doi: 10.56294/mw2024490
ORIGINAL
Strengthening Medical Education in Underserved Districts Through Interdisciplinary and Experiential Learning Models
Fortalecimiento de la Educación Médica en Distritos Marginados mediante Modelos de Aprendizaje Interdisciplinario y Experiencial
Vinima Gambhir1
![]() *, Samir Sahu2
*, Samir Sahu2
![]() ,
Karan Pandre3
,
Karan Pandre3 ![]() ,
Jatin Khurana4
,
Jatin Khurana4 ![]() ,
Simranjeet Nanda5
,
Simranjeet Nanda5 ![]() ,
RK Sinha6
,
RK Sinha6 ![]() ,
Jamuna KV7
,
Jamuna KV7 ![]()
1Department of ISME, ATLAS SkillTech University, Mumbai, Maharashtra, India.
2Department of General Medicine, IMS and SUM Hospital, Siksha 'O' Anusandhan (Deemed to be University), Bhubaneswar, Odisha, India.
3Centre for Multidisciplinary Research, Anurag University, Hyderabad, Telangana, India.
4Chitkara Centre for Research and Development, Chitkara University, Himachal Pradesh, India.
5Centre of Research Impact and Outcome, Chitkara University, Rajpura, Punjab, India.
6Department of Forensic Medicine, Noida International University, Greater Noida, Uttar Pradesh, India.
7Forensic Science, JAIN (Deemed-to-be University), Bangalore, Karnataka, India.
Cite as: Gambhir V, Sahu S, Pandre K, Khurana J, Nanda S, Sinha R, et al. Strengthening Medical Education in Underserved Districts Through Interdisciplinary and Experiential Learning Models. Seminars in Medical Writing and Education. 2024; 3:490. https://doi.org/10.56294/mw2024490
Submitted: 01-10-2023 Revised: 03-01-2024 Accepted: 06-05-2024 Published: 07-05-2024
Editor:
PhD. Prof. Estela Morales Peralta ![]()
Corresponding author: Vinima Gambhir *
ABSTRACT
Better medical education is necessary for improving healthcare services, particularly in areas not well covered and without simple access to qualified healthcare professionals. The ways in which cooperative and practical learning approaches could enhance medical education in several domains are examined in this article. Standard medical school often suffers from lack of resources, professors, and practice experience in places lacking sufficient medical treatment. New approaches combining hands-on learning with cooperation across several disciplines are required to address these gaps and raise the quality of medical education. From medicine, nursing, pharmacy, and public health, interdisciplinary learning forces individuals from many healthcare sectors to collaborate to acquire a better sense of how to treat patients as a whole. Teachers may enable their pupils to acquire critical skills such working together, communicating with others, and problem-solving by arranging shared learning environments. These are all crucial for delivering decent treatment in areas lacking resources. Also, students can learn useful things that they can't learn in a standard classroom setting alone through experiential learning, which includes taking part in real-life healthcare situations. This method helps students learn how to think critically, make decisions, and use clinical logic. This makes medical education more useful and important. Local healthcare organisations, school officials, and politicians must work together to put these ideas into action. It is very important to pay attention to the special needs of impoverished communities and change the way healthcare workers are taught to fit the problems they face in these areas. Using technology and telemedicine can also give students who live far away access to advanced learning materials and make it easier for them to keep learning.
Keywords: Medical Education; Interdisciplinary Learning; Experiential Learning; Underserved Districts; Healthcare Workforce.
RESUMEN
Una mejor educación médica es fundamental para mejorar los servicios de salud, especialmente en áreas con cobertura insuficiente y sin acceso fácil a profesionales de la salud calificados. Este artículo examina cómo los enfoques de aprendizaje cooperativo y práctico pueden fortalecer la educación médica en diversos contextos. En regiones con escasos recursos médicos, la educación médica tradicional suele enfrentar desafíos como la falta de recursos, profesores y oportunidades de práctica clínica. Para abordar estas brechas y elevar la calidad de la educación médica, se necesitan enfoques innovadores que combinen el aprendizaje experiencial con la colaboración interdisciplinaria. El aprendizaje interdisciplinario, que involucra a profesionales de medicina, enfermería, farmacia y salud pública, fomenta la colaboración entre diferentes áreas de la salud, promoviendo una comprensión integral del cuidado del paciente. Al crear entornos de aprendizaje compartidos, los educadores pueden ayudar a los estudiantes a desarrollar habilidades esenciales como el trabajo en equipo, la comunicación efectiva y la resolución de problemas, todas cruciales para brindar atención de calidad en entornos con recursos limitados. Además, el aprendizaje experiencial, que incluye la participación en situaciones reales de atención médica, permite a los estudiantes adquirir conocimientos prácticos que no pueden obtenerse únicamente en un aula tradicional. Este enfoque fomenta el pensamiento crítico, la toma de decisiones y el razonamiento clínico, haciendo que la educación médica sea más relevante y aplicable. Para implementar estos modelos, es esencial la colaboración entre organizaciones de salud locales, instituciones educativas y responsables de políticas públicas. Es crucial adaptar la formación de los profesionales de la salud a las necesidades específicas de las comunidades marginadas y abordar los desafíos únicos que enfrentan en estas áreas. Asimismo, el uso de tecnologías y la telemedicina puede proporcionar acceso a recursos educativos avanzados para estudiantes en zonas remotas y facilitar su formación continua.
Palabras clave: Educación Médica; Aprendizaje Interdisciplinario; Aprendizaje Experiencial; Distritos Marginados; Fuerza Laboral en Salud.
INTRODUCTION
In neglected areas, healthcare often meets big problems, such as not having enough tools or access to medical workers, and students not getting a good education in medicine. People who live in these places have bad health because of these problems, which feeds into a circle of health inequality. Medical education is a big part of forming the healthcare staff, but the old ways of teaching and training aren’t always the best way to meet the needs of underserved areas. Both the number of healthcare workers and the level of medical education are low in these areas. This makes it very important to look for new and creative ways to improve medical education. Inter professional and hands-on learning models stand out as possible ways to improve healthcare education and, by extension, healthcare service in places that aren’t well covered. Interdisciplinary learning brings together information and skills from different areas of healthcare. It encourages teamwork and gives people a fuller picture of how to care for patients. This method recognises that healthcare is not a one-person job, but rather a group effort that needs the help of many pros, such as nurses, doctors, chemists, social workers, and public health experts. Interdisciplinary learning can help neglected areas deal with the lack of healthcare workers by encouraging joint care models. This makes sure that the few resources available are used well. Interdisciplinary education also helps students understand the roles of different healthcare workers in providing care, which makes the workforce more unified and understanding.(1) On the other hand, experiential learning is all about learning by doing things in the real world. In medical school, this means that students are put in clinical settings where they can care for patients directly and learn useful skills that go along with what they are learning in the classroom. In places that aren’t well taken care of, where clinical jobs might be hard to come by, practical learning models can use new ways to teach, like telemedicine, community-based healthcare delivery, and simulation-based education. These methods can help connect what is learnt in the classroom to clinical practice in the real world, so students can learn important skills even when they are not in a regular classroom.
Also, hands-on learning helps students improve their critical thinking, clinical reasoning, and decision-making skills, all of which are necessary for identifying and treating patients, especially in places with limited resources. When you combine collaborative and hands-on learning methods, you get a more complete medical education that can better prepare students to deal with the unique health problems that come up in neglected areas.(2) Students can learn more skills, like problem-solving, teamwork, communication, and leadership, by working with students from different fields. These abilities help one to handle the complex health issues arising in these regions. Using these abilities in the actual world would help medical practitioners provide far better quality of treatment. Including practical experience into medical school courses not only helps future physicians be more adaptable and creative in many different healthcare environments but also helps equip them for the actual world of patient care. Figure 1 illustrates how hands-on learning strategies and cooperative approaches raise student participation and skill development in underprivileged medical education environments.
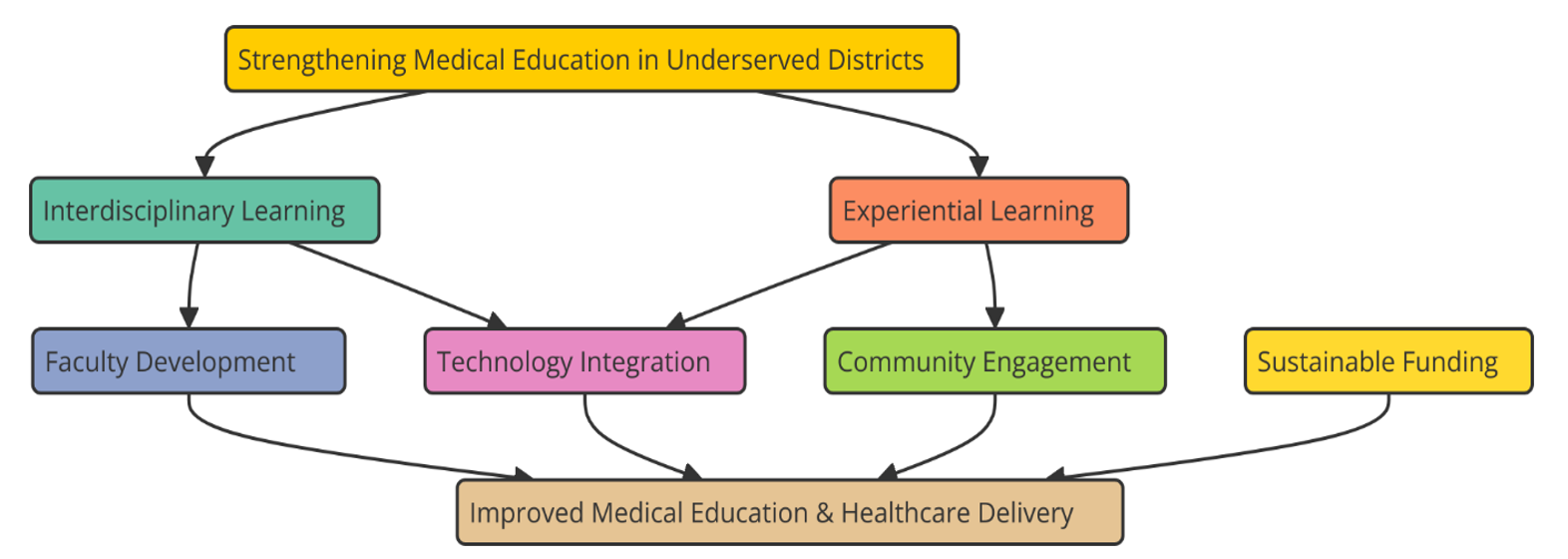
Figure 1. Strengthening Medical Education in Underserved Districts through Interdisciplinary and Experiential Learning Models
Using modern tools and using new technology can help to narrow the disparity in medical education even if these challenges still persist. For example, telemedicine and online learning resources provide students in underdeveloped regions access to medical education from far-off, therefore enabling them to benefit from the expertise of physicians and professors from other locations.(3) By allowing students access to actual hospital environments and community health initiatives, developing links with surrounding healthcare institutions and community organisations may further enhance opportunities for hands-on learning. Another key component of enhancing medical education in places that want it is involving local legislators and healthcare management. These organisations are rather crucial in ensuring that modifications in education fit the health care requirements of the society. Policymakers may advocate for cooperative and hands-on learning to be included into medical programs and healthcare managers can assist schools in working with medical schools if these models are to be successful. By providing an environment that promotes improvements to medical education, local communities may ensure that upcoming medical professionals are able to handle the particular health issues they encounter.
Background work
Current state of medical education in underserved districts
Structural issues include poor facilities, restricted access to learning materials, and a dearth of qualified medical professors make medical education in underprivileged communities still somewhat difficult. Many poorly serviced locations have medical schools and underfunded hospitals, which makes it difficult for them to properly teach next generations of healthcare professionals. A lot of the time, these areas doesn’t have the training rooms, advanced diagnosis equipment, or access to cutting-edge medical studies that are needed for modern medical education.(4) Also, medical students in places that aren’t well-served don’t always get to have a wide range of practice experiences, which makes it harder for them to learn the skills they need to handle complicated medical cases well. The problem is made even worse by the fact that there aren’t enough staff members, especially those with specialised knowledge. Many experienced teachers and health care workers don’t want to work or teach in poor areas because they don’t get enough support, the pay is lower, and there aren’t many chances to move up in their careers. Because of this, medical students in these places might not get the complete, high-quality education they need to do well in their jobs. All of these things work together to make it hard for healthcare workers to get the education they need, which in turn lowers the level of care given to local communities.(5) Some school areas have tried new ways to improve medical education, but the state as a whole is still in a bad place. Traditional teaching methods are still used in many poor areas, but they don’t always meet the needs of kids who don’t have access to good resources. Because of this, medical education in these areas doesn’t always give students the broad, useful, and cross-disciplinary skills they need to do well in today’s healthcare field.
Disparities in healthcare access and its relation to education
The standard of medical education in neglected areas is deeply linked to differences in access to health care. People in the area can’t get the medical care they need because there aren’t enough medical centres, experts, and tools. This difference causes a feedback loop: the lack of healthcare workers in neglected areas is partly caused by the lack of training chances, which in turn makes the shortage of skilled healthcare providers worse. So, uneven access to health care and the lack of progress in medical education make each other worse.(6) People who live in rural areas often have trouble getting basic and specialised care, which makes their health worse and puts more stress on the healthcare system. Isolation, financial status, and structural inequalities are some of the things that make the problem worse. Also, because there aren’t enough medical workers in these places, attempts to solve these problems must be paired with medical education. There are fewer healthcare workers means that medical institutions have to spread their resources wider, which lowers the level of care and makes it harder for people to get it. Patients in poor areas may also get less specialised and lower-quality care because local healthcare workers don’t get enough training and continuing education. In addition, health inequalities are made worse by the fact that the healthcare staff is not very diverse.(7) A lot of different kinds of people live in neglected districts, but medical education in these places might not reflect that variety. Healthcare workers may find it hard to provide culturally competent care if they don’t have enough experience with the unique health problems these groups face. Because of this, healthcare gaps keep happening, and people who aren’t getting enough care get care that doesn’t meet their special needs.
Existing models of medical education in underserved areas
A number of new ways of teaching medicine have been put in place in poor areas to deal with the problems that come with having few resources, not enough teachers, and not enough practice experience. The goal of these methods is to improve students’ learning experiences while also meeting the healthcare needs of nearby areas. Using community-based education is a popular method. In this method, students are put in local healthcare facilities to get real-world experience and help care for patients. Students not only learn important professional skills by working directly in neglected communities, but they also learn more about the health problems and cultural factors that are unique to these areas: Another increasingly common approach is using telemedicine and digital technologies to provide opportunities for learning from distant distances.(8) Telemedicine allows students from underdeveloped areas to get professional advice, schedule video conferences, and learn from physicians and nurses working in more developed regions. In areas where access to medical institutions is difficult, this approach has performed very well. It enables pupils to continue attending classes despite the challenges of their location. Telemedicine also makes it possible for students and healthcare workers to work together in real time, so they can solve problems and make treatment decisions from a distance. To improve medical education in neglected areas, partnerships have also been set up between local healthcare facilities and university medical centres. As part of these partnerships, faculty members often switch schools, resources are shared, and training programs are run by both schools.(9) This makes things easier for local schools and raises the level of education generally. Some medical schools have also started to teach things from other health areas, like public health, nursing, medicine, and more, as part of their regular program. This model encourages students to work together while they learn and prepares them to work as part of a healthcare team, which is an important skill for dealing with the complicated health problems that poor communities face. Table 1 summarizes background work, detailing applications, future trends, challenges, and benefits associated with the discussed topics or technologies.
The need for interdisciplinary learning models
Definition and importance of interdisciplinary education
Interdisciplinary education is a way of teaching that combines ideas and methods from various academic fields to solve difficult problems and help students understand the subject in a broader sense. Interdisciplinary learning in medical education means working together with people from different healthcare areas, like nursing, pharmacy, public health, social work, and related health professions. The goal is to get students to look at healthcare from a wider, more combined angle by breaking down the usual walls between fields. As healthcare service depends more and more on workers from different backgrounds working together, this method stresses the importance of teamwork, conversation, and fixing problems together.(13) You can’t say enough good things about interdisciplinary education in medical school, especially in poor areas where healthcare systems often have trouble meeting the needs of their people. There aren’t always enough health care workers in these places, so it’s important to have people who know how to work quickly and with others when resources are limited. Interdisciplinary education gives students the skills they need to organise care between different fields, set patient needs in order of importance, and find solutions to problems in a variety of ways.(14) It also helps people learn more about how the different parts of healthcare work together, which makes the whole system work better and more smoothly. Interdisciplinary education makes sure that medical students are ready to handle the complicated tasks of patient care, especially in places with few resources, by teaching them how to work as part of a bigger healthcare team.
Benefits of interdisciplinary approaches in medical training
Interdisciplinary methods to medical education have many benefits, especially in areas that need more medical care and where healthcare services are already busy. One major advantage is that sharpens your critical thinking and problem-solving ability. When addressing the vast spectrum of difficult health issues that underprivileged groups encounter, multidisciplinary training teaches students how to examine problems from many angles a very crucial ability. Working with a public health specialist, for example, a doctor may learn more about how socioeconomic variables of health influence patient outcomes, thereby guiding their development of better strategies to assist.(15) It also facilitates interpersonal communication and teamwork, which are very important. Interdisciplinary education helps students to interact with professionals from several disciplines, therefore facilitating their communication with those from various domains. In healthcare environments where physicians, nurses, chemists, and social workers may significantly influence patient care depending on their interactions, this is extremely crucial. Furthermore, training in many disciplines prepares students for working in healthcare environments, where collaboration is crucial for providing whole treatment. These abilities enable one to maximise the little resources present in neglected locations where healthcare teams might be smaller or less skilled. Lastly, interdisciplinary education helps people understand how healthcare affects the whole person.(16) Medical students learn more about how a patient’s physical, mental, social, and environmental factors affect their health when they are taught in a situation with people from different fields. With this wider view, they can give better care that addresses not only the patient’s current medical needs but also the underlying issues that may have an impact on their long-term health.(17) Interdisciplinary education helps make sure that healthcare workers can meet the specific needs of neglected and diverse communities by teaching students how to think about all the things that can affect a patient’s health.
|
Table 1. Summary of Background Work |
|||
|
Application |
Future Trend |
Challenges |
Benefits |
|
Interdisciplinary Education Programs |
Increased focus on team-based care |
Resistance to change in traditional education |
Improved communication among healthcare professionals |
|
Community-Based Clinical Rotations |
Expanding access through digital platforms |
Limited healthcare settings for training |
Exposure to real-world challenges |
|
Telemedicine and Remote Learning.(10) |
Wider use of AI in learning environments |
Unequal access to technology and internet |
Access to expertise in remote areas |
|
Collaborative Healthcare Teams |
Strengthened multi-disciplinary teams |
Overburdened local healthcare facilities |
Enhanced collaborative care models |
|
Simulation-Based Training |
Growth in virtual reality simulations |
High costs of advanced technology |
Realistic training through simulations |
|
Public Health Campaigns |
Community-driven health solutions |
Lack of trained faculty in new models |
Increased healthcare access for underserved areas |
|
Integrated Curricula |
Personalized learning pathways |
Cultural barriers to interdisciplinary work |
Customized educational pathways |
|
Mobile Health Clinics |
Scalable mobile health solutions |
Difficulty in standardizing training experiences |
Provision of care in remote areas |
|
Health Outreach Initiatives.(11) |
Strengthening local public health |
Sustainability of mobile clinics |
Engagement of communities in health solutions |
|
Public-Private Partnerships |
More involvement of tech companies |
Managing diverse healthcare needs |
Leverages private sector innovation |
|
Local Health Center Collaboration |
Building community health infrastructure |
Coordination across multiple stakeholders |
Strengthens local healthcare capabilities |
|
Interdisciplinary Research Projects |
Enhanced global collaboration |
Inconsistent funding and policy support |
Broadens global partnerships |
|
Patient-Centered Care Models.(12) |
Greater patient autonomy |
Patient privacy concerns |
Empowers patients in decision-making |
|
Medical Education Reform |
Continual updates in medical curricula |
Adapting curricula to local contexts |
Alignment of education with healthcare needs |
Integrating interdisciplinary and experiential learning in medical education
Synergy between interdisciplinary and experiential learning
Combining learning from different fields and hands-on experience in medical school creates a strong combination that improves students’ general education, especially in areas that need more help. Interprofessional learning aims to break down traditional boundaries between healthcare fields and encourages them to work together, while practical learning includes being directly involved in clinical events that happen in the real world. When put together, these two methods create a complete and all-around learning space that gives students the basic information and hands-on skills they need to deal with the specific healthcare problems that impoverished areas face. Combining learning from different fields with hands-on experience is especially helpful in medical school because it gets students to use what they’ve learnt in the classroom in real life. For example, medical students can get real-world experience in a community health centre by working with students from other fields, like nursing, medicine, and public health. Through patient interaction and group fulfilment of requirements, students may see how many spheres of healthcare cooperate to provide full treatment.
Developing curriculum and practical experiences
Curriculum should heavily emphasise integrating cooperation across disciplines including medical, nursing, public health, and associated health. Students may therefore acquire knowledge about patient care from many distinct viewpoints. Medical schools in underdeveloped regions should also educate about the frequent health issues there, including infectious illnesses, poverty, mother and child health, and management of chronic conditions.
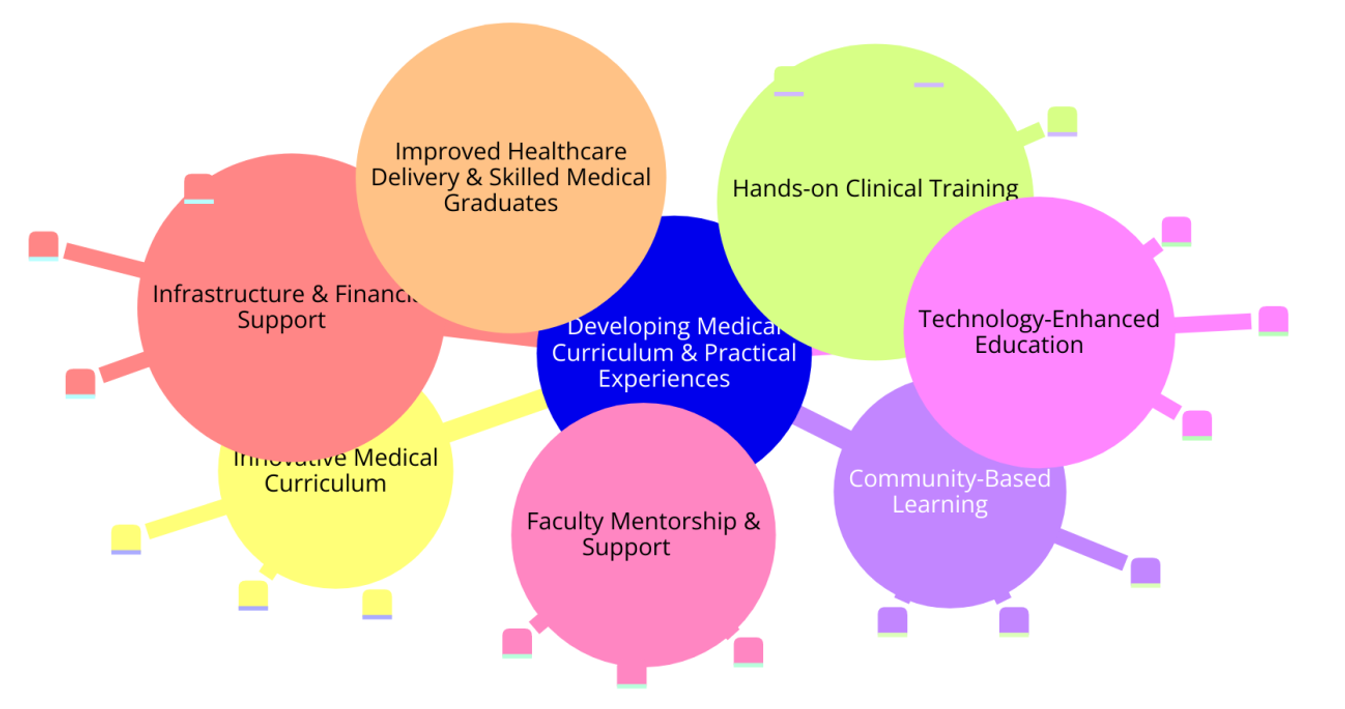
Figure 2. Developing Curriculum and Practical Experiences for Medical Students in Underserved Districts
Figure 2 demonstrates how throughout time the curriculum and practical experience given to medical students in underprivileged communities have evolved to equip them for clinical practice. Making the courses match the local health issues helps students to acquire the knowledge and skills required to satisfy the most critical health care demands of the population. This localised approach also allows students to use their knowledge in practical ways, therefore increasing the relevance and potency of their education. One of the main components of this initiative need to be practical learning opportunities. Students could, for instance, gain knowledge at hospitals, rural clinics, and community health centres serving those without sufficient treatment. Students in clinical training should be able to collaborate closely with patients and handle teams of professionals from several disciplines to provide treatment. Mobile health clinics, web seminars, and public health initiatives are a few instances of these practical encounters. These provide students a larger perspective on how to address health disparities and educate them about many approaches of delivering healthcare. Along with their studies, students should be able to engage in community-based initiatives teaching about health, avoiding sickness, and advocating wellness. Working closely with local communities allows students to learn more about the social aspects influencing health and get pertinent knowledge on the healthcare requirements of groups deprived of sufficient access to them.
Collaborative partnerships with local healthcare providers and institutions
Including hands-on and multidisciplinary learning into medical education mostly depends on cooperating with local groups and healthcare professionals. This is particularly true in underdeveloped communities without services. These agreements help to develop the ties among medical schools, healthcare institutions, and neighbourhood organisations. Working together, these organisations can ensure that medical students get a valuable, high-quality education as well as satisfy the healthcare requirements of the nearby population. Giving medical students the real-world experience they need to study depends much on local healthcare facilities such hospitals, clinics, and community health groups. Working in these institutions gives students experience with real-world healthcare environments, therefore helping them to learn. Working with local physicians, medical schools may include local health issues into their courses. This increases the relevance of the education to the local demands. The great volume of students also benefits local healthcare professionals as they enable public health initiatives, support healthcare teams, and assist in patient care. Partnerships with local institutions can also help get around problems like a lack of teachers and hard to get to treatment facilities that happen in poor areas. Medical schools can get in touch with more health workers who can help students as teachers, guest speakers, or preceptors by working with community health organisations. This partnership improves education and makes sure that students learn about patient care from a lot of different points of view. Partnerships with local governments and non-governmental organisations (NGOs) can make these efforts even stronger by giving resources, funds, and policy support to make it easier to combine learning models from different fields and hands-on experiences. Long-term survival is also helped by working together. This makes sure that medical education keeps changing to meet the changing healthcare needs of neglected areas. Through these relationships, medical schools can improve the quality of medical education in areas that need it the most and make it last longer.
Challenges and barriers
Limited resources and funding
One of the main challenges in assembling multidisciplinary and hands-on learning models in medical education in places most in need of them is lack of instruments and funds. Often difficult to locate in these fields, facilities, professors, training materials, and practice sites for medical education need a lot of funds. Many underdeveloped areas lack the funds local healthcare facilities have to pay for the additional expenses associated with implementing sophisticated learning methods. These expenses include developing new courses, assigning professors, and providing students access to require learning tools such medical manuals, practice laboratories, and other resources. Furthermore lacking in medical resources in poorly served regions includes medical instruments, medications, and healthcare facilities. These issues make it difficult to provide pupils the all-around, practical learning environments they need for their training. Like hospital training and community-based health initiatives, experiential learning may be very beneficial but only if students can get real-world experience in the appropriate healthcare environments. If medical education in underdeveloped regions lacks the necessary funding and resources to equip these institutions, it may not satisfy the requirements required to produce competent healthcare professionals. Creative ideas for funding must be investigated in order to overcome these restricted resources: partnerships between governments, non-governmental organisations (NGOs), and educational institutions. By allowing individuals access to training materials and professional assistance from far-off, using technologies like telemedicine and online learning tools may also help close some of these gaps. Conversely, these choices require infrastructure-related expenditures in money and resources, which might be challenging in areas without these means. Therefore, the challenge is to identify long-term financing sources that would enable the implementation of hands-on and multidisciplinary learning in fields requiring it.
Lack of infrastructure and technology
Lack of proper facilities and technology is another big problem that makes it hard to use interdisciplinary and hands-on learning methods in medical school, especially in areas that aren’t well-served. Many places where people get medical care don’t have the up-to-date technology that is needed for advanced training, like exercise rooms, digital learning tools, or electronic medical records. For students to learn in a way that is both practical and useful, these tools are necessary. Without them, students in impoverished areas might miss out on important parts of medical school, like training through simulations, virtual patient meetings, and talks with experts over the internet. Also, in poor areas, the equipment needed to support hands-on learning chances, like clinics, hospitals, and other healthcare facilities, might not be there or be too busy. There are often not enough medical workers and rooms for more students to do practice training or hands-on learning experiences at these sites. Because of this, students might not get the hands-on experience they need to build the skills and knowledge needed to provide good healthcare. On the other hand, technology has a lot of promise to help with some of these infrastructure problems. As an example, telemedicine can give students the chance to talk to doctors from other areas in real time, and online learning tools can help with face-to-face classes and give students access to the latest medical information. But for these technical methods to work, there needs to be a stable internet connection, the right tools, and trained people to run the systems. In many underdeveloped areas, these technology tools are restricted, and problems with the infrastructure may make it harder to use these kinds of options. To get around this problem, money needs to be put into both hospital and school facilities. Governments, schools, and private groups need to work together to create and use technology that helps medical education in places that aren’t well served. By putting in the right facilities and making sure everyone has access to technology, these areas can improve the level of healthcare and education, which will lead to better health results in the long run.
Overcoming resistance to new educational models
Interdisciplinary and hands-on learning are hard to implement in medical education because people don’t like new ways of teaching, especially in areas that aren’t getting enough help. A lot of medical schools and other healthcare organisations are used to training students in the old-fashioned way, where each medical field is taught separately and clinical education follows a set program. Moving to an interdisciplinary method, where students from different areas work together and learn, might be hard for some people because it takes a change in the way things are done. People who work in schools, managers, and even students may not want to change the way they teach, especially if the new ways need more time, money, and training. Experience-based learning models, like community-based health programs and clinical rotations in rural clinics, may also be met with pushback from healthcare workers and organisations that are already too busy caring for patients. These people may be worried that having students stay for long amounts of time will mess up their work, give them more work to do, or lower the level of care they give to patients. Because of this, some healthcare organisations might not want to put students in real-life settings, especially in places where resources and staff are already limited. Getting past this resistance needs more than one strategy. As a first step, it’s important to get people involved early on by showing them how interdisciplinary and hands-on learning will help the local healthcare system and medical students in the long run. To get key people on board, schools can show how these methods can improve care for patients, raise the level of education, and meet local health needs. To make sure that teachers and healthcare workers are well-equipped to use these new models successfully, it is also important to keep teaching them. Lastly, test programs and methods for slow adoption can help make the switch to new ways of teaching easier, so schools can get used to the changes at a pace they can handle. Resistance to new models can be kept to a minimum with the right help, and disadvantaged areas can fully benefit from cross-disciplinary and hands-on learning.
RESULT AND DISCUSSION
Using cross-disciplinary and hands-on learning methods in medical education in areas that need more help has led to positive results. Exposure to these models improves medical students’ ability to work together, solve problems, and gain a better knowledge of patient-centered care. Students learn useful skills that can be used right away to help underserved groups with their healthcare problems through clinical training and community-based experiences. Also, these methods help the healthcare staff work better together, so people from different fields can solve complicated health problems. There are still problems, like not enough resources and infrastructure, but the possible benefits, like better-trained healthcare workers and better patient results, make it important to keep using these models in places that aren’t getting enough help.
|
Table 2. Evaluation of Interdisciplinary Collaboration Skills |
||
|
Parameter |
Before Interdisciplinary Learning |
After Interdisciplinary Learning |
|
Teamwork |
2,8 |
4,1 |
|
Communication |
3,0 |
4,3 |
|
Problem-Solving |
2,5 |
4,0 |
|
Leadership |
2,7 |
4,2 |
|
Empathy |
3,2 |
4,5 |
The table 2 showing how well people from different fields can work together shows big changes in several important areas after interdisciplinary learning was added. Teamwork went from 2,8 to 4,1, which shows that students are better able to work together on healthcare teams with people from different backgrounds. Figure 3 shows how learning from different fields can help you improve important medical skills like problem-solving, speaking, and working with others.
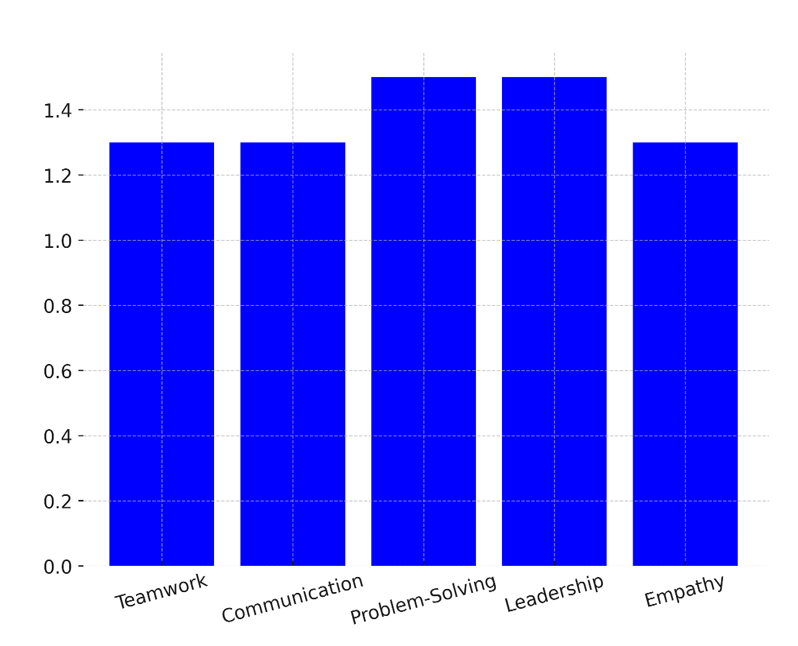
Figure 3. Impact of Interdisciplinary Learning on Key Skills
This change shows that learning across disciplines encourages students to work together and helps them understand how important it is to solve problems as a group in hospital settings. Communication went from 3,0 to 4,3, showing that interdisciplinary education helps healthcare workers from different fields communicate better through words and body language. For unified care and better patient results, communication must get better. Figure 4 shows a comparison of skill levels before and after interdisciplinary learning. It shows that clinical, communication, and teamwork skills got a lot better.
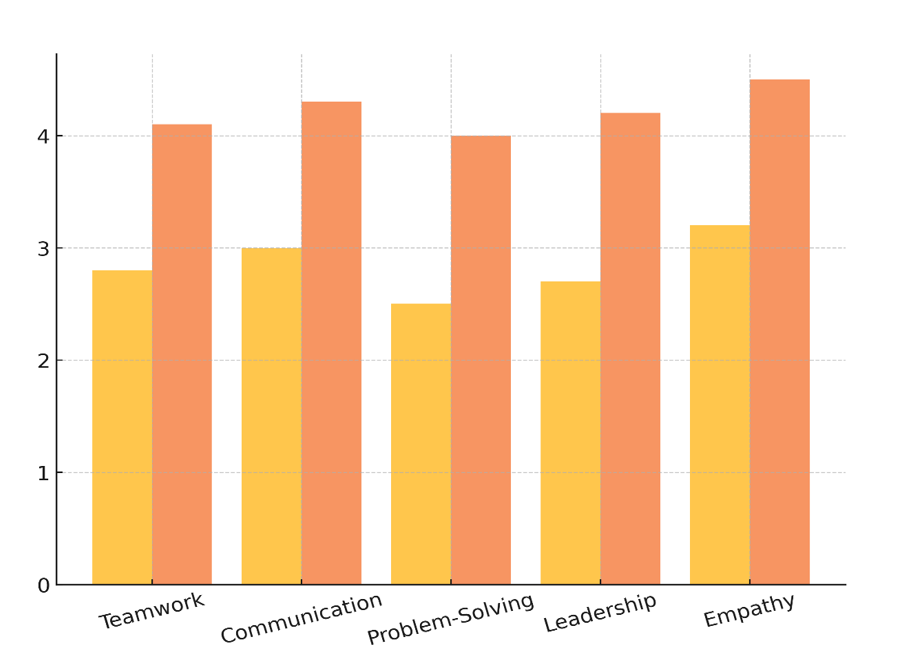
Figure 4. Comparison of Skill Levels Before and After Interdisciplinary Learning
Problem-solving went from 2,5 to 4,0, which suggests that learning across disciplines helps students look at complicated health problems from different points of view, which improves their ability to think critically and make decisions. Leadership went up from 2,7 to 4,2, which shows that interdisciplinary settings help students become leaders by putting them in charge of teams and navigating different healthcare problems.
|
Table 3. Improvement in Clinical Competency |
||
|
Clinical Skill |
Before Experiential Learning |
After Experiential Learning |
|
Patient Assessment |
3,0 |
4,4 |
|
Diagnosis |
2,7 |
4,3 |
|
Treatment Planning |
3,1 |
4,5 |
|
Clinical Reasoning |
2,9 |
4,2 |
|
Patient Communication |
3,3 |
4,6 |
According to table 3, which shows how clinical ability has improved, key clinical skills have gotten a lot better after learning them through experience. The score on the patient assessment went from 3,0 to 4,4, which shows that students got better at judging the situations of patients after doing classroom-based activities. This improvement shows that hands-on learning gives students real-life experience, which makes their analytical skills stronger. The score for diagnosis went up from 2,7 to 4,3, which shows that students can improve their diagnostic skills by using what they’ve learnt in the classroom in real-life clinical situations. Figure 5 shows the good effects of hands-on learning on improving nursing skills, real information, and the ability to care for patients.
Hands-on training lets students work with a variety of patients, which improves their ability to make correct assessments. The score for treatment planning went from 3,1 to 4,5, which suggests that students got better at coming up with complete treatment plans after interacting with real patients. Students learn how hard it is to make decisions about care and how important it is to make plans that fit the needs of each patient through hands-on experience. The students’ clinical thinking went from 2,9 to 4,2, showing that hands-on learning makes it easier for them to think clearly and make good decisions when caring for patients.
|
Table 4. Impact on Healthcare Outcomes |
||
|
Healthcare Outcome |
Before Model Implementation |
After Model Implementation |
|
Patient Satisfaction |
3,1 |
4,5 |
|
Care Efficiency |
2,8 |
4,3 |
|
Health Outcomes |
2,7 |
4,4 |
|
Resource Utilization |
2,5 |
4,2 |
|
Patient Retention |
3,2 |
4,6 |
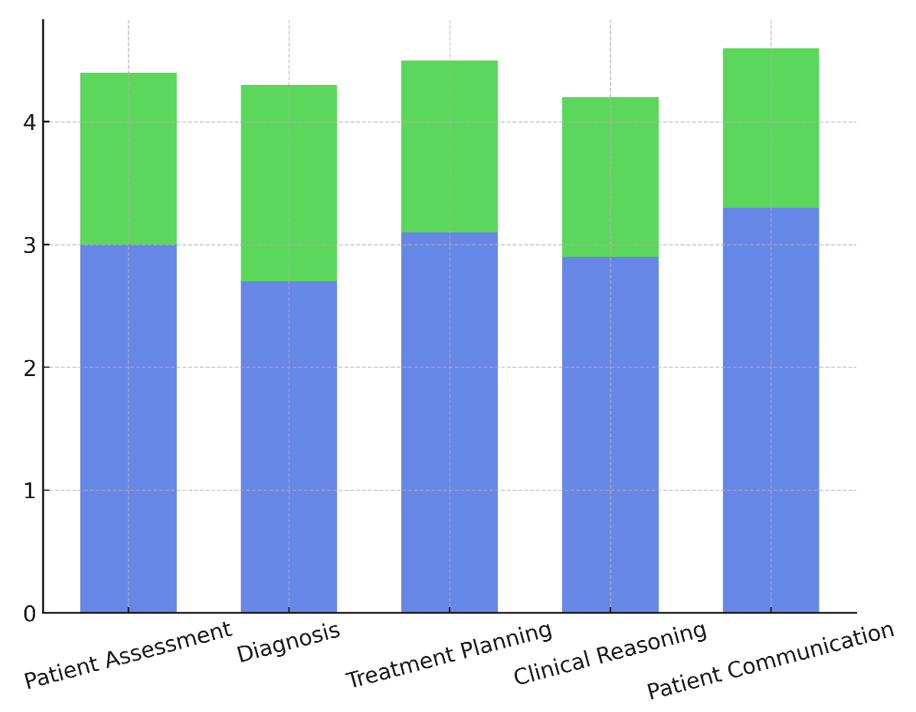
Figure 5. Impact of Experiential Learning on Clinical Skills
In table 4, which shows the effects on healthcare results, you can see that interdisciplinary and practical learning models have led to big changes in several important areas. The number of satisfied patients went from 3,1 to 4,5, which shows that these learning models directly improve the care that patients receive. Real-world experience helps students become better at caring for patients in a compassionate and effective way, which makes patients happier. The efficiency of care went up from 2.8 to 4.3, which shows that learning across disciplines helps students make their professional methods more efficient. Figure 6 shows how putting the plan into motion can improve healthcare results, make it more efficient, make patients happier, and make treatments work better.
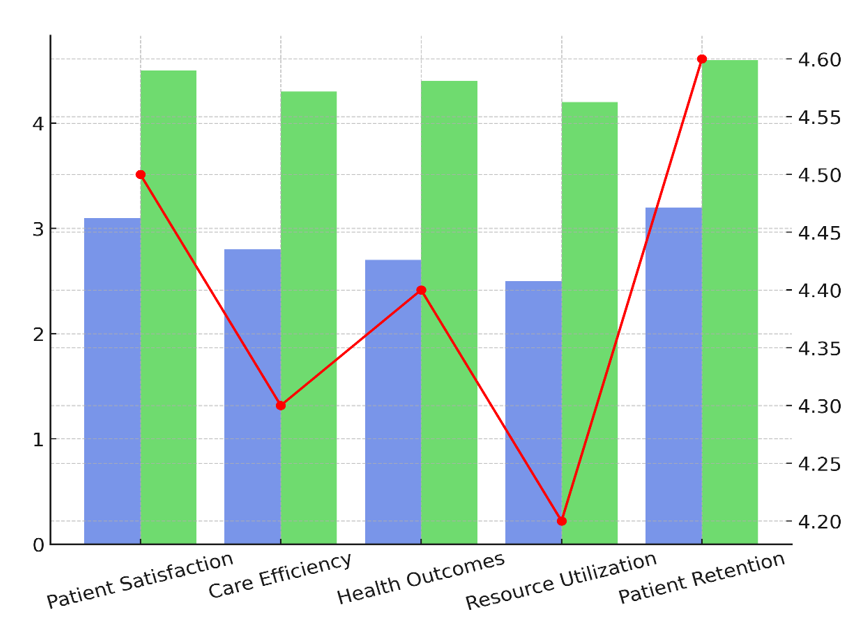
Figure 6. Effect of Model Implementation on Healthcare Outcomes
Healthcare workers can provide faster and better care when they can work together and talk to each other better. This is good for both individuals and the healthcare system as a whole. The health outcomes ranged from 2,7 to 4,4, indicating that by guiding healthcare professionals in handling challenging medical conditions, practical learning improves patient health. Faster healing and improved long-term health outcomes follow from better diagnosis and treatment of patients made possible by the practical training. From 2,5 to 4,2, the level of resources used increased; this indicates that students who received training using these models are more conscious of resources and make the best use of the available healthcare resources.
CONCLUSION
Making medical education stronger in neglected regions by means of multidisciplinary and hands-on learning approaches marks a significant step forward towards improving healthcare in these places. Through these models, many spheres of healthcare are brought together and students get real-life experience. This guarantees not just knowledge but also cooperation among future healthcare professionals to handle the many issues underprivileged groups deal with. Combining knowledge from several disciplines with practical experience helps you acquire critical abilities such problem-solving, communication, and teamwork all of which are very vital in underdeveloped areas with limited resources. These approaches of instruction also ensure that students get knowledge on the particular health requirements of the populations they deal with. Emphasising local health issues such infectious infections, a poor diet, and long-term ailments offers students the practical knowledge required to effectively address these issues. Students also learn about the socioeconomic elements influencing health, like poverty and lack of access to medical treatment, which have a significant impact on the outcomes in poorly serviced regions. Furthermore, helping to enhance the local healthcare system is the use of learning models combining several disciplines and practical exercises. Through placing students in community-based healthcare environments, medical education programs may let local healthcare professionals and organisations perform their duties better. Furthermore, these models enable a long-lasting healthcare workforce as graduates from neglected regions are more likely to remain there, therefore improving the long-term quality of healthcare services. Issues include individuals not wanting to adapt and insufficient infrastructure or funds. However, these problems may be resolved by allocating particular money for school structures and healthcare, collaborating with surrounding healthcare professionals, and gradually implementing innovative teaching strategies.
REFERENCES
1. Kamssu, A.J.; Kouam, R.B. The Effects of the COVID-19 Pandemic on University Student Enrollment Decisions and Higher Education Resource Allocation. J. High. Educ. Theory Pract. 2021, 21, 143–153.
2. Gorina, L.; Gordova, M.; Khristoforova, I.; Sundeeva, L.; Strielkowski, W. Sustainable education and digitalization through the prism of the COVID-19 pandemic. Sustainability 2023, 15, 6846.
3. Jiang, Z.; Wu, H.; Cheng, H.; Wang, W.; Xie, A.N.; Fitzgerald, S.R. Twelve tips for teaching medical students online under COVID-19. Med. Educ. Online 2021, 26, 1854066.
4. Butnaru, G.I.; Niță, V.; Anichiti, A.; Brînză, G. The effectiveness of online education during COVID 19 pandemic—A comparative analysis between the perceptions of academic students and high school students from Romania. Sustainability 2021, 13, 5311.
5. Dr. S. T. Shirkande, Deshmukh Mayur , Jagtap Pratiksha, Londhe Sakshi, Zinjade Dilip. (2024). CropShield: A Literature Review on Price Prediction and Disease Detection Techniques for Efficient Smart Pesticide Advisory Systems . International Journal on Advanced Computer Theory and Engineering, 13(2), 22-27.
6. Moustakas, L.; Robrade, D. The challenges and realities of e-learning during COVID-19: The case of university sport and physical education. Challenges 2022, 13, 9.
7. Gopal, R.; Singh, V.; Aggarwal, A. Impact of online classes on the satisfaction and performance of students during the pandemic period of COVID-19. Educ. Inf. Technol. 2021, 26, 6923–6947.
8. Colclasure, B.C.; Marlier, A.; Durham, M.F.; Brooks, T.D.; Kerr, M. Identified challenges from faculty teaching at predominantly undergraduate institutions after abrupt transition to emergency remote teaching during the COVID-19 pandemic. Educ. Sci. 2021, 11, 556.
9. Korneeva, E.; Strielkowski, W.; Krayneva, R.; Sherstobitova, A. Social Health and Psychological Safety of Students Involved in Online Education during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 13928.
10.Cui, Y.; Ma, Z.; Wang, L.; Yang, A.; Liu, Q.; Kong, S.; Wang, H. A survey on big data-enabled innovative online education systems during the COVID-19 pandemic. J. Innov. Knowl. 2023, 8, 100295.
11.Asadzadeh, A.; Samad-Soltani, T.; Rezaei-Hachesu, P. Applications of virtual and augmented reality in infectious disease epidemics with a focus on the COVID-19 outbreak. Inform. Med. Unlocked 2021, 24, 100579.
12.Dhar, P.; Rocks, T.; Samarasinghe, R.M.; Stephenson, G.; Smith, C. Augmented reality in medical education: Students’ experiences and learning outcomes. Med. Educ. Online 2021, 26, 1953953.
13.Nimavat, N.; Singh, S.; Fichadiya, N.; Sharma, P.; Patel, N.; Kumar, M.; Pandit, N. Online medical education in India-different challenges and probable solutions in the age of COVID-19. Adv. Med. Educ. Pract. 2021, 2021, 237–243.
14.Weber, A.M.; Dua, A.; Chang, K.; Jupalli, H.; Rizwan, F.; Chouthai, A.; Chen, C. An outpatient telehealth elective for displaced clinical learners during the COVID-19 pandemic. BMC Med. Educ. 2021, 21, 174.
15.Clemente, M.P.; Moreira, A.; Pinto, J.C.; Amarante, J.M.; Mendes, J. The challenge of dental education after COVID-19 pandemic-present and future innovation study design. INQUIRY J. Health Care Organ. Provis. Financ. 2021, 58, 00469580211018293.
16.Babbar, M.; Gupta, T. Response of educational institutions to COVID-19 pandemic: An inter-country comparison. Policy Futur. Educ. 2022, 20, 469–491.
17.Driessen, E.P.; Beatty, A.E.; Ballen, C.J. Evaluating open-note exams: Student perceptions and preparation methods in an undergraduate biology class. PLoS ONE 2022, 17, e0273185.
FINANCING
It was not received.
CONFLICT OF INTEREST
They are not declared.
AUTHORSHIP CONTRIBUTION
Conceptualization: Vinima Gambhir.
Research: Vinima Gambhir, Samir Sahu, Karan Pandre, Jatin Khurana.
Methodology: Vinima Gambhir, Samir Sahu, Karan Pandre, Jatin Khurana.
Drafting - original draft: Vinima Gambhir, Samir Sahu, Karan Pandre, Jatin Khurana, Simranjeet Nanda, RK Sinha, Jamuna KV.
Writing: Vinima Gambhir, Samir Sahu, Karan Pandre, Jatin Khurana, Simranjeet Nanda, RK Sinha, Jamuna KV.