doi: 10.56294/mw2024500
ORIGINAL
Medical Malpractice and Ethical Accountability A Case Study Analysis of Patient Safety Incidents
Negligencia médica y responsabilidad ética análisis de casos de incidentes relacionados con la seguridad del paciente
Tarun Kapoor1 ![]() *, Avinash Kumar2
*, Avinash Kumar2 ![]() , Vinima Gambhir3
, Vinima Gambhir3 ![]() , Samir Samal4
, Samir Samal4 ![]() , Syed Farhan5
, Syed Farhan5 ![]() , Prateek Aggarwal6
, Prateek Aggarwal6 ![]()
1Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
2Department of ENT, Noida International University. Greater Noida, Uttar Pradesh, India.
3Department of ISME, ATLAS SkillTech University. Mumbai, Maharashtra, India.
4Department of Critical Care Medicine, IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University). Bhubaneswar, Odisha, India.
5Centre for Multidisciplinary Research, Anurag University. Hyderabad, Telangana, India.
6Chitkara Centre for Research and Development, Chitkara University. Himachal Pradesh, India.
Cite as: Kapoor T, Kumar A, Gambhir V, Samal S, Farhan S, Aggarwal P. Medical Malpractice and Ethical Accountability A Case Study Analysis of Patient Safety Incidents. Seminars in Medical Writing and Education. 2024; 3:500. https://doi.org/10.56294/mw2024500
Submitted: 08-10-2023 Revised: 10-01-2024 Accepted: 12-05-2024 Published: 13-05-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Tarun Kapoor *
ABSTRACT
Since they directly impact patient safety and the quality of treatment generally, ethical responsibility and medical misbehaviour are fundamental elements of healthcare systems. Aiming at events influencing patient safety, this case study analysis seeks to explore the intricate relationship between medical misbehaviour and ethical responsibilities in the healthcare surroundings. Malpractice that is, negligence, mistakes, or inactivity among medical professionals affects not just patients but also doctors and has significant effects on both. Mostly ethical obligation of healthcare personnel determines following professional standards and protecting of patient rights and well-being. Examining numerous well-known cases of patient safety, the study looks at their moral implications, causes, and background. Analysing the actions and choices made by medical personnel during these events exposes patterns of non-following standard procedures, poor communication, and negligence. It also emphasises the moral duty of medical professionals in preventing misbehaviour and the importance of openness, ongoing education, and a strong culture of accountability in healthcare firms. The findings highlight the need of providing clear ethical norms and regulations to healthcare professionals so that patient safety is a first concern and errors are handled honestly. It also addresses how government authorities and medical boards, among other monitoring bodies, ensure ethical norms are fulfilled. There are suggestions for how to improve medical practices, make training in ethics better, and make it easier for patients and providers to talk to each other.
Keywords: Medical Malpractice; Ethical Accountability; Patient Safety; Healthcare Negligence; Professional Standards.
RESUMEN
Dado que repercuten directamente en la seguridad del paciente y en la calidad del tratamiento en general, la responsabilidad ética y el mal comportamiento médico son elementos fundamentales de los sistemas sanitarios. Con el objetivo de analizar los acontecimientos que influyen en la seguridad del paciente, este estudio de caso pretende explorar la intrincada relación entre el mal comportamiento médico y las responsabilidades éticas en el entorno sanitario. La mala praxis, es decir, la negligencia, los errores o la inactividad de los profesionales médicos, no sólo afecta a los pacientes, sino también a los médicos, y tiene efectos significativos en ambos. Principalmente, la obligación ética del personal sanitario determina el cumplimiento de las normas profesionales y la protección de los derechos y el bienestar del paciente. Examinando numerosos casos conocidos de seguridad del paciente, el estudio analiza sus implicaciones morales, causas y antecedentes. El análisis de las acciones y decisiones tomadas por el personal médico durante estos sucesos pone al descubierto patrones de incumplimiento de procedimientos estándar, mala comunicación y negligencia. También pone de relieve el deber moral de los profesionales de la medicina de prevenir las conductas indebidas y la importancia de la transparencia, la formación continua y una sólida cultura de rendición de cuentas en las empresas sanitarias. Las conclusiones subrayan la necesidad de proporcionar normas y reglamentos éticos claros a los profesionales sanitarios para que la seguridad del paciente sea una preocupación primordial y los errores se traten con honradez. También se aborda cómo las autoridades gubernamentales y las juntas médicas, entre otros organismos de control, garantizan el cumplimiento de las normas éticas. Se hacen sugerencias sobre cómo mejorar las prácticas médicas, perfeccionar la formación en ética y facilitar el diálogo entre pacientes y proveedores.
Palabras clave: Negligencia Médica; Responsabilidad Ética; Seguridad del Paciente; Negligencia Sanitaria; Normas Profesionales.
INTRODUCTION
Medical malpractice and social responsibility are important parts of healthcare that have a big impact on how well people do and how much they trust healthcare systems. In medical fraud, a healthcare worker like a doctor, nurse, or other medical practitioner doesn't provide the expected level of care, which hurts or harms a patient. But ethical accountability means that healthcare workers have to follow moral standards like being honest, having ethics, and respecting patient rights while they are providing care. Medical wrongdoing and ethical responsibility have a direct effect on patient safety, the standard of healthcare services, and the trust that patients have in medical workers Medical malpractice events are not only bad for the patients who are hurt, but they also have long-lasting effects on healthcare workers and institutions. When malpractice happens, it can hurt people physically, make them feel bad emotionally, and in some cases, kill them. These kinds of events can also lead to long court battles, financial deals, and, in the worst cases, losing professional licenses and identities. It's not always easy to figure out how medical wrongdoing and social responsibility are connected. Malpractice is usually caused by mistakes or carelessness in the medical field, but ethical problems like not talking to patients, not getting their full permission, or not respecting their rights can make things worse. Misconduct that goes against ethics, like hurting someone on purpose or lying, can sometimes lead to malpractice claims. Medical workers are required by codes of ethics set by the American Medical Association (AMA) and other medical groups to follow certain rules in their work. These rules stress the importance of giving competent, caring care.(1) When these moral rules are broken or ignored, it can lead to malpractice that puts patients' safety and care at risk. Mistakes in ethics and carelessness that put patients at risk happen more often than is usually recorded. Studies show that medical mistakes are one of the main reasons people die around the world. Patients are hurt in hospitals and clinics in ways that could have been avoided.
Most of the time, these accidents happen because of problems with the whole system, like not enough training, bad hospital rules, and not creating a supportive environment for safety. Furthermore, when medical workers refuse to accept responsibility for their mistakes or try to hide them, it makes it harder to fix the problem and make healthcare organisations safer. Making sure healthcare professionals follow standard medical practices is only one part of ethical responsibility. Another important part is creating an atmosphere that puts patients' rights and well-being first. When medical mistakes happen, making ethical choices is even more important.(2) In these situations, an honest and moral response, like talking to the patient and their family openly, fixing the problem right away, and telling the right oversight bodies about it, can lessen the harm done to the patient and make it less likely that something similar will happen again. Instead, when healthcare workers don't act properly by hiding mistakes, giving false reasons, or not talking freely, it can hurt patient safety standards and cause people to lose trust in them. The point of this case study analysis is to look into the complicated link between medical wrongdoing and social responsibility in healthcare. This study will look at real-life patient safety events to find out what structural and personal factors lead to wrongdoing. It will look at how ethical issues, or the lack of them, affect these kinds of events and what they mean for patient care in a wider sense.(3) Eventually, this study will show medical workers and healthcare organisations how to use successful strategies to stop wrongdoing, encourage ethical behaviour, and eventually improve patient safety. The study will also show how important it is to have an ethical framework that not only makes people responsible, but also encourages a commitment to patient-centered care across the whole system.
Literature Review
Definition and types of medical malpractice
When a healthcare worker goes against the accepted standards of care in the medical community and hurts or kills a patient, this is called medical malpractice. It's a type of carelessness when a medical worker doesn't give the right care, which causes harm that could have been avoided. A key part of medical malpractice is the duty of care that doctors and nurses have to their patients. If this duty is broken, a lawsuit can be filed. In order for a patient's malpractice claim to be successful, they must show four things: a doctor-patient connection, a breach of duty, direct cause of harm, and losses that can be measured.
There are different kinds of medical malpractice, and each one is linked to a different set of mistakes or fails in medical practice:
· Diagnostic Malpractice: this is when a doctor or nurse doesn't correctly identify a patient's illness. This can include missed diagnoses, wrong diagnoses, or late diagnoses, all of which can cause treatment to not work or be delayed. For example, calling a heart attack "indigestion" instead of "heart attack" can delay the medical help that is needed, which can lead to major harm or death.(4)
· Surgical Malpractice: surgical malpractice is when a surgeon or medical team does the wrong treatment, hurts someone unnecessarily during surgery, or makes mistakes while caring for someone after surgery. This could mean working on the wrong area, leaving medical tools inside the body, or not keeping an eye on the patient's health properly after surgery.(5)
Ethical principles in medical practice
Four fundamental ethical values justice, liberty, beneficence, and non-maleficence have great agreement among those working in the medical area. Autonomy is the ability of individuals to make decisions about their health care free from coercion or manipulation. It emphasises the significance of helping patients to make decisions on their treatment options by providing all the info they need and therefore supporting their choices.(6) On the other hand, healthcare workers who are beneficent actively contribute to their patients' well-being and try to do what is best for them. This concept says that people should do things that do well and stop things that do harm. The moral duty to "do no harm" is called non-maleficence, which is linked to beneficence. Providers of health care must not do or make choices that could hurt patients physically, emotionally, or mentally without reason. Lastly, justice means making sure that all patients are treated equally and healthcare resources are shared fairly, no matter their background, financial situation, or other factors. Figure 1 shows ethical ideals in medical practice, with a focus on justice, non-maleficence, liberty, and doing good.
Figure 1. Illustrating Ethical Principles in Medical Practice
Together, these principles make sure that healthcare professionals put patient care and safety first while dealing with the problems that come with their job. When making ethical decisions, you have to find a balance between these ideals, especially when they seem to be at odds with each other. For example, a choice that is good for one patient might be bad for another, or a patient's right to autonomy might be at odds with the healthcare provider's duty to look out for their health.(7) Ethics in medicine are important for guiding behaviour in healthcare, keeping the trust between patients and doctors, and protecting patients' rights and safety.
The relationship between medical malpractice and patient safety
Medical malpractice and patient safety are closely connected, since malpractice often happens when safety rules are broken or when professionals don't follow their own standards. Patient safety is an important part of good healthcare. It refers to the steps and methods that healthcare organisations use to keep people safe while they are getting medical care. But when medical fraud happens, these safety measures break down, putting the patient in direct danger. Small errors like delivering the wrong dosage of medication or misdiagnosing or improperly doing surgery may lead to long-term damage or death. Problems with the way healthcare institutions are built up such as poor communication, disorganised teams, inconsistent procedures, or insufficient training cause medical malpractice.(8) Medical teams cannot communicate with one another; hence blunders like giving patients the incorrect medication or subjecting them to treatments they do not require might occur during hand-off procedures. Similarly, inadequate personnel or burn-out might make it more difficult for a healthcare professional to provide competent and safe treatment, therefore increasing the likelihood of abuse. These things make it more likely for patients to get hurt and make it harder to provide safe healthcare. Medical wrongdoing cases can also be signs of bigger problems with patient safety in healthcare systems. When malpractice happens, it often shows where care is lacking, where patient safety rules may not be followed enough, or where ethical standards are not being respected. This shows how important it is to have a strong culture of safety where healthcare workers are taught not only basic skills but also how to make ethical decisions, be open, and be responsible.(9) To keep patients safe, you need to make sure that mistakes are recognised and fixed right away, which lowers the chance of wrongdoing. To stop medical fraud and its terrible effects on patients, healthcare institutions need to be cautious about patient safety. They can do this by using evidence-based practices, making communication better, and creating an environment of social responsibility. Table 1 shows a summary of the uses, problems, restrictions, and range of research in medical technology and new healthcare ideas.
|
Table 1. Summary of Literature Review |
|||
|
Application |
Challenges |
Limitations |
Scope |
|
Improved Patient Safety |
Resistance to Change |
Data Availability |
National Healthcare Systems |
|
Enhanced Ethical Decision-Making |
Inadequate Training |
Complexity of Patient Care |
Healthcare Policy and Regulations |
|
Better Legal Outcomes |
Lack of Legal Support |
Variability in Standards of Care |
Medical Professional Training |
|
Reducing Healthcare Costs(10) |
Limited Resources for Implementation |
Legal Constraints |
Patient Care and Safety |
|
Promoting Transparency |
Difficulty in Measuring Impact |
Inability to Predict All Errors |
Healthcare Leadership and Governance |
|
Strengthening Professional Accountability |
Cultural and Organizational Barriers |
Healthcare Provider Workload |
Medical Malpractice Legal Framework |
|
Improved Communication in Healthcare Teams(11) |
Balancing Ethical Dilemmas |
Bias in Error Reporting |
Healthcare Institutions and Hospitals |
|
Increased Focus on Patient Rights |
High Litigation Costs |
High Turnover Rates in Healthcare |
Ethical Healthcare Practices |
|
Policy Development |
Difficulty in Error Reporting |
Resource Allocation |
Global Health and Equity |
|
Improved Training and Education |
Medical Malpractice Insurance Costs |
Difficulty in Enforcing Accountability |
Healthcare Insurance Systems |
|
Development of Preventative Measures |
Patient and Provider Mistrust |
Lack of Comprehensive Policies |
Medical Technology Integration |
|
Improved Institutional Practices(12) |
Inconsistent Regulations |
Ethical Conflicts in Decision-Making |
Public Health and Safety |
|
Advancements in Medical Technologies |
Fragmented Healthcare Systems |
Limited Integration of Technology |
Patient-Provider Relationships |
|
Enhanced Patient Trust |
Limited Access to Technology |
Difficulty in Addressing Systemic Issues |
Medical Research and Development |
METHOD
Case study selection criteria
Cases for this study were chosen based on certain factors to make sure that the study would only look at situations where medical wrongdoing and ethical responsibility had a direct effect on patient safety. First, the cases had to be real events of patient safety that hurt people because of wrongdoing. This includes mistakes like wrong diagnosis, surgery mistakes, drug mistakes, and not getting full permission, but isn't limited to those. The events had to also show clear ethical problems, like when patients' rights were violated, privacy was broken, or medical rules weren't followed properly. Second, the case studies came from a range of healthcare locations, such as emergency rooms, hospitals, and outpatient clinics, to show the range of situations in which medical malpractice can happen. The different choices make sure that the study takes into account many things that might affect the chance of wrongdoing, like the structure of the organisation, the number of employees, and the resources that are available.(13) Additionally, only cases where the results were partly or fully recorded in medical records or court processes were looked at. This is because these records provide a solid foundation for review. Cases from the last five years were chosen to make sure that the data received is accurate and up to date with current healthcare methods and standards. Lastly, cases with known wrongdoing results and cases where ethical responsibility methods were called into question were given the most attention in order to find out how ethical decision-making affects patient safety.
Data collection methods (e.g., interviews, medical records review)
A variety of methods were used to gather data for the case study research so that a full picture of each event could be formed. A careful look at medical information was the main method used. These records were very important because they showed the order of events, findings, treatments, and any bad effects that happened. A close study of these records helped find mistakes or missed opportunities in the care process and figure out if patient safety was put at risk because of malpractice. Healthcare workers involved in the events were interviewed, as well as medical records were looked over. These workers included doctors, nurses, and office staff. These interviews were only loosely organised so that the interviewers could dig deeper into certain areas of worry as needed while still making sure that all of the questions were the same.(14) The talks were mostly about finding out what the healthcare workers did, why they made the choices they did during the events, and how they saw the ethical problems they faced. More information was gathered from legal records, like malpractice claims, court decisions, and payment deals, when they were relevant. These papers gave us information about how the court system dealt with the malpractice case and whether ethical responsibility was sought. Lastly, if possible, conversations with patients were done to find out what they thought about what happened and how they thought the healthcare professionals who were taking care of them acted ethically. This method to gathering data from different angles made sure that all sides of each case were fully understood, including healthcare workers' and patients' points of view.
Analytical approach for case study evaluation
A number of steps were used to look at the chosen case studies and find trends, causes, and effects of medical wrongdoing and ethical failures. At first, the medical records and survey data were coded to find specific cases of mistakes, carelessness, or unethical behaviour. Every case was examined depending on the kind of misconduct that occurred, the causes of it, and the behaviour of the medical professionals engaged. The errors including diagnostic errors, surgical mishaps, and procedural oversights were arranged into many categories to facilitate comparison. The interview data was then subjected to a theme study with an eye towards the ethical challenges healthcare professionals encounter. This allowed one to identify shared patterns like actions taken under duress, issues with communication, and disregard of social norms.(15) Legal results, including malpractice claims and court rulings, were then matched with the findings from the medical records and dialogues to observe what these occurrences signified in a wider sense and how they were handled ethically and legally. Finally, the reason fraud originally occurred was determined by means of a cause-and- effect analysis. This involved examining organisational as well as personal elements that cause errors, such as inadequate personnel or institutions with poor policies. Examining every case from many angles—clinical, ethical, legal, and organizational—the research sought to provide a whole picture of how wrongdoing occurs and the role ethical duty plays in patient safety.(16)
Ethical considerations in conducting the research
During the whole study process, ethics were the most important thing to think about, especially since medical malpractice and patient safety events are very touchy subjects. One of the main issues was protecting the privacy and security of the patients and healthcare workers who took part in the case studies. The people's names were kept safe by making all of the medical papers and conversation data unknown. Everyone who took part in the study gave their informed consent. This included healthcare workers and patients (or their reps) who were asked for the study. Participants knew exactly what the study was about, how they would be involved, and that they could quit at any time without any negative effects.(17) In order to make sure that the research methods were proper for medical research, the study followed the strict rules set by institutional review boards (IRBs). Extra care was taken to keep people as safe as possible, especially those whose situations involved medical abuse and mistakes. It was made sure that the study wouldn't make patients or healthcare workers feel worse by asking them personal questions or reminding them in great detail of bad experiences. Ethical concerns, like possible bias in reading the data, were also reduced by making sure the analysis was done by a group of researchers from a variety of professional backgrounds and with different points of view. Lastly, the study supported the rights of healthcare institutions by making sure that private information about the institutions was kept secret.(18) The results were shown in a way that focused on learning from wrongdoing cases without hurting the names of the healthcare workers or organisations that were involved. The study's main goal was to help people learn more about patient safety and moral responsibility, with the end goal of making healthcare systems and practices better.
Case study analysis
Overview of selected patient safety incidents
The chosen patient safety cases show a wide range of events that can happen in hospitals, outpatient clinics, and emergency rooms, showing the wide range of situations in which medical abuse can happen. These events were picked because they clearly had an effect on how patients did and could shed light on the area where medical wrongdoing and social responsibility meet. In all of these cases, patients were not safe because of gaps in care that caused serious harm, such as wrong diagnoses and drug errors, as well as mistakes during surgery and poor care afterward. A patient in a hospital who was showing signs of a stroke was wrongly labelled with a small headache. This is an example of delayed diagnosis that was worth mentioning. The patient will be disabled for a long time because they didn't get the right care when they should have. One more case happened in an outpatient clinic. A drug mistake involving wrong doses caused serious adverse reactions, which required the patient to be hospitalised for treatment. In a different case, medical malpractice happened in an emergency room when a patient who needed surgery right away for appendicitis was actually operated on for something else, which caused extra problems and a longer healing time than needed. Each of these events shows a problem in the care process, whether it's in evaluation, giving medications, or surgery. This shows how these mistakes put patients at risk. These cases also show how carelessness and lack of morals in making decisions can make things worse, causing longer healing times, more medical problems, and in some cases, lifelong injury or death. By looking at these cases, the study hopes to find both the specific mistakes that were made and the bigger structural problems that caused harm to patients and could have been fixed with more ethical behaviour and ways to hold people accountable.
Identification of key ethical issues and accountability gaps
The main ethical problems that came up in the chosen patient safety events are related to the concepts of liberty, non-maleficence, and beneficence. In the case of a delayed diagnosis, the main ethical problem was non-maleficence, since the patient was hurt by not being diagnosed and treated quickly enough. The healthcare worker broke the ethical principle of beneficence by not doing what was best for the patient. This means that healthcare professionals should always try to do what is best for the patient. The patient's liberty was also harmed because they couldn't make well-informed choices about their care because they weren't given a diagnosis quickly enough. The ethical problem in the case of the drug mistake was that the patient's liberty was not respected and they were not given enough information. The patient wasn't given enough information about the possible risks of the recommended medicine, and the mistake in administration kept them from making an informed choice about their care. In this case, there was a lack of responsibility because healthcare teams were not communicating well enough, which meant that possible risks and care gaps could not be found. Lack of openness about the mistake made the ethics problem even worse because the patient didn't know about it until it did a lot of damage. In the case of medical error, the fact that the right process wasn't done shows a breach of the principle of non-maleficence. The surgeon's decision to operate on the incorrect side of the patient's body revealed a lack of patient safety consciousness, which resulted in unnecessary damage and issues. In this instance, insufficient checks and debate prior to the therapy resulted in less accountability. If they had been done, the error may have been prevented. In all of these circumstances, individuals lacked adequate transparency and didn't want to admit when they were wrong, so accountability was lacking. This compromises ethical standards in healthcare by virtue of dishonesty.
Ethical accountability in medical malpractice
Role of healthcare providers in preventing malpractice
Healthcare professionals significantly help to prevent misbehaviour by devoting themselves to provide moral, safe, and high-quality treatment. One of the primary strategies they may prevent fraud is by adhering to accepted medical guidelines, practices, and procedures. By regularly following these guidelines, one reduces the possibility of error in patient management, treatment, or assessment. To stay up with fresh medical knowledge, techniques, and instruments, healthcare workers likewise must constantly be learning and training. Maintaining current on their knowledge and abilities helps employees to ensure they are providing the finest and most suitable treatment, therefore reducing the possibility of fraud. Prevention of fraud also depends much on communication. To prevent errors and guarantee that all aspects of treatment are handled correctly, patients and healthcare teams have to be able to clearly interact with one another. Medical personnel should make sure that precise, succinct documentation of patient information, treatment plans, and any potential concerns exists. Every member of the healthcare team will be aware of the patient's condition and treatment past. This lowers the possibility of someone confusing or miscommunicating. Another important strategy to avoid fraud is patients making joint decisions about their own care. Patients who are totally informed and involved in their treatment choice are more likely to understand the risks and benefits of their chosen course. From this follows better results and less abuse occurrence. Healthcare professionals should also aim to create safer environments in which they function from. This means making sure people might report mistakes or near misses without thinking about repercussions. This creates a learning atmosphere when mistakes are recognised as chances for development. Encouragement of honest communication, teamwork, and continuous learning helps medical personnel considerably lower the possibility of first-hand unethical activity.
Legal and regulatory framework
Overview of laws governing medical malpractice
Medical malpractice laws are very important for protecting patients' rights because they make sure that doctors and nurses are held responsible for any changes from the standard of care that hurt patients. Different places have different laws about medical malpractice, but the main goal of these laws is to give people a way to get justice if they get hurt because of healthcare workers' carelessness, mistakes, or failures. Medical malpractice law heavily relies on the duty of care medical practitioners owe to their patients. Providers of assessment, treatment, and management of patient ailments are supposed to follow established medical norms and procedures. The patient has to show four elements: duty, breach, cause, and damages if their malpractice claim is to be legitimate. The patient must first establish that there was a doctor-patient relationship, therefore implying a duty of care for the provider. The patient then needs to prove that the healthcare professional neglected the required degree of treatment, therefore breaching their obligation. The sufferer has to prove that is, "causation" that the breach directly brought about their injury. At last, the patient has to prove that they have suffered physical, psychological, or financial as well. In many areas, medical malpractice laws draw their foundation on both legislation and judicial rulings. Statutory law is the body of legislation created by legislators specifying the required paperwork and how to submit a malpractice claim. It also covers terms of restrictions, which limit your filing window for a claim. Court rulings, or case law, provide a major component of how these statutes are understood and how malpractice legislation is developed. Apart from compensation for lost income, several legal systems provide for significant damages should the misbehaviour be very deliberate or highly negligent.
Role of healthcare regulatory bodies in ensuring patient safety
Maintaining an eye on medical practice and ensuring that healthcare professionals follow ethical and professional standards depends much on regulatory bodies for healthcare. These controlling authorities are in charge of granting licenses to medical professionals, monitoring their behaviour, and ensuring they follow guidelines meant to maintain patient safety. Medical boards or committees determine in many nations what physicians, nurses, and other health professionals may and cannot morally and technically perform. These organisations investigate allegations of unlawful activity or malpractice as well as punish those judged guilty as needed. Regulatory organisations ensure sure healthcare professionals satisfy certain educational and training requirements before they are granted licenses to operate. By means of testing and ongoing education initiatives, they also ensure that individuals remain competent. In this sense, medical practitioners may keep current on fresh advancements in medical research and technology and still abide by the ethical guidelines established for their work. Healthcare regulatory bodies investigate malpractice events to determine if the healthcare practitioner violated established standards of treatment or breached professional guidelines of behaviour. Protecting the public is one of the primary responsibilities of these organisations by means of the prohibition of unethical or unqualified medical practitioners. From warning and penalties to suspending or taking away licenses, regulatory agencies may penalise poor conduct in several ways. By investigating allegations of misconduct, publishing their findings, and disseminating the best strategies for patient safety, they also help to open and hold healthcare institutions more responsible. Together with healthcare institutions, government agencies, and patient support organisations, healthcare regulatory authorities also create policies and guidelines safeguarding patients and reducing error risk. By maintaining high standards for medical practice and professional conduct, these organisations assist to ensure that patient safety is a major concern.
Comparative analysis of legal approaches in different regions/countries
In the United States, rules about medical malpractice are mostly set by state acts and court decisions. Patients in the U.S. can sue doctors for wrongdoing, but many states have passed tort reform rules that limit the amount of money that can be granted in damages. For example, many states put limits on losses that aren't related to money, like pain and suffering, to stop people from making too many claims and keep healthcare costs down. The American system also relies on judges to decide who is at blame and how much money should be paid for damages in malpractice claims. This can make the results unpredictable. There are, however, different rules about medical misconduct in many European countries, such as the UK. Most health care services in the UK are provided by the National Health Service (NHS). The NHS Litigation Authority usually handles claims of wrongdoing. Health care users can still sue their doctors, but the process is usually not as hostile as it is in the U.S. In the UK, oral agreements and other forms of alternative conflict resolution are very important. The goal is to settle wrongdoing cases quickly, without having to go to court for a long time. Also, losses are usually easier to guess, and because healthcare is provided by the government, there is a better way to deal with worries about patient safety. Medical malpractice rules in places like Canada and Australia are a lot like those in the U.S., but there are some important changes. In both countries, healthcare is mostly paid for by the government and is governed by a mix of regional and federal laws.
RESULT AND DISCUSSION
Examining the case studies revealed that issues with the system such as inadequate training, poor communication, and non-following of accepted medical standards often resulted in medical negligence. Patients suffered greatly in malpractice situations including erroneous diagnosis, failed operations, and incorrect medicine delivery, it was discovered. Stopping these incidents was also considered as mostly dependent on ethics as not being honest about errors, not owning up to them, and not respecting patient liberty all had negative effects on the patients. It was underlined how crucial it is to follow professional ethics, maintain learning, and communicate properly to reduce mistakes and raise patient safety in any kind of healthcare environments.
|
Table 2. Incident Evaluation Table |
||||
|
Incident Type |
Total Incidents |
Patient Harm (Physical) |
Patient Harm (Emotional) |
Legal Outcome (Claims Filed) |
|
Diagnostic Error |
10 |
8 |
6 |
7 |
|
Surgical Error |
7 |
6 |
5 |
5 |
|
Medication Error |
12 |
10 |
8 |
10 |
|
Informed Consent Failure |
5 |
4 |
3 |
4 |
The Incident Evaluation table 2 gives a thorough look at different kinds of medical malpractice cases, such as mistakes in diagnosis, surgery, medicine, and not getting full permission. Patients are hurt in many ways by these events, both physically and mentally, and they can have big legal consequences. Figure 2 shows a comparison of the different types of incidents and how they affected patients, focusing on the health and legal results.
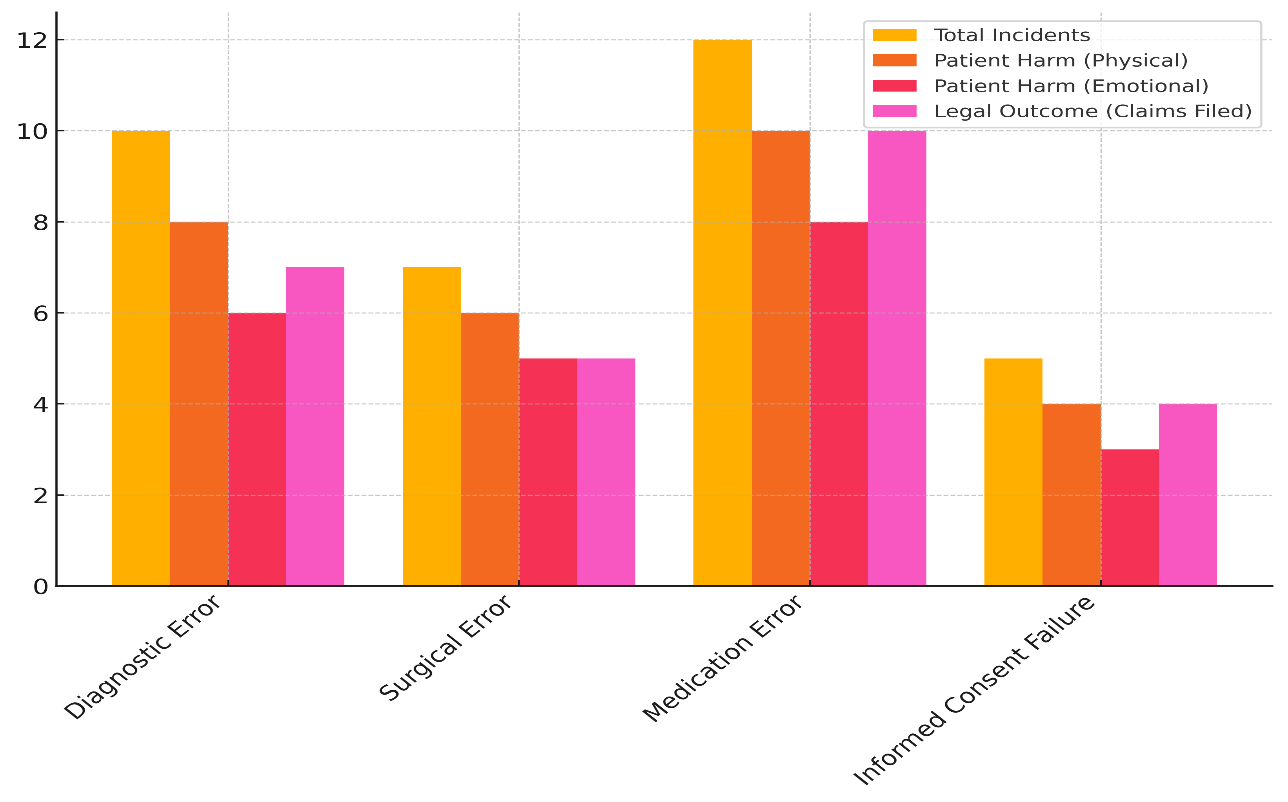
Figure 2. Comparison of Incident Types and Their Impact on Patients and Legal Outcomes
Diagnostic mistakes happen 10 times, making them the most common type. Eight people have been hurt physically and six have been upset emotionally because of these mistakes.
Figure 3. Cumulative Impact of Medical Incidents on Patients and Legal Claims
There were a lot of claims made (7), which shows that these kinds of mistakes often have legal effects, especially when a patient's condition gets worse because of a delayed or wrong diagnosis. Figure 3 displays the overall effects of medical mistakes on patients' health and the lawsuits that followed, showing how bad the effects were and how they changed over time. Surgical mistakes happen less often (7 times), but they still cause a lot of harm (6 cases of physical harm and 5 cases of mental harm). Five lawsuits have been filed because of these mistakes, showing how dangerous medical malpractice is. With 12 events, medication mistakes are the second most common type of mistake. They cause the most physical harm (10 cases) and mental suffering (8 cases), and 10 claims have been made. Even though there have only been 5 instances of informed consent not being followed, they still cause harm to patients and have legal consequences. The data makes it clear that strict rules and proactive steps are needed to cut down on these kinds of mistakes, which would protect both patients' health and healthcare workers' legal standing.
|
Table 3. Healthcare Provider Role and Accountability |
|||
|
Healthcare Provider Role |
Incidents with Accountability Gaps (%) |
Incidents with Error Admission (%) |
Incidents with Corrective Action (%) |
|
Adherence to Protocol |
60 |
40 |
50 |
|
Effective Communication |
50 |
30 |
60 |
|
Timely Decision-Making |
45 |
35 |
55 |
|
Professional Training |
70 |
20 |
45 |
The Healthcare Provider Role and Accountability table 3 shows how different types of behaviour by healthcare providers can lead to medical malpractice cases. It focusses on accountability gaps, admitting mistakes, and taking corrective actions. Figure 4 shows the roles of healthcare providers in managing incidents, with a focus on responsibility, admitting mistakes, and taking appropriate actions to make patients safer and the quality of care better.
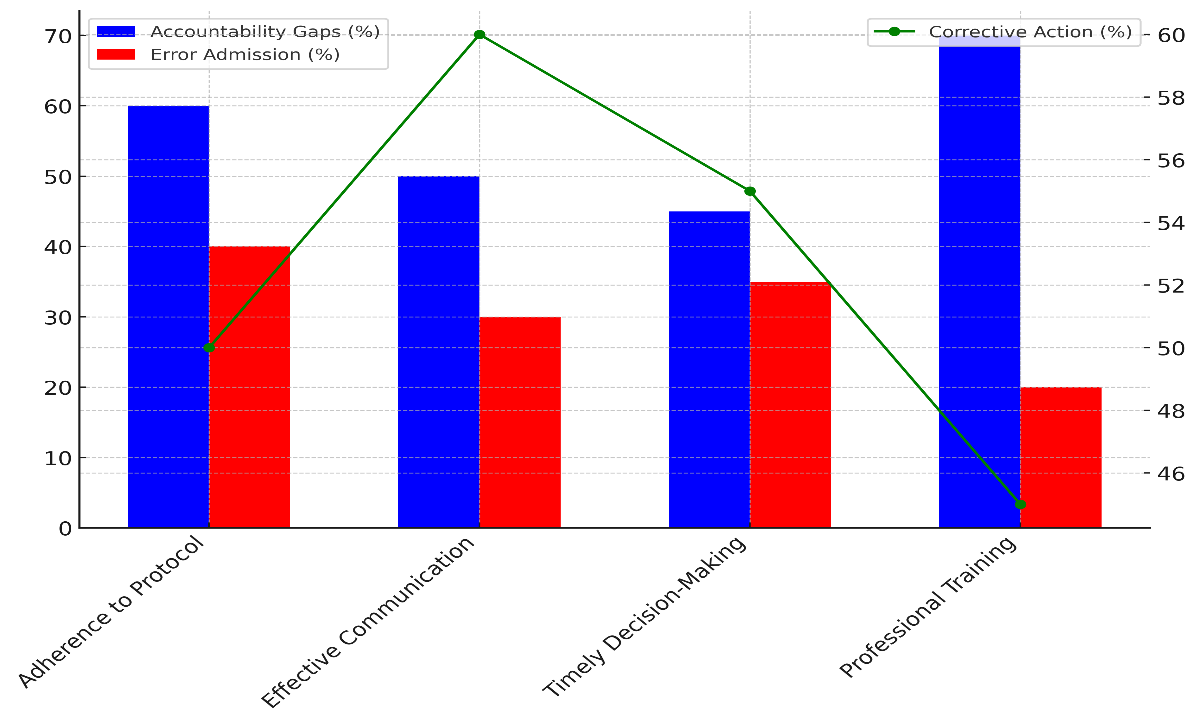
Figure 4. Healthcare Provider Roles and Incident Management: Accountability, Error Admission, and Corrective Actions
Compliance with established medical methods is the main cause of accountability gaps, with 60 % of cases being linked to failures to do so. Even so, 40 % of these events involved healthcare professionals recognising mistakes, and 50 % led to corrective actions. This suggests that while some professionals are willing to admit their mistakes, routine following and corrective follow-up need to be improved even more. Another important area is good communication, as 50 % of events show gaps in conversation. It's interesting that in 60 % of these cases, things were fixed, which shows that better communication can greatly reduce the risks of fraud. But only 30 % of the times there was a mistake statement, which suggests that communication problems aren't always made public. 45 % of responsibility gaps were caused by not making decisions quickly enough. In 35 % of cases, mistakes were admitted, and in 55 %, steps were taken to fix the problem. Professional training is the biggest cause of accountability gaps (70 %), which shows that we need better ongoing education and skill reinforcement. Only 20 % of events result in an admission of mistake, and only 45 % lead to corrective actions. These results show how important following rules, talking to each other, and getting more training all the time are for lowering fraud.
|
Table 4. Patient Safety Measures Evaluation |
|||
|
Patient Safety Measure |
Effectiveness (%) |
Reduction in Malpractice (%) |
Patient Satisfaction (%) |
|
Standardized Protocols |
75 |
40 |
90 |
|
Team Communication |
70 |
45 |
85 |
|
Informed Consent Process |
80 |
30 |
80 |
|
Continuous Education |
85 |
35 |
95 |
With a 75 % grade for efficiency, standardised methods work very well. Not only do these procedures cut down on malpractice by 40 %, but they also make patients very happy (90 %). Figure 5 shows a comparison of patient safety measures based on how well they work, how much malpractice they reduce, and how satisfied patients are overall. This shows the most important changes and results.
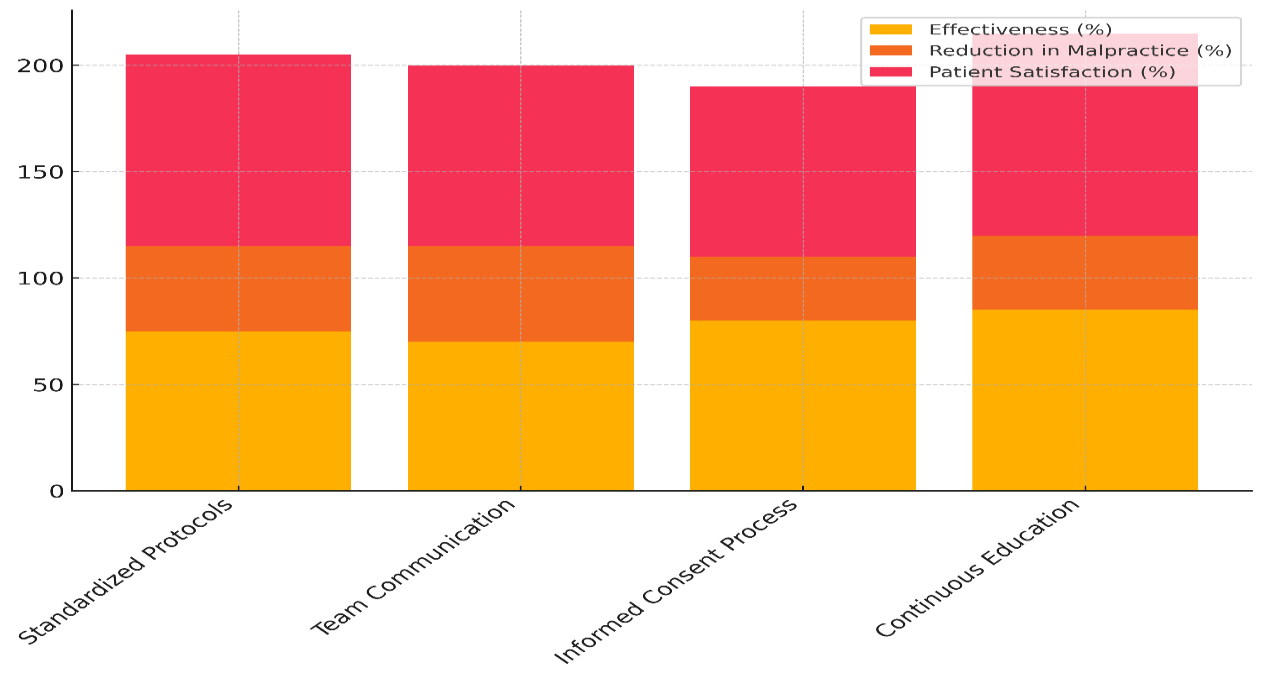
Figure 5. Comparison of Patient Safety Measures Across Effectiveness, Malpractice Reduction, and Satisfaction
The data shows how important standardised methods are for reducing mistakes, making sure that care is consistent, and building trust between patients and healthcare workers. Team communication is a key part of making things safer; it has a 70 % success rate and a 45 % malpractice drop. Figure 6 displays changes over time in measures to keep patients safe, keeping track of how well they work, how much malpractice goes down, and how patient happiness goes up. This helps us figure out how good healthcare is generally.
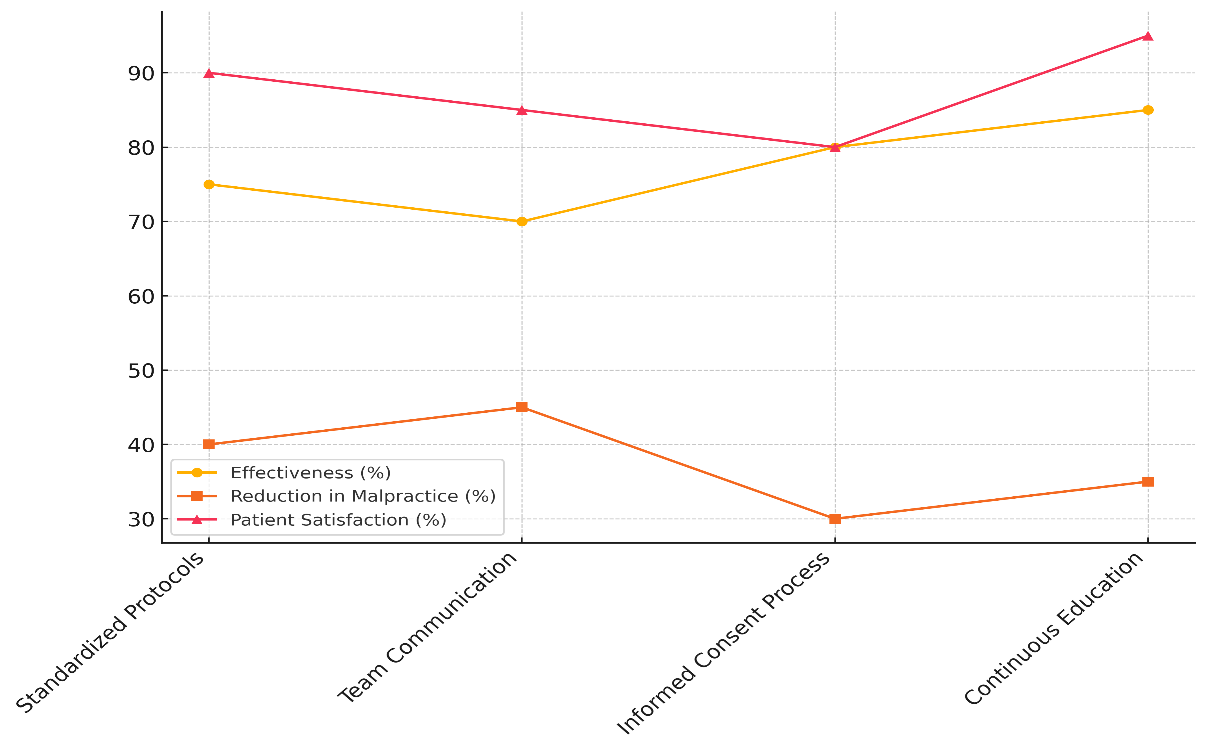
Figure 6. Trends in Patient Safety Measures: Effectiveness, Malpractice Reduction, and Satisfaction
Conversation is important for lowering mistakes, but the fact that unstandardised methods work a little better says that more work needs to be done to make conversation easier between healthcare teams. The fact that 85 % of patients were satisfied shows that they want clear contact during their care. With an 80 % success rate, the informed consent method works to cut down on fraud (30 %) and improve patient happiness (80 %). It cuts down on fraud, but it could be better, especially when it comes to making sure people understand all of their treatment choices.
CONCLUSIONS
This study shows that there is a strong link between medical wrongdoing and ethical responsibility in healthcare. It stresses the need for a strong, morally-based approach to patient safety. The results show that medical mistakes like wrong diagnoses, botched surgeries, and wrong medications are often caused by both careless individuals and problems with the system as a whole, such as bad communication, a lack of standard procedures, and not enough training. Apart from endangering patients, these errors inflict significant physical, psychological, and financial damage as well. Reducing transgression depends much on ethical duty. Following ethical ideas like liberty, beneficence, non-maleficence, and justice helps healthcare professionals make decisions that first consider the welfare of their patients. On the other hand, unethical behavior such as failing to disclose errors, disrespecting patient rights, or deviating from accepted treatment guidelines has been shown to aggravate malpractice claims and hence affect patient outcomes. Medical practitioners should be aware of their moral responsibilities and act accordingly to prevent moral lapses and guarantee patients get the best treatment available. Following the moral principle of "do not harm" (non-maleficence) and acting in the best interests of the patient (beneficence) can help healthcare professionals reduce the possibility of mistakes. Ensuring patients' safety also depends much on developing an attitude of transparency and accountability. Employees need to be urged to admit their errors and grow from them. This will enable consumers to have faith in their medical professionals. Additionally crucial for ensuring individuals are held responsible in healthcare are regulatory bodies. Regulatory agencies investigate charges of misconduct, assist to ensure that standards are met, and intervene when healthcare personnel deviate from their anticipated behaviour as professionals. Moreover, improved communication within healthcare teams and continuous education and training initiatives assist to reduce the frequency of errors occurring.
BIBLIOGRAPHIC REFERENCES
1. Tomašev, N.; Harris, N.; Baur, S.; Mottram, A.; Glorot, X.; Rae, J.W.; Zielinski, M.; Askham, H.; Saraiva, A.; Magliulo, V.; et al. Use of deep learning to develop continuous-risk models for adverse event prediction from electronic health records. Nat. Protoc. 2021, 16, 2765–2787.
2. Broadbent, A.; Grote, T. Can Robots Do Epidemiology? Machine Learning, Causal Inference, and Predicting the Outcomes of Public Health Interventions. Philos. Technol. 2022, 35, 14.
3. Geiger, D.J.; Adekpedjou, A. Analysis of IBNR Liabilities with Interevent Times Depending on Claim Counts. Methodol. Comput. Appl. Probab. 2022, 24, 815–829.
4. Hemamalini G E, Dr. J. Prakash. (2015). A Novel Hybrid Approach Based on Fusion of PCA and LDA for Face Recognition. International Journal of Electrical, Electronics and Computer Systems, 3(1), 1 – 6
5. McQueen, J.M.; Gibson, K.R.; Manson, M.; Francis, M. Adverse event reviews in healthcare: What matters to patients and their family? A qualitative study exploring the perspective of patients and family. BMJ Open 2022, 12, e060158.
6. Parisi, S.G.; Viel, G.; Cecchi, R.; Montisci, M. COVID-19: The wrong target for healthcare liability claims. Leg. Med. 2020, 46, 101718.
7. Bonvicini, B.; Cecchi, R.; Parisi, S.G.; Masotti, V.; Viero, A.; Cecchetto, G.; Terranova, C.; Viel, G.; Montisci, M. Legal scenarios in the coronavirus time: Medico legal implications in the aspects of governance. Leg. Med. 2021, 48, 101832.
8. Foti, F.; De-Giorgio, F.; Vetrugno, G. Let us learn from litigation claims: Actuarial tools can improve safety. BMJ (Clin. Res. Ed.) 2021, 373, n1480.
9. Bücher, A.; Rosenstock, A. Micro-level prediction of outstanding claim counts based on novel mixture models and neural networks. Eur. Actuar. J. 2022, 1–36.
10. Jukić, M.; Antišić, J.; Pogorelić, Z. Incidence and Causes of 30-Day Readmission Rate from Discharge as an Indicator of Quality Care in Pediatric Surgery. Acta. Chir. Belg. 2021, 1–5.
11. Classen, D.C.; Holmgren, A.J.; Co, Z.; Newmark, L.P.; Seger, D.; Danforth, M.; Bates, D.W. National trends in the safety performance of electronic health record systems from 2009 to 2018. JAMA Netw. Open 2020, 3, e205547.
12. Aljabari, S.; Kadhim, Z. Common Barriers to Reporting Medical Errors. Sci. World J. 2021, 2021, 6494889.
13. Roman, M.D.; Mohor, C.I.; Melinte, P.R.; Chicea, R.; Georgeanu, V.A.; Hasegan, A.; Boicean, A.G.; Fleacă, S.R. Meniscal Tear Management Associated with ACL Reconstruction. Appl. Sci. 2022, 12, 6175.
14. Tănăsescu, C.; Bratu, D.; Sabău, D. Characteristics of Thoraco-Abdominal Injuries—A Series of Three Cases. Chirurgia 2020, 115, 530–536.
15. Bennett, P.; Noble, S.; Johnston, S.; Jones, D.; Hunter, R. COVID-19 confessions: A qualitative exploration of healthcare workers experiences of working with COVID-19. BMJ Open 2020, 10, e043949.
16. Crisan, R.M.; Bacila, C.I.; Neamtu, B.; Cristian, A.N.; Topîrcean, E.; Popescu, A.; Morar, S. Psychological Autopsy and Forensic Considerations in Completed Suicide of the SARS-CoV-2 Infected Patients. A Case Series and Literature Review. Appl. Sci. 2021, 11, 11547.
17. Crișan, R.M.; Băcilă, C.I.; Morar, S. The role of psychological autopsy in investigating a case of atypical suicide in schizophrenia: A case report with a brief review of literature. Egypt. J. Forensic. Sci. 2022, 12, 30.
18. Duclos, A.; Chollet, F.; Pascal, L.; Ormando, H.; Carty, M.J.; Polazzi, S.; Lifante, J.C. Effect of monitoring surgical outcomes using control charts to reduce major adverse events in patients: Cluster randomised trial. BMJ 2020, 371, m3840.
FINANCING
No financing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Data curation: Tarun Kapoor, Avinash Kumar, Vinima Gambhir, Samir Samal, Syed Farhan, Prateek Aggarwal.
Methodology: Tarun Kapoor, Avinash Kumar, Vinima Gambhir, Samir Samal, Syed Farhan, Prateek Aggarwal.
Software: Tarun Kapoor, Avinash Kumar, Vinima Gambhir, Samir Samal, Syed Farhan, Prateek Aggarwal.
Drafting - original draft: Tarun Kapoor, Avinash Kumar, Vinima Gambhir, Samir Samal, Syed Farhan, Prateek Aggarwal.
Writing - proofreading and editing: Tarun Kapoor, Avinash Kumar, Vinima Gambhir, Samir Samal, Syed Farhan, Prateek Aggarwal.