doi: 10.56294/mw2023140
ORIGINAL
Integrating Electronic Health Records to Address Clinician Burnout and Improve Workplace Well-being in Healthcare Settings
Integración de las historias clínicas electrónicas para abordar el agotamiento de los médicos y mejorar el bienestar laboral en los centros sanitarios
Suhas Ballal1 ![]() *, Supriya
Awasthi2
*, Supriya
Awasthi2 ![]() , Maitreyee Panda3
, Maitreyee Panda3 ![]()
1School of Sciences, JAIN (Deemed-to-be University), Department of Biochemistry. Karnataka, India.
2School of Allied Health Sciences, Noida International University. Greater Noida, Uttar Pradesh, India.
3IMS and SUM Hospital, Siksha ‘O’ Anusandhan (deemed to be University), Department of Skin & Vd. Bhubaneswar, Odisha, India.
Cite as: Ballal S, Awasthi S, Panda M. Integrating Electronic Health Records to Address Clinician Burnout and Improve Workplace Well-being in Healthcare Settings. Seminars in Medical Writing and Education. 2023; 2:140. https://doi.org/10.56294/mw2023140
Submitted: 16-09-2022 Revised: 28-12-2022 Accepted: 01-06-2023 Published: 02-03-2023
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Suhas Ballal *
ABSTRACT
In the medical field, clinician burnout is a serious issue that has a negative influence on both the standard of patient care and professionals. To reduce clinician burnout and improve workplace well-being, it investigates the use of Electronic Health Records (EHRs). Focusing on healthcare environments, explore how EHRs can automate workflows, minimize administrative burdens, and facilitate communication among healthcare teams. Data were gathered by a survey given to 450 healthcare workers in different institutions that have installed EHR systems. The survey measured levels of clinician burnout, job satisfaction, and perceived effectiveness of the EHR system. Statistical analysis involved the use of three tests: Paired t-tests for burnout level comparisons before and after EHR integration, ANOVA for assessment of burnout level differences in various healthcare environments with different EHR stages of adoption, and Pearson’s correlation to inspect the suggestion among the usability of EHR systems and clinician well-being. The use of EHRs has been demonstrated to significantly reduce burnout, enhance job satisfaction, and enhance team collaboration in the healthcare sector. Nevertheless, issues including insufficient training and system interoperability were identified. According to the exploration, well-designed EHR systems that are adapted to the needs of practitioners can lessen administrative burden and promote a more encouraging workplace. Further research on the long-term effects of EHR systems on physician retention and mental health is suggested, along with recommendations for enhancing EHR adoption and continuing clinical support.
Keywords: Electronic Health Records (EHRs); Clinician Burnout; Healthcare Settings; Job Satisfaction; Healthcare Professionals; Mental Health.
RESUMEN
En el ámbito médico, el burnout del clínico es un problema grave que influye negativamente tanto en el nivel de atención al paciente como en el de los profesionales. Para reducir el burnout de los clínicos y mejorar el bienestar laboral, se investiga el uso de las historias clínicas electrónicas (HCE). Centrándose en los entornos sanitarios, explora cómo las HCE pueden automatizar los flujos de trabajo, minimizar las cargas administrativas y facilitar la comunicación entre los equipos sanitarios. Los datos se recogieron mediante una encuesta realizada a 450 trabajadores sanitarios de distintas instituciones que han instalado sistemas de HCE. La encuesta midió los niveles de agotamiento del personal clínico, la satisfacción laboral y la eficacia percibida del sistema de HCE. Para el análisis estadístico se utilizaron tres pruebas: Pruebas t pareadas para comparar los niveles de burnout antes y después de la integración de la HCE, ANOVA para evaluar las diferencias en los niveles de burnout en distintos entornos sanitarios con diferentes estadios de adopción de la HCE, y correlación de Pearson para inspeccionar la sugerencia entre la usabilidad de los sistemas de HCE y el bienestar de los clínicos. Se ha demostrado que el uso de HCE reduce significativamente el burnout, aumenta la satisfacción laboral y mejora la colaboración en equipo en el sector sanitario. No obstante, se identificaron problemas como la formación insuficiente y la interoperabilidad de los sistemas. Según la exploración, los sistemas de HCE bien diseñados y adaptados a las necesidades de los profesionales pueden disminuir la carga administrativa y promover un lugar de trabajo más alentador. Se sugieren nuevas investigaciones sobre los efectos a largo plazo de los sistemas de HCE en la retención y la salud mental de los médicos, junto con recomendaciones para mejorar la adopción de HCE y el apoyo clínico continuado.
Palabras clave: Historias Clínicas Electrónicas (HCE); Burnout Clínico; Entornos Sanitarios; Satisfacción Laboral; Profesionales Sanitarios; Salud Mental.
INTRODUCTION
Clinician burnout is a significant problem in today's healthcare systems that affects doctors, nurses, and other medical professionals globally.(1) Emotional weariness, depersonalization, and a decline in personal accomplishment were signs of burnout, which raised turnover, reduced productivity, and lowered job satisfaction. The overwhelming administrative burden, particularly the extensive it required for patient care, was one of the main reasons for burnout among clinicians.(2) Ineffective digital technologies and conventional Keeping records on material led to long workdays, elevated stress levels, and less time for direct patient care. Health workers frequently experience tremendous physical and emotional strain that compromises both their well-being and the standard of patient care.(3) Electronic Health Records (EHRs) were generally regarded as the most effective means of automating administrative duties and improving workplace productivity. EHRs were computerized systems that let healthcare companies store, manage, and securely access patient data. EHRs reduce mistakes, boost the availability of critical patient data, and remove redundancy by automating human documentation operations.(4) When the technologies were properly implemented, clinicians could spend longer caring for patients and less time on unnecessary paperwork. Despite the many advantages of EHRs, healthcare personnel might experience even more stress and annoyance as a result of poor system design, insufficient training, and workflow disruptions.(5) Despite these issues, effective implementation of EHRs could greatly enhance workplace health and mitigate burnout. Well-functioning EHR systems could decrease cognitive overload, streamline repetitive tasks, and enable more effective team communication in healthcare.(6) EHRs also help to enhance workplace well-being by enhancing workflow efficiency, which ensures doctors' general well-being, work-life balance, and job satisfaction. In addition, well-designed EHR systems could facilitate evidence-based practice, decrease the possibility of medical errors, and enable real-time access to patient data to support better decision-making.(7) Predictive analytics, automated reminders, and clinical decision support systems were some examples of higher-level capabilities that could further optimize treatment while decreasing the cognitive load on physicians. Moreover, interoperability between healthcare systems facilitates unimpeded communication and coordination among varied teams, which enhances overall performance.(8)
With logistic and linear regressions, it evaluated the burnout and stress that 282 clinicians felt about the Electronic Health Record (EHR) design.(9) The most critical factors were too much data entry (86,9 %), conflict between work and life (63,1 %), and long notes (75,2 %). 36,2 % of the difference in burnout and 58,1 % of the alteration in pressure were explained by the work environment. Self-report assessments and institutional issues were among the weaknesses. Resolving EHR inefficiencies was crucial for the welfare of clinicians. The investigation used logistic regression to examine burnout from an online survey of 368 doctors.(10) According to the findings, 36 % of respondents had burnout, with the primary stressors being inadequate EHR training (43 %) and less patient engagement (38 %). Burnout risk was reduced by improved hospital preparedness and EHR usage. The primary constraints were local scope and self-reported data. According to the analysis, technical assistance, open policies, and formal training were necessary. An institution-wide assessment using the Maslach Burnout Inventory (MBI) was used to gauge burnout at Mount Sinai Health System (MSHS) from 2018 to 2019.(11)
According to logistic analysis, burnout was predicted with over 60 minutes of secretarial job duties and more than 90 minutes of EHR use apart from work. Self-reported data was not without limits. It identifies thresholds that need intervention measures and has an impact on physicians' well-being. A 2017 survey found that nurse-reported EHR usability and burnout connection were positively correlated.(12) An average System Usability Scale (SUS) of 57,6 was reported, with a 2 % decrease in burnout odds per 1-point increment. However, it acknowledges potential response bias and self-reported data limitations. It aims to address low EHR usability and its impact on clinician well-being, emphasizing the need for optimized digital systems to enhance workplace efficiency and minimize burnout. Strategies for enhancing EHR functionality were being explored. To examine the connection between EHR utilization measures and physician fatigue, it employed multivariate regression analysis.(13) The findings indicated that while high message volume increased the risk of exhaustion by 6,17 times, clinicians who worked on EHRs for more than 68 minutes after hours had odds of exhaustion that were 4,78–12,52 times higher. Limitations were sample specificity and possible unmeasured confounders. It emphasizes the necessity for targeted EHR interventions. A specialized unit's 19 Advanced Practice Providers (APPs) participated in a 2-week EHR optimization race, 39 training sessions (2,8 hours per provider), and 21 EHR updates made up the intervention.(14) The results showed no significant change in emotional measures or EHR time, but an increase in Net Promoter Score (NPS) from 6 to 60 (P=0,01). The sample size and short duration were limitations.
Aim: To evaluate the degree to which integrating Electronic Health Records (EHRs) improves workplace wellness, reduces clinician burnout, and boosts job satisfaction by maximizing throughput and minimizing administrative load.
METHOD
The method of the examination involved distributing an inspection to 450 medical professionals from different institutions that used Electronic Health Records (EHRs) at different levels. Clinical burnout, job satisfaction, work-life balance, administrative burden, and team collaboration were the five primary characteristics that were examined. ANOVA was employed to compare differences among institutions at varying levels of EHR implementation, Pearson's correlation to compare the relationship between EHR usability and clinician well-being, and paired t-tests to compare before and after data regarding EHR integration. SPSS software version 26 was used for all statistical analysis. The results were used to investigate how EHR incorporation affected job satisfaction, collaboration, and burnout reductions, as shown in figure 1.
Figure 1. Overall Flow for Electronic Health Records to Address Clinician Burnout and Improve Workplace Well-being
Design of Investigation
To investigate how EHR integration affects clinician burnout and workplace well-being, it will utilize a survey-based quantitative examination design, collecting numerical information from healthcare workers. To have a deeper insight into five main variables: clinician burnout, job satisfaction, work-life balance, administrative burden, and collaboration in teams. The measurement of the effect of EHR systems on these traits illustrates how these behaviours could diminish burnout and increase clinician well-being.
Clinician burnout
It refers to the mental and physical exhaustion experienced by healthcare professionals as a result of prolonged stress and excessive workloads. By streamlining processes and cutting down on unnecessary paperwork, EHRs aim to lessen weakness.
Job satisfaction
Overall job satisfaction and happiness that healthcare employee feels in their roles. Because of improved productivity and reduced annoyance with bureaucratic tasks, well-performing EHR systems could result in increased job satisfaction.
Work-Life Balance
The healthcare professionals are able to handle their workload without negatively affecting their personal time. EHRs can improve work-life balance by increasing efficiency and reducing post-hours paperwork.
Administrative Burden
The amount of time and energy spent on non-clinical tasks like data input and documentation. By improving data management and automating procedures, well-designed EHR systems can reduce this load.
Team Collaboration
Medical teams' ability to collaborate effectively, EHRs improves communication, allow for coordinated treatment, and provide real-time access to patient data, all of which promote teamwork.
Collection of data
It assessed Electronic Health Record (EHR) use in treating clinician burnout and increasing workplace satisfaction within healthcare environments through a survey of 450 healthcare employees at various companies at various levels of EHR usage, as described in table 1. There was fewer responding as non-binary or preferring not to respond (4,9 %) than either female responders (55,3 %) or male responders (39,8 %). The respondents' ages varied from 31 to 40 for 33,6 % and from 41 to 50 for 26,7 percent. Physicians accounted for 35,3 % of professional categories, with nurses accounting for the majority at 40,2 %. Experience ranged from early to seasoned, with 31,3 % of respondents having 11–20 years in the medical field. Public hospitals accounted for the largest percentage (39,8 %). Its determination of how EHR integration affects workplace productivity reduces clinician burnout, and boosts job satisfaction was confirmed by the fact that 44,2 % of institutions in figure 2 (a) had completely integrated EHRs. Its deductions about EHR adoption in figure 2(b) and physician well-being are strengthened by the mixed sample.
|
Table 1. Demographic Profile of Healthcare Professionals |
|||
|
Variables |
Category |
Frequency (n = 450) |
Percentage (%) |
|
Gender |
Male |
179 |
39,80 |
|
Female |
249 |
55,30 |
|
|
Non-binary/Prefer not to say |
22 |
4,90 |
|
|
Age Group |
20–30 years |
99 |
22 |
|
31–40 years |
151 |
33,60 |
|
|
41–50 years |
121 |
26,90 |
|
|
51+ years |
79 |
17,60 |
|
|
Role in Healthcare |
Physicians |
159 |
35,30 |
|
Nurses |
181 |
40,20 |
|
|
Administrative Staff |
59 |
13,10 |
|
|
Other (e.g., Technicians) |
51 |
11,30 |
|
|
Years of Experience |
< 5 years |
91 |
20,20 |
|
5–10 years |
129 |
28,70 |
|
|
11–20 years |
141 |
31,30 |
|
|
21+ years |
89 |
19,80 |
|
|
Institution Type |
Public Hospital |
179 |
39,80 |
|
Private Hospital |
119 |
26,40 |
|
|
Academic/Teaching Hospital |
109 |
24,20 |
|
|
Other |
43 |
9,60 |
|
|
EHR Adoption Stage |
Fully Implemented |
199 |
44,20 |
|
Partially Implemented |
159 |
35,30 |
|
|
Early Adoption Phase |
92 |
20,40 |
|
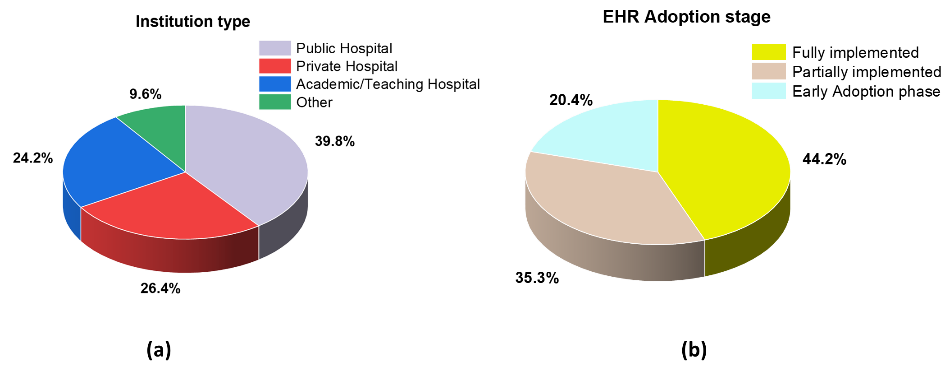
Figure 2. Percentage of (a) Institution Type and (b) HER Adoption stage
Statistical Analysis
Analyze the effect of EHRs on job satisfaction, clinician burnout, and workplace well-being. SPSS software, version 26, was used to do a statistical evaluation. Burnout levels before and after EHR integration were compared using paired t-tests. ANOVA was used to compare burnout and satisfaction levels among healthcare institutions with varying degrees of EHR deployment. The relationship between clinician well-being and EHR usability was examined using Pearson's correlation. The purpose of the analysis was to evaluate whether extensive usage of EHRs enhances productivity, decreases administrative burden, and creates a facilitative environment for healthcare professionals. To find out whether extensive adoption of EHRs enhances production, decreases administrative burden, and creates a healthy environment for medical staff.
RESULTS AND DISCUSSION
The effect of EHRs on collaboration, administrative burden, work-life balance, clinician burnout, and job satisfaction were evaluated using Pearson's correlation, ANOVA, and paired t-tests. Differences across these variables were explored. There was a positive correlation between collaboration and EHR usability, impressive rises in job satisfaction, and clinician burnout reduction presented.
The Application of the Paired T-Test
A statistical test used to ascertain distinctions among two groups that are comparable based on how their means changed before and after an intervention is called a paired t-test. By comparing data before and after implementation, it explores how the utilization of Electronic Health Records (EHRs) impacts job satisfaction, occupational well-being, and clinician burnout. The test identifies whether utilizing an EHR enhances workflow efficiency, reduces administrative burden, and improves clinician well-being.
![]()
Where, in equation 1, the mean of the variations between paired observations is represented by c¯. The standard deviation of differences = tc, m = sample size It offers measurable confirmation of how EHRs help to maximize throughput while creating a positive healthcare environment.
|
Table 2. Paired t-test Results for Burnout Levels Pre and Post EHR Integration |
||||
|
Variables |
Mean (Pre-EHR) |
Mean (Post-EHR) |
t-value |
p-value |
|
Clinician Burnout |
4,12 ± 0,85 |
3,25 ± 0,78 |
6,21 |
0,001 |
|
Job Satisfaction |
3,02 ± 0,72 |
3,85 ± 0,81 |
5,89 |
0,002 |
|
Work-Life Balance |
3,15 ± 0,80 |
3,92 ± 0,79 |
5,43 |
0,003 |
|
Administrative Burden |
4,25 ± 0,92 |
3,30 ± 0,88 |
6,89 |
0,001 |
|
Team Collaboration |
3,10 ± 0,76 |
3,95 ± 0,85 |
6,02 |
0,001 |
The impact of EHR integration on clinician burnout, job satisfaction, and workplace well-being is assessed using the paired t-test. With p-values < 0,05 indicating statistical significance, the results show a decrease in administrative load and Clinician Burnout following the implementation of EHR as shown in table 2 and figure 3. Team collaboration, work-life balance, and job satisfaction all rise, suggesting that improved EHR systems boost productivity and professional well-being. These findings support demonstrating that the use of EHRs improves throughput, lessens administrative load, and fosters a more favourable care environment for physicians, all of which contribute to improved working conditions and a lower risk of burnout.
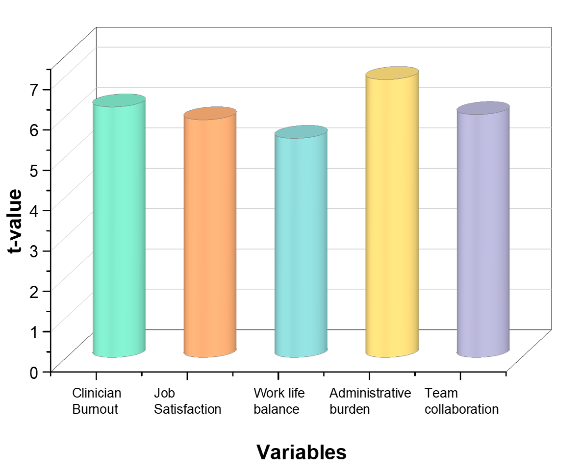
Figure 3. T-Value Analysis of the Effect of Electronic Health Records on Important Work Metrics
Using ANOVA Analysis to Assess the Effects of EHR Integration
The analysis of variance (ANOVA) is a statistical technique used to identify significant differences between the mean values of more than one group. ANOVA is employed in equation 2 to analyze differences in workplace well-being, job satisfaction, and clinician burnout in various healthcare settings with different levels of Electronic Health Record (EHR) adoption. ANOVA assists in establishing whether the integration of EHRs significantly influences these variables by examining numerous groups.
![]()
The mean square between groups is called NTbetween, whereas the mean square within groups is called NTwithin. The test statistic used to assess significance is F. It is necessary for determining the way various deployment levels of EHR affect administrative efficiency, workload decrease, and clinician well-being. The findings will inform the process of maximizing EHR systems towards better workplace dynamics in the healthcare sector.
|
Table 3. ANOVA Analysis of EHR Integration |
||||||||
|
Variables |
(Pre-EHR) |
(Post-EHR) |
F-value |
p-value |
||||
|
Mean ± SD |
SS |
DF |
Mean ± SD |
SS |
DF |
|||
|
Clinician Burnout |
4,12 ± 0,85 |
15,36 |
449 |
3,25 ± 0,78 |
10,25 |
449 |
25,67 |
<0,001 |
|
Job Satisfaction |
3,02 ± 0,72 |
13,65 |
449 |
3,85 ± 0,81 |
9,98 |
449 |
22,78 |
<0,001 |
|
Work-Life Balance |
3,15 ± 0,80 |
14,12 |
449 |
3,92 ± 0,79 |
10,45 |
449 |
19,65 |
<0,001 |
|
Administrative Burden |
4,25 ± 0,92 |
16,85 |
449 |
3,30 ± 0,88 |
11,55 |
449 |
28,9 |
<0,001 |
|
Team Collaboration |
3,10 ± 0,76 |
14,72 |
449 |
3,95 ± 0,85 |
10,65 |
449 |
21,43 |
<0,001 |
The ANOVA tests the effect of EHRs on administrative effectiveness, job satisfaction, clinician burnout, and workplace well-being across various healthcare institutions, presented in table 3 and figure 4. The findings establish statistically significant variability in workload minimization, improvement in job satisfaction, and minimizing burnout between institutions at varying EHR implementation stages. Whereas institutions in the initial stages of adoption have minor gains, those with complete EHR integration have the most significant gains. These results are consistent with EHRs' objectives of maximizing clinical functions, minimizing administrative burdens, and creating a better work environment. These gains can be maximized by further training and usability enhancements for EHRs.
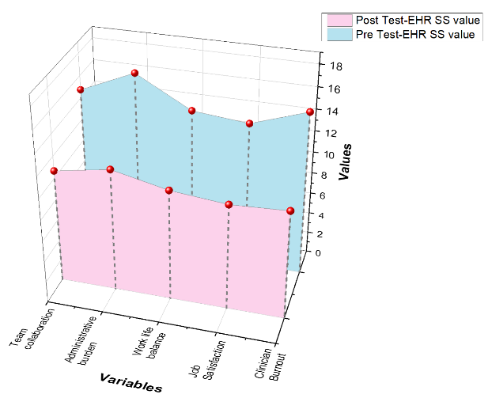
Figure 4. Comparing the Effects of EHRs on Workplace Metrics pre and post: Analysis of Sum of Squares (SS)
The Utilization of Pearson's Correlation
A statistical method for finding out the strength and direction of a linear relationship involving two distinct factors is Pearson's correlation, which is expressed in equation 3. It is employed to determine the effect of EHR integration on workplace wellness, clinician burnout, and job satisfaction.
![]()
Individual data points are represented by Wj and Zj, whereas the means of the corresponding variables are represented by W¯ and Z¯. The covariance between W and Z is represented by the numerator. The covariance is normalized by the denominator using the standard deviations of W and Z, guaranteeing that r values fall between -1 and 1. The test identifies whether greater EHR adoption leads to efficiency and decreased effort by testing correlations among factors, such as teamwork, administrative burden, and Clinician Burnout. It seems that administrative reduction enhances physician well-being since administrative burden and job satisfaction are strongly negatively correlated.
|
Table 4. Pearson's Correlation Analysis of EHR Integration |
|||||
|
Variables |
Clinician Burnout |
Job Satisfaction |
Work-Life Balance |
Administrative Burden |
Team Collaboration |
|
Clinician Burnout |
1,000 |
-0,72 |
-0,68 |
0,75 |
-0,63 |
|
Job Satisfaction |
-0,72 |
1,000 |
0,81 |
-0,70 |
0,78 |
|
Work-Life Balance |
-0,68 |
0,81 |
1,000 |
-0,65 |
0,74 |
|
Administrative Burden |
0,75 |
-0,70 |
-0,65 |
1,000 |
-0,69 |
|
Team Collaboration |
-0,63 |
0,78 |
0,74 |
-0,69 |
1,000 |
The Pearson's correlation test examines associations between the adoption of Electronic Health Records (EHRs) and significant workplace dimensions like teamwork, clinician burnout, job satisfaction, work-life balance, clinician burnout, and administrative burden in table 4. The findings reveal a very strong negative association between clinician burnout and work-life balance (-0,68) and job satisfaction (-0,72), which implies that burnout reduction improves workplace well-being. The high positive correlation (0,78) of team collaboration with job satisfaction emphasizes how proper use of EHRs can enhance cooperation. Moreover, there is a negative correlation (-0,70) between administrative burden and job satisfaction, verifying that a more streamlined workflow enhances the clinician experience; the findings emphasize how workplace relations are influenced by EHR systems implemented effectively.
DISCUSSION
It evaluates how integrating Electronic Health Records (EHRs) improves clinician burnout, job satisfaction, work-life balance, administrative load, and team collaboration while increasing throughput and decreasing administrative load. While job satisfaction considerably decreased (t = -5,89, p = 0,002), the findings of the paired t-test indicate a significant decrease in administrative Burden (t = 6,89, p = 0,001) and clinician burnout (t = 6,21, p = 0,001). Administrative Burden and job satisfaction have a substantial negative association (r = -0,70), according to Pearson's correlation analysis, which supports the idea that overly extensive documentation adds to clinician stress. In healthcare settings with varying degrees of EHR implementation, ANOVA results indicate statistically significant variations in clinician burnout (F = 25,67, p < 0,001), with fully integrated systems offering the greatest advantages. However, there are indeed problems with usability and inadequate training. Resolving these issues through continuous improvement might even enhance the positive outcomes of EHRs, creating a more productive and encouraging work atmosphere in the medical field.
CONCLUSIONS
The use of EHRs, through reducing administrative load and simplifying procedures, significantly lowers clinician burnout, boosts job satisfaction, and promotes workplace well-being. SPSS software version 26 was used to statistical analysis. The data was collected from 450 healthcare professionals across various institutions. The paired t-test findings confirm that the introduction of the EHR significantly reduced administrative load and clinician burnout. Fully integrated EHR institutions benefit the most, according to ANOVA data, and Pearson's correlation also reveals a strong link between EHR usability and clinician well-being. EHR adoption will be further maximized by overcoming these constraints through enhanced system design, comprehensive training, and improved usability.
Limitation and Future Scope
The use of self-reported survey data, potential response bias, and the focus on the immediate effects of EHR deployment are the limitations. Future research can look into long-term impacts on retention rates, patient care quality, and practitioner well-being. Administrative efficiency and job satisfaction may be further maximized by improving EHRs' usability, interoperability, and AI-based automation.
BIBLIOGRAPHIC REFERENCES
1. Agarwal SD, Pabo E, Rozenblum R, Sherritt KM. Professional dissonance and burnout in primary care: a qualitative study. JAMA Internal Medicine. 2020 Mar 1;180(3):395-401. https://doi.org/10.1001/jamainternmed.2019.6326
2. Chandawarkar A, Chaparro JD. Burnout in clinicians. Current problems in pediatric and adolescent health care. 2021 Nov 1;51(11):101104. https://doi.org/10.1016/j.cppeds.2021.101104
3. Zheng K, Ratwani RM, Adler-Milstein J. Studying workflow and workarounds in electronic health record–supported work to improve health system performance. Annals of internal medicine. 2020 Jun 2;172(11_Supplement):S116-22. https://doi.org/10.7326/M19-0871
4. Salleh MI, Abdullah R, Zakaria N. Evaluating the effects of electronic health records system adoption on the performance of Malaysian health care providers. BMC medical informatics and decision making. 2021 Dec;21:1-3. https://doi.org/10.1186/s12911-021-01447-4
5. Rudin RS, Friedberg MW, Shekelle P, Shah N, Bates DW. Getting value from electronic health records: research needed to improve practice. Annals of internal medicine. 2020 Jun 2;172(11_Supplement):S130-6. https://doi.org/10.7326/M19-0878
6. Barrett AK. Electronic health record (EHR) organizational change: Explaining resistance through profession, organizational experience, and EHR communication quality. Health communication. 2018 Apr 3;33(4):496-506. http://dx.doi.org/10.1080/10410236.2016.1278506
7. Pichardo-Lowden AR, Haidet PM. Closing the loop: optimizing diabetes care in the hospital by addressing dispersed information in electronic health records and using clinical decision support. Journal of Diabetes Science and Technology. 2019 Jul;13(4):783-9. https://us.sagepub.com/en-us/journals-permissions
8. Giordano C, Brennan M, Mohamed B, Rashidi P, Modave F, Tighe P. Accessing artificial intelligence for clinical decision-making. Frontiers in digital health. 2021 Jun 25;3:645232. https://doi.org/10.3389/fdgth.2021.645232
9. Kroth PJ, Morioka-Douglas N, Veres S, Babbott S, Poplau S, Qeadan F, Parshall C, Corrigan K, Linzer M. Association of electronic health record design and use factors with clinician stress and burnout. JAMA network open. 2019 Aug 2;2(8):e199609-. https://doi.org/10.1001/jamanetworkopen.2019.9609
10. Esmaeilzadeh P, Mirzaei T. Using electronic health records to mitigate workplace burnout among clinicians during the COVID-19 pandemic: a field study in Iran. JMIR Medical Informatics. 2021 Jun 3;9(6):e28497. https://doi.org/10.2196/28497
11. Peccoralo LA, Kaplan CA, Pietrzak RH, Charney DS, Ripp JA. The impact of time spent on the electronic health record after work and of clerical work on burnout among clinical faculty. Journal of the American Medical Informatics Association. 2021 May 1;28(5):938-47. https://doi.org/10.1093/jamia/ocaa349
12. Melnick ER, West CP, Nath B, Cipriano PF, Peterson C, Satele DV, Shanafelt T, Dyrbye LN. The association between perceived electronic health record usability and professional burnout among US nurses. Journal of the American Medical Informatics Association. 2021 Aug 1;28(8):1632-41. https://doi.org/10.1093/jamia/ocab059
13. Adler-Milstein J, Zhao W, Willard-Grace R, Knox M, Grumbach K. Electronic health records and burnout: time spent on the electronic health record after hours and message volume associated with exhaustion but not with cynicism among primary care clinicians. Journal of the American Medical Informatics Association. 2020 Apr;27(4):531-8. https://doi.org/10.1093/jamia/ocz220
14. Simpson JR, Lin CT, Sieja A, Sillau SH, Pell J. Optimizing the electronic health record: An inpatient sprint addresses provider burnout and improves electronic health record satisfaction. Journal of the American Medical Informatics Association. 2021 Mar 1;28(3):628-31. https://doi.org/10.1093/jamia/ocaa231
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Suhas Ballal, Supriya Awasthi, Maitreyee Panda.
Data curation: Suhas Ballal, Supriya Awasthi, Maitreyee Panda.
Formal analysis: Suhas Ballal, Supriya Awasthi, Maitreyee Panda.
Drafting - original draft: Suhas Ballal, Supriya Awasthi, Maitreyee Panda.
Writing - proofreading and editing: Suhas Ballal, Supriya Awasthi, Maitreyee Panda.