doi: 10.56294/mw2023147
ORIGINAL
Investigating factors affecting prosthetic use and adjustment in lower limb amputee rehabilitation
Investigación de los factores que afectan al uso y ajuste de prótesis en la rehabilitación de amputados de miembros inferiors
Samir Ranjan Jena1 ![]() *, Renuka Jyothi S2
*, Renuka Jyothi S2 ![]() , Ranjana Singh3
, Ranjana Singh3 ![]()
1IMS and SUM Hospital, Siksha ‘O’ Anusandhan (deemed to be University), Department of General Medicine. Bhubaneswar, Odisha, India.
2JAIN (Deemed-to-be University), Department of Biotechnology and Genetics. Bangalore, Karnataka, India.
3Noida International University, Department of Community Medicine. Greater Noida, Uttar Pradesh, India.
Cite as: Jena SR, Renuka JS, Singh R. Investigating Factors Affecting Prosthetic Use and Adjustment in Lower Limb Amputee Rehabilitation. Seminars in Medical Writing and Education. 2023; 2:147. https://doi.org/10.56294/mw2023147
Submitted: 18-09-2022 Revised: 30-12-2022 Accepted: 03-03-2023 Published: 04-03-2023
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Samir Ranjan Jena *
ABSTRACT
Successful rehabilitation following lower limb amputation relies on effective prosthetic use and adjustment, influenced by various physical, psychological, and environmental factors. Understanding these factors is essential for optimizing rehabilitation strategies and improving amputees’ quality of life. Research investigates the key factors affecting prosthetic use and adjustment in lower limb amputee rehabilitation, focusing on prosthetic functionality, user characteristics, psychosocial adaptation, and rehabilitation-related influences. A total of 298 adult’s lower limb amputees participated in structured interviews. Patient demographics, amputation-related information, prosthetic use, and the Prosthetic Limb Users Survey of Mobility (PLUS-M) were all evaluated using standardized questionnaires to gather data. Key factors analyzed included physical and health, psychological, activity, functional and lifestyle, personal and social, and environmental factors. Statistical analysis methods, including descriptive statistics, correlation and regression analysis, were conducted to determine significant associations between prosthetic use and adjustment outcomes. Findings show that prosthetic satisfaction was usually positive, and participants reported functional mobility and moderate psychological adjustment. The use of prosthetics, socket fit, residual limb health, and daily prosthesis wear time were important factors affecting prosthetic use. Employment position, psychological resilience, social reintegration, and access to rehabilitation were all substantially correlated with adjustment results. Research emphasizes that to optimize prosthesis use and long-term adjustment, rehabilitation must incorporate medical, psychological, and social support measures.
Keywords: Prosthetic Use; Lower Limb Amputation; Rehabilitation; Adjustment; Functional Mobility.
RESUMEN
El éxito de la rehabilitación tras una amputación de miembro inferior depende del uso y la adaptación eficaces de la prótesis, en los que influyen diversos factores físicos, psicológicos y ambientales. Comprender estos factores es esencial para optimizar las estrategias de rehabilitación y mejorar la calidad de vida de los amputados. La investigación estudia los factores clave que afectan al uso de prótesis y a la adaptación en la rehabilitación de amputados de miembros inferiores, centrándose en la funcionalidad protésica, las características del usuario, la adaptación psicosocial y las influencias relacionadas con la rehabilitación. Un total de 298 adultos amputados de miembros inferiores participaron en entrevistas estructuradas. Los datos demográficos de los pacientes, la información relacionada con la amputación, el uso de prótesis y la Encuesta de Movilidad de Usuarios de Prótesis (PLUS-M) fueron evaluados utilizando cuestionarios estandarizados para recopilar datos. Los factores clave analizados incluyeron factores físicos y de salud, psicológicos, de actividad, funcionales y de estilo de vida, personales y sociales, y ambientales. Se llevaron a cabo métodos de análisis estadístico, incluyendo estadística descriptiva, correlación y análisis de regresión, para determinar asociaciones significativas entre el uso de prótesis y los resultados de la adaptación. Los resultados muestran que la satisfacción con la prótesis fue generalmente positiva, y los participantes informaron de movilidad funcional y ajuste psicológico moderado. El uso de prótesis, el ajuste del encaje, la salud del muñón y el tiempo diario de uso de la prótesis fueron factores importantes que afectaron al uso protésico. La posición laboral, la resiliencia psicológica, la reintegración social y el acceso a la rehabilitación se correlacionaron sustancialmente con los resultados del ajuste. La investigación subraya que, para optimizar el uso de prótesis y la adaptación a largo plazo, la rehabilitación debe incorporar medidas de apoyo médico, psicológico y social.
Palabras clave: Uso de Prótesis; Amputación de Miembro Inferior; Rehabilitación; Ajuste; Movilidad Funcional.
INTRODUCTION
Amputation is the abrupt limb loss, causing drastic changes in the individual's life. A person suffers from loss of the lower limb due to trauma, disease, or congenital reasons, which immediately affects the person physically, emotionally, and socially. Notably, lower limbs can impair proper mobility, independence, and standard living conditions, therefore requiring an effective rehabilitation strategy given recovery. A decrease in participation could also delay the attainment of functional mobility. Hence, to further elucidate the post-rehabilitation phase, it is important to consider the interaction of body-image perception with mobility.(1) Rehabilitation is multidisciplinary physical activity, psychosocial support, implementation, and utilization of prosthetics that help individuals regain mobility and independence. After amputation, psychological-social health problems could arise and affect life quality. When amputees and extremity injuries were compared, those who lost a limb were more likely to have mental health diagnoses, such as post-concussion syndrome, pain disorders, and non-organic sleep problems.(2)
Rehabilitation of lower limb amputation (LLA) is largely dependent upon prosthetics. Modern prosthetic limbs are to function instead of what has been lost, allowing the amputee to walk, run, or carry on with normal activities. Many issues come into play in the success of a prosthetic limb, however, ranging from design and fit of the prosthesis-influencing psychological and emotional adjustment to the device on a personal level.(3) A major LLA is a painful life transition that puts the patient at risk for a significant decline in postoperative autonomy, involvement, efficiency, and life function. The majority of LLAs in adults are caused by diabetes, while other causes include trauma, cancer, infection, anatomical conditions, or birth abnormalities. The fitting and functioning of the prosthesis play an important role, but several physical factors, psychosocial factors, environmental factors, and other factors also influence the selection of the prosthesis. Physical factors refer to the fit, functioning, and comfort of the prosthesis. Psychosocial factors include the mental state of the user, that is, emotional resilience or stress. Environmental factors include access to rehabilitation and support in their physical environment.(4)
Geographical and loading variables cause LLA to walk asymmetrically due to the prolonged time spent and the strains exerted on the entire limb. Step or stance time is typically used to calculate spatiotemporal irregularity, and takes into account the vertical ground response force's (GRF) initial peak. Prosthetic adjustment is often complicated by psychological dilemmas. Therefore, for assisting emotional and mental well-being, strongly positive factors can enhance successful outcomes concerning the use of the prosthetic limb.(5) The smaller cognitive illustration of the lower limbs and surrounding areas across the sensory homunculus, it is likely more difficult to pinpoint particular areas of interest, including amputees with lower limbs. It has been identified that influencing factors related to prosthetic use and adjustment are vital in effecting changes during rehabilitation among lower limb amputees. In such an approach, rehabilitation programs could be designed to give individuals a better chance at realizing the best possible outcomes and leading full lives after amputation.(6) Research aims to identify and analyze the most important factors influencing the use or adjustment of prosthetic in lower limb amputees. Evaluation of the functional aspects of prosthetic, profile of the users, psychosocial adjustment, and other rehabilitation-related factors could help in optimizing rehabilitation approaches for improved quality of life for amputees.
Food intakes and prevalence of obesity was examined among adult lower limb amputees, concentrating on eating patterns, levels of physical activity, and variables that lead to weight growth or make it difficult to control weight after transplantation.(7) Cross-sectional research that compared consumption trends to nutritional requirements using food frequency questionnaires. Consumption of foods associated with cardiovascular risk exceeded dietary reference values by a substantial margin. Overweight and obesity were significantly more common, as evidenced by higher average body mass index (BMI) and waist-to-hip ratios. The cross-sectional nature makes it difficult to prove causation and self-identified dietary information. The function of obstacle avoidance and tolerance on phantom sensations and the embodiment of prosthetics in lower limb amputees are investigated.(8) Research involved 12 amputees, who received stimulation of the phantom limb observed obstacle avoidance and tolerance. Phantom limb sensations disappeared with obstacle avoidance in the presence of an object, while tolerance permitted stronger constraints to apparent movement. A limited sample size and only two behaviors compromise the generalizability of the research. The aim is to assess lower limb muscle properties for high-resolution magnetic resonance imaging (MRI) in individuals who had transtibial and transfemoral leg amputations.(9) Patients with transtibial and transfemoral amputations enrolled in the research were subjected to whole-limb muscle volume assessment using MRI of the amputated and intact limbs. An important reduction in muscle volume was seen concerning the residual limb, with minor reductions found in the intact. While both transfemoral amputees exhibited increases in gluteus Medius, hip flexors, and short adductors, decreases were found in longer adductors. The data evaluated from twelve subjects, however, permit generalization beyond this sample. Amputees and rehabilitation specialists have explored the influence of socket fit on rehabilitation for lower limb prostheses.(10) Phone interviews were conducted with amputees and rehabilitation specialists to learn about the perceptions regarding the importance of socket fit during rehabilitation. Research found the socket fit was viewed as the greatest influence on the rehabilitation process. Clinicians were preoccupied with making adjustments to the socket and gait rehabilitation; amputees, on the contrary, were concerned with socket fit in terms of lifestyle and daily living. Since interviews were complete over the phone, there was no opportunity for in-depth examination of the replies for the use of suitable indirect signals.
The effects of post-traumatic lower limb amputation on mental health were investigated.(11) Interviews were conducted with twelve participants, whose experiences and emotions after the amputation were analyzed. Thematic analysis was utilized to identify major themes. Five themes have emerged; a sociocultural divide, negative future perspectives, modified feelings and behavior, poor body image and self-esteem, and the need for psychosocial support for survival. The small sample size (12 participants) limited the generalizability of findings, and being self-reported introduces a bias within the research. The efficiency of a substitute tactile stimulation system on standing stability among those with lower limb amputations was evaluated.(12) Participants with and without amputation The Person tested a wearable device consisting of two vibrators and four pressure sensors to measure body wobble and posture resilience under vision disturbances. Body wobble and posture resilience improved during system familiarization, with the effects more prominent under conditions with severe visual impairment. A brief familiarization during the experiment does not seem to reflect system adaptation during long-term application, and sample size and other aspects of impairment are not specified.
The efficacy of closed-loop perceptual neuroproteins in securing and maintaining stability in symmetrical LLA is evaluated when sensory inputs are considered.(13) The neuroproteins used non-penetrating electrodes for stimulation of the brain, while at the same time, somatosensory inputs from the uninjured leg and visual inputs were disrupted. The intervention significantly improved balance and reduced influence in LLAs, indicating that brain stimulation compensates for the loss of sensory information to enhance stability. The long-term effects of brain stimulation, and applicability in dynamic real-life scenarios were not tested. Research aims to explores the main factors that impact prosthetic use and adjustment in lower limb amputee rehabilitation as shown in figure 1, with a focus on prosthetic functionality, user characteristics, psychosocial adaptation, and rehabilitation-related factors.
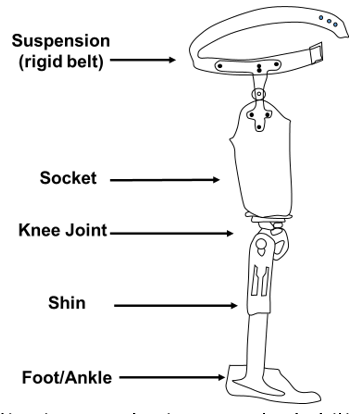
Figure 1. Factor influencing rehabilitation prosthetic use and rehabilitation adjustment in lower limb
METHOD
The cross-sectional research design encompasses the use of structured interviews with 298 lower-limb amputees as the research instrument for obtaining data on prosthesis use and adjustment. Various key variables, including physical and health, psychological, activity, functional and lifestyle, personal and social, as well as environmental factors, were assessed through standardized questionnaires based on PLUS-M. The statistical analysis, including regression, correlation and descriptive significant predictors such as socket fit, were time and psychological resilience for prosthetic outcomes.
Data collection
Data were collected using structured interviews with 298 adults with lower limb amputation. Research provided demographic and amputation-related information and completed standardized questionnaires. This information facilitates the evaluation of influences on prosthetic use and adjustment, considering physical, psychological, and environmental aspects. Table 1 shows the amputation level of participants.
|
Table 1. Demographic details for the patients |
|||
|
Demographic Variable |
Categories |
Frequency (n) |
Percentage (%) |
|
Age |
18-21 years |
45 |
15,1 |
|
22-24 years |
51 |
17,1 |
|
|
25-27 years |
60 |
20,1 |
|
|
28-35 years |
65 |
21,8 |
|
|
36-38 years |
50 |
16,8 |
|
|
40+ years |
27 |
9,1 |
|
|
Gender |
Male |
187 |
62,8 |
|
Female |
111 |
37,2 |
|
|
Amputation Level |
Above knee (AK) |
120 |
40,3 |
|
Below knee (BK) |
160 |
53,7 |
|
|
Bilateral |
18 |
6,0 |
|
|
Cause of Amputation |
Trauma |
90 |
30,2 |
|
Vascular disease |
85 |
28,5 |
|
|
Diabetes-related |
65 |
21,8 |
|
|
Cancer |
25 |
8,4 |
|
|
Other |
33 |
11,1 |
|
|
Time Since Amputation |
Less than 1 year |
50 |
16,8 |
|
1-5 years |
95 |
31,9 |
|
|
6-10 years |
75 |
25,2 |
|
|
11-15 years |
45 |
15,1 |
|
|
15+ years |
33 |
11,1 |
|
|
Employment Status |
Employed |
143 |
47,9 |
|
Unemployed |
95 |
31,9 |
|
|
Retired |
60 |
20,1 |
|
|
Prosthetic Use |
Daily |
210 |
70,5 |
|
Occasionally |
65 |
21,8 |
|
|
Never |
23 |
7,7 |
|
|
Prosthetic Type |
Prosthetic leg |
230 |
77,2 |
|
Prosthetic foot |
45 |
15,1 |
|
|
Other |
23 |
7,7 |
|
Questionnaires
Assessment of the questionnaires used in this research adapted from the PLUS-M is constructs supposed to affect prosthetic use and adjustment of lower-limb amputees. Participants are requested to answer questions about the physical health, psychological coping, and participation in activities, functional performance, social support, and approaches toward the environment. The results provide insights into identifying construct inhibiting and facilitating prosthetic use, thus giving direction into how such findings could contribute to the enhancement of rehabilitation strategies. Table 2 shows the questionnaires for the patients.
|
Table 2. Questions evaluating the factors influencing prosthetic use and adjustment |
|
|
Variable |
Question |
|
Physical and Health Factors |
1. To what extent does your prosthesis affect your daily mobility? |
|
2. What level of discomfort do you experience when using your prosthesis? |
|
|
Psychological Factors |
3. In your opinion, how well do you cope with challenges related to using your prosthesis? |
|
4. What is your overall sense of independence while using your prosthesis? |
|
|
Activity Factors |
5. How satisfied are you with your ability to engage in activities using your prosthesis? |
|
6. What is the most challenging activity you struggle with when using your prosthesis? |
|
|
Functional and Lifestyle Factors |
7. How well does your prosthesis allow you to carry out essential daily tasks (e.g., walking, standing)? |
|
8. To what extent does your prosthesis meet your expectations for mobility and comfort? |
|
|
Personal and Social Factors |
9. How often do you feel supported by family and friends in using your prosthesis? |
|
10. In your view, how accepted do you feel in social settings when using your prosthesis? |
|
|
Environmental Factors |
11. How accessible do you find public spaces (e.g., transportation, buildings) while using your prosthesis? |
|
12. How would you rate the ease of movement on different types of terrain with your prosthesis? |
|
The questionnaires based on the ratings range from 1 to 5; there are strongly disagree, disagree, neutral, agree, and strongly agree. A 5-point scale in the questionnaires, which inquire about mobility, discomfort, independence, activity satisfaction, social acceptance, and environmental accessibility based on the user's experience and satisfaction.
Factors
The factors are analyzed to identify key predictors of rehabilitation and long-term prosthetic adaption. The factors and definitions are follows:
Physical and health: The degree of fit of the prosthesis, health of the residual limb, average daily use of the prosthesis, general state of health, etc.; these physical and health factors affect comfort, mobility, and success in adapting to the prosthesis.
Psychological: Factors considered in the research include psychological resilience, which refers to the capacity to deal with stress and adversities, and depression level, which serves as a depressive symptom measure. Both psychological factors affect an amputee's emotional adaptation toward the use of a prosthetic and overall rehabilitation outcomes.
Activity: The term defines a dimension that covers the amount of daily prosthesis wear and physical activity. For instance, it comprises Daily Prosthesis Wear Time - a measurement unit that shows how many hours the device is in the body daily- and also Physical Activity Levels that define an individual activity such as frequency and intensity level of different physical exercises or kinds of movements done.
Functional and lifestyle: The aspects covering daily living and one's context by which the use and adaptation to prostheses have been influenced. The employment status and mobility levels, define the individual's efficiency in performing work and physical activities.
Personal and social: The individual's psychological well-being factor and social ties, which include social support (the facility of family, friends, and community to be available in emotional or practical assistance) and social reintegration (the act of re-establishing society roles and relationships post-amputation).
Environmental factor: Pre-registration for rehabilitation services and environmental quality are two examples of environmental factors that could affect how prostheses are used and the changes that are made. It included factors such as accessibility, safety, and support networks that either facilitate or hinder rehabilitation.
Statistical analysis
Statistical analysis performed to assess the linkages of important variables; physical health, psychological resilience, levels of activity, functional lifestyle factors, social support, and environmental factors with prosthetic use and adjustment in lower-limb amputees. Descriptive statistics and regression analyses were performed to identify highly significant predictors. Important parameters in terms of socket fitting, daily wear time, and psychological resilience, contributing towards the enhancement of rehabilitation strategies.
RESULTS
The section discusses the outcome of statistical analysis performed on various factors influencing dementia progression.
Descriptive Statistics
To analyze the impact of significant determinants upon prosthesis usage and adjustment provisions about lower limb amputees during rehabilitation, descriptive statistics were used. These determinants include physical health, psychological resilience, activity levels, functional and lifestyle factors, personal and social aspects, and environmental conditions. Factors with computed means, standard deviations (SD), minimum, and maximum represented various experiences of participants with prosthetics. Insights would therefore be drawn from the findings into variability and general trends across different dimensions of rehabilitation shown in equation (1).
![]()
T is determined using the equation for the standard deviation, which evaluators how much prosthetic use and adjustment scores w deviate from the average score w ̅. It could be a consequential measure that reflects an acceptable of factors, such as socket fit, activity or participation levels, and psychological resilience of lower limb amputees in their rehabilitation outcomes are shown in table 3.
|
Table 3. Descriptive statistics for factors influencing prosthetic use in lower limb amputees |
|||||
|
Factors |
Mean |
Standard Deviation |
Minimum |
Maximum |
|
|
Physical and Health |
Socket Fit |
4,5 |
0,8 |
1 |
5 |
|
Residual Limb Health |
3,8 |
1,1 |
1 |
5 |
|
|
Psychological |
Psychological Resilience |
3,9 |
1,0 |
1 |
5 |
|
Depression Level |
3,7 |
1,2 |
1 |
5 |
|
|
Activity |
Daily Prosthesis Wear Time |
8,2 |
2,5 |
0 |
16 |
|
Physical Activity Level |
2,8 |
1,3 |
1 |
5 |
|
|
Functional and Lifestyle |
Employment Status |
4,2 |
1,0 |
1 |
5 |
|
Mobility Level |
3,5 |
1,4 |
1 |
5 |
|
|
Personal and Social |
Social Support |
3,6 |
1,1 |
1 |
5 |
|
Social Reintegration |
4,1 |
0,9 |
1 |
5 |
|
|
Environmental factors |
Access to Rehabilitation |
4,3 |
0,7 |
2 |
5 |
|
Living Environment Quality |
4,0 |
1,0 |
1 |
5 |
|
The table contains descriptive statistics for the important factors affecting prosthesis use and adjustment. The mean values provide an impression of general trends in areas where satisfaction with the socket fit is very high (4,5) and access to rehabilitation is good (4,3), while residual limb health and depression levels were improved. Standard deviations speak to the variability of response; in this case, some factors, like daily prosthesis wear time (8,2), are more widely distributed. Maximum and minimum numbers highlight the whole variety of participant experiences for each factor shown in figure 2.
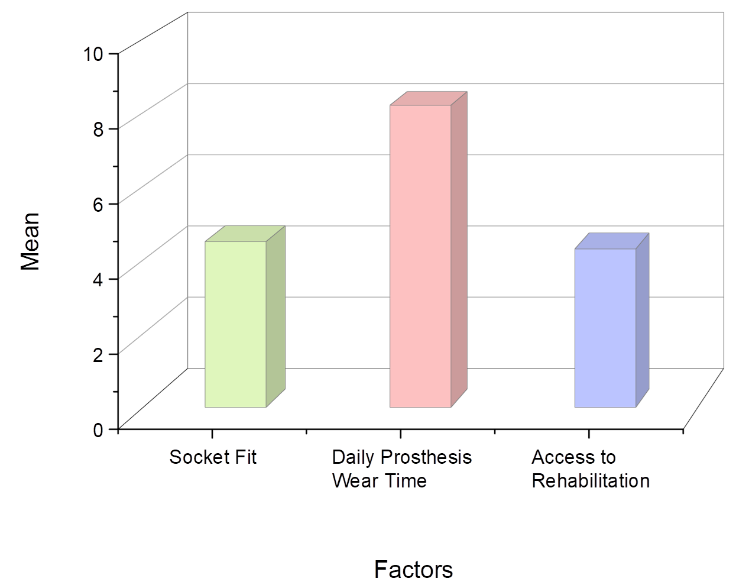
Figure 2. Comparison of key factors influencing prosthetic use and adjustment, highlighting the impact of daily wear time on prosthetic outcomes
Regression analysis
It is employed to explore the relationships between several dependent variables (socket fit, psychological resilience, and daily wear time of prosthesis) and the dependent variables of interest, such as prosthetic use and adjustment in lower limb amputees. By identifying the major predictors, regression also assesses how physical, psychological, and environmental variables affect outcomes, thus providing valuable information for the improvement of the design of prostheses and the management of rehabilitation strategies.
![]()
In the equation, Y stands for the outcome of adjustment and uses a prosthesis while for value x; it stands for factors such as socket fit or psychological resilience. The term m signifies how great the consideration weighs according to the impact of these factors, while b is the model intercession expected to correspond to the baseline levels of prosthetic uses to help predict rehabilitation outcomes shown in table 4.
|
Table 4. The outcome of regression analysis factor |
||||||
|
Factor |
β |
SE |
t-value |
p-value |
R² |
|
|
Physical and Health |
Socket Fit |
0,34 |
0,05 |
6,80 |
0,001 |
0,21 |
|
Residual Limb Health |
0,31 |
0,06 |
5,17 |
0,002 |
||
|
Psychological |
Psychological Resilience |
0,28 |
0,07 |
4,00 |
0,003 |
0,18 |
|
Depression Level |
0,25 |
0,06 |
4,17 |
0,004 |
||
|
Activity |
Daily Prosthesis Wear Time |
0,41 |
0,05 |
8,20 |
<0,001 |
0,30 |
|
Physical Activity Level |
0,32 |
0,06 |
5,33 |
0,005 |
||
|
Functional and Lifestyle |
Employment Status |
0,36 |
0,05 |
7,20 |
<0,001 |
0,25 |
|
Mobility Level |
0,33 |
0,06 |
5,50 |
0,001 |
||
|
Personal and Social |
Social Support |
0,29 |
0,07 |
4,14 |
0,002 |
0,16 |
|
Social Reintegration |
0,27 |
0,07 |
3,86 |
0,003 |
||
|
Environmental factors |
Access to Rehabilitation |
0,33 |
0,06 |
5,50 |
0,001 |
0,22 |
|
Living Environment Quality |
0,30 |
0,07 |
4,29 |
0,004 |
||
The table shows the regression analysis of factors that influence prosthetic use and adjustment. The Beta (Standardized) values represent the strength of influence, where higher numbers show higher associations. At a strong association, for example, Daily Prosthesis Wear Time (0,41) is the strongest factor for prosthetic use, followed by Socket Fit (0,34). The p-values indicated the level of statistical significance, where below 0,05 shows a meaningful relationship. The R² values indicate the percentage of variance explained by the individual factor, much like that for Daily Prosthesis Wear Time (0,30), thereby showing its pivotal role in predicting the various rehabilitation outcomes.
Correlation analysis
The analysis considers the different variables; such as physical condition, psychological resilience, activity level, functionality and lifestyle factors, personal and social aspects, and environmental conditions that correlate to the effects of using and adjusting a prosthesis during lower limb amputation rehabilitation. It defines the relationship between the determinants and the rehabilitation results to improve prosthetic design and rehabilitation approaches, as shown in equation (3).
![]()
It measures the strength and direction of the linear relationship between two measures: prosthetic use wj and psychological resilience z ̅. It computes the linear correlation coefficient between r these measures. Such a coefficient helps assess whether prosthetic use correlates with psychological factors or adjusting in lower limb amputee rehabilitation, as shown in table 5.
|
Table 5. Correlation matrix factor influencing prosthetic use and adjustment |
||||||
|
Variable |
Physical and Health |
Psychological |
Activity |
Functional and Lifestyle |
Personal and Social |
Environmental factors |
|
Physical and Health |
1,00 |
0,45 |
0,38 |
0,52 |
0,47 |
0,55 |
|
Psychological |
0,45 |
1,00 |
0,36 |
0,43 |
0,53 |
0,50 |
|
Activity |
0,38 |
0,36 |
1,00 |
0,56 |
0,51 |
0,59 |
|
Functional and Lifestyle |
0,52 |
0,43 |
0,56 |
1,00 |
0,62 |
0,60 |
|
Personal and Social |
0,47 |
0,53 |
0,51 |
0,62 |
1,00 |
0,63 |
|
Environmental factors |
0,55 |
0,50 |
0,59 |
0,60 |
0,63 |
1,00 |
The correlation matrix (figure 3) illustrates the relationships between several factors influencing prosthesis usage and adjustment in lower limb amputees. All variables recorded moderate to strong positive correlations ranging from a low of 0,36 to a high of 1,00. The highest correlation of 0,63 recorded is between personal and social and environmental factors, demonstrating the social support and environmental conditions affect prosthetic adjustment outcomes.
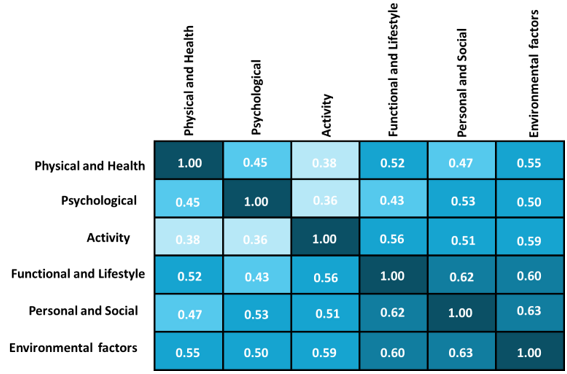
Figure 3. Outcome of correlation matrix
DISCUSSION
Research examines the factors affecting prosthetic use and adjustment in lower limb amputees in rehabilitation. The results suggest that physical, psychological, and environmental factors are significantly involved in prosthetic outcomes. Descriptive statistics were found between satisfaction with prosthetic fit, access to rehabilitation, and successful use, whereas residual limb health and depression demonstrated higher variability. The correlation analysis showed that all factors had moderate to high positive correlations with the highest correlation being between personal and social factors and environmental factors. This indicates a strong impact that all these factors would have on the use and adjustment outcomes of lower limb amputees. Regression analysis identified some of the strongest predictors, including socket fit, psychological resilience, daily prosthesis wear time, and employment status, which appeared to correlate strongly with prosthetic use and adjustment. Daily wear time, in particular, proves to be an important factor affecting rehabilitation success. These findings suggest that physical and psychological factors must be integrated into rehabilitation strategies for optimizing prosthetic use and permanent adjustment for amputees.
CONCLUSIONS
Research focused on assessing the fundamental influences that determine the application and adjustment of the prosthesis among lower-limb amputees during rehabilitation. Structured interviews were conducted on a sample of 298 adult amputees across several important areas of physical, psychological, activity, functional, lifestyle, personal, and environmental factors. The results of the descriptive statistical analysis suggested high satisfaction with socket fit (mean = 4,5) and access to rehabilitation (mean = 4,3), while the average daily prosthesis wear time at 8,2. Regression analysis identified the significant determinants in prosthetic use and adjustments, namely socket fit (β = 0,34), daily prosthesis wear time (β = 0,41), and social reintegration (β = 0,27). The correlation analysis revealed strong positive relationships, while personal and social factors correlated most strongly with environmental factors (r = 0,63). Research recognizes the significance of integrated medical, psychological, and social support for long-term better rehabilitation. However, the research was cross-sectional and based entirely on self-reported information. Future research could be directed to longitudinal studies looking into the long-term influence of these factors and the effect of personalized rehabilitation strategies on prosthetic use and adjustment.
BIBLIOGRAPHIC REFERENCES
1. Desrochers J, Frengopoulos C, Payne MW, Viana R, Hunter SW. Relationship between body image and physical functioning following rehabilitation for lower-limb amputation. International Journal of Rehabilitation Research. 2019 Mar 1;42(1):85-8. https://doi.org/10.1097/MRR.0000000000000329.
2. Amorelli C, Yancosek K, Morris R. Amputees Unanimous: A 12-step program. Prosthetics and Orthotics International. 2019 Jun;43(3):293-300. https://doi.org/10.1177/0309364619836027.
3. Talbot SG, Carty MJ, Jensen SE, Dumanian GA. Adjustment to amputation and interest in upper limb transplantation. SAGE open medicine. 2019 Jun;7:2050312119858248. https://doi.org/10.1177/2050312119858248.
4. Dekker R, Hristova YV, Hijmans JM, Geertzen JH. Pre-operative rehabilitation for dysvascular lower-limb amputee patients: A focus group study involving medical professionals. Plos one. 2018 Oct 15;13(10):e0204726. https://doi.org/10.1371/journal.pone.0204726.
5. Cutti AG, Verni G, Migliore GL, Amoresano A, Raggi M. Reference values for gait temporal and loading symmetry of lower-limb amputees can help in refocusing rehabilitation targets. Journal of neuroengineering and rehabilitation. 2018 Sep;15:1-2. https://doi.org/10.1186/s12984-018-0403-x.
6. Richardson C, Olleveant N, Crawford K, Kulkarni J. Exploring the role of cortical reorganization in postamputation phantom phenomena, including phantom limb pain in lower limb amputees: a cross-sectional study of the patterns of referral of sensations into the phantom. Pain Management Nursing. 2018 Dec 1;19(6):599-607. https://doi.org/10.1016/j.pmn.2018.04.004.
7. Westerkamp EA, Strike SC, Patterson M. Dietary intakes and prevalence of overweight/obesity in male non-dysvascular lower limb amputees. Prosthetics and Orthotics International. 2019 Jun;43(3):284-92. https://doi.org/10.1177/0309364618823118.
8. Saetta G, Grond I, Brugger P, Lenggenhager B, Tsay AJ, Giummarra MJ. Apparent motion perception in lower limb amputees with phantom sensations:“obstacle shunning” and “obstacle tolerance”. Cortex. 2018 Jul 1;104:220-31. https://doi.org/10.1016/j.cortex.2018.03.003.
9. Henson DP, Edgar C, Ding Z, Sivapuratharasu B, Le Feuvre P, Finnegan ME, Quest R, McGregor AH, Bull AM. Understanding lower limb muscle volume adaptations to amputation. Journal of biomechanics. 2021 Aug 26;125:110599. https://doi.org/10.1016/j.jbiomech.2021.110599.
10. Turner S, McGregor AH. Perceived effect of socket fit on major lower limb prosthetic rehabilitation: a clinician and amputee perspective. Archives of rehabilitation research and clinical translation. 2020 Sep 1;2(3):100059. https://doi.org/10.1016/j.arrct.2020.100059.
11. Şimsek N, Öztürk GK, Nahya ZN. The mental health of individuals with post-traumatic lower limb amputation: a qualitative study. Journal of patient experience. 2020 Dec;7(6):1665-70. https://doi.org/10.1177/2374373520932451.
12. Chen L, Feng Y, Chen B, Wang Q, Wei K. Improving postural stability among people with lower-limb amputations by tactile sensory substitution. Journal of neuroengineering and rehabilitation. 2021 Dec;18:1-4. https://doi.org/10.1186/s12984-021-00952-x.
13. Charkhkar H, Christie BP, Triolo RJ. Sensory neuroprosthesis improves postural stability during Sensory Organization Test in lower-limb amputees. Scientific reports. 2020 Apr 24;10(1):6984. https://doi.org/10.1038/s41598-020-63936-2.
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Samir Ranjan Jena, Renuka Jyothi S, Ranjana Singh.
Data curation: Samir Ranjan Jena, Renuka Jyothi S, Ranjana Singh.
Formal analysis: Samir Ranjan Jena, Renuka Jyothi S, Ranjana Singh.
Drafting - original draft: Samir Ranjan Jena, Renuka Jyothi S, Ranjana Singh.
Writing - proofreading and editing: Samir Ranjan Jena, Renuka Jyothi S, Ranjana Singh.