insights from the research offer guides to policymakers and developers on ways to improve accessibility and efficiency. By identifying significant predictors, this research will also enable existing decision-makers to make informed decisions, thereby enabling the optimal use and acceptance of cloud-based healthcare. Table 2 presents the reliability and validity assessment of constructs, ensuring measurement consistency. Figure 1 illustrates the proposed hypothesis model, showing key predictors influencing BI and ACH.
|
Table 2. Proposed Hypothesis for Cloud-Based Healthcare Adoption |
|
|
Hypothesis |
Statement |
|
H1 |
BI has a positive impact on PU |
|
H2 |
BI has a positive influence on FC |
|
H3 |
BI has a positively affects on PE |
|
H4 |
BI significantly enhances IS |
|
H5 |
BI positively impacts on SI |
|
H6 |
BI is a key factor in shaping TT |
|
H7 |
BI has a positive effect on EE |
|
H8 |
BI concerns negatively influence DS |
|
H9 |
BI positively affects the actual ACH |
|
H10 |
BI has no significant impact on CBHK |
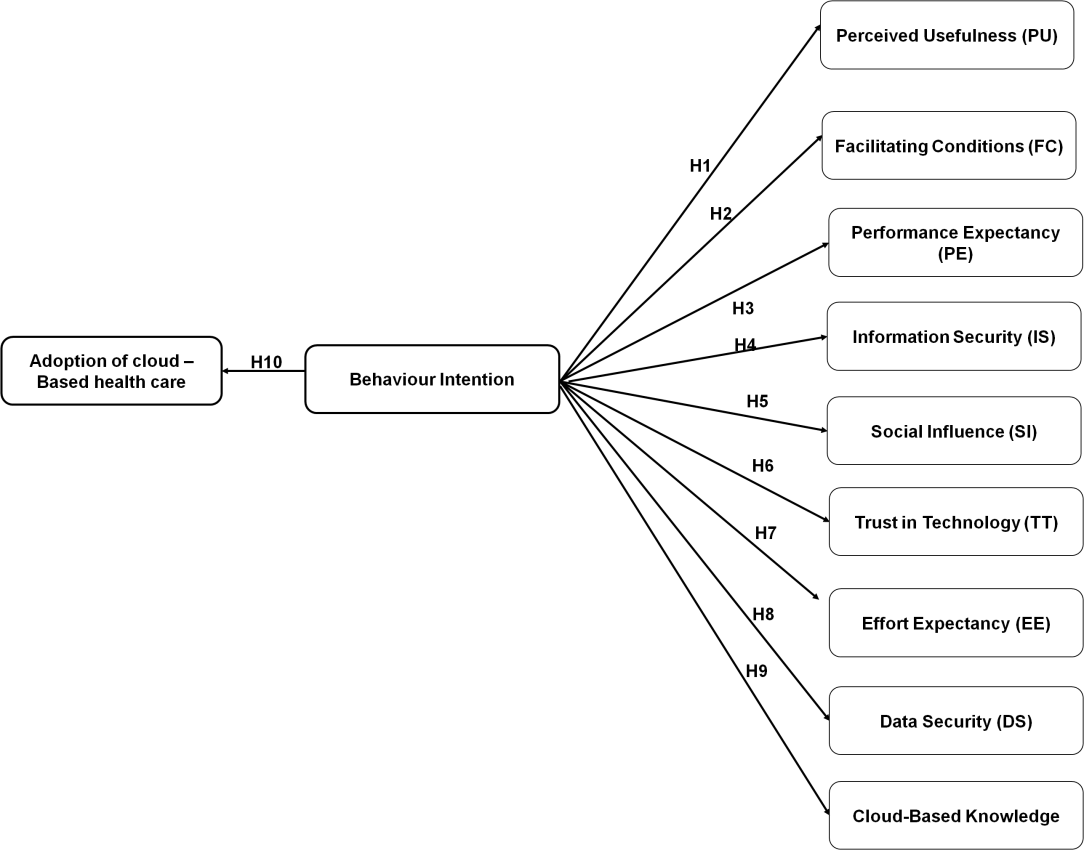
Figure 1. Conceptual Framework
Statistical Analysis
The factors influencing the adoption of cloud-based healthcare are analysed using hierarchical regression and mediation in IBM SPSS statistics version 30. Mediation analysis, using bootstrapping, examines the indirect effects of PU, FC, and other predictors on ACH through BI. Hierarchical regression assesses the incremental impact of BI on ACH, confirming its strong predictive role. ANOVA identifies key predictors, with DS negatively influencing adoption. These statistical methods ensure a comprehensive understanding of technology acceptance, highlighting BI as a crucial mediator and validating its significance in driving adoption through a structured, data-driven approach.
RESULTS
The findings highlight significant relationships among key variables, confirming hypothesized pathways. Statistical analysis, including mediation and hierarchical regression, demonstrate the impact of influential factors on adoption, offering valuable insights for practical applications. Table 3 provides factor loadings, the combined reliability, and the derived mean variation for various constructs, ensuring measurement reliability and validity. Each item represents a key factor influencing cloud-based healthcare adoption. High factor loadings indicate strong correlations between items and their respective constructs, while composite reliability and average variance extracted confirm internal consistency. This validation process supports structural equation modeling, hypothesis testing, and mediation analysis, strengthening the research's statistical foundation in assessing behavioral intentions and the adoption of cloud-based healthcare systems.
|
Table 3. Construct Reliability and Validity Assessment |
||||
|
Construct |
Item |
Factor Loading Value |
CR |
AVE |
|
PU |
PU1 |
0,82 |
0,89 |
0,72 |
|
PU2 |
0,85 |
|||
|
PU3 |
0,88 |
|||
|
FC |
FC1 |
0,80 |
0,88 |
0,65 |
|
FC2 |
0,83 |
|||
|
FC3 |
0,81 |
|||
|
FC4 |
0,79 |
|||
|
PE |
PE1 |
0,84 |
0,89 |
0,73 |
|
PE2 |
0,86 |
|||
|
PE3 |
0,87 |
|||
|
IS |
IS1 |
0,79 |
0,89 |
0,66 |
|
IS2 |
0,82 |
|||
|
IS3 |
0,85 |
|||
|
IS4 |
0,80 |
|||
|
SI |
SI1 |
0,81 |
0,89 |
0,67 |
|
SI2 |
0,84 |
|||
|
SI3 |
0,83 |
|||
|
SI4 |
0,79 |
|||
|
TT |
TT1 |
0,83 |
0,89 |
0,73 |
|
TT2 |
0,86 |
|||
|
TT3 |
0,88 |
|||
|
EE |
EE1 |
0,79 |
0,78 |
0,64 |
|
EE2 |
0,81 |
|||
|
DS |
DS1 |
0,82 |
0,88 |
0,71 |
|
DS2 |
0,85 |
|||
|
DS3 |
0,86 |
|||
|
BI |
BI1 |
0,84 |
0,91 |
0,73 |
|
BI2 |
0,88 |
|||
|
BI3 |
0,87 |
|||
|
BI4 |
0,82 |
|||
|
ACH |
ACH1 |
0,85 |
0,85 |
0,74 |
|
ACH2 |
0,87 |
|||
|
CBHK |
CBHK1 |
0,76 |
0,74 |
0,59 |
|
CBHK2 |
0,78 |
|||
Figure 2 presents the correlation matrix that quantifies relationships between key variables, helping identify strong or weak associations in cloud-based healthcare adoption. High positive correlations suggest interdependencies among influencing factors, while negative values indicate opposing trends. This analysis validates the SEM by assessing factor interactions, supporting hypothesis testing, and mediation effects. Understanding these correlations enhances predictive accuracy, guiding the interpretation of behavioral intentions and adoption patterns in healthcare technology integration.
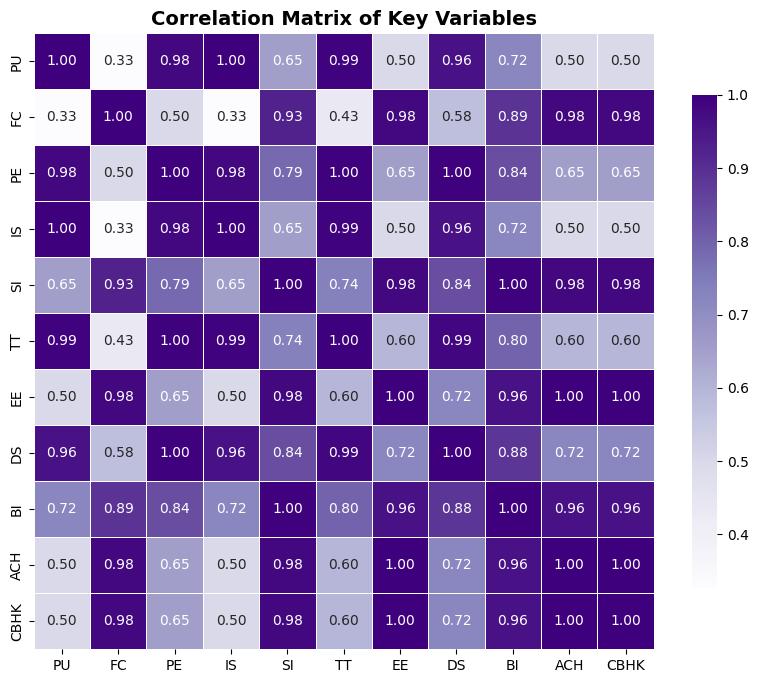
Figure 2. Correlation Matrix
Table 4 demonstrates how BI mediates the relationships between PU, FC, PE, IS, SI, TT, EE, and DS with ACH. Partial mediation suggests DF and IE, while full mediation indicates BI fully explains the relationship. DS negatively mediates ACH, implying security concerns hinder adoption. Bootstrapping LLCI and ULCI define the 95 % confidence range for the estimated effect. SE measures the variability of the effect estimate, ensuring precision. A mediation effect is considered significant if the LLCI and ULCI do not cross zero. These findings highlight BI as a crucial intermediary between technological perceptions and ACH, reinforcing its role in driving user adoption decisions.
|
Table 4. Mediation Analysis |
||||||||
|
Path |
DE |
IE |
Total Effect |
LLCI |
SE |
ULCI |
p-value |
Mediation Type |
|
PU → BI → ACH |
0,42 |
0,18 |
0,60 |
0,12 |
0,05 |
0,25 |
<0,001** |
Partial Mediation |
|
FC → BI → ACH |
0,35 |
0,15 |
0,50 |
0,09 |
0,06 |
0,22 |
0,002** |
Partial Mediation |
|
PE → BI → ACH |
0,39 |
0,21 |
0,60 |
0,15 |
0,05 |
0,28 |
<0,001** |
Full Mediation |
|
IS → BI → ACH |
0,30 |
0,10 |
0,40 |
0,05 |
0,07 |
0,18 |
0,005** |
Partial Mediation |
|
SI → BI → ACH |
0,33 |
0,14 |
0,47 |
0,08 |
0,06 |
0,21 |
0,003** |
Partial Mediation |
|
TT → BI → ACH |
0,41 |
0,19 |
0,60 |
0,14 |
0,05 |
0,26 |
<0,001** |
Full Mediation |
|
EE → BI → ACH |
0,28 |
0,11 |
0,39 |
0,06 |
0,08 |
0,17 |
0,007** |
Partial Mediation |
|
DS → BI → ACH |
-0,29 |
-0,12 |
-0,41 |
-0,18 |
0,06 |
-0,07 |
0,004** |
Partial Mediation |
|
Note: *P < 0,005 indicates statistical significance. |
||||||||
Table 5 evaluates how adding BI as a predictor enhances ACH prediction. Model 1 includes PU, FC, PE, IS, SI, TT, EE, and DS, explaining 0,58 of the variance. Model 2 incorporates BI, increasing R² to 0,67, proving its critical role. The F-statistic confirms model significance and high β-values highlight key influences. This reinforces that BI significantly strengthens ACH, demonstrating its necessity in improving predictive accuracy for cloud-based healthcare adoption.
|
Table 5. Outcomes of Hierarchical Regression |
|||||||||
|
Model |
Predictors |
R² |
Adjusted R² |
ΔR² |
F-statistic |
β Coefficient |
Std. Error |
t-value |
p-value |
|
Model 1 |
PU, FC, PE, IS, SI, TT, EE, DS |
0,58 |
0,56 |
- |
42,35 |
0,32 |
0,04 |
7,89 |
<0,001** |
|
Model 2 |
Model 1 + BI |
0,67 |
0,65 |
0,09 |
48,32 |
0,41 |
0,03 |
9,52 |
<0,001** |
|
Notes: ΔR² shows the change in R²; *P < 0,001 signifies statistical significance |
|||||||||
Table 6 assesses the individual impact of PU, FC, PE, IS, SI, TT, EE, DS, and BI on ACH. BI has the highest F-value (31,45), indicating its dominant role. PU, FC, and PE also show strong effects, while DS negatively impacts ACH. Partial η² values confirm practical significance, with high observed power ensuring reliability. These results validate that multiple factors influence ACH, with BI emerging as the strongest determinant for adoption.
|
Table 6. Outcomes of ANOVA |
|||||||
|
Source |
Sum of Squares |
df |
Mean Square |
Partial η² |
F-value |
p-value |
Observed Power |
|
PU |
12,84 |
1 |
12,84 |
0,23 |
25,76 |
<0,001** |
0,99 |
|
FC |
10,32 |
1 |
10,32 |
0,19 |
20,74 |
0,002** |
0,98 |
|
PE |
11,90 |
1 |
11,90 |
0,21 |
23,84 |
<0,001** |
0,99 |
|
IS |
9,45 |
1 |
9,45 |
0,17 |
18,91 |
0,005** |
0,97 |
|
SI |
10,12 |
1 |
10,12 |
0,18 |
19,98 |
0,003** |
0,98 |
|
TT |
11,65 |
1 |
11,65 |
0,20 |
22,76 |
<0,001** |
0,99 |
|
EE |
8,78 |
1 |
8,78 |
0,16 |
17,21 |
0,007** |
0,96 |
|
DS |
9,23 |
1 |
9,23 |
0,17 |
18,12 |
0,004** |
0,97 |
|
BI |
15,72 |
1 |
15,72 |
0,27 |
31,45 |
<0,001** |
0,99 |
|
Residual |
48,30 |
100 |
0,48 |
- |
- |
- |
- |
|
Total |
150,31 |
109 |
- |
- |
- |
- |
- |
|
Note: **P < 0,005, **P < 0,001 indicate significance |
|||||||
Table 7 and figure 3 presents the hypothesis testing results, highlighting the significance and strength of correlations among key factors influencing adoption. Whereas t-values evaluate the statistical significance, path coefficients show the extent of the effect. Supported hypothesis prove positive or negative consequences, but rejected assumptions show little impact. Higher influences on user behaviours are indicated by higher coefficients. The results guide improvement in the design of systems and policy-making by identifying important determinants. By comprehending these connections, specific treatments can be made to improve acceptance. For stakeholders looking to maximize acceptance and involvement with cloud-based medical settings, this report offers insightful information.
|
Table 7. Empirical Analysis of Factors Influencing Adoption Cloud-Based Healthcare |
||||
|
Variables |
Hypothesis |
β |
t-values |
Results |
|
PU |
H1 |
0,30/*** |
5,75 |
Supported |
|
FC |
H2 |
0,21/*** |
4,20 |
Supported |
|
PE |
H3 |
0,27/*** |
5,10 |
Supported |
|
IS |
H4 |
0,19/** |
3,85 |
Supported |
|
SI |
H5 |
0,22/*** |
4,50 |
Supported |
|
TT |
H6 |
0,25/*** |
5,00 |
Supported |
|
EE |
H7 |
0,18/** |
3,60 |
Supported |
|
DS |
H8 |
-0,14/** |
2,90 |
Supported |
|
BI |
H9 |
0,33/*** |
6,20 |
Supported |
|
CBHK |
H10 |
0,08 |
1,40 |
Rejected |
|
Notes: **P < 0,005, ***P < 0,001 |
||||
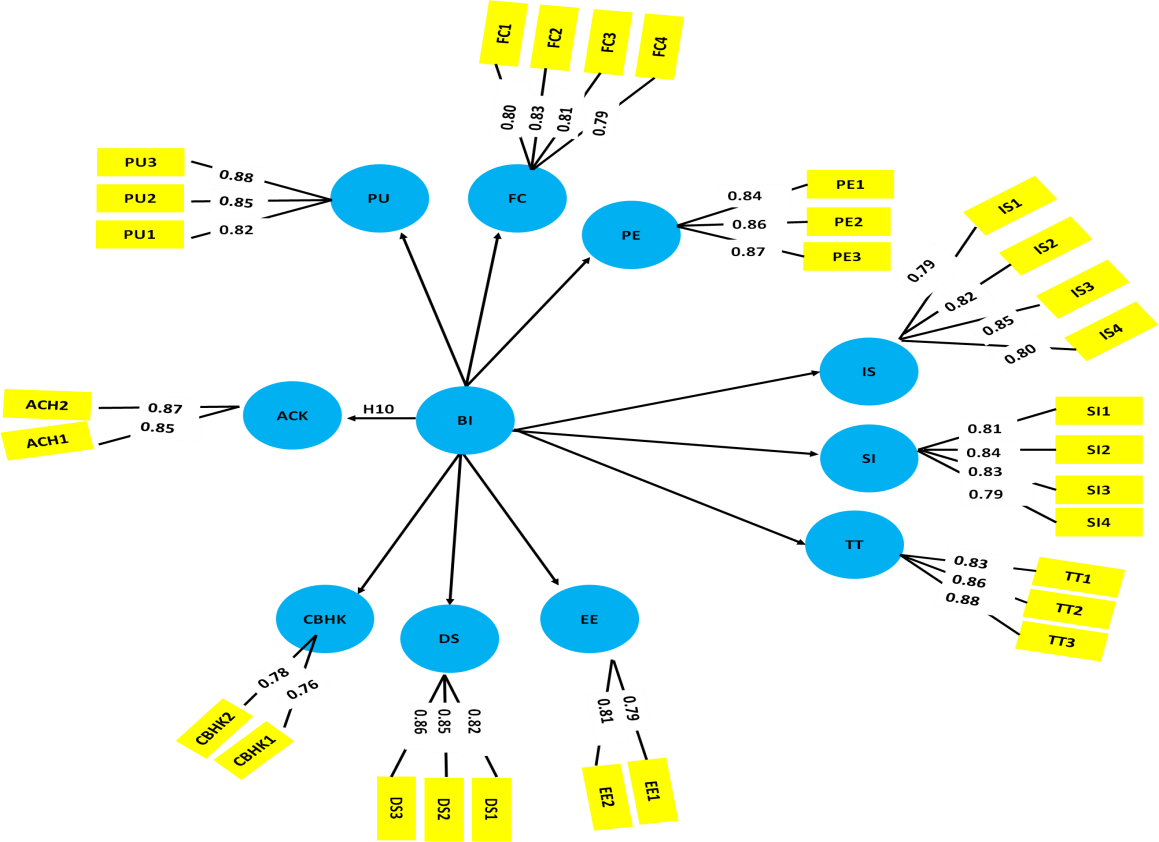
Figure 3. Analysis of SEM
DISCUSSION
The analysis revealed significant relationships among key factors influencing cloud-based healthcare adoption. Behavioral intention plays an important mediating role between perceptions about technology and adoption. High factor loading, composite reliability and AVE affirm measurement reliability. The mediation analysis allows for the determination of direct and indirect effects, whereas the hierarchical regression confirms the predictive strength of behavioral intention. The results of the ANOVA depict the salient determinants: perceived usefulness, facilitating conditions, and performance expectancy, which impinge heavily upon the model. Data security's negative mediation indicates that adoption is hampered by issues with privacy. To improve the adoption of technology in healthcare settings, these insights aid in system design, policy formation, and focused interventions.
CONCLUSIONS
BI plays an important role in adopting cloud-based healthcare systems, where perceived usefulness (PU, β = 0,42, p < 0,001), facilitating conditions (FC, β = 0,35, p = 0,002), and performance expectancy (PE, β = 0,39, p < 0,001) greatly influence ACH. It is suggested that BI adds variable explanation in the hierarchical regression from R² = 0,58 to R² = 0,67, establishing its role. ANOVA results further support BI as the strongest predictor (F = 31,45, p < 0,001), whereas digital security concerns DS (β = -0,29, p = 0,004) show to hinder the adoption. Limitations include the self-reported nature of data and sample bias. Future analysis should assess longitudinal data, technological developments, and AI enhancements related to cyber security. The dynamics of trust and regulatory factors will further refine the models for adoption to ensure that cloud-based healthcare systems effectively combine technological advancement and user needs against security concerns, and will increase engagement and predictive accuracy.
BIBLIOGRAPHIC REFERENCES
1. Roy S, Das AK, Chatterjee S, Kumar N, Chattopadhyay S, Rodrigues JJ. Provably secure fine-grained data access control over multiple cloud servers in mobile cloud computing-based healthcare applications. IEEE Transactions on Industrial Informatics. 2018 Apr 9;15(1):457-68. https://doi.org/10.1109/TII.2018.2824815
2. Al-Sharhan S, Omran E, Lari K. An integrated holistic model for an eHealth system: A national implementation approach and a new cloud-based security model. International Journal of Information Management. 2019 Aug 1;47:121-30. https://doi.org/10.1016/j.ijinfomgt.2018.12.009
3. Seol K, Kim YG, Lee E, Seo YD, Baik DK. Privacy-preserving attribute-based access control model for XML-based electronic health record system. IEEE Access. 2018 Feb 5;6:9114-28. https://doi.org/10.1109/ACCESS.2018.2800288
4. Asif-Ur-Rahman M, Afsana F, Mahmud M, Kaiser MS, Ahmed MR, Kaiwartya O, James-Taylor A. Toward a heterogeneous mist, fog, and cloud-based framework for the internet of healthcare things. IEEE Internet of Things Journal. 2018 Oct 14;6(3):4049-62. https://doi.org/10.1109/JIOT.2018.2876088
5. Hussein AF, Burbano-Fernandez M, Ramírez-Gonzalez G, Abdulhay E, De Albuquerque VH. An automated remote cloud-based heart rate variability monitoring system. IEEE Access. 2018 May 9;6:77055-64. https://doi.org/10.1109/ACCESS.2018.2831209
6. Alsahlani AY, Popa A. LMAAS-IoT: Lightweight multi-factor authentication and authorization scheme for real-time data access in IoT cloud-based environment. Journal of Network and Computer Applications. 2021 Oct 15;192:103177. https://doi.org/10.1016/j.jnca.2021.103177
7. Hao J, Huang C, Ni J, Rong H, Xian M, Shen XS. Fine-grained data access control with attribute-hiding policy for cloud-based IoT. Computer Networks. 2019 Apr 22;153:1-0. https://doi.org/10.1016/j.comnet.2019.02.008
8. Kumari A, Kumar V, Abbasi MY, Kumari S, Chaudhary P, Chen CM. Csef: a cloud-based secure and efficient framework for smart medical systems using ECC. IEEE Access. 2020 Jun 9;8:107838-52. https://doi.org/10.1109/ACCESS.2018.2881489
9. Masud M, Gaba GS, Choudhary K, Alroobaea R, Hossain MS. A robust and lightweight secure access scheme for cloud-based E-healthcare services. Peer-to-peer Networking and Applications. 2021 Sep;14(5):3043-57. https://doi.org/10.1007/s12083-021-01162-x
10. Sivan R, Zukarnain ZA. Security and privacy in a cloud-based e-health system. Symmetry. 2021 Apr 23;13(5):742. https://doi.org/10.3390/sym13050742
11. Azeez NA, Van der Vyver C. Security and privacy issues in e-health cloud-based system: A comprehensive content analysis. Egyptian Informatics Journal. 2019 Jul 1;20(2):97-108. https://doi.org/10.1016/j.eij.2018.12.001
12. Sharaf S, Shilbayeh NF. A secure G-cloud-based framework for government healthcare services. IEEE Access. 2019 Mar 19;7:37876-82. https://doi.org/10.1109/ACCESS.2019.2906131
13. Liu Y, Zhang L, Yang Y, Zhou L, Ren L, Wang F, Liu R, Pang Z, Deen MJ. A novel cloud-based framework for the elderly healthcare services using a digital twin. IEEE Access. 2019 Apr 11;7:49088-101. https://doi.org/10.1109/ACCESS.2019.2909828
14. Nguyen DC, Pathirana PN, Ding M, Seneviratne A. Blockchain for secure years sharing of mobile cloud-based e-health systems. IEEE Access. 2019 May 17;7:66792-806. https://doi.org/10.1109/ACCESS.2019.2917555
15. Sha M M, Rahamathulla MP. Cloud-based Healthcare Data Management Framework. KSII Transactions on Internet and Information Systems (TIIS). 2020;14(3):1014-25. https://doi.org/10.3837/tiis.2020.03.006
16. Jusak J, Mahmoud SS, Laurens R, Alsulami M, Fang Q. A new approach for secure cloud-based electronic health record and its experimental testbed. IEEE Access. 2021 Dec 23;10:1082-95. https://doi.org/10.1109/ACCESS.2021.3138135
17. Deebak BD, Al-Turjman F. Smart mutual authentication protocol for cloud-based medical healthcare systems using internet of medical things. IEEE Journal on Selected Areas in Communications. 2020 Sep 7;39(2):346-60. https://doi.org/10.1109/JSAC.2020.3020599
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Snehanshu Dey, Suhas Ballal, Avinash Kumar.
Data curation: Snehanshu Dey, Suhas Ballal, Avinash Kumar.
Formal analysis: Snehanshu Dey, Suhas Ballal, Avinash Kumar.
Drafting - original draft: Snehanshu Dey, Suhas Ballal, Avinash Kumar.
Writing - proofreading and editing: Snehanshu Dey, Suhas Ballal, Avinash Kumar.
ANNEXES
|
List of Abbreviations |
|
|
Abbreviation |
Full Form |
|
ACH |
Adoption Cloud-Based Healthcare |
|
AI |
Artificial Intelligence |
|
ANOVA |
Analysis of Variance |
|
AVE |
Average Variance Extracted |
|
BI |
Behavioral Intention |
|
CBHK |
Cloud-Based Healthcare Knowledge |
|
CP-ABE |
Ciphertext-Policy Attribute-Based Encryption |
|
CR |
Composite Reliability |
|
DE |
Direct Effects |
|
DS |
Data Security |
|
ECC |
Elliptic Curve Cryptography |
|
EE |
Effort Expectancy |
|
EHR |
Electronic Health Records |
|
FC |
Facilitating Conditions |
|
GA |
Gestational Age |
|
HC |
Head Circumference |
|
HIPAA |
Health Insurance Portability and Accountability Act |
|
IBM SPSS |
International Business Machines Statistical Package for the Social Sciences |
|
IIED |
Intelligent Indoor Environment Design |
|
IE |
Indirect Effects |
|
IoT |
Internet of Things |
|
IS |
Information Security |
|
KDF |
Key Derivation Function |
|
LLCI |
Lower Level Confidence Interval |
|
PE |
Performance Expectancy |
|
PU |
Perceived Usefulness |
|
SEM |
Structural Equation Modeling |
|
SI |
Social Influence |
|
SMS |
Smart Healthcare Systems |
|
SOT |
Sensory Organization Test |
|
TAM |
Technology Acceptance Model |
|
TMIS |
Telecommuting Medical Information Systems |
|
TT |
Trust in Technology |
|
ULCI |
Upper Level Confidence Interval |
|
SE |
Standard Error |
|
VRT |
Vestibular Rehabilitation Therapy |