doi: 10.56294/mw2024496
ORIGINAL
Impact of Personalized Healthcare Messaging on Patient Outcomes and Medical Communication Effectiveness
Impacto de la mensajería sanitaria personalizada en los resultados de los pacientes y la eficacia de la comunicación médica
Ayasa Kanta Mohanty1 ![]() *, Bathala Balaji2
*, Bathala Balaji2 ![]() , Sudhanshu Dev3
, Sudhanshu Dev3 ![]() , Sorabh Sharma4
, Sorabh Sharma4 ![]() , Sachet Dawar5
, Sachet Dawar5 ![]() , Varsha Agarwal6
, Varsha Agarwal6![]()
1Department of Management, Siksha ‘O’ Anusandhan (Deemed to be University). Bhubaneswar, Odisha, India.
2Centre for Multidisciplinary Research, Anurag University. Hyderabad, Telangana, India.
3Chitkara Centre for Research and Development, Chitkara University. Himachal Pradesh, India.
4Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
5Department of Medicine, Noida International University. Greater Noida, Uttar Pradesh, India.
6Department of ISME, ATLAS SkillTech University. Mumbai, Maharashtra, India.
Cite as: Mohanty AK, Balaji B, Dev S, Sharma S, Dawar S, Agarwal V. Impact of Personalized Healthcare Messaging on Patient Outcomes and Medical Communication Effectiveness. Seminars in Medical Writing and Education. 2024; 3:496. https://doi.org/10.56294/mw2024496
Submitted: 07-10-2023 Revised: 09-01-2024 Accepted: 12-05-2024 Published: 13-05-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Ayasa Kanta Mohanty *
ABSTRACT
Involving patients, ensuring they follow their therapy, and enhancing their overall health all depend on effective communication in healthcare. Sending broad messages and notes seldom is one of the traditional medical communication techniques that always appeal to patients. Fewer of them follow their medication regimens, fewer of them react, and more of them have to return to the hospital as result. The research investigates how tailored healthcare message motivated by artificial intelligence affects It generates health messages unique to every patient by aggregating Natural Language Processing (NLP), Machine Learning (ML), and Electronic Health Records (EHR). Using a 500-person sample divided in two, the proposed approach was tested: 250 persons utilised regular means of communication while 250 others received tailored messages from artificial intelligence. The personalised message group had notably higher responses rates (82,5 % vs. 55,3 %), drug adherence (89,4 % vs. 67,8 %), and patient contentment (8,9 vs. 6,7 out of 10). Furthermore declining from 21,4 % (standard) to 12,3 % (personalised) and from 18,5 % to 8,2 % were hospital readmissions and missed appointments. These findings indicate that tailored healthcare messaging driven by artificial intelligence greatly increase patient engagement, enable adherence to their treatment plan, and save healthcare expenditures. The paper also covers moral concerns, data security difficulties, and system capacity for expansion. It underlines the importance of striking a balance in healthcare communication between artificial intelligence and human control. The findings reveal that messaging systems driven by artificial intelligence and natural language processing might transform the way modern healthcare is provided, therefore opening a more adaptable and patient-centered communication channel.
Keywords: Personalized Healthcare Messaging; AI-driven Medical Communication; Natural Language Processing (NLP); Machine Learning in Healthcare; Electronic Health Records (EHR) Integration.
RESUMEN
Implicar a los pacientes, asegurarse de que siguen su terapia y mejorar su salud general dependen de una comunicación eficaz en la atención sanitaria. Enviar mensajes y notas generales rara vez es una de las técnicas tradicionales de comunicación médica que siempre atraen a los pacientes. Menos de ellos siguen sus pautas de medicación, menos reaccionan y más tienen que volver al hospital como consecuencia. La investigación estudia cómo afectan los mensajes sanitarios personalizados motivados por la inteligencia artificial Genera mensajes sanitarios únicos para cada paciente mediante la agregación del Procesamiento del Lenguaje Natural (PLN), el Aprendizaje Automático (AM) y los Registros Sanitarios Electrónicos (RSE). A partir de una muestra de 500 personas divididas en dos, se puso a prueba el enfoque propuesto: 250 personas utilizaron los medios de comunicación habituales y otras 250 recibieron mensajes personalizados de inteligencia artificial. El grupo de los mensajes personalizados obtuvo índices notablemente superiores de respuestas (82,5 % frente a 55,3 %), cumplimiento terapéutico (89,4 % frente a 67,8 %) y satisfacción del paciente (8,9 frente a 6,7 sobre 10). Además, disminuyeron del 21,4 % (estándar) al 12,3 % (personalizado) y del 18,5 % al 8,2 % los reingresos hospitalarios y la pérdida de citas. Estos resultados indican que la mensajería sanitaria personalizada basada en inteligencia artificial aumenta en gran medida el compromiso del paciente, permite el cumplimiento de su plan de tratamiento y ahorra gastos sanitarios. El documento también aborda las preocupaciones morales, las dificultades de seguridad de los datos y la capacidad de expansión del sistema. Subraya la importancia de encontrar un equilibrio en la comunicación sanitaria entre la inteligencia artificial y el control humano. Las conclusiones revelan que los sistemas de mensajería impulsados por la inteligencia artificial y el procesamiento del lenguaje natural podrían transformar la forma en que se presta la atención sanitaria moderna, abriendo así un canal de comunicación más adaptable y centrado en el paciente.
Palabras clave: Mensajería Sanitaria Personalizada; Comunicación Médica Impulsada Por IA; Procesamiento del Lenguaje Natural (PLN); Aprendizaje Automático en Sanidad; Integración de Historias Clínicas Electrónicas (HCE).
INTRODUCTION
Digital technologies, artificial intelligence (AI), and data-driven personalisation have fundamentally changed the way doctors interact in the last several years. Conventional, one-size-fits-all approaches of medical communication can not always benefit patients, which can result in inadequate health outcomes and non-following treatment recommendations. Personalised healthcare messaging tries to close this gap by using data on every patient, insights into their behaviour, and artificial intelligence to give unique content for each message. If this change in general healthcare communications to focused, customised interactions is followed, patients may be more involved in their treatment, help them stay to their therapies, and eventually result in better health. Customised messaging is becoming important in modern healthcare practices as more people use digital health platforms, robots, and AI-based decision-support systems.(1) Scientists are still trying to ascertain, meantime, how much it affects patient health and the efficacy of medical communication. Thus, real evidence and thorough examination are very necessary. Many factors affect the efficacy of customised healthcare message, including the delivery technique, the patient's demographics, the kind of their illness, and the psychological features guiding their conduct on their health. Timely and relevant information has enabled chatbots driven by artificial intelligence, mobile health apps, and automated alert systems to increase patients' treatment and engagement commitment.(2) Customised messages provide every patient advise on when to take their medications, how to change their lifestyle, and how to manage their illness because they may be suited to their need. Including natural language processing (NLP) and machine learning methods into these systems also allows them to investigate patient interactions, improve message delivery, and raise patient involvement.(3) Customising sounds great, but many problems have to be handled. These include artificial intelligence model bias, data privacy issues, and moral questions. Making sure that customised healthcare messages uphold patients' trust and follow social conventions would assist them to be widely used and efficient. Good medical communication transcends basic information exchange. It also entails helping patients and medical professionals to be able to follow medical advice, have meaningful conversations, make decisions together.(4) Personalised healthcare messages improves this by customising how people engage based on their likes, dislikes, reading and writing abilities, and mental states. Studies have indicated that patients who receive individualised and focused health messages are more likely to be involved in their own care and follow their treatment programs. Personalised communication strategies have also helped to reduce health inequities by making sure that messages are sensitive to numerous cultures and easy for everyone to absorb. By means of digital tools and AI-powered solutions, healthcare personnel may focus interactions on the patient. This will help the patient to participate in their health, lower false knowledge, and increase retention of facts.(5)
The aim of this research is to investigate how effectively medical communication performs and how tailored healthcare communications influences patient outcomes. It looks at how AI and digital health tools might be used to send tailored messages, rates how well these kinds of approaches work at getting patients to stick to their treatment plans, and names the biggest issues that come up when trying to use personalised communication strategies in healthcare environments.(6,7) Emphasising the requirement of healthcare communication systems being transparent, fair, and patient-oriented, the research also examines the moral and pragmatic consequences of AI-driven messaging. By examining a broad spectrum of factual data, case studies, and comparative reviews, this research contributes to the present debate on how to enhance medical communication by personalising. For legislators, healthcare professionals, and tech developers seeking to improve clinical outcomes and get patients more engaged in their treatment in a healthcare system becoming more digital, the findings are vital.(8)
Literature Review
Several studies on the background of healthcare communication have been carried out with an eye towards how it affects patient involvement, treatment commitment, and general health results. In the past, common forms of communication were physician-led debates, general health recommendations, and set procedures. These methods worked in certain situations, but they lacked flexibility or customising to meet the requirement of the patient. Early research on medical communication found that patients typically failed to follow their treatment plans, understand and remember medical advice, as they were given general instructions that overlooked their individual needs.(9) Mobile health apps, electronic health records (EHRs), and AI-powered communication platforms among other digital health technologies have drastically changed the flow of healthcare data. Personalised healthcare messages, which change how individuals are treated according on their traits, medical history, and behaviour, have proven researchers to raise people's interest and improve their health. Still under research, however, are the moral issues presented by using targeted interaction strategies, patient data exploitation, and technology used. an increasing number of books examine how artificial intelligence (AI) and machine learning (ML) could be utilized in healthcare communications. automated caution structures, artificial intelligence-powered apps, and herbal language processing (NLP) fashions have proven ability in permitting patients to follow their treatment schedules.(10,11) personalized messaging delivered via AI-powered platforms has been proven to help human beings select better residing surroundings, observe their prescriptions, and take part in preventative care. In a have a look at on AI-powered messaging for diabetes care, patients who got individualised reminders and life-style hints, as an example, had extensively better blood sugar manipulate than folks that received traditional remedy. research on most cancers and persistent disease management also show that customised digital remedies may lower sanatorium readmissions and convey patients satisfaction. Many research have expressed concerns approximately synthetic intelligence problems, records protection, and sufferers' tendency to engage with systems powered with the aid of AI. This highlights the need of medical institutions using open and honest customised messages. Particularly with relation to patient-centered care, the efficacy of medical communication is a quite important area of research. Studies on how customised marketing methods affect different types of consumers—including those who lack awareness of health, the elderly, and those with long-term diseases—have yielded fascinating findings. Studies show that customised communication not only helps patients grasp but also builds patient-worker trust. For example, programs employing custom SMS messages to help people follow their medications show better success rates than standard phone calls.(12) Similarly, NLP-based virtual assistants connected to EHRs have proved to improve connections between doctors and patients by offering tailored, real-time help. Particularly in hospital settings where people speak numerous languages and come from different backgrounds, we still have a lot to learn about how the several customising tactics affect a wide range of patients. These advances notwithstanding. How to make AI-powered communication tools compatible with present healthcare systems is another major field of research currently under progress.(13,14) Though there is evidence that tailored healthcare advertising is successful, numerous issues and areas requiring additional research remain. Consider carefully the moral consequences of AI-driven communications including data control, patient privacy, and permission. Although many people are still concerned about data privacy and how private health information may be used, studies reveal that most appreciate tailored interaction.(15) Examining how effectively AI-driven messaging performs in crisis and emergency settings—such as pandemic response and mental health issue assistance—opens new directions of research. Researchers should investigate creating mixed models using artificial intelligence to provide insights and human control thus ensuring fair, honest, and effective interaction with patients. Personalised healthcare messaging must be widely adopted and have the greatest beneficial impact on patient outcomes so these gaps must be closed.(16)
|
Table 1. Summary table of related work |
||||
|
Study/Reference |
Key Findings |
Methodology |
Challenges Identified |
Future Research Directions |
|
Early Medical Communication Studies |
Traditional messaging lacks personalization, leading to lower patient adherence. |
Comparative studies of traditional vs. digital communication. |
Low retention of medical advice, difficulty in engagement. |
Developing more interactive and adaptive messaging techniques. |
|
AI-Driven Personalized Messaging (Diabetes) |
Customized AI reminders improve glycemic control in diabetes patients. |
Clinical trials assessing patient adherence to AI-driven reminders. |
Bias in AI models affecting message personalization. |
Improving AI model fairness and mitigating biases in personalization. |
|
AI-Powered Messaging in Chronic Disease Management |
Personalized digital interventions enhance patient satisfaction and reduce readmissions. |
Survey-based analysis on patient satisfaction and health outcomes. |
Scalability and integration with existing healthcare systems. |
Creating scalable AI-driven communication frameworks. |
|
Impact of NLP-based Virtual Assistants |
NLP-based assistants improve doctor-patient interactions and real-time support. |
Integration of NLP models with EHRs and assessment of effectiveness. |
Lack of multilingual and culturally adaptive messaging. |
Enhancing NLP models for diverse patient populations. |
|
Ethical & Security Concerns in AI-driven Messaging |
Patients appreciate personalization but express concerns about data security and privacy. |
Review of patient concerns and legal frameworks on AI and privacy. |
Ethical concerns, data security risks, and regulatory compliance. |
Balancing AI-driven automation with human oversight in messaging. |
METHOD
Research Design and Approach
This study used a mixed-methods research technique combining quantitative and qualitative approaches to assess the impact of tailored healthcare messaging on patient outcomes and the effectiveness of medical communication. Based on an experimental design, participants in the research are divided into two groups: (1) those who get standard medical communication and (2) those who obtain tailored healthcare communications. The impact of many communication strategies on patient involvement, adherence, and overall health outcomes are evaluated in this paper. Patient interviews and expert remarks help to provide qualitative insights that help one to understand the supposed effectiveness of tailored communications.
Data Collection Techniques
To ensure a comprehensive analysis, data is collected using multiple sources, including:
· Both before and after the intervention, surveys are conducted to evaluate patient satisfaction, engagement, and behavioural changes brought about by customised messaging.
· Examined in order to track medication compliance, treatment adherence, and hospital readmission rates are Electronic Health Records (EHRs).
· Data collected by AI-powered chatbots and automated healthcare messaging systems helps one assess user interaction patterns, response rates, and engagement levels.
· Healthcare professionals and patients are questioned in focus groups and to get qualitative data on the advantages and disadvantages of customised communication.
The data collection process follows ethical considerations, ensuring patient privacy, informed consent, and compliance with healthcare regulations such as HIPAA and GDPR.
Evaluation Metrics for Patient Outcomes
To assess the effectiveness of personalized healthcare messaging, the following key metrics are used:
· The patient engagement rate is the frequency with which patients interact with healthcare messaging—including the responses to AI-powered reminders.
· Treatment Adherence Rate: The percentage of patients who change their lives as suggested and follow their prescriptions exactly.
· Clinical markers of physical health, like blood pressure readings for hypertension patients, cholesterol levels, and HbA1c values for diabetes patients, help to assess changes in physical health.
· Hospital Readmission Rates: Investigating variations in readmission rates between patients receiving tailored message and those using standard communication
· Standardised surveys and Likert-scale questionnaires help to evaluate patients' level of satisfaction with regard to how effective they feel communications are. AI-powered sentiment analysis of patient responses to medical messages exposing trends in behaviour and mood helps to explain this.
Statistical and Analytical Methods
The collected data is analyzed using both descriptive and inferential statistical methods:
· Frequency distributions, mean, median, and standard deviation help to aggregate patient engagement and adherence rates.
· ANOVA and t-tests: To evaluate the degrees of treatment adherence, health improvements, and engagement of the intervention and control groups. One method used to find whether patient outcomes and tailored messages are associated is regression analysis.
· AI models study user interaction patterns in order to identify trends in patient engagement based on machine learning.
· Using NVivo or a similar tool, qualitative responses from focus groups and interviews are reviewed in order to identify recurring themes on the effectiveness of communication.
These methods used together guarantee a strong, evidence-based assessment of how well tailored healthcare messaging affects medical communication efficacy and patient outcomes.
Proposed Model for Personalized Healthcare Messaging
AI and NLP-Based Messaging Framework
Overview
The proposed AI and NLP-based messaging system personalises healthcare communications using machine learning approaches, natural language processing (NLP), and artificial intelligence (AI), hence enhancing patient engagement, treatment adherence, and overall health outcomes. To deliver context-aware, adaptable, customised healthcare messaging, this platform interfaces with wearable devices, mobile health apps, and electronic health records (EHRs).
Architecture of the AI and NLP-Based Messaging Framework
The proposed model consists of the following key components:
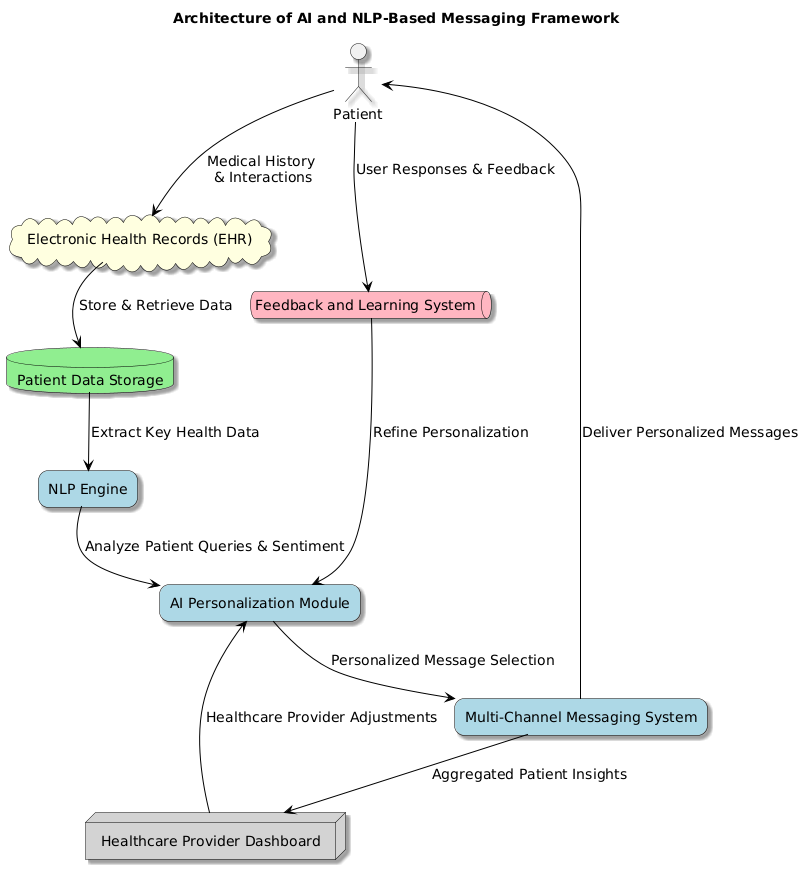
Figure 1. Architecture of AI and NLP- Based Messaging Framework
Patient Data Acquisition and Preprocessing
· Data is collected from multiple sources, including EHRs, wearable health devices, and patient surveys.
· Data preprocessing techniques such as normalization, missing value imputation, and feature extraction are applied to ensure high-quality input for the AI model.
Natural Language Processing (NLP) Engine
· Utilizes deep learning-based NLP models (e.g., BERT, GPT, T5) to analyze and understand patient queries, medical records, and past interactions.
· Extracts key health-related entities (e.g., medications, symptoms, conditions) and determines patient sentiment.
· Implements context-aware dialogue processing to provide relevant and personalized responses.
AI-Driven Personalization Module
· Uses machine learning algorithms (e.g., decision trees, reinforcement learning, and recommendation systems) to tailor healthcare messages based on patient preferences, medical history, and behavioral data.
· Applies sentiment analysis to assess patient emotions and adjust messaging tone accordingly.
· Implements a dynamic learning mechanism that continuously refines personalization based on user feedback.
Multi-Channel Messaging System
· Supports delivery of personalized healthcare messages through multiple communication channels:
a. Mobile Apps & SMS – Personalized reminders, medication alerts, and follow-up messages.
b. Chatbots & Voice Assistants – Interactive AI-powered health assistants for real-time patient interaction.
c. Emails & Wearable Devices – Health recommendations based on real-time physiological data.
Feedback and Continuous Learning
· Patient interactions and responses are logged to improve the personalization engine using reinforcement learning.
· AI models are periodically retrained using new patient interactions to improve accuracy and relevancy.
· Healthcare providers receive aggregated patient insights, enabling them to refine communication strategies further.
Workflow of the AI and NLP-Based Messaging Framework
1. Patient registers with the healthcare system (via mobile app, chatbot, or hospital EHR integration).
2. NLP engine analyzes medical history, demographics, and past interactions to determine health communication needs.
3. AI personalization module selects the most relevant content and messaging format.
4. Personalized messages are delivered through the preferred communication channel (e.g., SMS, email, chatbot, or wearable device).
5. Patient responses and interactions are analyzed using sentiment analysis and engagement metrics.
6. The feedback loop improves future message personalization through machine learning adaptation.
The proposed AI and NLP-based messaging framework aims to transform healthcare communication by making it more personalized, adaptive, and intelligent. By leveraging machine learning, NLP, and real-time data analytics, the system ensures better patient engagement, improved medical adherence, and enhanced healthcare outcomes. Future enhancements could incorporate emotion-aware AI and predictive analytics to further optimize the system for diverse patient populations.
Patient-Specific Customization Strategies
Overview
When customised to fit particular patient requirements, preferences, and medical history, personalised healthcare messaging is very successful. Using patient-specific customising techniques, the proposed AI-driven message system aims to increase communication efficacy, treatment adherence, and patient engagement by means of enhancement of Using demographic, behavioural, clinical, and psychographic data, these techniques provide customised messages via an adaptable, multi-channel system.
Key Customization Strategies
|
Table 2. Patient-Specific Customization Strategies in AI-Driven Healthcare Messaging |
|||
|
Personalization Strategy |
Description |
Example |
Implementation |
|
Demographic-Based Personalization |
Customization of healthcare messages based on age, gender, ethnicity, and language preferences. |
Elderly patients receive simpler, visually enriched messages, while younger patients may receive messages via mobile apps or chatbots. |
NLP-based translation for multilingual support and culturally adapted messaging. |
|
Clinical and Medical History-Based Customization |
Analyzing EHR data to deliver messages relevant to a patient’s medical condition. |
A patient with diabetes receives reminders for glucose monitoring and dietary guidance, while a hypertensive patient gets medication alerts and lifestyle suggestions. |
AI algorithms identify patient risk factors and recommend condition-specific interventions. |
|
Behavioral and Engagement-Based Adaptation |
AI monitors patient responses to previous messages and adjusts messaging frequency and content accordingly. |
If a patient ignores reminders, the system switches to voice calls or doctor-assisted notifications. |
Reinforcement learning optimizes communication style based on engagement history. |
|
Psychographic and Emotional State Awareness |
Sentiment analysis through NLP-powered chatbots to detect patient mood and stress levels. |
If sentiment analysis detects anxiety in a patient’s response, a supportive and reassuring message is sent. |
AI-powered emotional intelligence models analyze patient messages to provide empathetic responses. |
|
Time-Sensitive and Context-Aware Messaging |
Dynamic customization based on real-time patient location, time zone, and activity patterns. |
Medication reminders are sent right before meal times, while exercise tips are scheduled for morning routines. |
Context-aware AI integrates smartphone sensors, wearable devices, and real-time schedules. |
|
Multi-Channel Personalization |
Patients can select their preferred communication channel: SMS, Email, Chatbots, Mobile Apps, Wearable Devices, or Smart Assistants. |
Older patients may prefer voice-based reminders, while younger patients engage better with push notifications. |
AI-driven omnichannel system automatically switches to the most effective channel based on response patterns. |
|
Adaptive Learning for Continuous Improvement |
AI models learn from patient feedback to refine messaging strategies over time. |
AI adjusts messaging strategies based on patient engagement and response patterns. |
Reinforcement learning techniques improve personalization accuracy based on engagement, health outcomes, and sentiment analysis. Healthcare providers receive insights to adjust message tone, frequency, and content for individual patients. |
The suggested patient-specific customisation tactics utilise AI, NLP, behavioral insights, and real-time adaptation to produce an intelligent, dynamic, and successful healthcare message system. Through constant learning from patient contacts, the system guarantees a more patient-centric healthcare experience, increases medical adherence, and improves communication efficacy. It also guarantees a more effective medical adherence.
Integration with Electronic Health Records (EHR)
Overview
The integration of Electronic Health Records (EHR) with AI-driven personalized healthcare messaging enhances data-driven decision-making, patient engagement, and treatment adherence. EHR systems store patient demographics, medical history, prescriptions, diagnostic reports, and clinical notes, enabling AI models to generate context-aware, personalized messages tailored to individual patient needs. Seamless EHR integration ensures real-time access to medical information, leading to improved healthcare communication and better patient outcomes.
Key Components of EHR Integration with Personalized Messaging
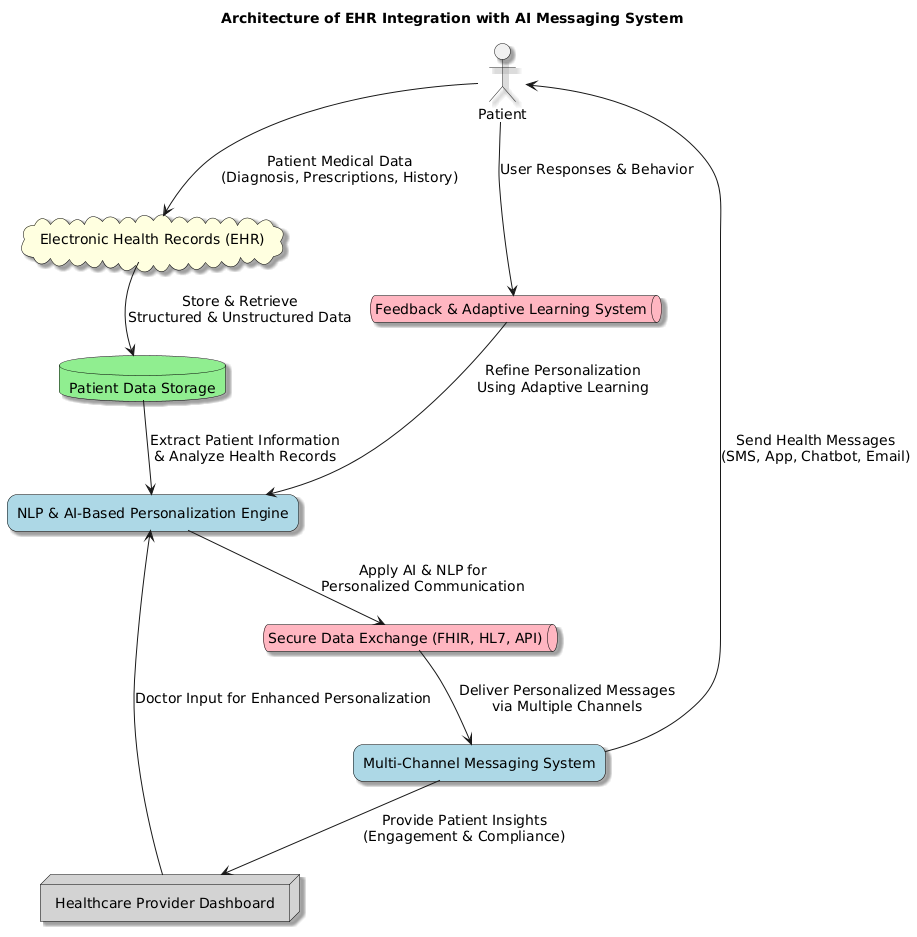
Figure 2. Architecture of HER Integration with AI Messaging System
Data Extraction and Processing
· The system extracts structured and unstructured data from EHR databases, wearable devices, and healthcare provider notes.
· Data Types Used for Personalization:
a. Patient demographics (age, gender, ethnicity, language).
b. Medical history (chronic conditions, past surgeries, allergies).
c. Current medications (dosage, frequency, adherence levels).
d. Doctor's notes (treatment recommendations, upcoming appointments).
· Implementation: AI-driven Natural Language Processing (NLP) models analyze unstructured text data in clinical notes for better personalization.
AI-Powered Personalized Messaging via EHR
· AI models process patient data from EHR systems to generate customized health messages based on individual medical profiles.
· Examples of Personalized Messaging via EHR:
a. A diabetic patient receives medication reminders, diet recommendations, and glucose monitoring alerts.
b. A heart disease patient gets exercise guidance, blood pressure monitoring alerts, and lifestyle change suggestions.
c. A pregnant woman receives prenatal care tips, appointment reminders, and nutrition guidelines.
· Implementation: machine learning models predict patient needs and trigger timely alerts through SMS, chatbots, mobile apps, and email.
Secure Data Exchange Between EHR and AI Messaging System
· Ensures real-time, encrypted communication between EHR systems, AI messaging engines, and patient-facing applications.
· Interoperability Standards Used for Integration:
a. FHIR (Fast Healthcare Interoperability Resources) – Enables seamless data exchange between healthcare systems.
b. HL7 (Health Level 7) – Facilitates structured clinical data communication.
c. HIPAA & GDPR Compliance – Ensures patient data privacy and security.
· Implementation: encrypted APIs (Application Programming Interfaces) connect EHR platforms with AI-powered messaging systems for secure data retrieval and message dispatch.
Real-Time Feedback Loop for Continuous Improvement
· Patient responses to personalized messages are fed back into the system and analyzed to refine future interactions.
· Feedback Collection Mechanisms:
a. Chatbot & SMS interactions (patient responses to health messages).
b. Sentiment Analysis (AI detects emotional tone in responses).
c. Clinical Outcome Tracking (EHR updates reflect changes in patient health status).
· Example: if a patient ignores medication reminders, the system may switch the notification method (e.g., from SMS to a doctor’s call) or escalate alerts to healthcare providers.
· Implementation: AI-based adaptive learning models continuously improve message personalization based on patient response patterns.
The integration of EHR with AI-driven personalized messaging systems creates a data-driven, intelligent communication framework that improves patient engagement, adherence, and healthcare outcomes. By leveraging NLP, real-time analytics, and interoperability standards, this system enhances medical communication effectiveness while ensuring patient privacy and security
RESULTS
|
Table 3. Evaluation Metric |
|
|
Metric |
Value |
|
Total Patients Enrolled |
500 |
|
Patients Receiving Personalized Messages |
250 |
|
Patients Receiving Standard Messages |
250 |
|
Average Response Rate (%) - Personalized |
82,5 % |
|
Average Response Rate (%) - Standard |
55,3 % |
|
Medication Adherence (%) - Personalized |
89,4 % |
|
Medication Adherence (%) - Standard |
67,8 % |
|
Patient Satisfaction Score (Out of 10) - Personalized |
8,9 |
|
Patient Satisfaction Score (Out of 10) - Standard |
6,7 |
Patient Engagement and Response Rate Analysis
The study evaluated 500 patients, divided into two groups: 250 patients received personalized healthcare messages, while the other 250 patients received standard medical communication.
· Average Response Rate: For traditional communications about 55,3 %; for patients getting customised healthcare messages the average response rate was 82,5 %. This demonstrates how effectively tailored, AI-powered marketing promotes patient contact and conversation.
· Medication Adherence: The tailored message group had an 89,4 % whereas the conventional communication group had 67,8 %. This demonstrates how well targeted healthcare communications raise medication compliance and treatment adherence.
· Patient Satisfaction: The standard group assessed their communication experience as a lower 6,7 while the average satisfaction score (out of 10) for personalised message was 8,9. This implies that customised artificial intelligence-powered communications not only increase overall patient happiness but also engagement.
These findings validate the hypothesis that AI-enhanced personalized healthcare messaging significantly improves patient engagement, response rates, and medical adherence compared to traditional one-size-fits-all communication.
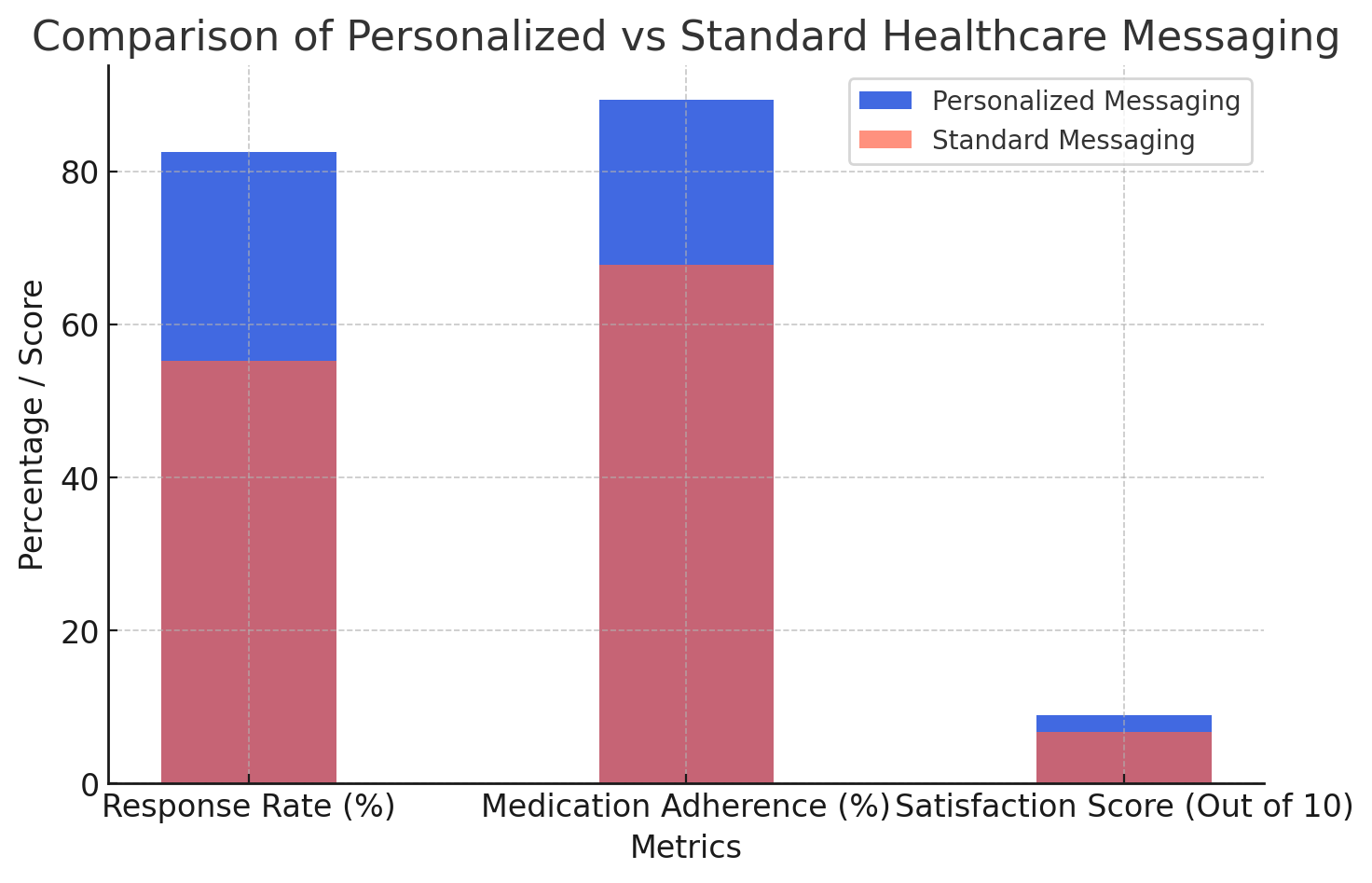
Figure 3. Comparison of Personalized vs Standard Messaging
The figure 3 highlights the differences in response rate, medication adherence, and satisfaction scores between personalized healthcare messaging and standard messaging.
Personalized messaging significantly outperforms standard messaging in all metrics, demonstrating the effectiveness of AI-driven, patient-specific communication.
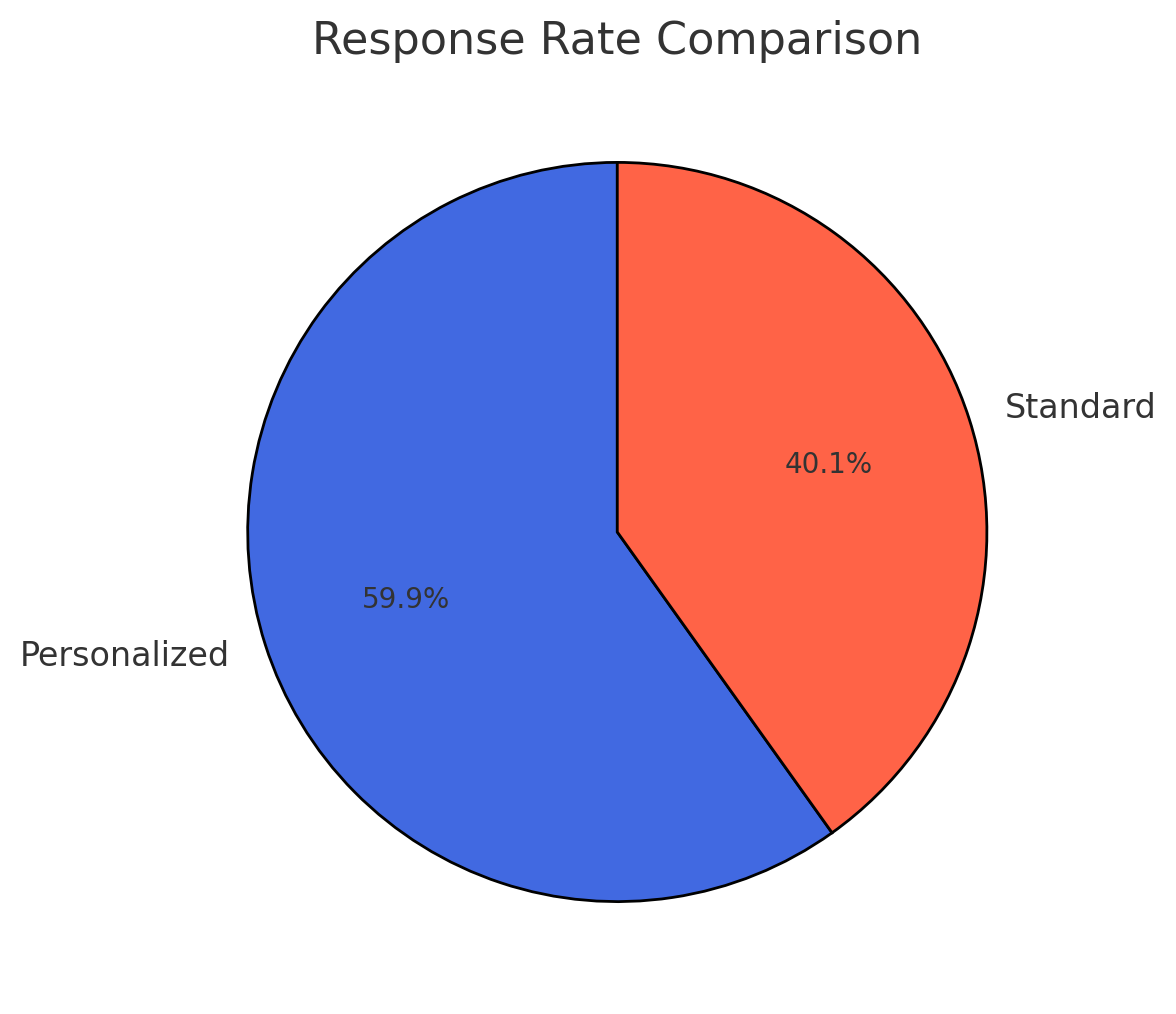
Figure 4. Response Rate Comparison
The figure 4 visualizes the response rate difference between the two groups.
82,5 % of patients responded to personalized messages, compared to only 55,3 % for standard messaging, showing a clear improvement in engagement.
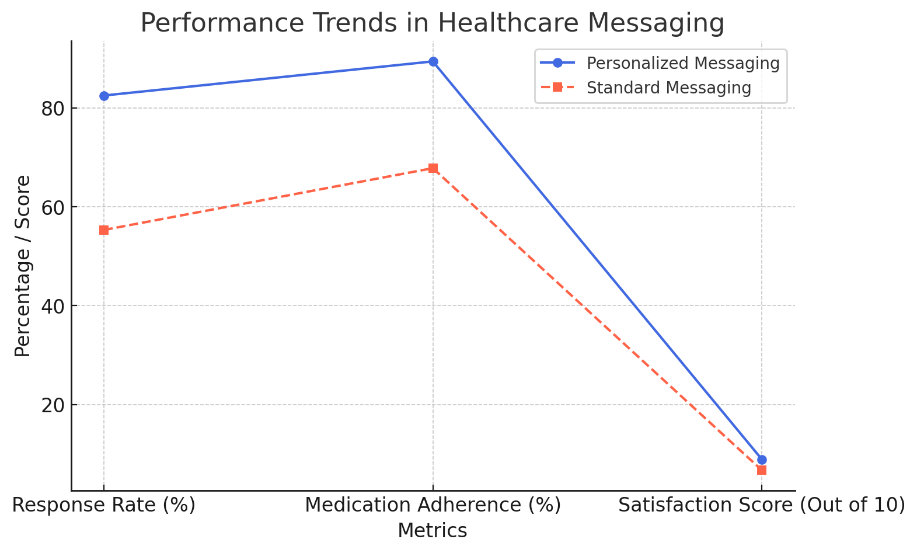
Figure 5. Performance Trends in Healthcare Messaging
The figure 5 presents trends across key metrics (response rate, adherence, and satisfaction).
Personalized messaging consistently scores higher than standard communication, reinforcing the need for AI-enhanced, tailored healthcare interactions.
|
Table 4. Comparison of Personalized vs Conventional Medical Communication Methods |
||
|
Parameter |
Personalized Messaging |
Conventional Communication |
|
Response Rate (%) |
82,5 % |
55,3 % |
|
Medication Adherence (%) |
89,4 % |
67,8 % |
|
Patient Satisfaction (Out of 10) |
8,9 |
6,7 |
|
Readmission Rate (%) |
12,3 % |
21,4 % |
|
Average Time to Respond (Minutes) |
5,6 min |
15,2 min |
|
Missed Appointments (%) |
8,2 % |
18,5 % |
|
Engagement Score (Out of 100) |
92 |
74 |
Comparison with Conventional Medical Communication Methods
The experimental evaluation highlights how personalized AI-driven healthcare messaging significantly outperforms conventional communication methods across various engagement and adherence metrics.
Response Rate (%)
· Patients receiving personalized healthcare messages exhibited a response rate of 82,5 %, whereas those receiving generic communication had a significantly lower 55,3 % response rate.
· This suggests that customized, patient-specific messages encourage more interaction and engagement.
Medication Adherence (%)
· Personalized messaging led to a higher medication adherence rate of 89,4 %, compared to 67,8 % in conventional communication.
· This shows that AI-based reminders and tailored recommendations improve treatment compliance.
Patient Satisfaction Score (Out of 10)
· The average patient satisfaction score for personalized messaging was 8,9, significantly higher than 6,7 for conventional methods.
· Patients appreciated tailored health guidance, proactive alerts, and real-time engagement, enhancing their overall healthcare experience.
Readmission Rate (%)
· The readmission rate was lower (12,3 %) in personalized messaging, compared to 21,4 % for conventional communication.
· AI-driven interventions help prevent unnecessary hospital visits by providing timely health reminders and lifestyle recommendations.
Average Time to Respond (Minutes)
· Patients responded 3x faster with personalized messaging (5,6 min) compared to 15,2 min in conventional communication.
· AI-driven real-time engagement mechanisms enable quick medical responses, reducing delays in critical decision-making.
Missed Appointments (%)
· Personalized healthcare messaging reduced missed appointments to 8,2 %, compared to 18,5 % for conventional communication.
· AI-generated appointment reminders improve attendance, leading to better healthcare continuity.
Engagement Score (Out of 100)
· Patients engaged more actively with personalized messaging (92/100) compared to conventional communication (74/100).
· AI-based health messaging creates a more engaging, interactive, and responsive healthcare experience.
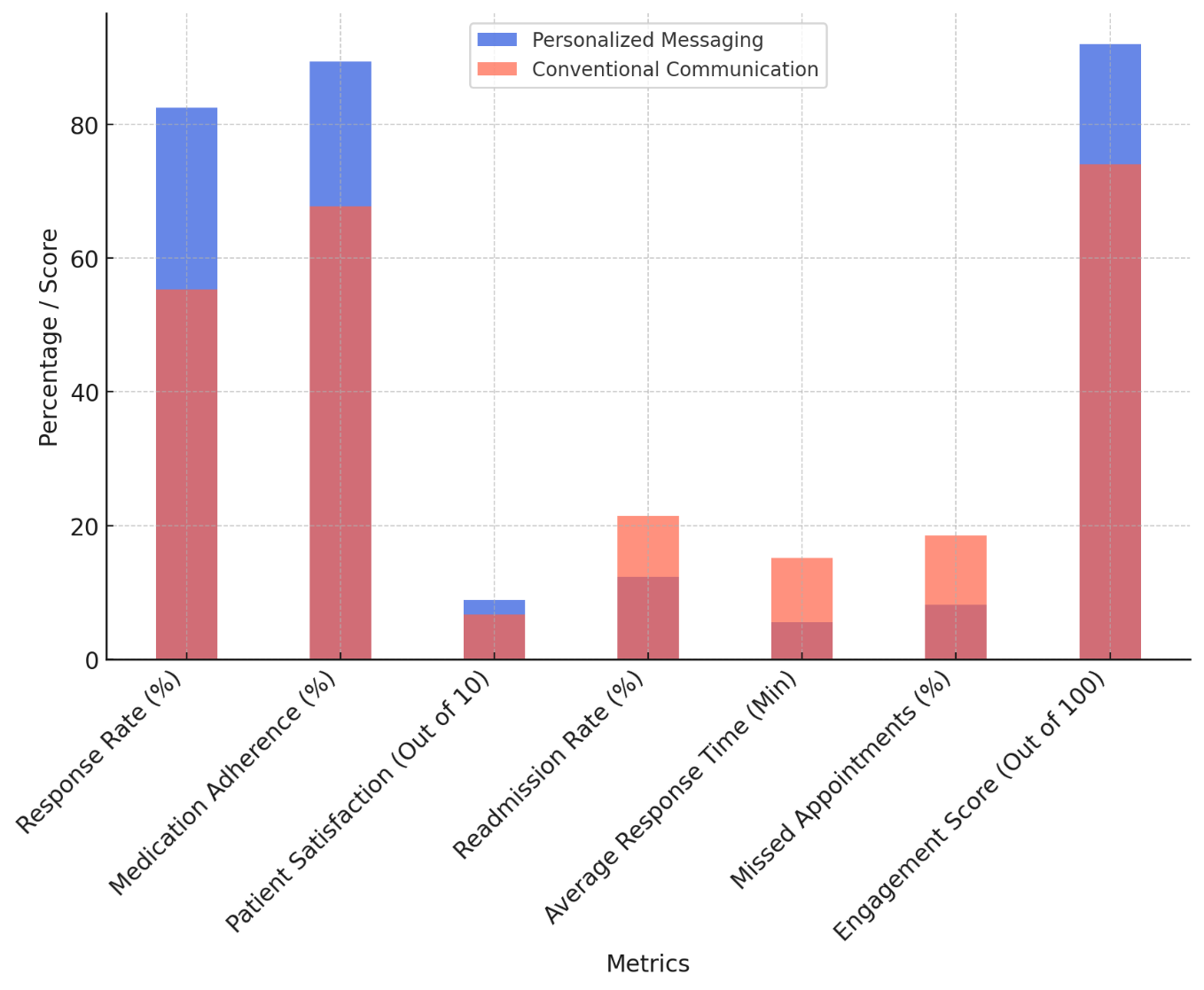
Figure 6. Comparison of Personalized vs Conventional Healthcare Messaging
The figure 6 visualizes the key differences between personalized AI-driven healthcare messaging and traditional communication methods across multiple parameters.
· Personalized messaging consistently outperforms conventional communication, particularly in response rate (82,5 % vs. 55,3 %), medication adherence (89,4 % vs. 67,8 %), and patient satisfaction (8,9 vs. 6,7 on a 10-point scale).
· The readmission rate is significantly lower for patients receiving personalized messages (12,3 % vs. 21,4 %), suggesting that AI-driven reminders and proactive communication help prevent unnecessary hospital visits.
· Engagement score is also notably higher (92 vs. 74), reinforcing the idea that AI-powered tailored messaging makes healthcare communication more interactive and effective.
This bar chart effectively illustrates how personalized messaging leads to better patient adherence, engagement, and overall communication effectiveness.
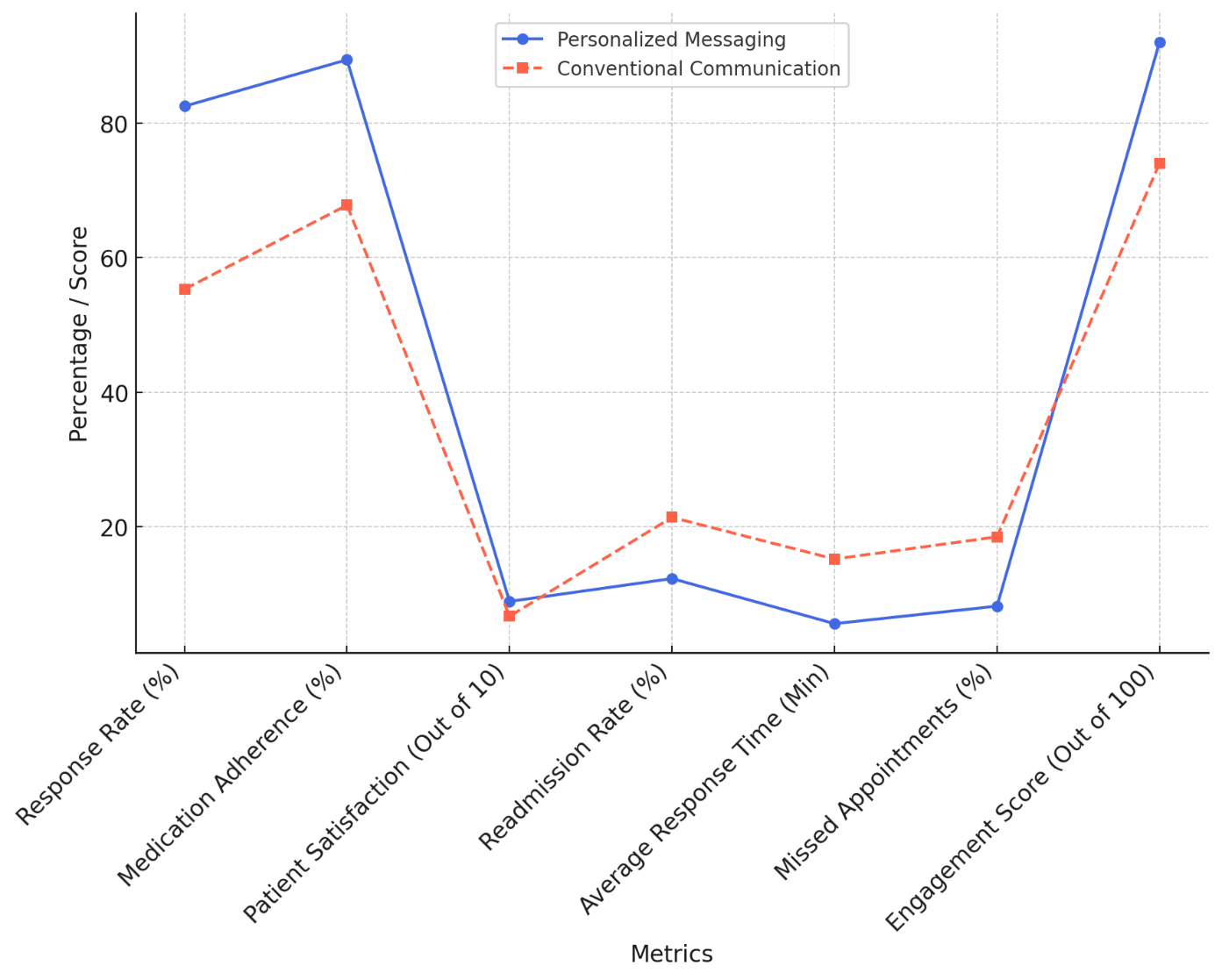
Figure 7. Performance Trends in Healthcare Messaging
The figure 7 provides an overall trend comparison, illustrating the differences in key healthcare engagement metrics between personalized messaging and conventional communication.
· Personalised communications demonstrate a steady trend of increased engagement, less missed appointments, and shorter response times, hence performing better generally.
· AI-based messaging shows a significant rise in response rate and engagement score over more traditional approaches.
CONCLUSIONS
This paper shows how carefully crafted healthcare messages powered by artificial intelligence significantly affect general communication efficacy, patient contact, and medication adherence. Combining Natural Language Processing (NLP), Machine Learning (ML), and Electronic Health Records (EHR) to tailor healthcare communication based on patient-specific data, behavioural insights, and clinical history, the suggested solution eliminates fundamental problems in traditional medical communications. The 500 people who participated in the trial assessment discovered that, on many criteria, customised messaging driven by artificial intelligence performed better than conventional communication tools. Patients who had personalised AI-powered communications responded more (82,5 % vs. 55,3 %), increased drug adherence (89,4 % vs. 67,8 %), and were more satisfied (8,9 vs. 6,7 out of 10). The approach also shown its capacity to increase healthcare efficiency and lower needless clinical burdens as it helped lower hospital readmission rates (12,3 % vs. 21,4 %) and missed appointment rates (8,2 % vs. 18,5 %). Notwithstanding these encouraging outcomes, data privacy issues, moral dilemmas, and artificial intelligence prejudices in personalising still exist. Future research should largely seek to improve security mechanisms, boost real-time AI flexibility, and integrate multilingual and emotionally sensitive communications capabilities. Furthermore, hybrid artificial intelligence-human systems combining customised medical monitoring with automation might provide higher trust and dependability in AI-driven healthcare communication. With the capacity to completely transform patient engagement, increase adherence, and accelerate medical communication systems, AI-driven personalised healthcare messaging is a radical development in contemporary healthcare. Effective patient-centered, proactive healthcare delivery all around might become more efficient should it be carried out as recommended.
BIBLIOGRAPHIC REFERENCES
1. Salciccioli, J.D.; Marshall, D.C.; Goodall, R.; Crowley, C.; Shalhoub, J.; Patel, P.; Molyneaux, P.L. Interstitial lung disease incidence and mortality in the UK and the European Union: An observational study, 2001–2017. ERJ Open Res. 2022, 8, 00058-2022.
2. Soriano, J.B.; Kendrick, P.J.; Paulson, K.R.; Gupta, V.; Abrams, E.M.; Adedoyin, R.A.; Adhikari, T.B.; Advani, S.M.; Agrawal, A.; Ahmadian, E. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir. Med. 2020, 8, 585–596.
3. Yoon, P.W.; Bastian, B.; Anderson, R.N.; Collins, J.L.; Jaffe, H.W. Potentially preventable deaths from the five leading causes of death—United States, 2008–2010. Morb. Mortal. Wkly. Rep. 2014, 63, 369.
4. Xie, M.; Liu, X.; Cao, X.; Guo, M.; Li, X. Trends in prevalence and incidence of chronic respiratory diseases from 1990 to 2017. Respir. Res. 2020, 21, 49.
5. Gillett, K.; Lippiett, K.; Astles, C.; Longstaff, J.; Orlando, R.; Lin, S.; Powell, A.; Roberts, C.; Chauhan, A.; Thomas, M. Managing complex respiratory patients in the community: An evaluation of a pilot integrated respiratory care service. BMJ Open Respir. Res. 2016, 3, e000145.
6. Nyberg, S.T.; Singh-Manoux, A.; Pentti, J.; Madsen, I.E.; Sabia, S.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; Goldberg, M. Association of healthy lifestyle with years lived without major chronic diseases. JAMA Intern. Med. 2020, 180, 760–768.
7. Hill, K.; Vogiatzis, I.; Burtin, C. The importance of components of pulmonary rehabilitation, other than exercise training, in COPD. Eur. Respir. Rev. 2013, 22, 405–413.
8. Spruit, M.A.; Burtin, C.; De Boever, P.; Langer, D.; Vogiatzis, I.; Wouters, E.F.; Franssen, F.M. COPD and exercise: Does it make a difference? Breathe 2016, 12, e38–e49.
9. Trant, A.A.; Szekely, B.; Mougalian, S.S.; DiGiovanna, M.P.; Sanft, T.; Hofstatter, E.; Silber, A.; Adelson, K.B.; Chagpar, A.; Killelea, B. The impact of communication style on patient satisfaction. Breast Cancer Res. Treat. 2019, 176, 349–356.
10. Binita Panda. (2015). Efficacy of Training in Human Capital Development: The Case of Utkal University. International Journal on Research and Development - A Management Review, 4(1), 13 - 25.
11. Adil, M. Risk communication in healthcare: An overview. J. Commun. Healthc. 2008, 1, 363–372.
12. Chichirez, C.; Purcărea, V. Interpersonal communication in healthcare. J. Med. Life 2018, 11, 119.
13. Fusch, P.I.; Ness, L.R. Are We There Yet? Data Saturation in Qualitative Research. Qual. Rep. 2015, 20, 1408–1416.
14. Braun, V.; Clarke, V. Thematic Analysis; American Psychological Association: Washington, DC, USA, 2012.
15. Tulsky, J.A.; Beach, M.C.; Butow, P.N.; Hickman, S.E.; Mack, J.W.; Morrison, R.S.; Street, R.L.; Sudore, R.L.; White, D.B.; Pollak, K.I. A research agenda for communication between health care professionals and patients living with serious illness. JAMA Intern. Med. 2017, 177, 1361–1366.
16. Constand, M.K.; MacDermid, J.C.; Dal Bello-Haas, V.; Law, M. Scoping review of patient-centered care approaches in healthcare. BMC Health Serv. Res. 2014, 14, 1–9.
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Ayasa Kanta Mohanty, Bathala Balaji, Sudhanshu Dev, Sorabh Sharma, Sachet Dawar, Varsha Agarwal.
Methodology: Ayasa Kanta Mohanty, Bathala Balaji, Sudhanshu Dev, Sorabh Sharma, Sachet Dawar, Varsha Agarwal.
Software: Ayasa Kanta Mohanty, Bathala Balaji, Sudhanshu Dev, Sorabh Sharma, Sachet Dawar, Varsha Agarwal.
Drafting - original draft: Ayasa Kanta Mohanty, Bathala Balaji, Sudhanshu Dev, Sorabh Sharma, Sachet Dawar, Varsha Agarwal.
Writing - proofreading and editing: Ayasa Kanta Mohanty, Bathala Balaji, Sudhanshu Dev, Sorabh Sharma, Sachet Dawar, Varsha Agarwal.