doi: 10.56294/mw2023137
ORIGINAL
Research on Health Informatics Systems and Their Influence on Patient Decision-Making in the Digital Age
Investigación sobre sistemas informáticos sanitarios y su influencia en la toma de decisiones de los pacientes en la era digital
Renuka Jyothi S1 ![]() *,
Sonia Mehta2
*,
Sonia Mehta2 ![]() , Lulup Kumar Sahoo3
, Lulup Kumar Sahoo3 ![]()
1JAIN (Deemed-to-be University), Department of Biotechnology and Genetics. Bangalore, Karnataka, India.
2School of Nursing, Noida International University. Greater Noida, Uttar Pradesh, India.
3IMS and SUM Hospital, Siksha ‘O’ Anusandhan (deemed to be University), Department of Neurology. Bhubaneswar, Odisha, India.
Cite as: Renuka JS, Mehta S, Sahoo LK. Research on Health Informatics Systems and Their Influence on Patient Decision-Making in the Digital Age. Seminars in Medical Writing and Education. 2023; 2:137. https://doi.org/10.56294/mw2023137
Submitted: 15-09-2022 Revised: 27-12-2022 Accepted: 01-03-2023 Published: 02-03-2023
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Renuka Jyothi S *
ABSTRACT
The healthcare industry has changed due to the quick development of health informatics systems, particularly in the digital age, where patients increasingly rely on technology to manage their health. The aim is to investigate the influence of health informatics systems on patient decision-making quality in the digital age. Survey data from 317 patients using health informatics systems were collected. To evaluate factors, participants used a 5-point Likert scale to grade their experiences with these systems. Independent variables include type of health informatics system (THIS), Frequency of Use of Digital Health Tools (FUDHT), patient health literacy (PHL), access to technology (AT), and trust in digital tools (TDT), all of which influence decision-making behavior. The dependent variable is patient decision-making in the Digital Age (PDM), patient satisfaction with health decisions (PSHD), and Patient confidence in health choices (PCHC). Data was analyzed with SPSS 26, employing multiple linear regression, and path analysis to explore relationships between independent variables and patient decision-making quality, showing significant predictors of decision quality in the digital health setting. Results indicated support for hypothesis 3 (H3), as positive significant relationships among all the path coefficients and p-values validate the hypothesis. Findings highlight the critical role of digital tool accessibility, trust, and literacy in enhancing patient decision-making. Healthcare providers should focus on improving these aspects to support more informed and confident decision-making among patients in the digital age.
Keywords: Health Informatics Systems; Patient Decision; Electronic Health Records (EHRs).
RESUMEN
El sector sanitario ha cambiado debido al rápido desarrollo de los sistemas informáticos sanitarios, sobre todo en la era digital, en la que los pacientes confían cada vez más en la tecnología para gestionar su salud. El objetivo es investigar la influencia de los sistemas informáticos sanitarios en la calidad de la toma de decisiones de los pacientes en la era digital. Se recopilaron datos de encuestas realizadas a 317 pacientes que utilizaban sistemas informáticos sanitarios. Para evaluar los factores, los participantes utilizaron una escala Likert de 5 puntos para calificar sus experiencias con estos sistemas. Las variables independientes incluyen el tipo de sistema informático sanitario (THIS), la frecuencia de uso de herramientas sanitarias digitales (FUDHT), los conocimientos sanitarios del paciente (PHL), el acceso a la tecnología (AT) y la confianza en las herramientas digitales (TDT), todas las cuales influyen en el comportamiento a la hora de tomar decisiones. La variable dependiente es la toma de decisiones del paciente en la Era Digital (PDM), la satisfacción del paciente con las decisiones sanitarias (PSHD) y la confianza del paciente en las elecciones sanitarias (PCHC). Los datos se analizaron con SPSS 26, empleando regresión lineal múltiple y análisis de trayectorias para explorar las relaciones entre las variables independientes y la calidad de la toma de decisiones del paciente, mostrando predictores significativos de la calidad de la decisión en el entorno sanitario digital. Los resultados indicaron el apoyo a la hipótesis 3 (H3), ya que las relaciones significativas positivas entre todos los coeficientes de trayectoria y los valores p validan la hipótesis. Los resultados destacan el papel fundamental de la accesibilidad a las herramientas digitales, la confianza y la alfabetización en la mejora de la toma de decisiones de los pacientes. Los profesionales sanitarios deberían centrarse en mejorar estos aspectos para favorecer una toma de decisiones más informada y segura entre los pacientes en la era digital.
Palabras clave: Sistemas Informáticos de Salud; Decisión del Paciente; Historias Clínicas Electrónicas (HCE).
INTRODUCTION
As digital tools like mobile health apps, telemedicine platforms, and electronic health records (EHRs) are increasingly incorporated into routine medical procedures, patients are empowered with more information, personalized care options, and the ability to make more informed decisions about their health.(1) Such advancements can improve clinical outcomes, simplify healthcare processes, and expand patient engagement, but effective use of these systems for influencing patient decisions will depend on patient health literacy, access to digital tools, and trust in technology. The presence of health informatics systems in the digital era has greatly transformed healthcare delivery, changing the interaction mode between patients and providers.(2) EHR systems have been accepted and adopted by healthcare organizations around the world rapidly. Large, varied data sets that incorporate prepared and organized data items, including diagnoses, are included in the databases created by EHR systems and prescriptions (RxNorm), in addition to the rich, unorganized information that is carved into clinical narratives and makes up over 80 % of the data in EHRs.(3) Press releases and white papers frequently address the evolving medical landscape and changes to medical education that will better prepare physicians for current practice. Increased focus on aspects such as patient safety, risk management, teamwork, and communication were quite common reform themes. To believe that whilst these actions can be important advancements, such measures are insufficient on their own. There is an urgency to start paying some attention to what in the view can be considered the biggest paradigm shift happening at present: the fast transition of medical practice moving into the artificial intelligence (AI) age after the information era.(4) There is currently a substantial amount of data showing that patient decision aids are a useful tool for promoting informed choice in a variety of medical issues. Well-made decision aids offer fair information about the possibilities that are accessible, their advantages and disadvantages, and their likelihood of happening. Patients will perceive and comprehend the magnitude of those advantages and risks more accurately if the results of various alternatives are quantified using best practice methodologies. This is a key element of wise health decisions.(5)
The health system has verified COVID-19 instances from the past and current. Early in the pandemic, an occurrence command center was established to help identify EHR-based solutions to enhance clinical care and to explain the deployment of technical assistance essential for optimizing clinical management.(6) The COVID-19 pandemic put the necessity of global solutions and collaborative decision-making to the forefront, requiring data and analytics. The reuse of clinical data from EHR could be a very complex process. It mainly discusses collaborative data infrastructures for COVID-19 research along with concerns about data governance and sharing. Data governance, standardized protocols, healthcare process modeling, and data interoperability were crucial components. Lessons learned could illuminate the path for improved preparedness in times of sudden catastrophes worldwide research in older formats.(7) Instead of being skill-based, the bulk of the criteria for the existing health informatics program were competency-based. By examining the current knowledge and skills requirements in graduate health informatics courses, the research’s main objective was to assess graduate students' confidence in certain health informatics competencies.(8) The possibility for data science technologies to enhance care delivery is presented by the increasing accessibility of medical data through computer hardware and software technologies. However, producing reliable results across populations is challenging due to scattered and personal medical data. Federated learning, a method that trains a maintained sensitive data at local institutions while integrating a global model with a central server, has the potential to connect diverse healthcare data sources while respecting privacy.(9) The World Health Organization (WHO) seeks to lower and manage maternal, newborn, and infant mortality. There was a discussion of automating verbal autopsy reporting for these illnesses with an emphasis on user-centered design for workforces that lack technology literacy.(10) Concerns about privacy and security, interoperability, health literacy, the digital gap, and excessive dependence on technology are some of the obstacles that health informatics systems must overcome. While health literacy is essential for efficient utilization, the digital gap leads to inequalities in healthcare access and decision-making. Trust in these technologies could be weakened by privacy and security issues. For the best health informatics solutions to be delivered, these issues had to be resolved.(11)
Objective of the research: research aims to examine how health informatics systems influence patient decision-making in the digital age. Specifically, the research seeks to measure how the factors, including the type of health informatics system, frequency of using digital health tools, users' health, technology access, and distrust toward digital tools, affect patients' decision-making confidence, accuracy, and satisfaction about healthcare decisions. The relationships among these variables will aim to identify key predictors in the digital health context that will help enhance patient decision-making, thus translating into useful insights for healthcare practice and the effective use of digital tools.
Organizations of the research: the rest of the research is sectioned with a thorough discussion of the materials and methods for research-specific design, data gathering, and analytic methods. Results and discussions present the findings while contextualizing the interpretation of findings within existing literature, thus highlighting central trends and discoveries. Finally, the research rounds up and summarizes the primary findings, discusses implications for healthcare practice, and recommends avenues for future investigation in health informatics systems.
METHOD
Hypothesis Development
Section presents 5 hypothesis regarding how digital health tools influence patients' decision-making in the digital age. It checks how the frequency of use, patient health literacy, easy adaptability, and trust in digital tools affect the quality of decision-making in healthcare situations. The conceptual framework displayed in figure 1 captures these relationships, illustrating how these key variables contribute to the improvement of decisions made by patients in their digital health encounters.
Hypothesis 1: The type of health informative system (THIS) will significantly affect patient decision-making (PDM). (THIS →PDM)
Hypothesis 2: Frequency of use of digital health tools (FUDHT) will positively correlate with patient satisfaction with health decisions (PSHD). (FUDHT→ PSHD)
Hypothesis 3: Patient health literacy (PHL) will positively influence patient confidence in health choices (PCHC) made through digital health tools. (PHL→ PCHC)
Hypothesis 4: Access technology (AT) will positively influence patient satisfaction with health decisions (PSHD). (AT→ PSHD)
Hypothesis 5: Trust in digital tools (TDT) will be a significant predictor of patient decision-making (PDM). (TDT→ PDM)
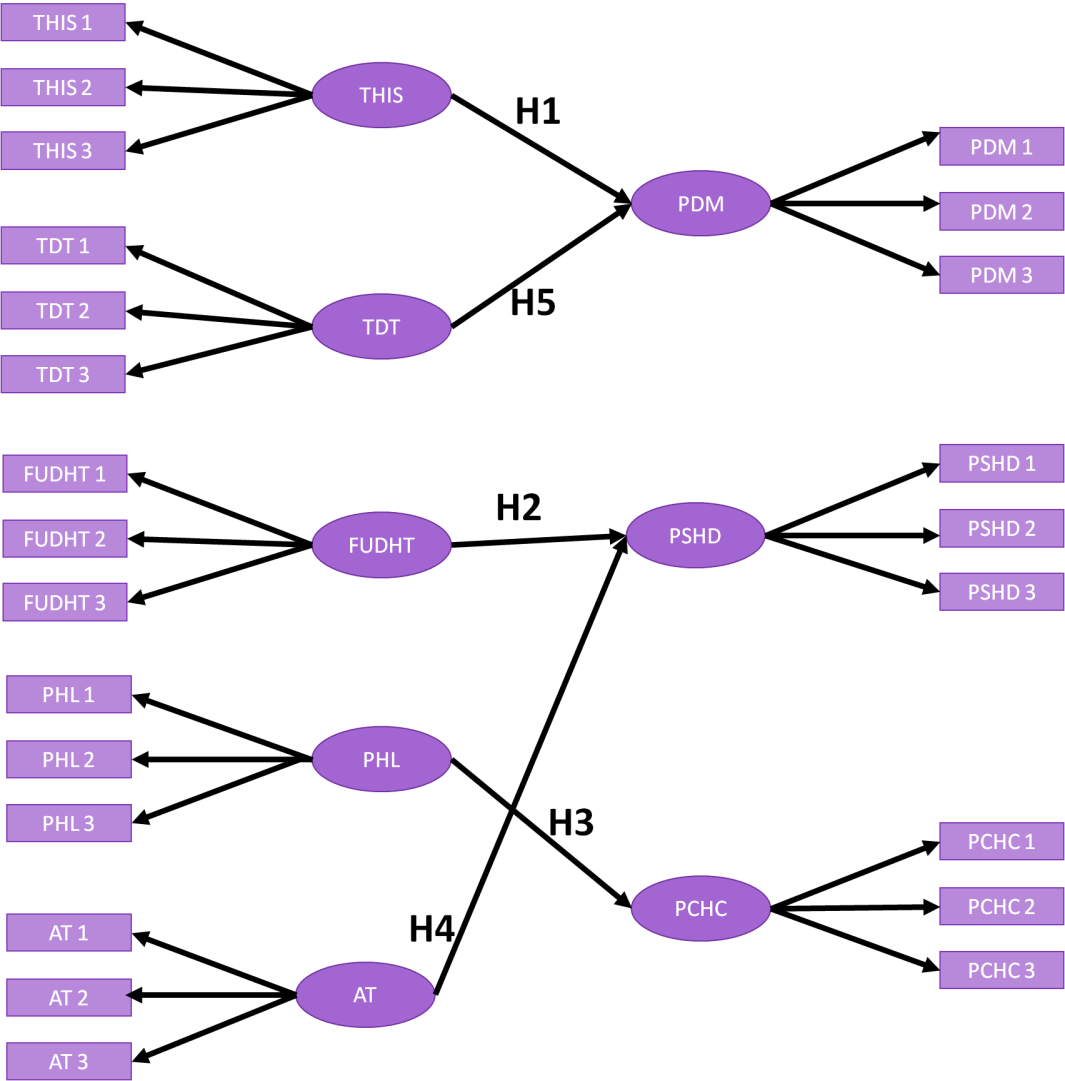
Figure 1. Conceptual model for hypothesis
Data Collection
The dataset is made up of responses from 317 participants: 160 patients and 157 doctors, all of whom availed themselves of health information systems, like EHR, platforms for telemedicine, and apps for mobile health. The patient database includes demographic data, with a focus on age (a), gender (b), frequency of visits (c), health issues (d), and digital tool usage (e) as shown in figure 2. The doctor dataset consists of age (a), gender (b), and years of experience (c) as shown in figure 3. For both datasets, analysis will be conducted to determine the influence of these variables on patient decision-making within the digital health environment, e.g., factors like trust in digital tools, access to technology, and health literacy.
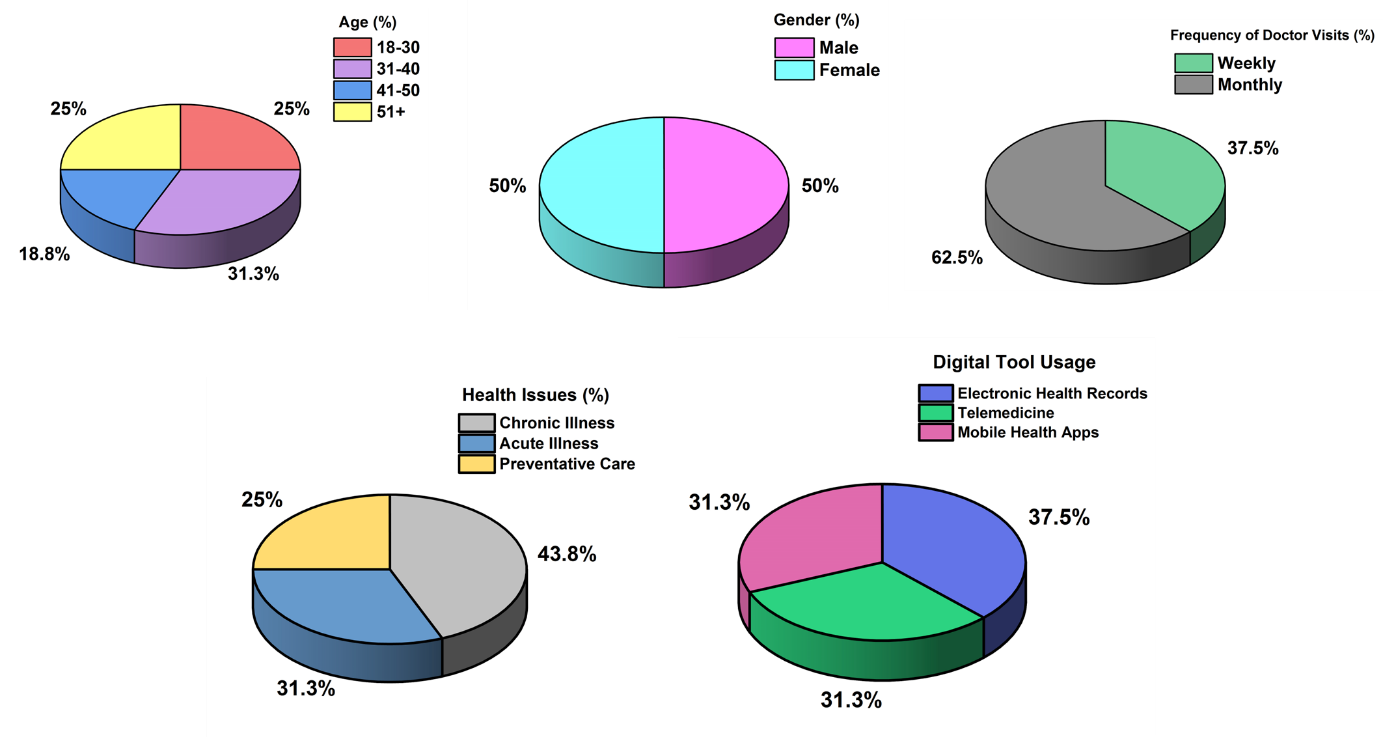
Figure 2. Demographics details of patient (a) age (b) gender, (c) Frequency of Doctor visits (d) Health issues (e) Digital tool usage
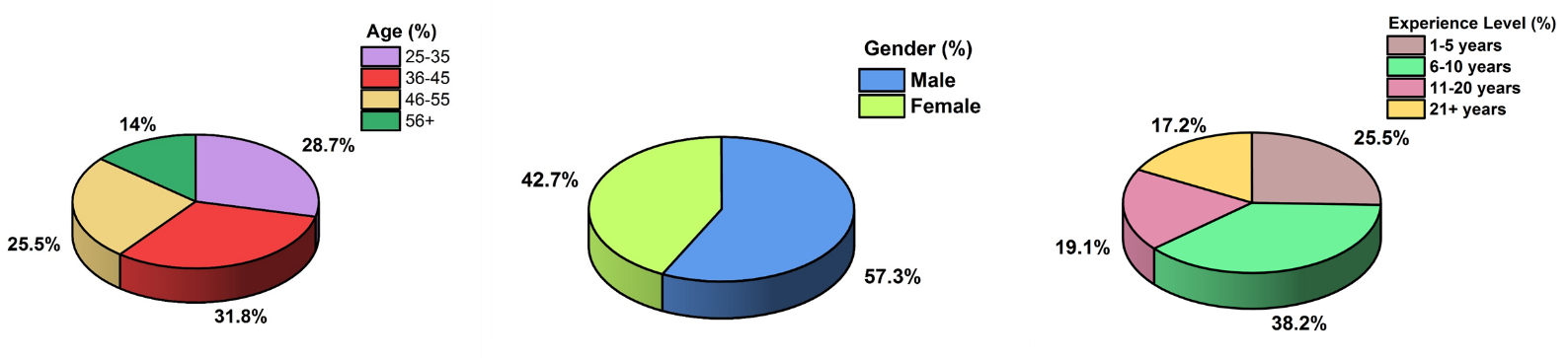
Figure 3. Demographics details of doctor (a) age (b) gender, (c) experience level
Research Instrument
Survey intends to provide information on evaluation variables regarding the influence of health informatics systems on patient decision-making in the digital age. Eight key variables are reviewed: THIS, FUDH, PHL, AT, TDT, PDM, PSHD, PCHC. The survey had a quantitative design, with an online survey delivered using Google. To gather information on participants' experiences using digital health tools and making decisions, there will be three questions for each variable, for a total of twenty-four questions.
Data Analysis
Data analysis acts as an essential for turning raw survey responses into useful insights that will guide patient decision-making within the scope of digital health. In this research, data analysis will be employed to examine the relationship between several key factors. This will be analyzed using SPSS v26 statistical software to conduct multiple linear regression and path analysis. These methods will offer a comprehensive grasp of how each component affects the patient's confidence in their ability to make decisions, accuracy, and satisfaction with healthcare choices in the digital age. Regression analysis identifies the significant predictors of decision-making quality. The paper is organized in a logical path analysis structure, beginning with a Structural Equation Modeling (SEM) process, which involves two models: the measurement model, which aims at evaluating the relationship between indicators and latent constructs, and the structural model, which focuses on analyzing the causal relationships between variables. The structural model is subjected to path analysis. The path analysis will demonstrate both direct and indirect relationships among the factors at play and provide the full image of dynamics influencing patient decision-making in digital health settings.
Multiple linear Regression (MLR) analysis
Using several explanatory variables, the statistical method known as MLR models the linear relationship between response (dependent) and explanatory (independent) factors. Ordinary least-squares (OLS) regression is extended by multiple regression as it incorporates several explanatory variables. MLR is a statistical technique that predicts the outcomes of an indicator by using the values of two or more variables; the dependent variable itself is the thing to be predicted, and the independent or explanatory variables are those they utilize to predict (equation 1).
![]()
Zi is the dependent variable, xj is the explanatory variable, β0 is the y-interest, βo = slope coefficient for each explanatory variable, ϵ- is the model error term.
Path analysis
To model and analyze the indirect and direct relationships between multiple variables, path analysis is a statistical technique that helps identify the causal pathways that connect independent variables to dependent variables, providing a clear image of how one variable influence another, either directly or through intermediate variables. By estimating path coefficients and representing these relationships as a set of equations, path analysis gives researchers insight into the direction and strength of each relationship, which helps them understand the complex interactions between factors in a given system, such as how trust, health literacy, and the use of digital health tools affect patient decision-making.
RESULTS
The evaluation performance of quantitative assessments and data analysis techniques are examined in this phase.
Measurement model
In structural equation modeling (SEM), the measurement model links the associated latent constructs (those underlying components) to the observed indicators (reflective indicators). Based on an assessment of factor loadings, validity, and reliability, it guarantees that the indicators do contribute suitably to the representation of latent variables. Metrics that address internal consistency and the degree to which the indicators represent their underlying components, the measuring approach is strengthened with metrics like Cronbach's Alpha, Composite Reliability (CR), and Average Variance Extracted (AVE).
Factor loadings for each indicator are provided in table 1, which displays the measurement model's results and shows how well each item reflects its latent construct. Each construct's internal consistency is gauged by Cronbach's Alpha, where higher values denote more trustworthy measurements. Average Variance Extracted (AVE) is a measure of dependability, whereas Composite dependability is an internally consistent construct. Extracted shows how much of the variance in each construct is explained by the indicators type of health informatics system and patient decision-making (e.g., EHR, telemedicine, and health applications, respectively) are two examples of latent variables with many indicators. High factor loadings (such as PHL2's 0,90), which attest to the model's validity and dependability, confirm the high correlation between the indicators and latent components.
|
Table 1. Results of examination of measurement model |
|||||
|
Construct |
Indicator |
Factor Loading |
Cronbach's Alpha |
CR |
AVE |
|
Type of Health Informatics System (THIS) |
THIS1 |
0,83 |
0,87 |
0,90 |
0,74 |
|
THIS2 |
0,79 |
||||
|
THIS3 |
0,80 |
||||
|
Frequency of Use of Digital Health Tools (FUDHT) |
FUDHT1 |
0,76 |
0,82 |
0,85 |
0,69 |
|
FUDHT2 |
0,78 |
||||
|
FUDHT3 |
0,74 |
||||
|
Patient Health Literacy (PHL) |
PHL1 |
0,88 |
0,91 |
0,93 |
0,83 |
|
PHL2 |
0,90 |
||||
|
PHL3 |
0,87 |
||||
|
Access to Technology (AT) |
AT1 |
0,87 |
0,90 |
0,92 |
0,80 |
|
AT2 |
0,85 |
||||
|
AT3 |
0,86 |
||||
|
Trust in Digital Tools (TDT) |
TDT1 |
0,85 |
0,88 |
0,91 |
0,78 |
|
TDT2 |
0,82 |
||||
|
TDT3 |
0,81 |
||||
|
Patient Decision-Making (PDM) |
PDM1 |
0,84 |
0,89 |
0,92 |
0,76 |
|
PDM2 |
0,82 |
||||
|
PDM3 |
0,83 |
||||
|
Patient Satisfaction with Health Decisions (PSHD) |
PSHD1 |
0,80 |
0,85 |
0,88 |
0,72 |
|
PSHD2 |
0,79 |
||||
|
PSHD3 |
0,81 |
||||
|
Patient Confidence in Health Choices (PCHC) |
PCHC1 |
0,83 |
0,86 |
0,90 |
0,74 |
|
PCHC2 |
0,81 |
||||
|
PCHC3 |
0,82 |
||||
Structural model
SEM is concerned with the structural model, which describes the proposed relationships and causal directions among latent constructs. A hypothesized one-way relationship of one latent variable was examined with another. Understanding direct and indirect effects provides insight into how interventions affect manifest variables and reveals any direct and indirect paths in a given model. The structural model is estimated by path coefficients representing the size of the operation and mode of that particular relationship, along with standard errors, t-values, and p-values to show if there is sufficient significant analysis in the correlations.
The outcomes of the structural model that calculates the route coefficients between the latent variables are shown in table 2 and figure 4, each depicting the strength and direction of the relationships. For instance, a path coefficient of 0,35 is indicative of a reasonable positive effect of the THIS on PDM. Standard error and t-value have been utilized to ascertain the reliability and statistical significance of every path, with a higher t-value indicating stronger evidence against the null hypothesis. All p-values (all <0,001) indicate that each relationship is statistically significant in supporting the hypotheses that the factors THIS, FUDHT, PHL, AT, and TDT significantly influence patient decision-making and satisfaction. All paths were confirmed in hypothesis status, thus implying that the proposed relationships exist in the model.
|
Table 2. Path analysis through structural model |
|||||
|
Path |
Path Coefficient |
Standard Error |
t-value |
p-value |
Hypothesis Status |
|
THIS → PDM |
0,35 |
0,08 |
4,38 |
< 0,001 |
Supported |
|
FUDHT → PSHD |
0,30 |
0,07 |
4,29 |
< 0,001 |
Supported |
|
PHL → PCHC |
0,45 |
0,10 |
4,50 |
< 0,001 |
Well Supported |
|
AT → PSHD |
0,33 |
0,06 |
5,50 |
< 0,001 |
Supported |
|
TDT → PDM |
0,38 |
0,09 |
4,22 |
< 0,001 |
Supported |
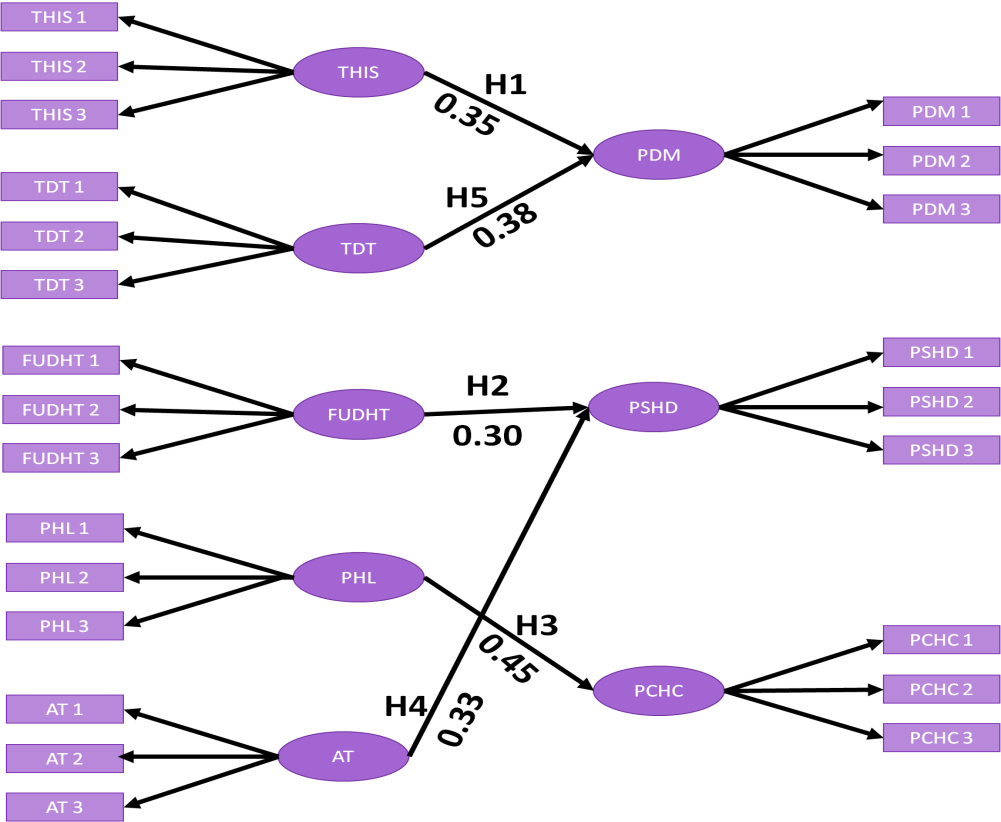
Figure 4. Outcome of Conceptual models with β
Multiple linear regression
In terms of a multiple regression analysis examining relationships between independent variables (THIS, FUDHT, PHL, AT, and TDT) and three dependent variables: PDM, PSHD, and PCHC, a summary of the results are presented in table 3. While the Standardized Coefficients (β) enable cross-variable comparisons, the Unstandardized Coefficients (B) values show the unprocessed each independent variable's effect on the dependent one. The precision of the coefficients, values for the t-values, and p-values used for each relationship's statistical significance test are estimated by standard errors (SE). All relationships in the table are statistically significant (p < 0,05), and high enough R² and Adjusted R² values indicate a substantial amount of variance that the model accounts for independent variables, thereby affirmatively suggesting the importance of digital health tools, literacy, and trust when it comes to influencing patient outcome dominantly being denoted by this high correlation.
|
Table 3. Outcomes of Multiple linear regression |
||||||||
|
Independent Variables |
Unstandardized Coefficients (B) |
Standardized Coefficients (β) |
SE |
t-value |
p-value |
R² |
Adjusted R² |
|
|
PDM |
THIS |
0,25 |
0,28 |
0,07 |
3,57 |
< 0,001 |
0,41 |
0,40 |
|
FUDHT |
0,12 |
0,14 |
0,05 |
2,40 |
0,018 |
|||
|
PHL |
0,23 |
0,25 |
0,06 |
3,83 |
< 0,001 |
|||
|
AT |
0,17 |
0,20 |
0,07 |
2,43 |
0,015 |
|||
|
TDT |
0,30 |
0,33 |
0,08 |
3,75 |
< 0,001 |
|||
|
PSHD |
THIS |
0,18 |
0,21 |
0,05 |
3,60 |
< 0,001 |
0,38 |
0,37 |
|
FUDHT |
0,25 |
0,30 |
0,06 |
4,16 |
< 0,001 |
|||
|
PHL |
0,15 |
0,17 |
0,05 |
2,96 |
0,003 |
|||
|
AT |
0,22 |
0,25 |
0,07 |
3,14 |
0,002 |
|||
|
TDT |
0,35 |
0,38 |
0,09 |
3,89 |
< 0,001 |
|||
|
PCHC |
THIS |
0,20 |
0,22 |
0,06 |
3,33 |
0,001 |
0,35 |
0,34 |
|
FUDHT |
0,10 |
0,12 |
0,05 |
2,00 |
0,047 |
|||
|
PHL |
0,18 |
0,21 |
0,06 |
3,00 |
0,003 |
|||
|
AT |
0,13 |
0,15 |
0,06 |
2,17 |
0,031 |
|||
|
TDT |
0,22 |
0,25 |
0,07 |
3,14 |
0,002 |
|||
DISCUSSION
The outcomes from the measurement model and structural model support the significant relationships between those constructs influencing the patient's decision-making, satisfaction, and confidence in their health choices. The high factor loadings, reliability scores (Cronbach's Alpha, CR), and AVE values confirm strong content validity and consistency of the measuring model within itself. In the structural model, there is an impressive positive path coefficient of 0,35 for the THIS on PDM, suggesting very solid relationships between digital health tools, literacy, trust, and patient outcomes. Multiple linear regression further supports these results, with high standardized coefficients (B), strong t-values, and low p-values (all < 0,05), suggesting that health informatics systems, frequency of use, literacy, access to technology, and trust in digital tools are significant contributors to predicting patient decision-making, satisfaction, and confidence. Hypothesis H3- determining the impact of Patient Health Literacy on Patient Confidence in Health Choices was very strongly supported with a coefficient of 0,45 (p<0,001), indicating an important way in which patients are empowered to trust their health decisions.
CONCLUSIONS
In the contemporary digital era, the aim of this research was to investigate how health informatics systems affect patient decision-making. Finding the following independent elements influencing decision quality was the primary goal of the current research described THIS (EHRs, telemedicine, mobile health apps) FUDHT, PHL, AT, TDT. The dependent variables included PDM, PSHD, and PCHC. Based on the direction of the proposed hypothesis, they were considered likely to make a significant impact upon patient decision-making behaviors. Survey data were collected to assess the impacts of digital health tools on 160 patients and 157 doctors. Participants rated items on a 5-point Likert scale. Data were analyzed using SPSS 26 with multiple regression and SEM. Results showed strong evidence supporting the hypothesis: access to technology, trust in digital tools, and health literacy were clearly having a significant influence with path analysis indicating positive relationships amongst these variables and patient outcomes. Specifically, the scientific research confirmed that the type of health informatics systems and the confidence in digital tools strongly predicted patient decision-making, thus supporting the hypothesis in H3. This emphasizes the need to focus on the improvements in these elements in the healthcare sector. Among the few limitations identified in the research were the self-reported data, leading to possible biases, and the cross-sectional nature of the data, which would have limited any causal inference. Future research could, therefore, be longitudinal, aiming to observe the long-term effects of digital health tools on the decision-making procedure and broaden the findings' applicability to different patient populations and healthcare models.
BIBLIOGRAPHIC REFERENCES
1. Kernebeck S, Busse TS, Böttcher MD, Weitz J, Ehlers J, Bork U. Impact of mobile health and medical applications on clinical practice in gastroenterology. World journal of gastroenterology. 2020 Aug 7;26(29):4182.Doi: https://doi.org/10.3748/wjg.v26.i29.4182.
2. Brewer LC, Fortuna KL, Jones C, Walker R, Hayes SN, Patten CA, Cooper LA. Back to the future: achieving health equity through health informatics and digital health. JMIR mHealth and uHealth. 2020 Jan 14;8(1):e14512.Doi: https://doi.org/10.2196/14512.
3. Giordano C, Brennan M, Mohamed B, Rashidi P, Modave F, Tighe P. Accessing artificial intelligence for clinical decision-making. Frontiers in digital health. 2021 Jun 25;3:645232. Doi: https://doi.org/10.3389/fdgth.2021.645232.
4. Wartman SA, Combs CD. Medical education must move from the information age to the age of artificial intelligence. Academic Medicine. 2018 Aug 1;93(8):1107-9.Doi: https://doi.org/10.1097/ACM.0000000000002044.
5. Trevena LJ, Bonner C, Okan Y, Peters E, Gaissmaier W, Han PK, Ozanne E, Timmermans D, Zikmund-Fisher BJ. Current challenges when using numbers in patient decision aids: advanced concepts. Medical Decision Making. 2021 Oct;41(7):834-47. Doi: https://doi.org/10.1177/0272989X21996342.
6. Reeves JJ, Hollandsworth HM, Torriani FJ, Taplitz R, Abeles S, Tai-Seale M, Millen M, Clay BJ, Longhurst CA. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. Journal of the American Medical Informatics Association. 2020 Jun;27(6):853-9.Doi: https://doi.org/10.1093/jamia/ocaa037.
7. Dagliati A, Malovini A, Tibollo V, Bellazzi R. Health informatics and EHR to support clinical research in the COVID-19 pandemic: an overview. Briefings in bioinformatics. 2021 Mar;22(2):812-22.Doi: https://doi.org/10.1093/bib/bbaa418.
8. Sapci AH, Sapci HA. Teaching hands-on informatics skills to future health informaticians: a competency framework proposal and analysis of health care informatics curricula. JMIR medical informatics. 2020 Jan 21;8(1):e15748.Doi: https://doi.org/10.2196/15748.
9. Xu J, Glicksberg BS, Su C, Walker P, Bian J, Wang F. Federated learning for healthcare informatics. Journal of healthcare informatics research. 2021 Mar;5:1-9.Doi: https://doi.org/10.1007/s41666-020-00082-4.
10. Durrani MI, Qureshi NS, Ahmad N, Naz T, Amelio A. A health informatics reporting system for technology illiterate workforce using mobile phone. Applied clinical informatics. 2019 Mar;10(02):348-57.Doi: https://doi.org/10.1055/s-0039-1688830.
11. Quinn TP, Senadeera M, Jacobs S, Coghlan S, Le V. Trust and medical AI: the challenges we face and the expertise needed to overcome them. Journal of the American Medical Informatics Association. 2021 Apr 1;28(4):890-4.Doi: https://doi.org/10.4102/sajim.v21i1.1069.
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Renuka Jyothi S, Sonia Mehta, Lulup Kumar Sahoo.
Data curation: Renuka Jyothi S, Sonia Mehta, Lulup Kumar Sahoo.
Formal analysis: Renuka Jyothi S, Sonia Mehta, Lulup Kumar Sahoo.
Drafting - original draft: Renuka Jyothi S, Sonia Mehta, Lulup Kumar Sahoo.
Writing - proofreading and editing: Renuka Jyothi S, Sonia Mehta, Lulup Kumar Sahoo.