doi: 10.56294/mw2024494
ORIGINAL
Analyzing the Effectiveness of Virtual Reality in Medical Training and Patient Communication
Análisis de la eficacia de la realidad virtual en la formación médica y la comunicación con el paciente
Yuvraj Parmar1 ![]() *,
Siddharth Sriram2
*,
Siddharth Sriram2 ![]() , Amit Vassney3
, Amit Vassney3 ![]() , Naresh Kaushik4
, Naresh Kaushik4 ![]() , Sarita Mohapatra5
, Sarita Mohapatra5 ![]() , Mittapalli Premchand6
, Mittapalli Premchand6 ![]()
1Chitkara Centre for Research and Development, Chitkara University. Himachal Pradesh, India.
2Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
3Department of Medicine, Noida International University. Greater Noida, Uttar Pradesh, India.
4Department of uGDX, ATLAS SkillTech University. Mumbai, Maharashtra, India.
5Department of Computer Applications, Siksha ‘O’ Anusandhan (Deemed to be University). Bhubaneswar, Odisha, India.
6Centre for Multidisciplinary Research, Anurag University. Hyderabad, Telangana, India.
Cite as: Parmar Y, Sriram S, Vassney A, Kaushik N, Mohapatra S, Premchand M. Analyzing the Effectiveness of Virtual Reality in Medical Training and Patient Communication. Seminars in Medical Writing and Education. 2024; 3:494. https://doi.org/10.56294/mw2024494
Submitted: 06-10-2023 Revised: 08-01-2024 Accepted: 11-05-2024 Published: 12-05-2024
Editor:
PhD. Prof. Estela Morales Peralta ![]()
Corresponding Author: Yuvraj Parmar *
ABSTRACT
A game-changing technology in medicine, virtual reality (VR) might enable physicians to pick up fresh skills and improve their patient communication. Using VR in medical education generates realistic experiences that help medical professionals learn by doing in a regulated environment. Professionals and students may mimic difficult operations and apply therapies using this technology. Learning more about the human body also aids in their development of skills and improves their decision-making. Since VR allows physicians explain medical issues, treatment plans, and procedures in enjoyable and engaging ways that let patients comprehend and follow through, it is also rather vital for doctors interacting with patients. Two key uses for VR are teaching physicians and enabling patients to communicate with one another; this article explores both uses. Regarding medical training, we examine how VR models enable medical students practice again and over in real-world scenarios and assist in learning and memory of operations. Especially for patients with complex diseases, adopting VR to visualise medical concepts in 3D is a major step forward from the past approaches of interacting with patients. Virtual environments help patients be happy and less stressed as they simplify the understanding of how treatments operate. The research examines present VR usage as well as potential future applications for both hospitals and educational institutions. According to many case studies, virtual reality (VR) not only improves patient-provider interactions but also aids in more effective learning. For many individuals, however, issues like cost, simplicity of access, and restricted technology still make usage difficult. Improvements in VR technology—that which makes VR more affordable and user-friendly may help to address these issues going forward. This would enable VR use in medicine much further.
Keywords: Virtual Reality; Medical Training; Patient Communication; Medical Education; Healthcare Technology.
RESUMEN
La realidad virtual (RV), una tecnología revolucionaria en medicina, podría permitir a los médicos adquirir nuevas habilidades y mejorar su comunicación con los pacientes. El uso de la RV en la formación médica genera experiencias realistas que ayudan a los profesionales de la medicina a aprender haciendo en un entorno regulado. Profesionales y estudiantes pueden imitar operaciones difíciles y aplicar terapias utilizando esta tecnología. Aprender más sobre el cuerpo humano también ayuda a desarrollar sus habilidades y mejora su toma de decisiones. Dado que la RV permite a los médicos explicar cuestiones médicas, planes de tratamiento y procedimientos de forma amena y atractiva para que los pacientes los comprendan y los sigan, también es bastante vital para los médicos en su interacción con los pacientes. Dos usos clave de la RV son la formación de los médicos y la comunicación entre los pacientes. En cuanto a la formación médica, examinamos cómo los modelos de RV permiten a los estudiantes de medicina practicar una y otra vez en escenarios del mundo real y ayudan en el aprendizaje y la memoria de las operaciones. Especialmente en el caso de pacientes con enfermedades complejas, la adopción de la RV para visualizar conceptos médicos en 3D supone un gran avance respecto a los enfoques anteriores de interacción con los pacientes. Los entornos virtuales ayudan a los pacientes a estar contentos y menos estresados, ya que simplifican la comprensión del funcionamiento de los tratamientos. La investigación examina el uso actual de la RV, así como sus posibles aplicaciones futuras tanto en hospitales como en instituciones educativas. Según muchos estudios de casos, la realidad virtual (RV) no sólo mejora las interacciones entre pacientes y proveedores, sino que también ayuda a un aprendizaje más eficaz. Para muchas personas, sin embargo, cuestiones como el coste, la sencillez de acceso y la tecnología restringida siguen dificultando su uso. Las mejoras en la tecnología de la RV, que la hacen más asequible y fácil de usar, pueden ayudar a resolver estos problemas en el futuro. De este modo, la RV podría utilizarse mucho más en medicina.
Palabras clave: Realidad Virtual; Formación Médica; Comunicación con el Paciente; Educación Médica; Tecnología Sanitaria.
INTRODUCTION
Over the last 10 years, the technology behind virtual reality (VR) has advanced and changed several sectors, including healthcare. In the field of medicine, VR has showed great potential as a means of enhancing medical training and facilitating patient contact. VR allows patients and medical professionals encounter fictitious worlds that would be difficult or impossible to create as it is strong, interactive, and fascinating. This is why it is employed increasingly in healthcare environments, hospitals, and classrooms. This article examines how well virtual reality (VR) may be used for patient communication and medical education. It considers how it may support patient involvement, procedural training, and skill development. Long emphasising theory, research, and living experiences to educate those aspiring to work in the healthcare what they need to know, medical school has long been centred on Although these techniques have proven successful in the past, they do not always provide individuals with the practical knowledge required to become technically competent and make wise judgements in the future. Virtual reality allows medical students to experience imagined occurrences akin to actual ones, therefore addressing this issue. With VR simulators, professionals and students may rehearse treatments, medical procedures, and evaluations in a controlled environment. This not only reduces the possibility of errors in the actual world but also aids in memory, learning how to do things, and confidence building during demanding tasks. One of the nicest things about utilising VR to teach physicians is that it may replicate unusual or risky medical scenarios they would not see in real life.
Virtual worlds allow therapies involving uncommon illnesses, complex anatomy, or odd difficulties to be recreated. This allows physicians to learn handling these sorts of situations free from concern about what could transpires in real life. By repeatedly running similar scenarios in VR, trainees may hone their abilities and prepare ready for the erratic character of actual practice. VR also allows students to practice at their own pace, which enables the provision of customised courses fit for various learning environments and speeds. VR helps patients communicate with one another better, not just helps physicians be trained. Concerning complex or innovative medical procedures, traditional approaches of informing patients about medical concerns and treatment options depend on talking, writing, or 2D visuals, which might be difficult for patients to completely grasp.(1) Virtual reality makes these concepts simpler to grasp and more potent for expression by presenting them in 3D, dynamic, and immersive environments. When patients can visualise medical procedures, bodily components, and treatment plans, they are more suited to grasp their circumstances and the options they have. This not only makes them wiser but also helps them to feel more in control of the medical decisions they choose. Those scheduled for surgery, for instance, may see what the procedure will be like virtually before it takes place. Patients and healthcare professionals may benefit from this realistic experience in terms of reduced anxiety, greater trust, and more efficient team work.(2) Knowing what to anticipate from their therapy helps patients to be satisfied with it and increase their likelihood of following their doctor's advice, therefore enhancing the outcome of their treatment. For those with cognitive issues such as dementia who find it difficult to grasp complex medical information the traditional manner, virtual reality (VR) may also be very beneficial. VR makes education simpler to grasp and more fascinating, therefore linking patients and healthcare professionals. This will help to prioritise the patient and enhance communication. While VR has numerous advantages, its implementation in medical education and patient engagement may be challenging. Because VR technology is costly, you need specific equipment, and you may have to learn how to use VR tools—all of which might be challenges in healthcare environments lacking resources. Furthermore under question is how effectively VR can replace the human touch, which remains a vital component of patient treatment.(3) Although VR may help patients comprehend better and replicate medical procedures, technology cannot replace the care, compassion, and in-person interaction so vital in the connection between a patient and a clinician.
Literature Review
Overview of existing VR applications in medicine
Virtual reality (VR) technology has been extensively used in the medical sector, particularly for training physicians and facilitating patient communication among other purposes. Virtual reality (VR) has been demonstrated to be a helpful technology for improving therapeutic outcomes, increasing the enjoyment of learning for medical professionals, and facilitating patient and physician communication.(4) This usage of VR has been shown by researchers to enhance practical abilities, reduce errors in actual operations, and assist in memory of acquired knowledge. VR is also very useful in enabling patients to recover. By assigning interesting activities that enhance their mental health, physical skills, and cognitive capacities, VR systems have been utilised to assist individuals recover after operations, strokes, or major injuries. Real-time feedback provided by these therapeutic applications keeps patients engaged and accelerates their recovery. By providing those with anxiety, PTSD, and anxieties soothing environments, VR has also advanced mental health treatment.(5) For example, VR is used in exposure therapy to slowly expose people to things that make them feel stressed in a safe and controlled setting. Virtual reality has been shown to help people with anxiety and PTSD a lot by letting them face their fears while still feeling safe.
VR in medical training
When used in medical teaching, Virtual Reality (VR) has completely changed how doctors and nurses learn important skills. In traditional medical education, students learn complicated processes by watching their teachers do them, working on dead bodies, or having few hands-on experiences. Some problems with these methods are that they can't always be used in the same way or at the same time, and they can't be used in rare or high-risk situations. VR seems like a good idea because it creates a virtual, realistic space where medical students can practise processes over and over again without worrying about making major mistakes. One big benefit of using VR to teach medicine is that it makes it possible to practise complicated processes in a very real way.(6) Medical workers and students can interact with 3D models of organs, tissues, and bones in a safe environment to practise surgery, diagnose diseases, and carry out treatments. Because these virtual experiences are based on real life, they help trainees learn more about the human body and improve their medical skills. VR gives trainees quick input, so they can see how they're doing and change their methods as needed. This makes learning more personalised. Figure 1 shows how virtual reality is used to improve skill development and simulations in medical training.
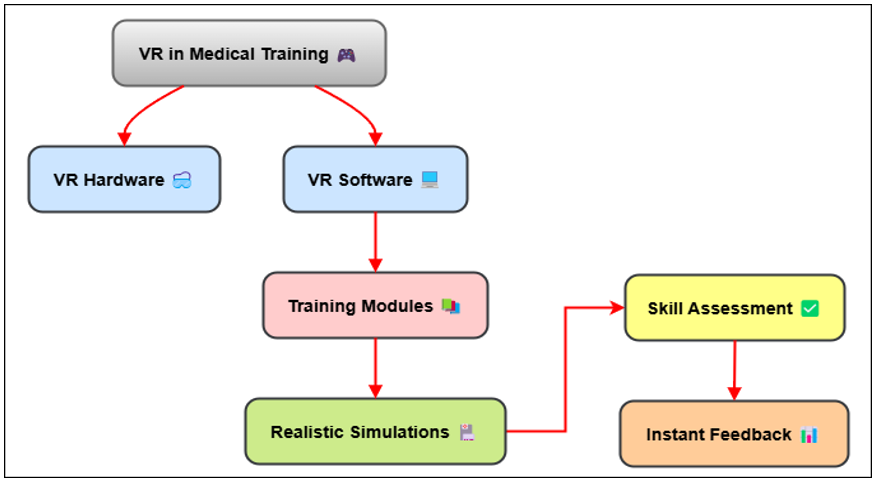
Figure 1. Illustrating VR in Medical Training
VR also lets you practise medical situations that are rare or dangerous, which might not happen very often in real-life training settings. VR can, for instance, recreate tough medical problems, emergency treatments, or shock care cases that would be hard to do in a real hospital.(7)
VR in patient communication
Good communication with patients is essential in healthcare if one wants to help them grasp, establish confidence, and provide improved treatment outcomes. Particularly when it comes to medical issues or procedures that are difficult to grasp, conventional means of communication—like talking and writing things down—are not always sufficient. Giving patients more interesting and cooperative experiences that enable them to grasp medical information has made virtual reality (VR) a significant tool for enhancing interaction with them. Virtual reality has one big advantage for communicating with patients: it helps them see and feel difficult medical concepts in a 3D, hands-on environment. Those scheduled for surgery or other medical procedures may go through a virtual reality simulation of the process. This clarifies for them the procedures, the reasons for their treatment, and what to anticipate. This visual approach of communication helps patients grasp a lot more, therefore lowering uncertainty and doubt.(8) A patient is more likely to feel qualified to make decisions that are best for them if they can see and interact with a digital form of their sickness or therapy. Common responses to medical treatments include anxiety and fear; hence VR not only helps patients comprehend better but also helps them feel less nervous and terrified. When patients can psychologically go through a procedure or therapy before it occurs, they are more equipped for what they will encounter in real life. For those coping with the stress of surgery, cancer treatments, or childbirth, this approach has particularly been effective. By allowing patients to get habituated to the procedure and provide them a feeling of control, VR may help reduce some of the emotional tension accompanying medical treatments.(9)
|
Table 1. Summary of Literature Review |
|||
|
Aspect |
Key Findings |
Impact |
Scope |
|
Surgical Training Simulation |
Improved procedural skills, reduced error rates |
Increased skill retention and competence |
Medical schools, surgical training centers |
|
VR in Laparoscopic Surgery |
Increased precision, reduced mistakes |
Better surgical outcomes, safer procedures |
Hospitals, surgery rooms, training institutes |
|
Medical Education with VR |
Enhanced engagement, deeper understanding |
Improved educational retention, more interactive learning |
Medical classrooms, universities |
|
VR for Anatomy Learning(10) |
Better spatial comprehension of anatomy |
Enhanced 3D understanding of human body |
Anatomy departments, medical schools |
|
VR in Pain Management |
Reduced perception of pain, effective distraction |
Non-invasive, alternative pain management |
Hospitals, pain clinics, rehabilitation centers |
|
Psychological Effects of VR on Patients |
Lowered anxiety levels, increased trust |
Improved doctor-patient relationships, better mental health |
Psychiatric clinics, hospitals |
|
VR for Communication in Healthcare |
Improved patient understanding, reduced misunderstandings |
Clearer explanation of conditions and treatments |
Healthcare settings, clinics |
|
Impact of VR on Patient Anxiety(11) |
Significant reduction in anxiety for surgical patients |
Effective tool for calming anxious patients |
Surgical departments, outpatient clinics |
|
VR in Pediatric Care |
Enhanced communication, reduced stress in children |
Improved coping skills and comfort during treatment |
Children’s hospitals, pediatric clinics |
|
VR for Chronic Pain Therapy |
Improved pain management, reduced medication use |
Reduced need for opioids, better quality of life |
Pain management centers, rehabilitation hospitals |
|
VR in Stroke Rehabilitation |
Enhanced motor recovery, higher patient participation |
Increased motivation and recovery rates |
Rehabilitation centers, stroke recovery units |
|
VR in Post-Operative Recovery |
Faster recovery times, better mobility outcomes |
Accelerated recovery and rehabilitation progress |
Post-operative care, rehabilitation facilities |
|
VR for Mental Health Treatment(12) |
Effective for reducing stress and trauma-related symptoms |
Reduced post-trauma symptoms and stress |
Psychological clinics, trauma centers |
|
VR in Medical Decision Making |
Improved clinical decisions, informed choices |
Better informed clinical decisions, personalized care |
Hospitals, clinical decision-making tools |
METHOD
Research design
The framework guides the studies manner and ensures that the objectives of the assignment are fulfilled as well as that the findings are correct and actual. A nicely-organised observes plan provides researchers with a clear street map that courses them in determining what, how, and how to examine information. Finding out how effectively virtual truth (VR) plays for clinical coaching and affected person verbal exchange calls for a mixed-techniques research strategy. To offer an entire picture of the topic beneath investigation, a mixed-techniques studies approach combines qualitative and quantitative research strategies.(13) Polls, assessments, and pre- and publish-tests might be employed as measurable contraptions in this studies to check how well VR plays for medical coaching and how it aids in affected person expertise and discount of hysteria. Those contraptions could offer quantifiable statistics on how VR affects patient pleasure, reminiscence of what one has received, and acquisition of recent abilities. Using qualitative techniques such interviews, attention corporations, and statement studies might assist one get examine how medical college students and patients who have experienced digital truth feel about it. By means of interactions with clinical experts and patients, researchers may additionally get greater understanding on how VR enhances gaining knowledge of and communication, the problems springing up from its usage, and the overall effect on healthcare carrier. Focus groups might provide insightful data on the extent and quality of usage of VR applications for medical education and patient interaction.(14) Statistical techniques allow one to search for trends, variations, and links between VR usage and learning outcomes or patient interaction by means of the gathered numerical data. By categorising and generally assessing the qualitative data, researchers may uncover trends and themes regarding how well and what impact VR has. Three distinct kinds of data are used in a mixed-methods research methodology to fully understand VR's impact on healthcare. It gives both measured results and deep, situation-specific insights.
Data collection methods
Surveys and interviews with medical professionals
Surveys and conversations with medical workers are important ways to get information about how Virtual Reality (VR) affects and improves medical training. Surveys are an organised way to get numbers from a lot of medical workers about their experiences with training that is based in virtual reality. The poll can ask about how easy VR tools are to use, how well they are thought to work, and how satisfied people are with them generally when they are used to teach medical processes and ideas. People often use Likert scales (from "strongly agree" to "strongly disagree") to find out how people feel about VR and how useful they think it is for training. These polls can also look at specific aspects of VR systems, like how realistic the models are, how interactive they are, and how much material they contain.(15) This clarifies for professionals how VR is used in medical education. Another approach to get qualitative data with plenty of detail about the experiences of medical professionals is in-depth interviews with them. Interviews allow researchers to probe the ways in which VR training has altered medical practice, including the issues that have emerged and how patients believe their fundamental abilities and capacity for decision-making have evolved. Open-ended questions in interviews allow you to learn about VR in training's unexpected benefits and drawbacks, including how it could increase confidence, enhance patient outcomes, or expose technological-related constraints. Combining polls with interviews helps you to better understand VR's contribution to medical education by displaying both general patterns and individual experiences.(16)
Patient feedback on VR experiences
Feedback from sufferers is fantastically essential for locating out how successfully virtual reality (VR) helps people speak and recognize scientific techniques. As part of this approach, replies are received from patients who have used VR equipment to examine greater about their sickness, destiny capsules, or planned surgical procedure. Researchers can also discover how patients sense about VR's capability to educate difficult medical standards in a way this is captivating and easy to recognise by means of using surveys, questionnaires, and based interviews. The take a look at would possibly have questions on how comfy sufferers are with VR generation, how easy it's miles for them to understand medical facts in 3D, and whether VR helped them feel less demanding or scared about medical remedies.(17) It could use Liker scales to discover how happy humans have been with their VR revel in usually, and open-ended inquiries to discover extra about how the era affected their choices, emotions, and feel of manipulate over their healthcare ride. Interviews are also a very good way to examine extra about the affected person's revel in and figure out if there are any troubles with the use of VR, like technical problems or no longer being acquainted with the tool. moreover, feedback from patients with certain situations, like those having surgery or most cancers remedy, can be very helpful in identifying how VR can assist reduce fear, improve compliance, and build trust in healthcare workers.(18) Researchers can figure out how VR affects patients' learning, happiness, and general health by getting comments from patients.
Evaluation of VR-based training effectiveness
Determining how effectively VR-based teaching performs is a major component of understanding its value in medical education. This method of data collecting tests how effectively VR models enhance medical abilities, memory of what you have studied, and overall capacity to execute medical procedures. Pre- and post-assessments—tests or examinations individuals take before to and during virtual reality training—are common. These assessments may evaluate your knowledge, ability to execute operations, and comprehension of difficult medical concepts. Apart from verifying data, determining the effectiveness of VR training entails monitoring the technical skill development. Experts may examine, for example, how students do certain activities such stitching, cutting, or condition identification both before and after VR training in surgical education. Examining objective elements like the time it takes to complete activities, how effectively the processes operate, and the frequency of errors can help you determine how VR models influence individuals. Data on how well operations go may also be compared to VR training to see which is better than conventional approaches. Teachers who see trainees using VR systems may also provide remarks that help to monitor the effectiveness of VR-based instruction.
· Step 1: Define Skill Improvement (SI). Skill improvement can be quantified as the percentage increase in competency after VR training.
![]()
· Step 2: Quantify Time Efficiency (TE). Time efficiency can be measured as the reduction in the time taken to complete tasks after VR training.
![]()
· Step 3: Calculate Accuracy (A). Accuracy can be defined as the percentage of correct steps performed during a task.
![]()
· Step 4: Evaluate Confidence Level (CL). Confidence can be measured by surveys, typically on a scale of 1-5, before and after VR training. We can quantify this as:
![]()
· Step 5: Overall Effectiveness (OE). The overall effectiveness of VR-based training can be a weighted average of skill improvement, time efficiency, accuracy, and confidence.
![]()
Sampling technique
Research using Virtual Reality (VR) for medical education and patient engagement depends much on the choice of sampling technique. This is meant to ensure fair and accurate data collecting. Sampling is the technique used in selecting the persons to provide data for the research. Together, deliberate and chance selection will help you to get a large and accurate group for this kind of research. Purposive sampling is a non-random approach of selecting subjects. Individuals are selected depending on certain characteristics or elements that are crucial for the research. In this regard, deliberate selection is the ideal approach to choose physicians who have trained with VR systems previously and patients who have utilised VR systems for medical education or treatment. Focussing on physicians, medical students, and nursing staff among others, the research may interact with those who have personally utilised VR technologies and provide insightful analysis on how they might be used in medical teaching. Furthermore carefully selected to ensure that the input comes from individuals who have really used the technology are patients who have used VR to learn about operations, comprehend therapies, or get well. Another approach utilised in the research is random selection, particularly in cases of gathering data from several sources. Like when examining how effectively VR training performs with a large group of medical students or professionals, random selection guarantees that everyone has an equal opportunity of being selected. This approach helps to reduce prejudice and guarantee that the outcomes can be used by a larger population. For patient communication research, a wide spectrum of patients from many backgrounds may be selected at random. This will therefore allow the comments on VR experiences to highlight a lot of diverse points of view.
Analysis techniques
Strong structure is necessary for surveys, interviews, and other forms of data analysis to provide relevant outcomes. Both quantitative and qualitative research approaches are used to get a whole picture of the data for a study on how well Virtual Reality (VR) performs for medical instruction and patient engagement. Numerical poll and pre- and post-test data is examined using statistical instruments for quantitative study. Common techniques assist to sum up and explain the key patterns and variations in the data by means of descriptive statistics like means, medians, and standard deviations. Inferential statistics let you determine if observed linkages or variances are statistically significant.
VR in Medical Training
Effectiveness of VR simulations in skill development
VR models can also be changed to fit the level of skill of the learner, which makes them useful for both new and experienced medical workers. Virtual reality (VR) lets new students get used to basic processes, while more experienced students can play more difficult models, like those of emergency treatments or rare medical conditions. Virtual reality (VR) can also recreate high-stakes situations that are hard to do in real life. This gives people practice in tough situations they might not face in real life. Overall, VR models work because they offer realistic, repeated, and adaptable learning experiences that help medical workers get better at what they do and learn new skills.
Comparison with traditional training methods
When you compare VR models to other ways of teaching medicine, the best thing about VR is that it lets you do hands-on practice without the restrictions that come with regular training. Some old ways of learning, like classes, learning from books, and observing, don't let you learn as interactively or practise medical situations that are hard to find or complicated. Traditional methods teach basic information, but VR models let you learn by doing, which can greatly improve the growth of technical skills and the ability to make professional decisions. VR training is different from standard training in a big way: you can practise things over and over again in a virtual world. In traditional hands-on training, trainees often practise on dead bodies, dummies, or real patients. This means that they may only be able to do a certain process a certain number of times. Conversely, VR gives trainers more opportunity to improve as it enables you repeatedly does the same action. VR models may also be created to vary depending on the learner's development, therefore providing a tailored experience that grows more challenging as one gets better. Furthermore more interesting and engaged than more passive approaches of learning are VR-based training. Trainees in VR are placed in a 3D environment where they may interact directly with bodily components, execute therapies, and make real-time judgements. This degree of participation enables individuals to understand more about medical concepts like anatomy, technique in a treatment, and probable complications. Conversely, traditional approaches could not allow you to interact as much or obtain feedback as a way, which would complicate learning and memory retention.
Case studies of VR success in medical education
Several case studies highlight how Virtual Reality (VR) has been effectively used in medical education to illustrate how it may assist students acquire new skills and perform better in their training. One well-known instance is how laparoscopy in particular is taught doctors using virtual reality. Medical students who studied how to conduct laparoscopic surgery using virtual reality models performed much better than those who learnt the same thing the conventional manner, according a research at the University Of Illinois College Of Medicine. The VR group completed tasks quicker, made fewer errors, and was more precise throughout actual operations. Using VR models repeatedly in a secure environment helps students develop muscle memory and hone their abilities, the research revealed. They were thus more ready for actual therapies. Another excellent case study is the use of virtual reality in emergency care instruction. Together, the University of California, San Francisco, and Osso VR developed a VR game physicians may use to learn how to treat major injuries such heavy bleeding or fractured bones. Under a lot of pressure, trainees might rehearse stabilising patients, appropriately tending to wounds, and making crucial decisions. The participants said that VR was a more fascinating and practical approach to learn than conventional trauma care training as it enabled them rehearse unusual and hazardous events difficult to replicate in real life. According to the case study, VR improved people's technical ability as well as their decision-making under great pressure. A third Mayo Clinic case study demonstrated how medical students may learn about the human body via virtual reality. Designed in cooperation with an interactive technology business, students may see and interact with 3D representations of human organs, cells, and systems on the VR platform.
VR in Patient Communication
Enhancing doctor-patient interactions through VR
Most of the time, processes, diagnoses, and treatment plans are explained using spoken language, written directions, and visual tools like maps and handouts. These methods don't always work, though, to make sure that people fully understand their illnesses or the treatments they will have to go through. VR fills in this gap by giving patients a three-dimensional, dynamic experience that lets them see and interact with medical data in real time. One way VR can be used is to mimic surgery or a medical process, so patients can see what will happen during their care in a virtual way. This method helps people understand each step better, along with the risks and expected results. Because VR is participatory, patients can ask questions and get more information during the experience. This builds trust and a sense of working together between the patient and the doctor. VR can help patients understand medical situations better and feel less anxious about treatments they don't know much about by making the explanations more natural and interesting. VR also improves the mental side of relationships between doctors and patients. Patients often feel more in charge of their health care decisions when they have a better understanding of their condition and how they will be treated. This can make patients happier, help them stick to their treatment plans better, and make the relationship between the patient and provider stronger.
Impact on patient comprehension of medical procedures
One of the best things about Virtual Reality (VR) in healthcare is that it can help patients understand complicated medical processes better. Patients often have trouble fully understanding what will happen and how it will affect their body and health when they are about to have surgery, diagnostic tests, or treatments they have never had before. VR is a creative response as it allows patients to undergo medical procedures in an interactive, realistic environment. This clarifies their expectations and allows them to grasp much more. Patients may virtually reality (VR) undergo medical procedures step by step online. They may see, for instance, how surgery is performed or learn about the goals behind other medical treatments. For example, someone scheduled for spinal surgery may use VR to see a 3D model of their spine displaying precisely what will happen during the procedure. This comprehensive approach enables patients to better image the body's relevant areas, grasp the medical objectives of the therapy, and comprehend the procedure. This degree of thorough, interesting explanation is much better than conventional approaches such providing patients with 2D images or difficult to completely grasp spoken explanations. When patients can see and engage with their doctors, researchers have shown that they grasp more, feel more secure and ready for treatments. Not knowing what will happen is generally the most stressful aspect of medical treatment, hence individuals also feel less terrified and nervous.
Use of VR for pain management and therapy
This method, called "distraction therapy," is based on the idea that focussing on interesting things, like colourful, interacting 3D worlds, can make pain seem less real. VR is often used in hospitals to help people deal with pain during treatments or recovery. For instance, burn patients who are going through the painful process of wound care or bandage changes might get lost in a relaxing or fun virtual world. Researchers have found that people who use VR during these kinds of treatments feel less pain and worry. When patients are immersed in a VR world that takes their mind away from pain, their brains' focus changes away from pain signs. This can help them feel less pain generally. VR is being used to treat diseases that cause ongoing pain as well as to ease pain during certain surgeries. By putting calming methods, guided meditation, and cognitive-behavioral therapy (CBT) into virtual settings, virtual reality-based treatment can help people deal with chronic pain. The goal of these treatment approaches is to help patients calm down, take control of their breathing, and do positive mental tasks that break the circle of pain perception. VR is also used in recovery treatments to help people who have recently had surgery or an injury improve their movement, function, and strength while also lowering their pain levels through engaging exercises.
RESULTS AND DISCUSSION
The study found that Virtual Reality (VR) makes both medical teaching and talking to patients a lot better. In medical training, people who used models were better at routine tasks, finished jobs faster, and were more accurate than when they used standard methods. Medical workers have said that VR's ability to simulate difficult situations and uncommon diseases is a big plus that lets people practise and gain confidence. When it came to communicating with patients, VR helped them understand medical methods better. Patients said they felt less anxious and had a better grasp on their treatment plans. Both medical students and patients were happier with VR experiences, which suggests that it could change the way doctors teach and patients connect with each other.
|
Table 2. VR Effectiveness in Medical Training |
||
|
Evaluation Parameters |
Pre-VR Training |
Post-VR Training |
|
Skill Improvement (%) |
55 |
85 |
|
Time Taken to Complete Task (mins) |
45 |
25 |
|
Accuracy in Task (%) |
65 |
92 |
|
Confidence Level (%) |
66,2 |
83,6 |
Table 2 shows a clear comparison of important rating factors before and after VR training, showing that VR does improve the results of medical training. There is a big jump in Skill Improvement, from 55 % to 85 %. This shows that VR-based training is a better way to get better than traditional methods. Figure 2 shows how VR training can help medical workers do their jobs better and learn new skills.
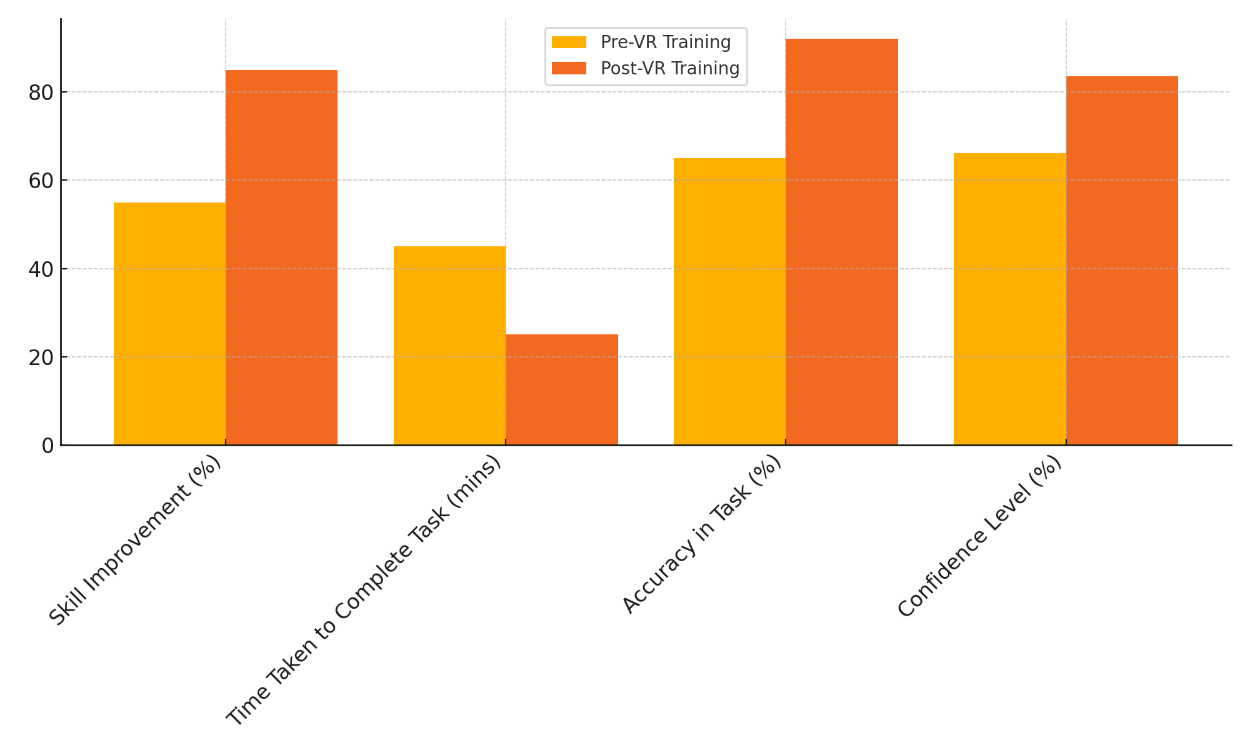
Figure 2. Effect of VR Training on Performance
This is probably because VR lets you practise over and over again and get feedback in real time. This big of a gain shows that VR helps people learn complicated medical processes faster. Figure 3 shows how performance changed before and after VR training, showing that results got a lot better.
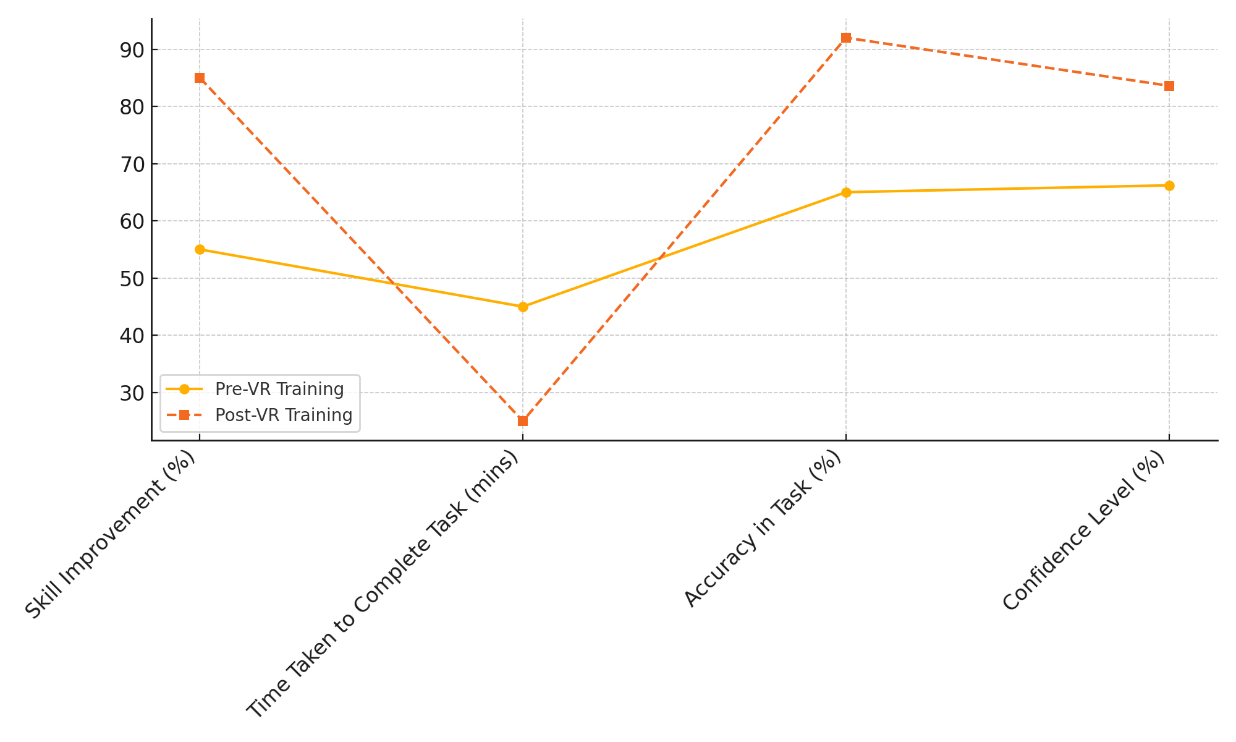
Figure 3. Performance Progression Pre & Post VR
It takes 25 minutes to finish the task instead of 45 minutes, which shows that the job is being done more quickly. This drop in the number of cases shows that as trainers use VR models more, they get better at doing medical treatments. As you can see in figure 4, performance and skill growth got better overall after VR training was used.
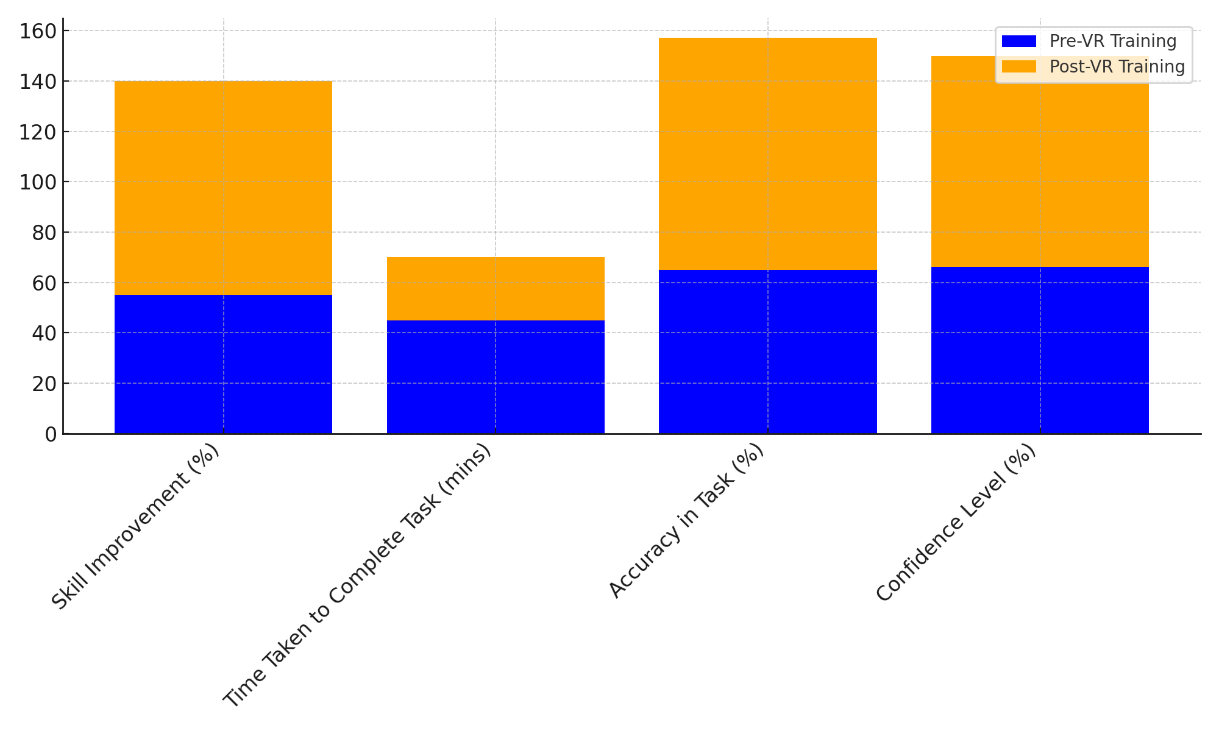
Figure 4. Overall Improvement with VR Training
Because of this, VR speeds up the learning process, which could save time in real-life professional situations. Also, Task accuracy went from 65 % to 92 %, which is a big jump. This shows that VR training not only improves speed and skill, but it also improves accuracy, which is very important in medical practice.
|
Table 3. VR Effectiveness in Patient Communication |
||
|
Evaluation Parameters |
Pre-VR Communication |
Post-VR Communication |
|
Comprehension (%) |
60 |
90 |
|
Anxiety Reduction (%) |
50 |
80 |
|
Satisfaction Level (%) |
62,4 |
88,7 |
|
Engagement Level (%) |
60,1 |
80,6 |
The table 3 shows how virtual reality (VR) has improved contact with patients, showing big gains in important rating factors. From 60 % to 90 %, comprehension went up, showing that VR helps people understand complicated medical problems, processes, and treatment plans better. Interactive, visual, and realistic models help patients understand their medical journey better and more naturally, which can be hard to do with traditional methods like vocal descriptions alone. The level of anxiety reduction also got a lot better, going from 50 % to 80 %. Because VR is so intense, it helps patients picture their medical treatments, which reduces their fear and confusion. This decrease in worry is very important for making patients feel better and making sure they follow their treatment plans, which will eventually lead to better health results. Figure 5 shows that medical workers' speaking skills get better after doing VR training.
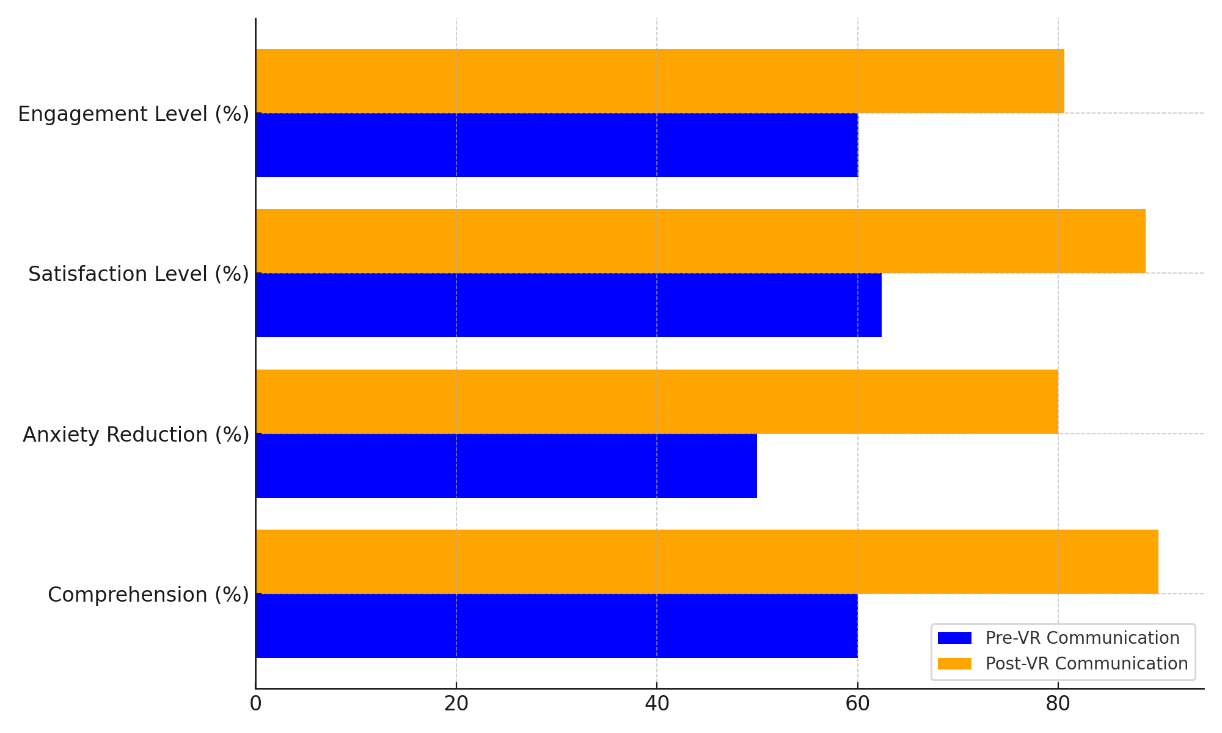
Figure 5. Impact of VR on Communication Skills
If you use VR in contact with patients, their satisfaction level goes up from 62,4 % to 88,7 %, which means they are happier with their healthcare. Virtual reality (VR) helps people understand things better and feel better emotionally, which makes patients happier. Figure 6 shows the breakdown of the conversation skills that got better with VR training, pointing out specific areas of growth.
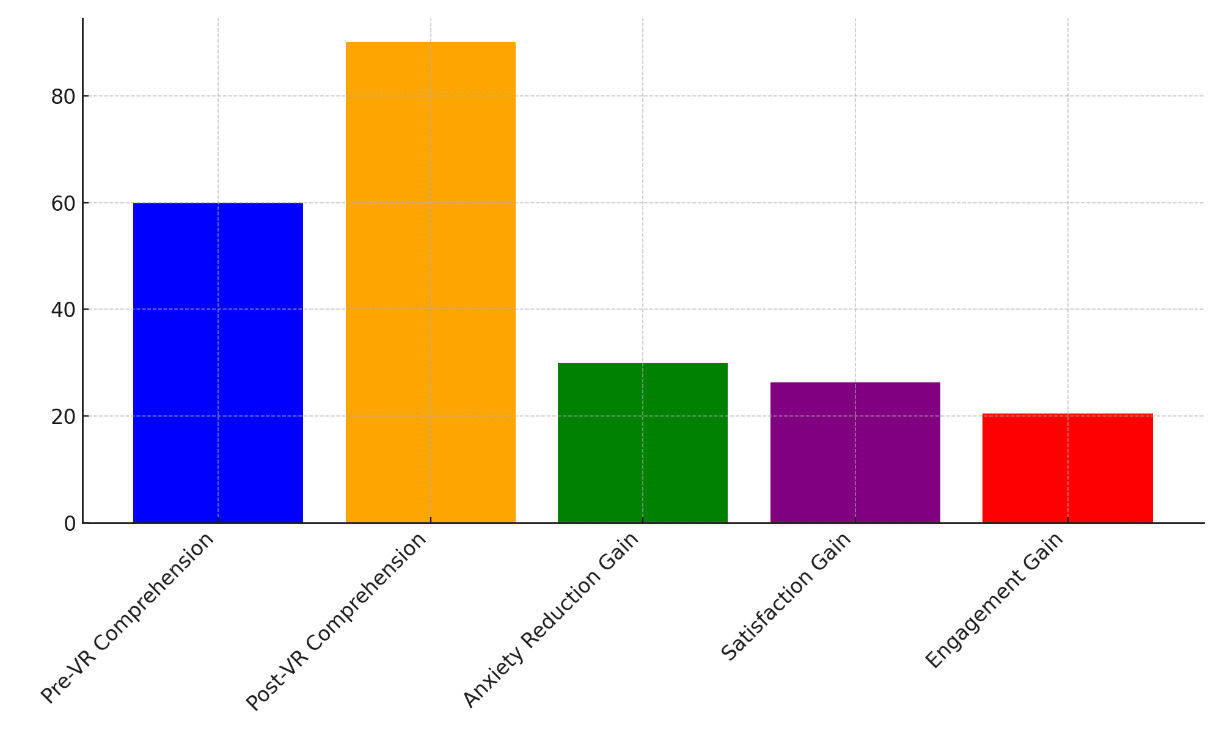
Figure 6. VR Communication Gains Breakdown
Lastly, the Engagement Level went from 60,1 % to 80,6 %, showing that VR is a better way to get patients' attention than standard ways of talking to them. This increased involvement builds a better bond between patients and their doctors, which is important for establishing trust and getting people to follow medical advice.
CONCLUSIONS
Virtual reality (VR) has been shown to be a very useful tool for both medical teaching and communicating with patients, with many advantages over older methods. VR models are used to teach medical procedures and skills because they create a realistic, hands-on learning environment that boosts confidence and knowledge. Medical workers can practise difficult processes over and over, which makes them better at them and better prepared for events that might happen in the real world. Because rare conditions and high-risk situations can be simulated in a safe, controlled setting, more people can be exposed to critical situations that would be hard to repeat in a hospital setting. When it comes to communicating with patients, VR is a completely new way to explain medical processes, evaluations, and treatment plans. By providing live 3D simulations of their ailments and drugs, VR helps individuals comprehend better, feel less stressed, and trust more. When patients can see the procedures of surgery or therapy, they become more in command of their health care choices. Along with making patients happy, this improved knowledge increases their likelihood of following treatment programs, which produces better outcomes. It's clear that virtual reality (VR) can help with medical training and contact with patients. However, problems like cost, usability, and the need for special tools must be fixed before VR is widely used. Additionally, more in-depth studies are still needed to fully understand how VR affects the long-term success of medical workers and the results for patients. Even with these problems, VR in healthcare seems to have a bright future. Technology is likely to be used more and more in medical teaching and patient care as it continues to improve and become cheaper. VR has the ability to change the way healthcare is provided by improving medical education, making it easier for patients to talk to doctors, and leading to better patient results and healthcare delivery. A more complete and patient-centered approach to care can be provided by healthcare workers who use VR along with standard medical methods.
BIBLIOGRAPHIC REFERENCES
1. Jensen, L.X.; Buhl, A.; Hussain, S.; Karan, A.; Konradsen, F.; Bearman, M. Digital education for health professionals in India: A scoping review of the research. BMC Med. Educ. 2023, 23, 561.
2. Jiang, H.; Vimalesvaran, S.; Wang, J.K.; Lim, K.B.; Mogali, S.R.; Car, L.T. Virtual reality in medical students’ education: Scoping review. JMIR Med. Educ. 2022, 8, e34860.
3. Barteit, S.; Lanfermann, L.; Bärnighausen, T.; Neuhann, F.; Beiersmann, C. Augmented, mixed, and virtual reality-based head-mounted devices for medical education: Systematic review. JMIR Serious Games 2021, 9, e29080.
4. Chen, F.Q.; Leng, Y.F.; Ge, J.F.; Wang, D.W.; Li, C.; Chen, B.; Sun, Z.L. Effectiveness of virtual reality in nursing education: Meta-analysis. J. Med. Internet Res. 2020, 22, e18290.
5. Miltykh, I.; Kafarov, E.S.; Covantsev, S.; Dadashev, A.S.; Skarlis, A.A.; Zenin, O.K. A new dimension in medical education: Virtual reality in anatomy during COVID-19 pandemic. Clin. Anat. 2023, 36, 24098.
6. Camargo-Vargas, D.; Callejas-Cuervo, M.; Mazzoleni, S. Brain-computer interfaces systems for upper and lower limb rehabilitation: A systematic review. Sensors 2021, 21, 4312.
7. Zagury-Orly, I.; Solinski, M.A.; Nguyen, L.H.; Young, M.; Drozdowski, V.; Bain, P.A.; Gantwerker, E.A. What is the current state of extended reality use in otolaryngology training? A scoping review. Laryngoscope 2023, 133, 227–234.
8. Treat, C.; Maniker, R.; Kessler, D. 182 All clear! Virtual reality defibrillator training for medical students is feasible, liked, and improves perceived knowledge, comfort, and skills. Ann. Emerg. Med. 2022, 80, S83.
9. Jeong, Y.; Lee, H.; Han, J.W. Development and evaluation of virtual reality simulation education based on coronavirus disease 2019 scenario for nursing students: A pilot study. Nurs. Open 2022, 9, 1066–1076.
10. Dilip Mishra, Nilesh Kumar Rajwade, Krishan Pal, Don Banjara, Rupendra Sonkar. (2015). Estimation of CO2 Saving From Household (Residential) Appliances Assisted With "Solar Technology". Advance Physics Letter, 2(1), 5-12
11. Chao, Y.P.; Kang, C.J.; Chuang, H.H.; Hsieh, M.J.; Chang, Y.C.; Kuo, T.B.J.; Yang, C.C.H.; Huang, C.G.; Fang, T.J.; Li, H.Y.; et al. Comparison of the effect of 360 versus two-dimensional virtual reality video on history taking and physical examination skills learning among undergraduate medical students: A randomized controlled trial. Virtual Real. 2023, 27, 637–650.
12. Lim, J.E.; Gu, J.Y.; Bae, J.H.; Lee, J.G. Comparative study of 360° virtual reality and traditional two-dimensional video in nonface-to-face dental radiology classes: Focusing on learning satisfaction and self-efficacy. BMC Med. Educ. 2023, 23, 855.
13. Cao, Y.; Ng, G.W.; Ye, S.S. Design and evaluation for immersive virtual reality learning environment: A systematic literature review. Sustainability 2023, 15, 1964.
14. Qiao, J.; Huang, C.R.; Liu, Q.; Li, S.Y.; Xu, J.; Li, L.; Redding, S.R.; Ouyang, Y.Q. Effectiveness of non-immersive virtual reality simulation in learning knowledge and skills for nursing students: Meta-analysis. Clin. Simul. Nurs. 2023, 76, 26–38.
15. Kim, H.-Y.; Kim, E.-Y. Effects of Medical Education Program Using Virtual Reality: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 3895.
16. Abreu, J.M.; Guimarães, B.; Castelo-Branco, M. The role of virtual interactive simulators in medical education: Exploring their integration as an assessment methodology in clinical years. Educ. Med. 2021, 22, 325–329.
17. Bray, L.; Spencer, S.; Pearson, E.; Meznikova, K.; Hepburn, D. Assessing the impact of immersion on learning in medical students: A pilot study comparing two-dimensional and three-dimensional virtual simulation. Simul. Gaming 2023, 54, 576–592.
18. Gan, W.; Mok, T.N.; Chen, J.; She, G.; Zha, Z.; Wang, H.; Li, H.; Li, J.; Zheng, X. Researching the application of virtual reality in medical education: One-year follow-up of a randomized trial. BMC Med. Educ. 2023, 23, 3.
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Yuvraj Parmar, Siddharth Sriram, Amit Vassney, Naresh Kaushik, Sarita Mohapatra, Mittapalli Premchandh.
Methodology: Yuvraj Parmar, Siddharth Sriram, Amit Vassney, Naresh Kaushik, Sarita Mohapatra, Mittapalli Premchandh.
Software: Yuvraj Parmar, Siddharth Sriram, Amit Vassney, Naresh Kaushik, Sarita Mohapatra, Mittapalli Premchandh.
Drafting - original draft: Yuvraj Parmar, Siddharth Sriram, Amit Vassney, Naresh Kaushik, Sarita Mohapatra, Mittapalli Premchandh.
Writing - proofreading and editing: Yuvraj Parmar, Siddharth Sriram, Amit Vassney, Naresh Kaushik, Sarita Mohapatra, Mittapalli Premchandh.