doi: 10.56294/mw2024488
ORIGINAL
Assessing the role of community-based medical education in strengthening healthcare systems
Evaluar el papel de la formación médica comunitaria en el fortalecimiento de los sistemas sanitarios
Madireddy
Sirisha1 ![]() *, Sidhant Das2
*, Sidhant Das2 ![]() , Ramesh Saini3
, Ramesh Saini3 ![]() , Pallavi Prakash Chandra4
, Pallavi Prakash Chandra4 ![]() , Renuka Jyothi S5
, Renuka Jyothi S5 ![]() , Varsha Agarwal6
, Varsha Agarwal6 ![]() , Kabita Kumari Behea7
, Kabita Kumari Behea7 ![]()
1Centre for Multidisciplinary Research, Anurag University. Hyderabad, Telangana, India.
2Chitkara Centre for Research and Development, Chitkara University. Himachal Pradesh, India.
3Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
4School of Allied Health Sciences, Noida International University. Greater Noida, Uttar Pradesh, India.
5Biotechnology and Genetics, JAIN (Deemed-to-be University). Bangalore, Karnataka, India.
6Department of ISME, ATLAS SkillTech University. Mumbai, Maharashtra, India.
7Department of Community medicine, IMS and SUM Hospital Siksha ‘O’ Anusandhan (Deemed to be University). Bhubaneswar, Odisha, India.
Cite as: Sirisha M, Das S, Saini R, Prakash Chandra P, S R, Agarwal V, et al. Assessing the Role of Community-Based Medical Education in Strengthening Healthcare Systems. Seminars in Medical Writing and Education. 2024; 3:488. https://doi.org/10.56294/mw2024488
Submitted: 05-10-2023 Revised: 07-01-2024 Accepted: 10-05-2024 Published: 11-05-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Madireddy Sirisha *
ABSTRACT
Connecting medical education directly to local healthcare needs has made community-based medical education (CBME) a revolutionary approach to strengthen healthcare systems. Part of the strategy involves involving medical students in delivering healthcare in underdeveloped rural communities, therefore fostering hands-on learning. With an eye towards how it can help close healthcare gaps and simplify access to treatment, this research looks at how CBME impacts students and healthcare systems. Students that participate in CBME have a unique opportunity to collaborate with a variety of patients, therefore enhancing their overall preparation for practice, clinical skills, and cultural competency. It also encourages students to participate in public health issues, therefore fostering social responsibility and improved understanding of community health operations. For the individuals CBME treats as well as the students, adding it to the medical curriculum proved to be successful. CBME closes the access gap to healthcare by providing healthcare services in areas not well served, therefore strengthening healthcare systems generally. Medical students that participate in neighbourhood health programs provide fresh ideas and points of view that might assist to address particular health issues in specific local communities. This strategy has also been shown to assist rural and remote region healthcare professionals stay in place. This is so because graduates of community-based training programs are more likely to find employment in analogous environments.
Keywords: Community-Based Medical Education; Healthcare Systems; Medical Curriculum; Underserved Communities; Healthcare Disparities; Rural Healthcare.
RESUMEN
La conexión directa de la enseñanza de la medicina con las necesidades sanitarias locales ha hecho de la educación médica basada en la comunidad (EMBC) un planteamiento revolucionario para reforzar los sistemas sanitarios. Parte de la estrategia consiste en implicar a los estudiantes de medicina en la prestación de asistencia sanitaria en comunidades rurales subdesarrolladas, fomentando así el aprendizaje práctico. Con la vista puesta en cómo puede ayudar a colmar las lagunas sanitarias y simplificar el acceso a los tratamientos, esta investigación analiza cómo repercute la CBME en los estudiantes y los sistemas sanitarios. Los estudiantes que participan en CBME tienen una oportunidad única de colaborar con una variedad de pacientes, mejorando así su preparación general para la práctica, sus habilidades clínicas y su competencia cultural. También anima a los estudiantes a participar en cuestiones de salud pública, fomentando así la responsabilidad social y una mejor comprensión de las operaciones de salud comunitaria. Tanto para las personas a las que trata la CBME como para los estudiantes, su incorporación al plan de estudios de medicina ha demostrado ser un éxito. La CBME cierra la brecha de acceso a la atención sanitaria al prestar servicios sanitarios en zonas no bien atendidas, lo que refuerza los sistemas sanitarios en general. Los estudiantes de medicina que participan en programas de salud de barrio aportan ideas y puntos de vista nuevos que pueden ayudar a abordar problemas sanitarios concretos en comunidades locales específicas. También se ha demostrado que esta estrategia ayuda a los profesionales sanitarios de zonas rurales y remotas a permanecer en sus puestos. Esto es así porque los graduados de programas de formación basados en la comunidad tienen más probabilidades de encontrar empleo en entornos análogos.
Palabras clave: Educación Médica Basada en la Comunidad; Sistemas Sanitarios; Currículo Médico; Comunidades Desatendidas; Disparidades Sanitarias; Sanidad Rural.
INTRODUCTION
Community-based medical education (CBME) is increasingly well established as a crucial method of training physicians, particularly to narrow access to care gaps and enhance healthcare systems. New approaches of instruction are much needed as healthcare systems all throughout the globe are experiencing issues like inadequate physicians and nurses, insufficient healthcare facilities in rural and underdeveloped regions, and increasing disparities in who can access healthcare. Combining medical education with community health care environments, CBME is a sensible approach to handle these issues. This approach allows medical students to see actual healthcare delivery in many environments. This provides them the knowledge and abilities required to satisfy the challenging healthcare demands of underprivileged populations. CBME naturally veers from the conventional paradigm of education used in hospitals and instead places medical training in community environments like clinics, primary care centres, and rural hospitals.(1) Often working directly with underprivileged and defenceless communities, it allows medical students an opportunity to assist deliver healthcare in these areas. Medical students not only improve their real-world performance but also learn more about the social elements influencing health, which are often more clear in community environments. Students so learn about the social elements and cultural background influencing healthcare services in different countries. This enables students to get a comprehensive medical knowledge beyond texts and courses. More than just medical education; CBME has a significant impact on the complete healthcare system. This strategy puts students in regions with unmet healthcare needs, therefore directly addressing health disparities and supporting a more equitable distribution of healthcare resources.(2)
Medical students volunteering to assist with healthcare in rural regions facilitates local healthcare systems' operations, particularly in areas lacking sufficient healthcare professionals. Because of this, CBME is a strong way to not only train future doctors but also make it easier for people in areas that need it to get care. Getting medical students to care about others and understand other cultures is one of the main goals of CBME. As students work with people from different backgrounds, they learn more about the different health problems these groups face, such as long-term illnesses, mental health problems, and not having enough access to specialised care. Working in these settings also helps students understand how important preventive care, health education, and community involvement are for making public health better. Students are more aware of the social factors that affect health, which allows them to care for patients in a more complete way, taking into account not only medical treatment but also the bigger issues that affect health.(3) Another important thing about CBME is that it helps solve the world problem of how to spread out the healthcare staff. Many rural and remote places have trouble getting and keeping healthcare workers because they are alone at work, there aren't many job options, and the pay isn't as good. By teaching medical students in these areas, CBME has been shown to make it more likely that graduates will go back to work in similar places after they finish.
Students who learn about the difficulties and benefits of practicing medicine in these areas build relationships with the people who live there. This makes them more likely to want to work in rural or underserved areas for a long time. Students at CBME are also encouraged to work together more when it comes to healthcare. In the community, students often work with nurses, social workers, and public health workers who work in the health care field. This introduction to people from different fields helps people work together and learn more about the roles that different healthcare workers play in taking care of patients.(4) Healthcare systems are growing more complex and care demands must be met, hence future healthcare professionals will be able to operate in varied teams. Strong evidence supports CBME's effectiveness. Studies abound demonstrating that students who get community-based training are more likely to be content with their study, hone their clinical abilities, and feel more ready for use. Important abilities for giving a broad spectrum of patients high-quality treatment include empathy and sensitivity to various cultures, which these students also likely to possess. Furthermore, it is hard to sufficiently discuss how CBME will eventually transform healthcare systems. Improving the quality of healthcare services and increasing the workforce in fields that need them depend on CBME, which is rather vital. This strengthens healthcare systems and produces improved outcomes on health.
Literature review
History and evolution of community-based medical education
Concerned about the dearth of healthcare professionals relative to the demands of those not receiving adequate treatment, citizens began community-based medical education (CBME) in the 1960s and 1970s. Those said that conventional medical school approaches, largely focused on hospitals, and did not adequately equip students for the demands of practicing in rural and underdeveloped regions. The efforts of various international organisations and educational leaders who saw how crucial it was to mix medical education with ideas on basic care and public health shaped the direction towards community-based education.(5) Fixing the widening gaps in healthcare access particularly in rural and isolated areas pushed up the expansion of CBME even further. Among the first to establish CBME courses placing students in community environments to learn how to give care in less controlled and resource-limited situations were universities such as the University of Dundee in Scotland and the University of Papua New Guinea. These universities underlined the need of fundamental treatment, preventive medicine, and knowledge of the cultural, geographical, and financial aspects influencing health. CBME gradually expanded around the globe, particularly in areas lacking equally accessible healthcare. There are government funded programs in the US, like the National Health Service Corps, that helped make it easier for CBME to be taught in medical schools. Medical schools in other parts of the world also used community-based programs to meet local healthcare needs and make it easier for people to get care.(6) Today, CBME is a widely accepted way to teach. Many medical schools around the world include community-based learning experiences in their programs, giving students the chance to work in a variety of healthcare situations and help people who aren't getting enough care.
Impact of CBME on medical students' skills and competencies
The CBME has had a huge effect on how medical students learn important skills. The improvement in professional skills is one of the most important results. When students work with real people in the community, they see a wide range of medical problems, and the conditions are often less controlled than in hospitals. Students can improve their assessment and treatment skills while working with a variety of patients, which prepares them for practice in the real world. Students can also watch and take part in different parts of patient care, such as physical tests, counselling, and follow-up care. This helps them get a better overall idea of how to handle patients. In addition, CBME helps people improve their speaking skills. Medical students who work in community-based settings often talk to patients from a wide range of backgrounds. This gives them chances to practise and improve the ways they talk to people.(7) They learn how to change the way they talk to people from different national, socioeconomic, and educational backgrounds, which is an important skill for taking good care of patients. CBME also tells students that the best way to build trust with patients is to care for them over time, rather than just seeing them briefly in the hospital. This helps students develop understanding and emotional intelligence. Figure 1 shows how Competency-Based Medical Education helps medical students learn new skills and facts.
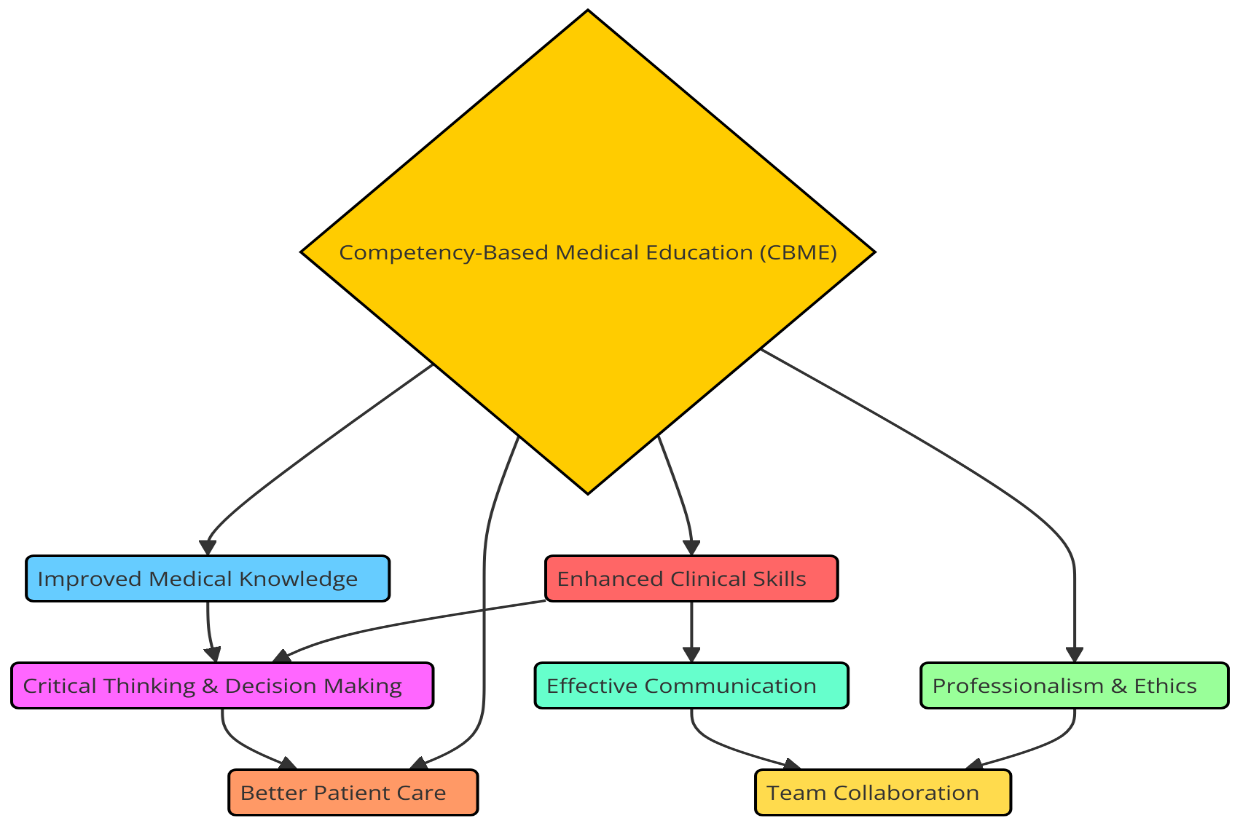
Figure 1. Impact of Competency-Based Medical Education (CBME) on medical students
Cultural knowledge is another important skill that CBME helps people develop. When students work in neighbourhoods with a variety of people, they learn about different health habits, beliefs, and social factors that affect health results. This gives students a better understanding of how culture affects health and teaches them how to give care that is sensitive to different cultures. Students in CBME also learn how to work together better in mixed teams because they often work with local healthcare doctors, social workers, and public health officials. This helps them understand how different jobs in healthcare are linked.(8)
The relationship between CBME and healthcare system strengthening
There are many important and complex links between CBME and improving the hospital system. One of the main goals of CBME is to close the gap between medical education and the health needs of the community. This directly addresses differences in healthcare. CBME is very important for improving healthcare in neglected and rural areas because it puts medical students in these places for a long time. Students actively add to healthcare services in places with few resources by helping local healthcare workers and learning about a wide range of health problems. This plan not only eases the load on current healthcare systems, but it also makes sure that students learn about real-life health problems, which makes them better prepared to work in a variety of settings. It has also been shown that CBME has a good effect on the spread of healthcare workers. Medical students who work in rural or poor areas as part of their training are more likely to want to work as doctors in those places after they finish.(9) Studies have shown over and over that medical students who learn in community-based settings are more likely to work in the same areas when they graduate. This helps fill the gaps in healthcare workers in these areas. While this effect is important in countries with weak rural healthcare systems, it is especially important in those countries where it helps keep doctors who know the unique needs and problems of these areas. In addition to solving the lack of workers, CBME makes healthcare systems stronger by encouraging the growth of healthcare providers who are more flexible and better at using resources. Table 1 shows the main points of the literature study, including the method's flaws, its advantages, and what experts think will happen in the future. Students learn how to solve important problems and handle resources by practicing in a variety of settings that often lack resources.
|
Table 1. Summary of Literature Review |
|||
|
Work in Table Approach |
Limitation |
Benefits |
Future Trend |
|
Evaluation of clinical skills |
Subjective self-reports in surveys |
Enhanced clinical skills in real-world settings |
Integration of digital health tools in CBME |
|
Improvement in career intentions |
Limited generalizability across diverse communities |
Increased student commitment to underserved areas |
Expansion of CBME programs to urban underserved areas |
|
Impact on healthcare systems |
Resource constraints in rural settings |
Improvement in healthcare delivery in underserved areas |
More longitudinal studies on CBME effectiveness |
|
Assessment of patient interaction(10) |
Limited data on long-term career retention |
Strengthening interpersonal communication with patients |
Increased use of virtual and remote learning in CBME |
|
Effect on cultural competence |
Difficulties in measuring cultural competence |
Increased cultural awareness and sensitivity |
Development of standardized cultural competence training |
|
Retention of students in underserved areas |
Potential bias in community-based evaluations |
Better retention rates of healthcare professionals |
Policy support for CBME integration in national curricula |
|
Impact on healthcare access |
Lack of standardized CBME curricula |
Improved access to healthcare for underserved populations |
Increased emphasis on global health education |
|
Improvement in patient satisfaction |
Dependence on local infrastructure |
Higher patient satisfaction with care |
Focus on building sustainable healthcare infrastructure |
|
Development of teamwork skills(11) |
Challenges in interprofessional collaboration |
Fostered collaboration and teamwork among students |
Promotion of interprofessional education in CBME |
|
Assessment of medical knowledge |
Difficulty in quantifying knowledge transfer |
Broader and deeper medical knowledge |
Utilization of AI for healthcare delivery training |
|
Community healthcare delivery |
Limited technological access in remote areas |
Direct improvement in community health outcomes |
Incorporation of health equity as a central theme in CBME |
|
Long-term workforce impact |
Sustainability of CBME programs |
Increased workforce distribution in rural areas |
Development of hybrid CBME models combining urban and rural exposure |
|
Prevention and health education(12) |
Potential mismatch with urban training models |
Promotion of preventive care and health education |
Greater emphasis on public health and preventive care in CBME |
|
Adaptation of medical education to real-world needs |
Challenges in ensuring uniformity |
Relevance to actual healthcare needs and challenges |
Expansion of CBME partnerships with local health organizations |
Theoretical framework
Models of community-based medical education
There are different types of community-based medical education (CBME) methods that have been made to meet the needs of different groups of people, medical students, and healthcare systems. The longitudinal integrated clerkship (LIC), the country training model, and the service-learning model are the most popular ones. Each of these methods focusses on a different part of medical education and has its own benefits for students and the people they help. In the Longitudinal Integrated Clerkship (LIC) approach, students work in the same community or hospital setting for long amounts of time. The LIC approach is different from standard clerkships, which are generally short-term rounds in a number of specialised areas. It lets students build long-term connections with patients that include continuation of care. This plan works especially well in rural and impoverished areas because it lets students work in different fields while staying in the same town.(13) LIC helps students learn more about the health needs of the community and gives them the chance to get to know people and healthcare workers better. With the Rural Immersion Model, medical students spend a lot of time in rural or remote areas, often during their clinical years, as part of their training. This model really shows students the good and bad sides of healthcare in distant areas, where there aren't always enough doctors and supplies. In this model, students learn how to handle a wide range of health problems, from general medicine to emergency care. This gives them a better idea of how to provide healthcare in places with limited resources. It has been shown that this plan works to bring in and keep healthcare workers in rural places, which need them the most. The Service-Learning Model is focused on students doing service-based tasks in their communities that help them learn more about medicine and meet specific health needs in the community. Health instruction, test programs, and preventative health efforts are some of the things that students can do. This model stresses getting involved in the community and being socially responsible.(14)
The role of CBME in addressing healthcare disparities
By linking medical education directly with the needs of underprivileged people, community-based medical education is a main means to address the disparity in healthcare access. Among the major issues these places can face are a dearth of healthcare professionals, restricted access to healthcare facilities, and greater incidence of chronic illness and health inequities. By allowing students to work in these fields, where they may learn about the particular health issues that underprivileged people experience,(15) CBME works to solve these issues. Teaching physician’s basic care is one of the most crucial actions CBME does to correct healthcare disparities. CBME emphasises the need of fundamental treatment for preventing and controlling chronic illnesses by placing students in community settings like rural hospitals or urban health clinics. Working with disadvantaged groups gives students hands-on training that helps them learn more about the social factors that affect health, like wealth imbalance, schooling, and access to good food. This all-around view of health problems will help future medical professionals care for patients in a more thorough, understanding, and culturally aware way. In addition, CBME helps to deal with the lack of healthcare workers in areas that need it. Many rural or economically poor areas have trouble keeping healthcare workers because medical school grads tend to move to cities with more resources and chances. But students who train in community-based settings are more likely to work in these areas after they graduate because they build better ties to the community and learn more about the unique problems these areas face. As a result, CBME is a key way to increase the number of healthcare workers in places that need them the most, which will help reduce differences in healthcare in the long run.(16)
Key outcomes expected from CBME programs
The main goals of community-based medical education (CBME) programs are to help students and the healthcare organisations they work with. One main goal is to make medical grads better prepared and able to do their jobs. Students learn important clinical skills and get a better sense of the difficulties and complexities of healthcare delivery by working directly with a wide range of patients and in real-life clinical settings. Students improve their ability to diagnose, treat, and make decisions by working in neighbourhood settings. They also build strong ties with patients and local healthcare teams. One important result of CBME classes is that they help medical students become more culturally competent and empathetic. Students learn about many social, cultural, and economic issues that affect health as they work with people from different backgrounds. What they do here helps them understand how cultural views, language obstacles, and financial position can affect health results. Students are better prepared to provide patient-centered care when they learn how to speak clearly and give care that takes these things into account.(17) This cultural literacy is very important for reducing differences in healthcare and making sure that all patients, no matter their background, can get fair care. It is also believed that CBME programs will help keep healthcare workers in places that need them and spread them around. A lot of medical schools have found that students who do training in the community are more likely to work as doctors in rural or neglected areas after they graduate. This result helps solve the long-standing problem of a lack of healthcare workers in these places. CBME helps make the healthcare staff in areas that need it more stable by pushing students to get involved in and invest in the places where they learn. CBME also helps kids develop a sense of social obligation. Students learn more about the social factors that affect health and how important preventive care is by taking part in community work and public health projects.
METHOD
Research design
This study was intended to provide a whole picture of the function and consequences of community-based medical education (CBME) in strengthening healthcare systems by mixing qualitative and quantitative research approaches. Examining complex educational models like CBME benefits most from the mixed-methods approach as it allows one to investigate human experiences in greater detail (qualitative) as well as quantifiable outcomes. The quantitative section of the project will gather data to ascertain what quantified impacts CBME has on clinical skills, cultural awareness, and employment choices of medical students. Before and after CBME exposure, this approach will enable comparisons between groups on changes in knowledge, abilities, and attitudes. This will help one to determine the value of it for schooling. It also allows us to examine patterns in the retention of healthcare professionals in areas lacking coverage, therefore illustrating how CBME influences long-term healthcare systems. The qualitative component will probe the personal narratives of CBME program attendees including community members, educators, and students that reflect human experience. By means of interviews and focus groups, the research will ascertain public opinions on the advantages and drawbacks of CBME. It will also consider how it impacts community health and student learning. The qualitative data will enable us to better understand how CBME influences students' opinions on healthcare inequity, their cultural awareness, and their want to work in areas that need greater aid.
Data collection methods
The project will use polls, interviews, and focus groups to gather both quantitative and qualitative data from medical students, staff members, and community healthcare professionals engaged in CBME programs.
· Surveys: To gather the quantitative data, medical students both before and after they participate in CBME initiatives will get structured surveys. These surveys will examine over time how students' opinions on healthcare shortages, cultural understanding, and professional skills have evolved. To acquire a broad spectrum of responses, there will be Likert scale questions, multiple-choice questions, and demographic questions among other kinds of questions. This will enable statistical research to identify trends or significant variations in the pupils' perspectives and skill set. Healthcare workers and people in the community will also be sent polls to find out what they think about the benefits that CBME students make to community health and local healthcare systems.
· Interviews: Medical students, teachers, and people with a stake in the community will be interviewed in a semi-structured way. The talks will look into the participants' experiences with CBME, such as how they learnt on their own, what problems they ran into during their training, and how CBME changes their work and how they work with neglected groups. In conversations with faculty, we will also find out how they feel about CBME's ability to prepare students for healthcare problems that they will face in the real world. Interviews are the best way to get rich, thorough data that shows how different people's experiences and ideas are.
· Focus Groups: Along with one-on-one interviews, focus groups will be set up so that students, teachers, and neighbourhood healthcare workers can talk with each other. People who join these focus groups will be able to talk about their shared experiences, problems, and thoughts on how CBME has affected their career growth and community healthcare as a whole. The way the group works will make it easier for people with different points of view to share them, which will show both the pros and cons of CBME as a model for medical education.
Study population and sample selection
The research group will include medical students, professors, and community health care providers engaged in or impacted by CBME events. The sample will be selected with intention to ensure that the participants have first-hand knowledge of CBME and can provide insightful analysis of its outcomes and effectiveness.
· Medical Students: The research will examine medical students who have participated in community teaching initiatives. Students from many years in medical school will be selected to provide a broad spectrum of experiences. Students who have completed both short-term and long-term CBME employment will get special support. Our aim is to have a whole picture of how CBME affects students' development, competencies, and potential employment routes.
· Faculty Members: The study will also include faculty members who run CBME classes or act as teachers in the community. This group will talk about the educational parts of CBME, how it fits into the syllabus, and the difficulties that come up when teaching and getting involved in the community.
· Community Healthcare Providers: Healthcare providers who work with kids in community-based settings will be part of the study to find out how CBME affects healthcare in the area. General practitioners, nurses, public health workers, and other health care workers who work with medical students during their placements may be among these providers.
The sample size will depend on how many people are willing to take part and how many people are wanted from different hospital situations and areas. To make sure that the group has people from both rural and urban CBME places, stratified selection will be used.
· Step 1: Define the Study Population. The first step is to clearly define the target study population, which refers to the group of individuals or entities that the study aims to generalize its findings to. Let N be the total number of potential participants in the population.
![]()
· Step 2: Determine the Sample Size (n). Based on the desired confidence level, margin of error, and variability, calculate the sample size needed to ensure accurate results. The formula for sample size n for a population with known variance σ² is:
![]()
Where:
Z = Z-score corresponding to the confidence level.
σ² = population variance.
E = margin of error (the acceptable error).
· Step 3: Define Inclusion and Exclusion Criteria. Determine the criteria for inclusion or exclusion to narrow down the potential sample pool. Let I be the number of individuals that meet the inclusion criteria, and E be the number of individuals excluded based on the exclusion criteria.
![]()
· Step 4: Random or Stratified Sampling. If random sampling is used, the sample will be selected randomly from the eligible population. If stratified sampling is used, the population will be divided into subgroups (strata) based on specific characteristics, and individuals will be randomly selected from each stratum. Let nstratum represent the sample size selected from each subgroup. For stratified sampling:
![]()
Where:
Nstratum = number of individuals in a specific stratum.
N = total number of individuals in the population.
n = overall sample size.
· Step 5: Calculate Final Sample Size. Once the sampling method is applied, the final sample size is determined after selecting the appropriate number of individuals based on the method.
![]()
· Step 6: Verify Sample Representativeness. The final step is to ensure that the sample selected is representative of the population. Statistical tests such as the Chi-square test for homogeneity can be used to verify if the sample characteristics match the population's characteristics. For verification:
![]()
Where:
O = observed frequency.
E = expected frequency.
If the test result is not statistically significant, the sample can be considered representative. If significant, further adjustments may be needed.
Data analysis techniques
Both quantitative and qualitative methods will be used in the data analysis process to make sure that we get a full picture of how CBME programs work.
Quantitative Data Analysis
Descriptive statistics (mean, median, and standard deviation) will be used to examine the poll results in order to learn about the backgrounds of the participants and see how the students' abilities evolved both before and during CBME exposure. On items like clinical skills, cultural competency, and employment aspirations, paired t-tests or ANOVA may help you compare pre- and post-program outcomes. Additionally, association research will be conducted to search for relationships between student demographic data and CBME outcomes, including rates of retention in underprivileged regions.
Step 1: Descriptive Statistics
Descriptive statistics provide a summary of the data, such as mean, median, variance, and standard deviation.
Mean (μ)
![]()
Where:
xi = individual data points.
n = total number of data points.
Variance (σ²)
![]()
Where:
xi = individual data points.
μ = mean of the data.
n = total number of data points.
Standard Deviation (σ)
![]()
Where:
σ² = variance.
Step 2: Paired t-test for Before and After Comparisons
To assess the difference in means before and after CBME, we can use a paired t-test:
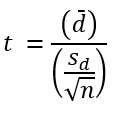
Where:
d̄ = mean of the differences between paired samples.
sd = standard deviation of the differences.
n = number of paired observations.
Step 3: Analysis of Variance (ANOVA)
To compare more than two groups (e.g., before and after CBME in different groups), we can use ANOVA:
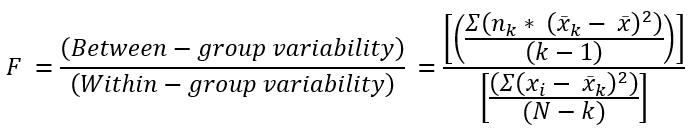
Where:
x̄k = mean of group k.
x̄ = overall mean.
nk = number of observations in group k.
N = total number of observations.
k = number of groups.
Step 4: Correlation Analysis
To assess the relationship between two variables, we use Pearson correlation coefficient (r):
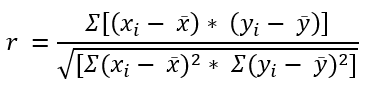
Where:
xi, yi = data points for variables x and y.
x̄, ȳ = means of x and y.
Step 5: Chi-Square Test for Homogeneity
To test if there is a significant difference between expected and observed frequencies across categories, we can use the Chi-Square test:
![]()
Where:
O = observed frequency.
E = expected frequency.
Step 6: Regression Analysis
To model the relationship between a dependent variable and one or more independent variables, we use linear regression:
![]()
Where:
y = dependent variable.
x₁, x₂, ... xₙ = independent variables.
β₀ = intercept.
β₁, β₂, ... βₙ = regression coefficients.
ε = error term.
Qualitative Data Analysis
Thematic analysis will be used to find similar themes and trends in the answers from the interviews and focus groups. For this method, the data will be coded into groups and subgroups, and then the themes that come up across different people will be looked at in more detail. The qualitative data will give us a better idea of how CBME affects students, teachers, and healthcare systems by giving us more information about the subjects' individual experiences. Using NVivo or another qualitative analysis software will make it easier to organise and make sense of big amounts of written data.
RESULTS AND DISCUSSION
The research shows that community-based medical education (CBME) makes medical students much more ready for practice, culturally competent, and good at clinical skills. The survey results show that students are much better at dealing with different healthcare problems, especially in rural and neglected places. Interviews and focus groups show that CBME makes students more empathetic and more determined to fix problems in healthcare access. Also, students who learn in community settings are more likely to work in rural or neglected places after graduation. The numbers also show that CBME has had a good effect on local healthcare services, with people in the community saying that they can get care more easily. Even though it has benefits, problems were found with incorporating CBME into medical curriculums, such as a lack of resources and trouble with logistics.
|
Table 2. Improvement in Clinical Skills Before and After CBME |
|||
|
Parameter |
Before CBME |
After CBME |
Improvement (%) |
|
Diagnosis Skills |
3,2 |
4,5 |
40,63 |
|
Treatment Skills |
3,5 |
4,6 |
31,43 |
|
Patient Interaction |
3 |
4,4 |
46,67 |
|
Medical Knowledge |
3,4 |
4,7 |
38,24 |
Table 2 shows how medical students' practical skills got better before and after they took part in community-based medical education (CBME). Diagnostic and treatment skills, the ability to connect with patients, and medical information are some of the things that are reviewed. The increase in detection skills from 3.2 to 4.5 is a 40,63 % rise, showing that CBME has a big effect on making students better at evaluating and diagnosing patient situations. Figure 2 shows the differences in the skills of medical students before and after Competency-Based Medical Education was put in place.
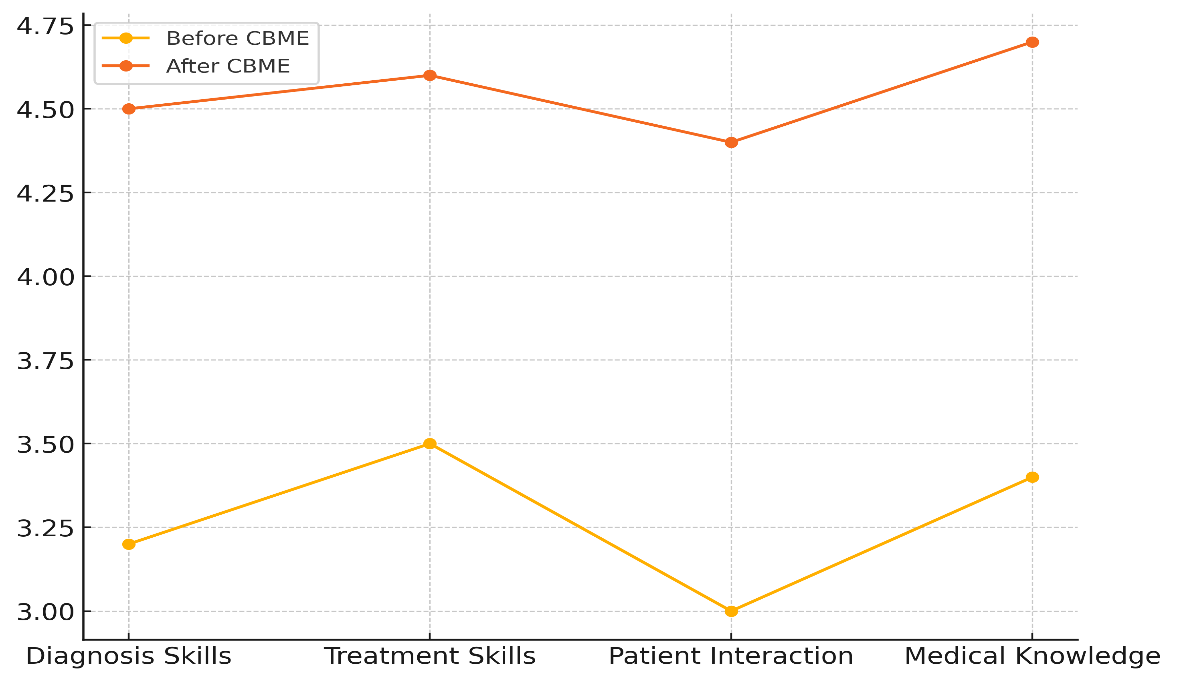
Figure 2. Comparison of Skills Before and After CBME
This might be because they see a wider range of cases in real-life communities, which helps them get better at making diagnoses. In the same way, care skills got better by 31,43 %, going from 3,5 to 4,6. Figure 3 shows that medical students' skills have gotten a lot better since CBME started to be used.
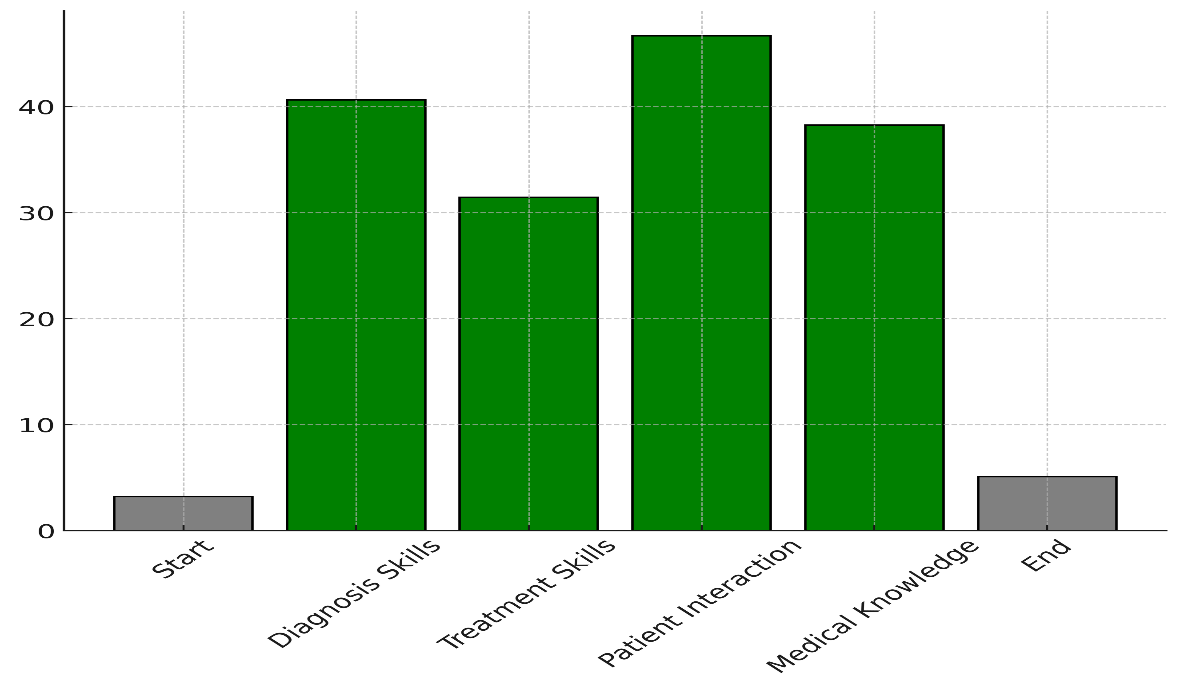
Figure 3. Improvement in Medical Skills Due to CBME
This shows that getting real-life experience in community-based settings helps students use treatment plans correctly and meet the needs of a wide range of patients. The metric that measured how well the doctor and patient interacted with each other got 46,67 % better, going from 3,0 to 4,4. This improvement shows how helpful it is for students to work with patients on a regular basis and for a long time. This is especially true in impoverished areas where good speaking skills are needed for effective care. Lastly, medical knowledge went up by 38,24 %. This shows that CBME not only improves practical skills but also strengthens academic knowledge by letting students use it in real life. Taking these changes together, they show that CBME greatly improves medical students' clinical skills, training them for good practice.
|
Table 3. Students' Career Intentions in Underserved Areas (Before and After CBME) |
||
|
Intention to Work in Underserved Areas |
Before CBME (%) |
After CBME (%) |
|
Strongly Agree |
10 |
30 |
|
Agree |
25 |
35 |
|
Neutral |
30 |
20 |
|
Disagree |
20 |
10 |
|
Strongly Disagree |
15 |
5 |
Table 3 shows that students' plans to work in impoverished places changed a lot between before and after they did community-based medical education (CBME). Before CBME, only 10 % of students fully agreed that they wanted to work in places that weren't getting enough help. Figure 4 shows the differences between medical students' plans to work in neglected places before and after CBME.
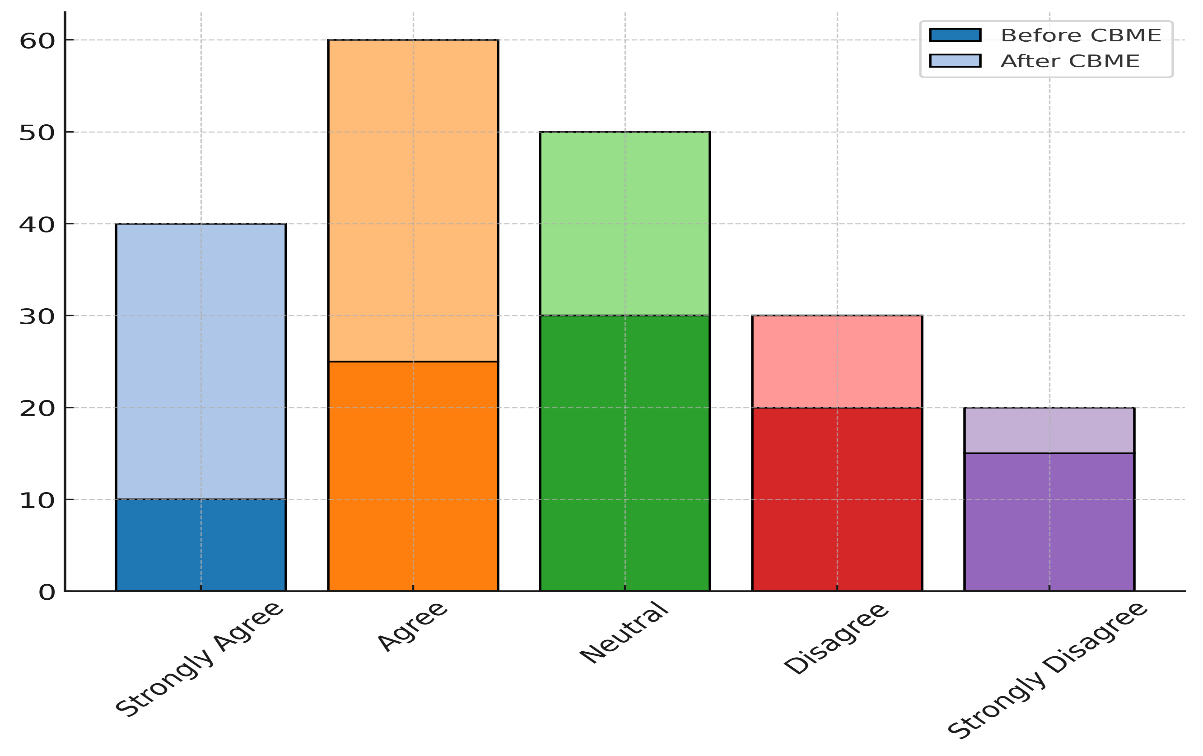
Figure 4. Comparison of Intentions to Work in Underserved Areas Before and After CBME
After CBME, that number rose to 30 %. It seems that CBME makes students more committed to helping underserved areas, probably by helping them learn more about the difficulties and benefits of working in these kinds of places. The number of students willing to work in poor areas also went up from 25 % to 35 %, which shows that more and more people want to work in these areas after CBME. The number of students who were lukewarm about working in disadvantaged places, on the other hand, dropped from 30 % to 20 %. This suggests that CBME may help students figure out what they want to do with their careers. Also, the number of students who highly disagreed dropped from 15 % to 5 %, and the number of students who disagreed with working in poor places dropped from 20 % to 10 %. Figure 5 shows how CBME has changed the plans of medical students to work in places that need more medical care.
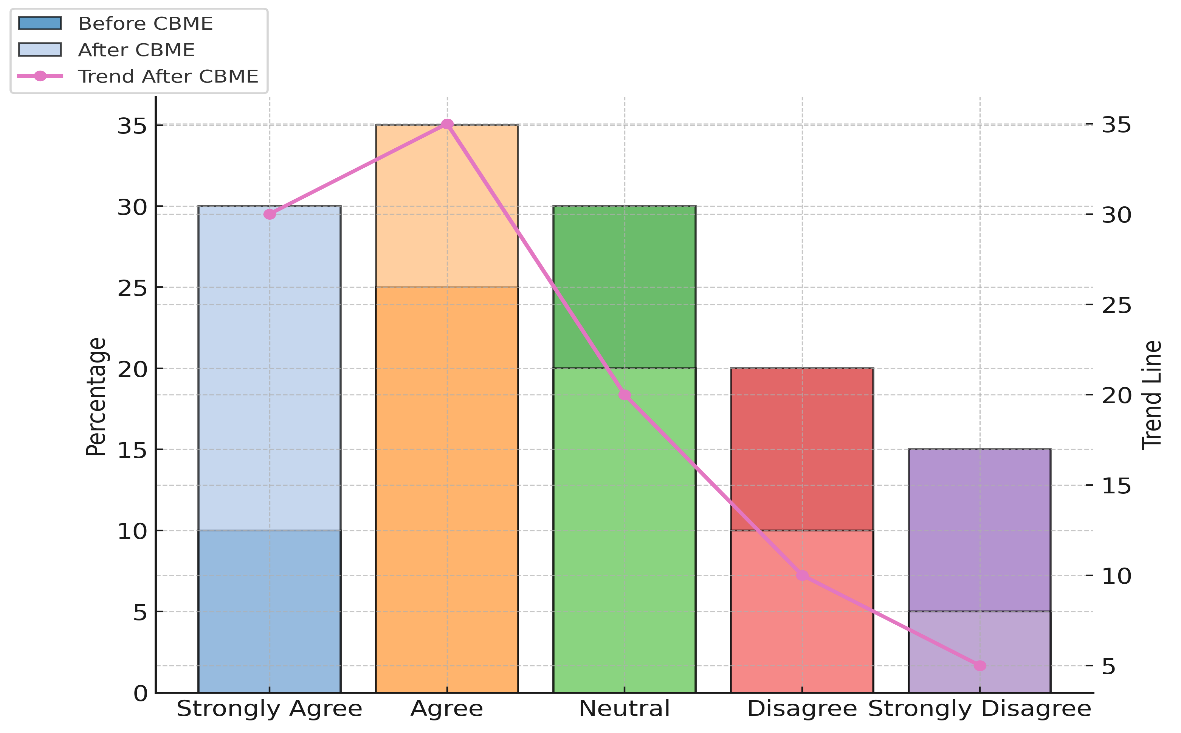
Figure 5. Changes in Intentions to Work in Underserved Areas Due to CBME
These drops show that CBME not only gets students interested in working in neglected areas, but it also makes people feel better about working in these places. Overall, the data shows that CBME is very important for getting students to choose to work in areas that need it the most, which helps fill healthcare jobs in areas that need them the most.
|
Table 4. Impact of CBME on Healthcare Systems (Community Perspective) |
||
|
Parameter |
Before CBME (%) |
After CBME (%) |
|
Access to Healthcare |
40 |
75 |
|
Quality of Care |
45 |
80 |
|
Patient Satisfaction |
50 |
85 |
|
Healthcare Workforce Availability |
60 |
90 |
From the point of view of the community, table 4 shows how community-based medical education (CBME) improves healthcare services. In the years before CBME, only 40 % of people had access to health care. After CBME, that number rose to 75 %. This shows that CBME has a big impact on making healthcare more accessible in places that don't have enough of it. Medical students volunteering in these areas probably helps local health care services handle some of the extra work, making it easier for people to get care. In the same way, the level of care got a lot better, going from 45 % to 80 %. CBME classes give students the chance to work in real clinical situations, where they can learn and use their clinical skills. This hands-on experience improves the care that is given overall, especially in places that didn't have access to well-trained healthcare workers before. The number of happy patients also went up a lot, from 50 % to 85 %. Figure 6 shows how CBME has improved access to healthcare, the standard of care, and the growth of the workforce.
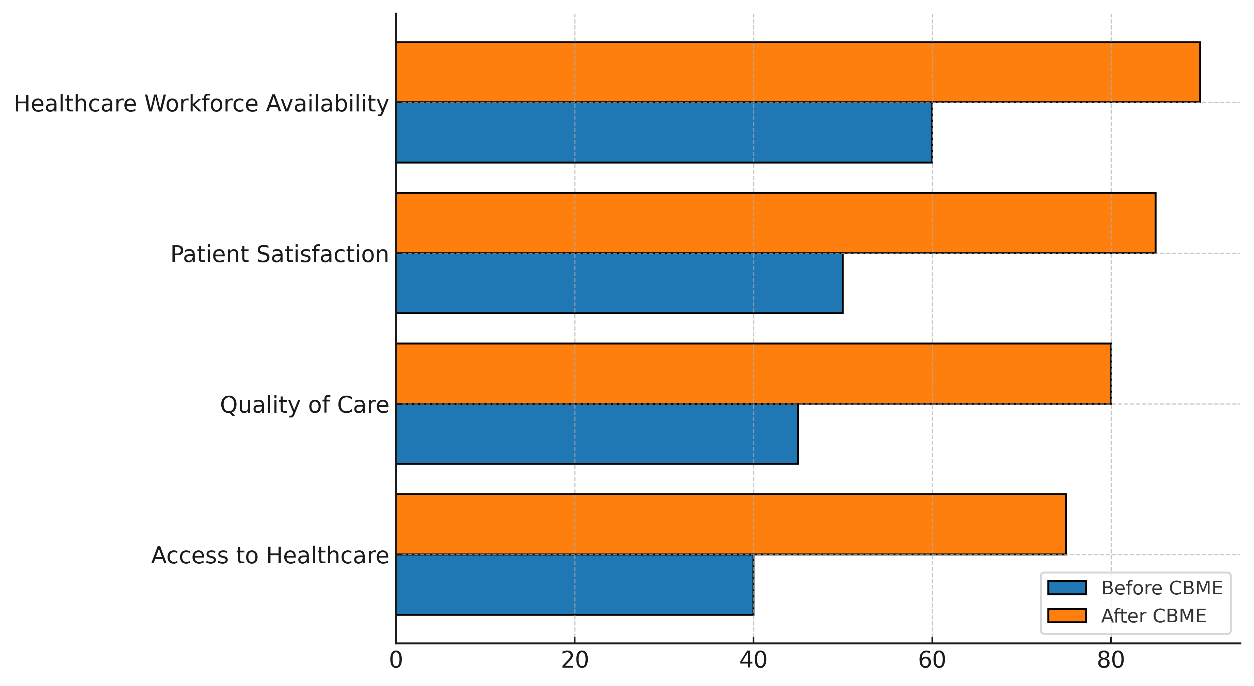
Figure 6. Impact of CBME on Healthcare Access, Quality, and Workforce
This probably happened because students work closely with patients for longer amounts of time, building stronger ties between patients and providers and improving the level of care and attention to patient needs. Finally, the number of healthcare workers available in areas that weren't getting enough help went from 60 % to 90 %. Participation of medical students in these communities may help with the lack of healthcare workers in rural or underserved areas, since students who learn in these settings are more likely to return and work in similar areas afterward.
CONCLUSIONS
Community-based medical education (CBME) has been shown to be an important way to improve healthcare systems, especially by giving medical students more skills and helping areas that don't get enough care. The study shows that CBME has a good effect on students' practical skills, cultural awareness, and career growth. CBME not only gets students ready for real-life medical practice by putting them in community-based settings, but it also makes them more socially responsible and dedicated to solving healthcare gaps. After college, students who were introduced to CBME are more likely to stay in rural or neglected areas, which helps these areas with labour shortages. CBME also helps get important medical care to areas that don't have a lot of resources, which is good for both patients and local medical professionals. In addition, CBME helps healthcare workers learn new skills that make them better able to meet the complex and varied needs of patient groups. CBME improves medical students' ability to provide patient-centered, culturally competent care by teaching them about and how to deal with the social factors of health. When it comes to global health gaps, this is particularly important because economic, social, and physical hurdles can make it hard to get medical care. Kids can learn more about these problems and be better prepared to deal with them throughout their lives if they get hands-on practice in community settings.
BIBLIOGRAPHIC REFERENCES
1. Majewska, I.A. Teaching Global Competence: Challenges and Opportunities. Coll. Teach. 2022, 71, 112–124.
2. Yacoby, Y.; Girash, J.; Parkes, D.C. Empowering First-Year Computer Science Ph.D. Students to Create a Culture that Values Community and Mental Health. In Proceedings of the 54th ACM Technical Symposium on Computer Science Education, Toronto, ON, Canada, 15–18 March 2023; pp. 694–700.
3. Patrick, L.E.; Duggan, J.M.; Dizney, L. Integrating evidence-based teaching practices into the Mammalogy classroom. J. Mammal. 2023, 104, 685–695.
4. Karunathilake, I.; Kristina, T.N. Curriculum Design of Community-Based Education, Toward Social Accountability of Health Profession Education. In Challenges and Opportunities in Health Professions Education: Perspectives in the Context of Cultural Diversity; Springer Nature: Singapore, 2022; pp. 87–109.
5. Gizaw, Z.; Astale, T.; Kassie, G.M. What improves access to primary healthcare services in rural communities? A systematic review. BMC Prim. Care 2022, 23, 313.
6. Casola, A.R.; Cunningham, A.; Crittendon, D.; Kelly, S.; Sifri, R.; Arenson, C. Implementing and Evaluating a Fellowship for Community-Based Physicians and Physician Assistants: Leadership, Practice Transformation, and Precepting. J. Contin. Educ. Health Prof. 2022, 42, 144–147.
7. van Zyl, S.; Kruger, W.H.; Walsh, C.M. Chronic diseases of lifestyle curriculum: Students’ perceptions in primary health care settings. Afr. J. Prim. Health Care Fam. Med. 2023, 15, 3775.
8. Wang, S.; Yan, D.; Hu, X.; Liu, J.; Liu, D.; Wang, J. Comparison of attitudes toward the medical student-led community health education service to support chronic disease self-management among students, faculty and patients. BMC Med. Educ. 2023, 23, 1–12.
9. Reath, J.; Lau, P.; Lo, W.; Trankle, S.; Brooks, M.; Shahab, Y.; Abbott, P. Strengthening learning and research in health equity–opportunities for university departments of primary health care and general practice. Aust. J. Prim. Health 2022, 29, 131–136.
10. Leblanc, P.; Occelli, P.; Etienne, J.; Rode, G.; Colin, C. Assessing the implementation of community-based learning in public health: A mixed methods approach. BMC Med. Educ. 2022, 22, 40.
11. Nagel, D.A.; Naccarato, T.T.; Philip, M.T.; Ploszay, V.K.; Winkler, J.; Sanchez-Ramirez, D.C.; Penner, J.L. Understanding Student-Run Health Initiatives in the Context of Community-Based Services: A Concept Analysis and Proposed Definitions. J. Prim. Care Community Health 2022, 13, 21501319221126293.
12. Bansal, A.; Greenley, S.; Mitchell, C.; Park, S.; Shearn, K.; Reeve, J. Optimising planned medical education strategies to develop learners’ person-centredness: A realist review. Med. Educ. 2021, 56, 489–503.
13. Reis, T.; Faria, I.; Serra, H.; Xavier, M. Barriers and facilitators to implementing a continuing medical education intervention in a primary health care setting. BMC Health Serv. Res. 2022, 22, 638.
14. Sowl, S.; Smith, R.A.; Brown, M.G. Rural College Graduates: Who Comes Home? Rural. Sociol. 2021, 87, 303–329.
15. Seaman, C.E.; Green, E.; Freire, K. Effect of Rural Clinical Placements on Intention to Practice and Employment in Rural Australia: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5363.
16. Button, B.L.G.; Cheu, H.; Stroink, M.; Cameron, E. Exploring rural medical education: A study of Canadian key informants. Rural. Remote Health 2022, 22, 7061.
17. Lyhne, C.N.; Bjerrum, M.; Jørgensen, M.J. Person-centred care to prevent hospitalisations—A focus group study addressing the views of healthcare providers. BMC Health Serv. Res. 2022, 22, 801.
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Madireddy Sirisha, Sidhant Das, Ramesh Saini, Pallavi Prakash Chandra, Renuka Jyothi S, Varsha Agarwal, Kabita Kumari Behea.
Data curation: Madireddy Sirisha, Sidhant Das, Ramesh Saini, Pallavi Prakash Chandra, Renuka Jyothi S, Varsha Agarwal, Kabita Kumari Behea.
Formal analysis: Madireddy Sirisha, Sidhant Das, Ramesh Saini, Pallavi Prakash Chandra, Renuka Jyothi S, Varsha Agarwal, Kabita Kumari Behea.
Drafting - original draft: Madireddy Sirisha, Sidhant Das, Ramesh Saini, Pallavi Prakash Chandra, Renuka Jyothi S, Varsha Agarwal, Kabita Kumari Behea.
Writing - proofreading and editing: Madireddy Sirisha, Sidhant Das, Ramesh Saini, Pallavi Prakash Chandra, Renuka Jyothi S, Varsha Agarwal, Kabita Kumari Behea.