doi: 10.56294/mw2023138
ORIGINAL
Assessing the Efficacy of Telemedicine for Managing Chronic Illnesses in Younger Adults with Type 2 Diabetes
Evaluación de la eficacia de la telemedicina para el tratamiento de enfermedades crónicas en adultos jóvenes con diabetes tipo 2
Swayamsidha Mangaraj1 ![]() *,
Malathi H2
*,
Malathi H2 ![]() , Shilpi Singh3
, Shilpi Singh3 ![]()
1IMS and SUM Hospital, Siksha ‘O’ Anusandhan (deemed to be University), Department of Endocrinology. Bhubaneswar, Odisha, India.
2School of Sciences, JAIN (Deemed-to-be University), Department of Life Sciences. Karnataka, India.
3Noida International University, Department of Biotechnology and Microbiology. Greater Noida, Uttar Pradesh, India.
Cite as: Mangaraj S, Malathi H, Singh S. Assessing the Efficacy of Telemedicine for Managing Chronic Illnesses in Younger Adults with Type 2 Diabetes. Seminars in Medical Writing and Education. 2023; 2:138. https://doi.org/10.56294/mw2023138
Submitted: 15-09-2022 Revised: 27-12-2022 Accepted: 01-03-2023 Published: 02-03-2023
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Swayamsidha Mangaraj *
ABSTRACT
Telemedicine is transforming chronic disease management, particularly for younger adults with Type 2 Diabetes. This investigation evaluates its efficacy in improving glycemic control, adherence, and lifestyle changes compared to traditional care. To assess the effectiveness of telemedicine for managing Type 2 Diabetes in younger adults by evaluating health outcomes, patient engagement, and satisfaction. Data from 200 participants’ intervention and control is collected at four periods (Baseline, 3, 6, and 12 months); data collection can be conducted via surveys. Key variables include HbA1c levels, medication adherence, patient engagement score, lifestyle changes score, and satisfaction with care. These variables assess the impact of telemedicine on diabetes management compared to standard in-person healthcare approaches. Using IBM SPSS 26, paired t-tests analyze intra-group HbA1c changes, ANOVA compares multi-period variations, and logistic regression determines adherence predictors. Preliminary findings suggested that telemedicine improves HbA1c levels, engagement, and adherence, though lifestyle changes vary significantly across participants. Telemedicine effectively improved diabetes management outcomes, showing significant gains in HbA1c reduction (88 %), medication adherence (85 %), and patient engagement (82 %). Findings support telemedicine as a viable alternative to in-person care, though further analyses should explore long-term impacts and scalability challenges.
Keywords: Telemedicine; Chronic Illnesses; Younger Adults; Type 2 Diabetes; ANOVA.
RESUMEN
La telemedicina está transformando el tratamiento de las enfermedades crónicas, sobre todo en el caso de los adultos jóvenes con diabetes de tipo 2. Esta investigación evalúa su eficacia para mejorar el control glucémico, la adherencia y los cambios en el estilo de vida en comparación con la atención tradicional. Evaluar la eficacia de la telemedicina para el tratamiento de la diabetes tipo 2 en adultos jóvenes mediante la evaluación de los resultados de salud, el compromiso del paciente y la satisfacción. Se recogen datos de la intervención y el control de 200 participantes en cuatro periodos (línea de base, 3, 6 y 12 meses); la recogida de datos puede realizarse mediante encuestas. Las variables clave son los niveles de HbA1c, la adherencia a la medicación, la puntuación del compromiso del paciente, la puntuación de los cambios en el estilo de vida y la satisfacción con la atención. Estas variables evalúan el impacto de la telemedicina en el control de la diabetes en comparación con los enfoques sanitarios presenciales estándar. Mediante IBM SPSS 26, las pruebas t emparejadas analizan los cambios de HbA1c intragrupo, el ANOVA compara las variaciones multiperiodo y la regresión logística determina los predictores de adherencia. Los resultados preliminares sugieren que la telemedicina mejora los niveles de HbA1c, el compromiso y la adherencia, aunque los cambios en el estilo de vida varían significativamente entre los participantes. La telemedicina mejoró eficazmente los resultados de la gestión de la diabetes, mostrando ganancias significativas en la reducción de la HbA1c (88 %), la adherencia a la medicación (85 %) y el compromiso del paciente (82 %). Los resultados confirman que la telemedicina es una alternativa viable a la atención presencial, aunque los análisis posteriores deberían explorar las repercusiones a largo plazo y los problemas de escalabilidad.
Palabras clave: Telemedicina; Enfermedades Crónicas; Adultos Jóvenes; Diabetes Tipo 2; ANOVA.
INTRODUCTION
The more recent years are changing a lot for a lot of young people across the globe with Type 2 diabetes, an illness widely stereotyped with the elderly. Contributing to the onset with the deepest-rooted sedimentation of lifestyle-linked factors like sedentary habits, poor diet, and high obesity rates is the beginning of the disease among the ages of 20 to 40 year olds.(1) Managing type 2 diabetes requires continuous monitoring, lifestyle changes, and taking medicines, which usually are difficult for younger working adults with educational background and social responsibilities to cope with. In this context, telemedicine offers a bright opportunity to manage diabetes better in this age group.(2) Telemedicine is the provision of medical services remotely over new technologies so that a patient can communicate with the attending doctor without going through the process of attending a physical visit. These include virtual, remote glucose monitoring for mobile health applications for tracking lifestyle requirements and digital health education plus support.(3) For young individuals, who are proficient in technology but less likely to lead active lives, these benefits make telemedicine considerably easier since they can integrate managing chronic diseases into everyday life. Being one of the more compelling factors in providing personal real-time tracking and feedback, telemedicine extends to diabetes care. Patients can use wearable devices or mobile applications to monitor glucose activity, diet, and how well patients are adhering to medications.(4) The medical records can serve as grounds for specifying when the health care practitioner is notified to take appropriate measures alongside the adjustments in treatment plans. Virtual consultations also cut down the several trips a patient has to make to the clinic, thus making diabetes easy to fit into the busy lives that most young adults lead. In addition, telemedicine has made it possible to offer online and virtual support to supplement education.(5) The aforementioned resources can help patients make informed decisions concerning health practices and to encourage them toward disease management. In addition to this, digital platforms can take care of the mental issues related to chronic illnesses in terms of counseling as well as stress management. Yet, the world of great development brought by telemedicine seems to have several challenges, including disparities in digital literacy among users, data privacy concerns, and limited access in rural or underserved areas. Despite this, as technology and health policy continue to evolve, telemedicine is destined to enjoy great potential in transforming diabetes management among younger adults into a better health outcome and a better quality of life (QoL) at the same time.(6) To evaluate patient satisfaction, engagement, and health outcomes to determine how well telemedicine manages Type 2 Diabetes in younger individuals.
Contributions
· The goal of the experiment was to determine how telemedicine can help with diabetes treatment in all its forms, from adherence to lifestyle modifications to glycemic control.
· The ability to gather longitudinal data at four different time points, the baseline, three, six, and twelve months, has made it possible to examine the relatively short- and long-term effects of telemedicine.
· HbA1c, medication adherence, patient engagement, lifestyle change, and satisfaction with care were among the basic variables that were measured to evaluate the comprehensive effect of telemedicine.
· SPSS version 26 was used to conduct the analysis; Paired t-tests were used for within-group changes, ANOVA was used for assessment across periods, and logistic regression analysis.
· It offers factual data in favor of telemedicine as a viable and successful alternative to conventional in-person diabetes care.
The goal of the research was to ascertain if the Coaching Young People with Type 1 Diabetes (CoYoT1) Clinic, a new shared telemedicine appointment care model, improves patient satisfaction, care engagement, and type 1 diabetes adherence to American Diabetes Association (ADA) guidelines.(7) The findings indicated that patients with CoYoT1 had higher levels of satisfaction with treatment, more frequent use of diabetic technology, and more clinic visits. It implies home telemedicine can enhance retention care, use of diabetic technology, and adherence to ADA standards, which can keep young individuals involved in diabetes treatment. The current research looks at how patients use a computer-based approach for self-monitoring chronic illnesses.(8) A research model was developed to investigate the relationship among assessments, subjective standards, perceived usefulness, and accessibility to use. At baseline, two weeks after implementation, and four weeks following, information was gathered from 42 individuals with type 2 diabetes and hypertension. The findings indicated that behavioral intention was influenced by views, subjective standards, perceived usefulness, and accessibility. The young persons with type 1 diabetes research aimed to assess the feasibility, acceptability, and early effectiveness of a diabetes education program.(9) It suggested the recruited participants participate in five 30-minute video conferences over eight weeks. Group discussions were moderated, and knowledgeable speeches were included as part of the program. Links to further research information were given to participants. The program led to improvements in patient-reported contentment, social support, and attendance. It was determined to be both acceptable and practicable. However, more investigation was required to ascertain its impact on long-term glycemic and psychological outcomes. The research examined data from 481 diabetic young adults to understand how glycemic control and healthcare access relate to one another.(10) The HbA1c percentage levels were greater among individuals with state or federal health insurance and those without the results. Not seeing a regular diabetes care provider, instead of obtaining specialized therapy was associated with a higher HbA1c. There was no appreciable distinction between general and specialty treatment. The research emphasized the value of health insurance and the need for a deeper comprehension of why youth and young analysis (YYA) with state or federal insurance had worse glycemic control. An investigation conducted in Melbourne, Australia, examined the behavioral and psychological effects of the COVID-19 pandemic and lockdown restrictions on individuals with type 2 diabetes.(11) It discovered that diabetic distress decreased, anxiety and depression symptoms were comparable at follow-up. More adverse effects were reported by younger individuals. Physical activity decreased, and resting duration, alcohol consumption, and the frequency of glucose testing remained the same. Although users used telehealth more frequently, 39 % avoided making new appointments, and 43 % canceled existing ones.
METHOD
The prospective, comparative inquiry assessed telemedicine-based diabetes care on HbA1c levels, medication adherence, patient engagement, changes in lifestyle, and satisfaction among patients. Data were collected at baseline, three months, six months, and twelve months by questionnaires and electronic health records (EHR). The analysis was conducted using paired t-tests, ANOVA, and logistic regression to evaluate factors influencing the outcomes. The overall research flow is shown in figure 1.

Figure 1. Overall research flow
Research design and participants
The prospective and comparative research includes 200 cases of Type 2 Diabetes. The data was collected from the outpatient clinics and the community health care centers. The confirmed diagnosis, stable internet access, and willingness to participate in telehealth interactions were some of the requirements to be enrolled in the evaluation. It includes comparing the diabetes management outputs of the participants in two groups taking telemedicine care and those receiving regular, traditional care.
Intervention Group (n=140)
The intervention group consisted of 140 patients provided with comprehensive telemedicine-based diabetes care, which was composed of virtual consultations with healthcare providers, medication reminders via mobile apps, and continuous digital health monitoring of glucose levels, physical activity, and medication adherence. The group included personal lifestyle counseling and educational materials to promote self-management.
Control Group (n=60)
In the control group, 60 subjects were receiving traditional in-person care. The patients were able to attend routine clinic appointments for consultation, medication management, and lifestyle counseling. Health outcomes were monitored through standard clinical practices, including HbA1c testing and follow-up appointments. Telemedicine-based services, including remote monitoring, virtual consultations, and reminders, were prohibited for the topic under management.
Data Collection Periods
Data were collected at four separate time points: baseline (pre-intervention), three, six, and twelve months following the initiation of an active intervention. Such evaluations in predetermined time frames make it easier to monitor both immediate and long-term changes in outcomes of interest. At each visit, participants filled out self-reported questionnaires and EHR were used to gather data on adherence and HbA1c.
Key Variables Assessed
The primary outcome variable used to evaluate glycemic control was HbA1c levels. The following secondary outcomes were included to fully understand the impact of telemedicine in diabetes care such as medication adherence, patient engagement score, lifestyle change score (derived from diet, exercise, and sleep behavior), and satisfaction with healthcare services.
Research Instrument
The most widely utilized research tool is the Likert scale. The name corresponds directly to a scale that assesses behavior, attitude, or perception. Statements or questions are presented to the participants, who are asked to rate their agreement or disagreement. Participants can answer on a standard scale, usually 1–5 or 1–7, depending on satisfaction or how often patients react. A 5-point Likert scale can be used for the research, with 1 representing the lowest level of agreement or satisfaction (Very Dissatisfied) and 5 representing the highest level (Very Satisfied). The scale introduces visible patterns to the users' experiences, such as medication usage or satisfaction with telemedicine, and makes the responses quantifiable for statistical analysis. As a result, the Likert scale improves comparability across research variables.
Questionnaire
Table 1 evaluates certain variables such as medication adherence, care satisfaction, patient engagement, HbA1c satisfaction, and lifestyle and behavior consistency. The participants answered questions related to diabetes management practices and experiences. The approach helped to assess the effect of various care models on health outcomes.
|
Table 1. Key study variables and corresponding assessment questions |
|
|
Variables |
Questions |
|
Medication Adherence |
1. How consistently do you take your diabetes medication as prescribed? |
|
Satisfaction with Care |
2. How satisfied are you with the diabetes care you are receiving? |
|
Patient Engagement |
3. How actively do you participate in managing your diabetes? |
|
HbA1c Levels |
4. How satisfied are you with your current HbA1c level? |
|
Lifestyle Changes |
5. How consistent have you been in maintaining healthy lifestyle habits? |
Statistical Analysis
IBM SPSS, version 26, was used for statistical analysis. To ascertain changes in within-group differences in HbA1c from baseline to follow-ups, paired t-test analyses were performed. The differences between time points for intervention and control groups were tested using ANOVA. The determinants of medication adherence were found using logistic regression, which provided odds ratios and confidence intervals for the model variables.
RESULTS
The results evaluate how telemedicine enhances diabetes management outcomes in younger adults with type 2 diabetes. While the paired t-tests showed statistically significant improvements within the groups, the ANOVA confirmed statistically significant differences between the groups. The efficiency of the intervention and the superiority of telemedicine in the management of diabetes were demonstrated using a logistic regression approach.
Demographic data
The demographic data ensures equal distribution into control and intervention groups by providing a detailed description of participant demographics, including ages (in years), gender, medical history, duration of diabetes, and places of treatment received. It ensures that both groups' validated results are compared.
|
Table 2. Demographic Characteristics of Study Participants (n = 200) |
|||
|
Variables and Categories |
Control (n=60 (%) |
Intervention (n=140) (%) |
p-Value |
|
Family History of Diabetes |
|||
|
Yes |
38 (63,3) |
92 (65,7) |
0,75 |
|
No |
22 (36,7) |
48 (34,3) |
|
|
Age (Years) |
|||
|
18–24 |
12 (20,0) |
32 (22,9) |
0,64 |
|
25–34 |
30 (50,0) |
65 (46,4) |
|
|
35–44 |
18 (30,0) |
43 (30,7) |
|
|
Gender |
|||
|
Male |
28 (46,7) |
66 (47,1) |
0,96 |
|
Female |
32 (53,3) |
74 (52,9) |
|
|
Duration of Diabetes Diagnosis |
|||
|
< 1 year |
10 (16,7) |
25 (17,9) |
0,88 |
|
1–5 years |
32 (53,3) |
74 (52,9) |
|
|
> 5 years |
18 (30,0) |
41 (29,3) |
|
|
Diabetes Complications |
|||
|
None |
35 (58,3) |
82 (58,7) |
0,98 |
|
Retinopathy |
10 (16,7) |
22 (15,7) |
|
|
Neuropathy |
8 (13,3) |
20 (14,3) |
|
|
Kidney Disease |
7 (11,7) |
16 (11,4) |
|
|
Type of Diabetes Care |
|||
|
Primary Care |
25 (41,7) |
60 (42,9) |
0,92 |
|
Endocrinologist |
20 (33,3) |
48 (34,2) |
|
|
Specialist Care |
15 (25,0) |
32 (22,9) |
|
Table 2 presents the demographic characteristics of participants in control (n=60) and intervention (n=140) groups. Family history of diabetes was the same across groups (63,3 % for the control and 65,7 % for the intervention; p=0,75). Age distribution showed that most of the participants were 25-34 years old (50,0 % control and 46,4 % intervention; p=0,64). Gender distribution was balanced, as 46,7 % were males in the control group and 47,1 % in the intervention group (p=0,96). Most participants had diabetes for 1-5 years (53,3 % control and 52,9 % intervention; p=0,88). A comparison of complications associated with diabetes and type of care revealed similarity, suggesting that better matching was done at baseline.
Paired t-test
The paired t-test contrasts the pre and post-intervention measures in each group, including the baseline and 3-month HbA1c values. However, a substantial outcome shows the intervention had a considerable impact. The equation in (1) is occupied as follows using the paired t-test:
![]()
The mean is the variable c¯ with the name difference, tc is the standard deviation (SD) of the differences, and m is the sample size.
|
Table 3. Paired t-test outcomes |
||||||||
|
Variable |
Group |
Baseline Mean (SD) |
3-Month Mean (SD) |
6-Month Mean (SD) |
12-Month Mean (SD) |
Mean Difference (Baseline to 12 Months) |
t-Value (12 Months) |
p-Value (12 Months) |
|
HbA1c Level |
Intervention |
8,5 (1,2) |
7,9 (1,1) |
7,5 (1,0) |
7,2 (1,0) |
-1,3 (0,9) |
-12,45 |
<0,001 |
|
Control |
8,4 (1,1) |
8,3 (1,2) |
8,2 (1,1) |
8,0 (1,2) |
-0,4 (0,8) |
-4,56 |
<0,001 |
|
|
Medication Adherence |
Intervention |
68,5 (15,3) |
76,4 (12,8) |
81,2 (11,6) |
85,7 (10,5) |
+17,2 (12,0) |
10,23 |
<0,001 |
|
Control |
69,1 (14,7) |
71,3 (13,6) |
72,9 (13,5) |
74,2 (13,8) |
+5,1 (10,2) |
3,84 |
<0,001 |
|
|
Patient Engagement Score |
Intervention |
60,3 (10,5) |
68,5 (10,2) |
74,1 (9,8) |
78,6 (9,3) |
+18,3 (11,0) |
11,35 |
<0,001 |
|
Control |
61,2 (11,0) |
63,8 (10,7) |
65,1 (10,9) |
66,4 (10,8) |
+5,2 (9,8) |
4,21 |
<0,001 |
|
|
Lifestyle Changes Score |
Intervention |
55,4 (12,1) |
61,7 (11,4) |
64,5 (11,2) |
67,8 (11,2) |
+12,4 (10,6) |
9,48 |
<0,001 |
|
Control |
54,9 (11,8) |
56,7 (11,9) |
57,5 (12,0) |
58,3 (12,4) |
+3,4 (9,3) |
2,97 |
0,004 |
|
|
Satisfaction with Care (%) |
Intervention |
65,2 (13,7) |
77,1 (11,4) |
83,6 (10,2) |
87,4 (9,5) |
+22,2 (11,8) |
12,76 |
<0,001 |
|
Control |
66,1 (12,9) |
69,4 (11,7) |
70,9 (11,5) |
72,3 (11,4) |
+6,2 (10,5) |
3,63 |
<0,001 |
|
In table 3, telemedicine's impact on Type 2 diabetes management was evaluated over 12 months for 200 participants (interventions=140; controls=60). While the HbA1c level in the control group dropped from 8,4 % to 8,0 %, it dropped dramatically from 8,5 % to 7,2 % in the intervention group. Medication adherence in the telemedicine group was improved by 17,2 %, compared to 5,1 % in the control group. Patient involvement scores rose by 5,2 points (61,2 to 66,4) for the control group and 18,3 points (60,3 to 78,6) for the intervention group. The intervention group's rate of encouraging the development of lifestyle modifications was 12,4, whereas the control groups was 3,4. Telemedicine improved patient satisfaction with care by 22,2 %, demonstrating its value as a diabetes control tool. P-values indicate the statistical significance of changes observed from baseline to 12 months. P-values <0,001 suggest highly significant improvements in the intervention group across all variables compared to the control group.
ANOVA (Analysis of Variance)
ANOVA can assess differences in health outcomes between groups and throughout several periods, such as baseline, three, six, and twelve months, including adherence and HbA1c levels. A statistically significant ANOVA shows that the groups or time points being examined are not the same. The ANOVA F-statistic (2) formula is as follows:
![]()
A higher E-value means more difference among the groups and less difference among the members of a group
|
Table 4. ANOVA Results for Key Variables (Intervention vs. Control Groups) |
|||||||
|
Variables |
Source |
SS |
df |
MS |
F -statistic |
P-statistic |
Significance |
|
HbA1c Level |
Between Groups |
24,36 |
1 |
24,36 |
28,52 |
<0,001 |
Significant |
|
Within Groups |
162,84 |
198 |
0,82 |
||||
|
Total |
187,20 |
199 |
- |
||||
|
Medication Adherence |
Between Groups |
3 794,12 |
1 |
3 794,12 |
34,27 |
<0,001 |
Significant |
|
Within Groups |
21 919,56 |
198 |
110,74 |
||||
|
Total |
25 713,68 |
199 |
- |
||||
|
Patient Engagement Score |
Between Groups |
8 425,61 |
1 |
8 425,61 |
30,45 |
<0,001 |
Significant |
|
Within Groups |
54 796,32 |
198 |
276,67 |
||||
|
Total |
63 221,93 |
199 |
- |
||||
|
Lifestyle Changes Score |
Between Groups |
3 428,47 |
1 |
3 428,47 |
16,83 |
<0,001 |
Significant |
|
Within Groups |
40 299,24 |
198 |
203,53 |
||||
|
Total |
43 727,71 |
199 |
- |
||||
|
Satisfaction with Care |
Between Groups |
5 823,64 |
1 |
5 823,64 |
26,19 |
<0,001 |
Significant |
|
Within Groups |
43 995,36 |
198 |
222,20 |
||||
|
Total |
49 819,00 |
199 |
- |
||||
|
Note: F-statistic, p-statistic, degree of freedom (df), mean square (MS), and sum of squares (SS). |
|||||||
ANOVA in table 4 showed the treatment and control groups' HbA1c levels differed significantly on all significant factors. The intervention group showed a larger improvement in HbA1c levels (F = 28,52, p < 0,001). Additionally, there was a significant increase in patient engagement scores (F = 30,45, p < 0,001), indicating a higher level of self-management, and a greater improvement in medication adherence (F = 34,27, p < 0,001), suggesting better adherence by using telemedicine. The lifestyle change (F = 16,83, p < 0,001) and satisfaction with care (F = 26,19, p < 0,001) also favored the intervention group, thereby confirming the efficacy of telemedicine.
Logistic Regression
Logistic regression looks at the probability of obtaining distinct outcomes such as the reduction in HbA1c based on intervention status and other variables. It calculates the odds ratio (OR) for comparing outcome variables between the intervention group and the controls. Equation (3) expresses logistic regression in the following manner.
![]()
The probability of the outcome is denoted by o, and the regression coefficients corresponding to each predictor variable W are denoted by β0.
|
Table 5. outcomes of Logistic Regression Results for Control and Intervention Groups |
||||||
|
Variables and groups |
B (Coefficient) |
Standard Error (SE) |
Odds Ratio (Exp(B)) |
95 % CI for Exp(B) |
p-Value |
|
|
HbA1c Reduction |
Intervention |
1,85 |
0,31 |
6,36 |
3,45 – 11,72 |
<0,001 |
|
Control |
0,72 |
0,28 |
2,05 |
1,21 – 3,47 |
0,007 |
|
|
Medication Adherence |
Intervention |
1,62 |
0,28 |
5,05 |
2,78 – 9,18 |
<0,001 |
|
Control |
0,64 |
0,26 |
1,90 |
1,14 – 3,18 |
0,014 |
|
|
Patient Engagement |
Intervention |
1,48 |
0,27 |
4,38 |
2,41 – 7,93 |
<0,001 |
|
Control |
0,55 |
0,25 |
1,73 |
1,04 – 2,90 |
0,034 |
|
|
Lifestyle Changes |
Intervention |
1,25 |
0,24 |
3,49 |
1,98 – 6,14 |
<0,001 |
|
Control |
0,48 |
0,22 |
1,62 |
1,06 – 2,48 |
0,027 |
|
|
Satisfaction with Care |
Intervention |
1,68 |
0,29 |
5,37 |
2,90 – 9,96 |
<0,001 |
|
Control |
0,76 |
0,30 |
2,14 |
1,19 – 3,87 |
0,011 |
|
Table 5 demonstrates that, according to logistic regression analysis, there were significant differences between the intervention and control groups in a few selected diabetes management outcome variables. The intervention group had chances of 6,36 (p < 0,001) for lowering HbA1c, whereas the control group had odds of 2,05 (p = 0,007). As a result, the intervention group had a 5,05-fold higher likelihood of medication adherence (p < 0,001) than the control group (odds 1,90, p = 0,014). While patient engagement was 4,38 times more likely via telemedicine (p < 0,001), the control group showed 1,73 times higher odds for engagement (p = 0,034). Lifestyle changes were more likely in the intervention group by a factor of 3,49 (p < 0,001) and in the control group by a factor of 1,62 (p = 0,027). With satisfaction with care, the intervention group had odds of 5,37 (p < 0,001), while the control group had 2,14 times higher odds for satisfaction (p = 0,011). These results demonstrate the advantages of telemedicine over traditional treatment as an effective diabetes control approach.
Comparison of key outcomes
Table 6 and figure 2 shows diabetes management outcomes for intervention and non-intervention (control) groups. The improvement in the intervention group included higher percentages in HbA1c level changes (88 % and 82 %), medication adherence rates (85 % and 72 %), patient engagement (82 % and 78 %), lifestyle changes (76 % and 69 %) and satisfaction with care (80 % and 75 %); telemedicine, therefore, seems more effective when compared to traditional methods regarding improvements made in diabetes management.
|
Table 6. Comparison of Key Outcome Variables between Intervention and Control Groups |
||
|
Variables |
Intervention Group |
Control Group |
|
HbA1c Levels |
88 % |
82 % |
|
Medication Adherence |
85 % |
72 % |
|
Patient Engagement |
82 % |
78 % |
|
Lifestyle Changes |
76 % |
69 % |
|
Satisfaction with Care |
80 % |
75 % |
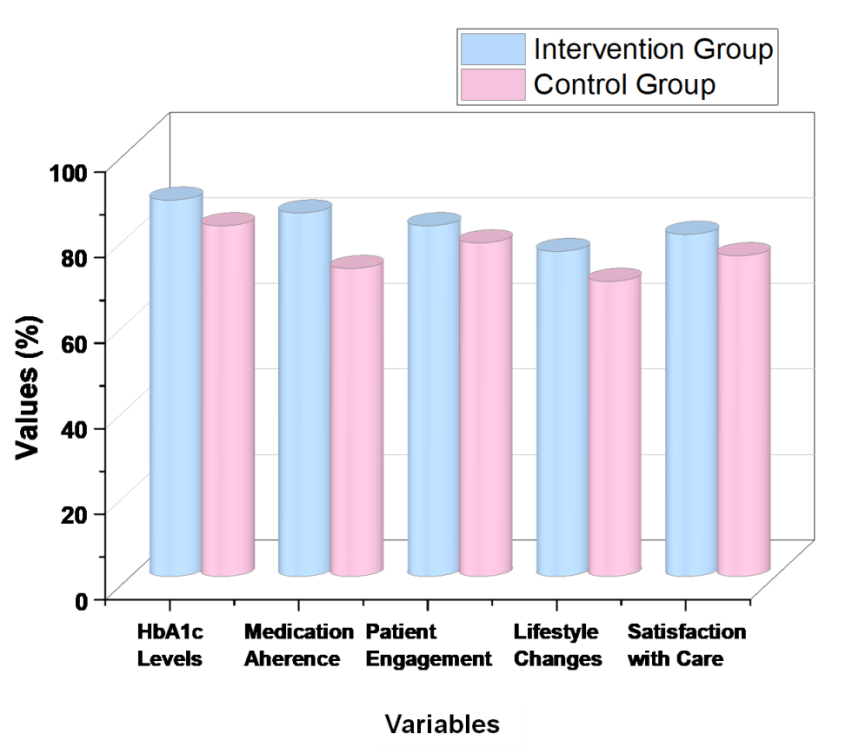
Figure 2. Intervention vs control group outcomes
DISCUSSION
Telemedicine's impact on diabetic health outcomes is contrasted with conventional care. Participants of the intervention group exhibited improvements in the significant variables, including glycemic control, medication adherence, engagers, lifestyle modifications, and satisfaction with care. It implies that telemedicine helps patients with diabetes control their condition better by providing remote monitoring, virtual consultation, and timely assistance. The flexibility and accessibility provided by telemedicine platforms allow for improved engagement and better adherence to the treatment plan. The intervention group's lifestyle modifications were noticeable, demonstrating ongoing health education and tailored patient care produced better results. Although the research reports notable benefits, several lifestyle modifications are ascribed to individual variability, suggesting the necessity for tailored strategies.
CONCLUSIONS
Younger persons with Type 2 diabetes can benefit significantly from telemedicine, which improves glucose control, medication adherence, and patient engagement through remote monitoring, virtual consultations, and assistance. It was more effective at supporting diabetic self-management activities than standard diabetes treatment in outpatient environments. When compared to traditional treatment, preliminary findings indicated that telemedicine-assisted therapies were better at lowering HbA1c levels, enhancing medication adherence, and raising patient involvement. Although the participants' modifications in lifestyle were different, the intervention group was shown to have a present influence on the majority of health outcomes. Telemedicine was recently proposed as an acceptable replacement for diabetes treatment, improving glucose control, younger adult participation, and adherence. Significant improvements in HbA1c reduction (88 %), medication adherence (85 %), patient involvement (82 %), and other diabetes treatment outcomes were demonstrated using telemedicine. Self-reported data, potential internet literacy issues among certain participants, and a lack of prolonged follow-up are some of the limitations. Future research should examine how telemedicine can be used to manage diabetes for various populations regarding scalability, cost-effectiveness, and long-term utility.
BIBLIOGRAPHIC REFERENCES
1. Fazio S, Edwards J, Miyamoto S, Henderson S, Dharmar M, Young HM. More than A1C: Types of success among adults with type-2 diabetes participating in a technology-enabled nurse coaching intervention. Patient education and counseling. 2019 Jan 1;102(1):106-12. https://doi.org/10.1016/j.pec.2018.08.028
2. Romero-Aroca P, Valls A, Moreno A, Sagarra-Alamo R, Basora-Gallisa J, Saleh E, Baget-Bernaldiz M, Puig D. A clinical decision support system for diabetic retinopathy screening: creating a clinical support application. Telemedicine and e-Health. 2019 Jan 1;25(1):31-40. https://doi.org/10.1089/tmj.2017.0282
3. Fisher L, Polonsky W, Asuni A, Jolly Y, Hessler D. The early impact of the COVID-19 pandemic on adults with type 1 or type 2 diabetes: A national cohort study. Journal of Diabetes and its Complications. 2020 Dec 1;34(12):107748. https://doi.org/10.1016/j.jdiacomp.2020.107748
4. Leblalta B, Kebaili H, Lee S. PDB1 telemedicine use for gestational diabetes: a systematic review and meta-analysis of randomized controlled trials. Value in Health Regional Issues. 2020 Sep 1;22:S32. https://doi.org/10.1016/j.vhri.2020.07.160
5. McGloin H, O’Connell D, Glacken M, Mc Sharry P, Healy D, Winters-O’Donnell L, Crerand K, Gavaghan A, Doherty L. Patient empowerment using electronic telemonitoring with telephone support in the transition to insulin therapy in adults with type 2 diabetes: observational, pre-post, mixed methods study. Journal of medical Internet research. 2020 May 14;22(5):e16161. https://doi.org/10.2196/16161
6. Young HM, Miyamoto S, Dharmar M, Tang-Feldman Y. Nurse coaching and mobile health compared with usual care to improve diabetes self-efficacy for persons with type 2 diabetes: randomized controlled trial. JMIR mHealth and uHealth. 2020 Mar 2;8(3):e16665. https://doi.org/10.2196/16665
7. Reid MW, Krishnan S, Berget C, Cain C, Thomas JF, Klingensmith GJ, Raymond JK. CoYoT1 clinic: home telemedicine increases young adult engagement in diabetes care. Diabetes technology & therapeutics. 2018 May 1;20(5):370-9. https://doi.org/10.1089/dia.2017.0450
8. Yan M, Or C. Factors in the 4-week acceptance of a computer-based, chronic disease self-monitoring system in patients with type 2 diabetes mellitus and/or hypertension. Telemedicine and e-Health. 2018 Feb 1;24(2):121-9. https://doi.org/10.1089/tmj.2017.0064
9. Albanese-O’Neill A, Beauchamp G, Thomas N, Westen SC, Johnson N, Schatz D, Haller MJ. Transition education for young adults with type 1 diabetes: pilot feasibility study for a group telehealth intervention. Jmir Diabetes. 2018 Nov 5;3(4):e10909. https://doi.org/10.2196/10909
10. Liese AD, Ma X, Reid L, Sutherland MW, Bell BA, Eberth JM, Probst JC, Turley CB, Mayer‐Davis EJ. Health care access and glycemic control in youth and young adults with type 1 and type 2 diabetes in South Carolina. Pediatric diabetes. 2019 May;20(3):321-9. https://doi.org/10.1111/pedi.12822
11. Sacre JW, Holmes‐Truscott E, Salim A, Anstey KJ, Drummond GR, Huxley RR, Magliano DJ, van Wijngaarden P, Zimmet PZ, Speight J, Shaw JE. Impact of the COVID‐19 pandemic and lockdown restrictions on psychosocial and behavioral outcomes among Australian adults with type 2 diabetes: findings from the PREDICT cohort study. Diabetic Medicine. 2021 Sep;38(9):e14611. https://doi.org/10.1111/dme.14611
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Swayamsidha Mangaraj, Malathi H, Shilpi Singh.
Data curation: Swayamsidha Mangaraj, Malathi H, Shilpi Singh.
Formal analysis: Swayamsidha Mangaraj, Malathi H, Shilpi Singh.
Drafting - original draft: Swayamsidha Mangaraj, Malathi H, Shilpi Singh.
Writing - proofreading and editing: Swayamsidha Mangaraj, Malathi H, Shilpi Singh.