doi: 10.56294/mw2024506
ORIGINAL
Advancing Patient-Centered Care through AI-Driven Medical Informatics and Real-Time Health Data Analysis
Avanzar en la atención centrada en el paciente mediante la informática médica impulsada por la IA y el análisis de datos sanitarios en tiempo real
Swati Kemothi1
![]() *,
Sujayaraj Samuel Jayakumar2
*,
Sujayaraj Samuel Jayakumar2
![]() , Swarna Swetha Kolaventi3
, Swarna Swetha Kolaventi3
![]() , Pratyashi Satapathy4
, Pratyashi Satapathy4
![]() , Kollathur Sudheer5
, Kollathur Sudheer5
![]() , Gunveen Ahluwalia6
, Gunveen Ahluwalia6
![]() , Ansh Kataria7
, Ansh Kataria7
![]()
1School of Allied Health Sciences, Noida International University. Greater Noida, Uttar Pradesh, India.
2Forensic science, JAIN (Deemed-to-be University). Bangalore, Karnataka, India.
3Department of uGDX, ATLAS SkillTech University. Mumbai, Maharashtra, India.
4Department of Computer Science and Engineering, Siksha ‘O’ Anusandhan (Deemed to be University). Bhubaneswar, Odisha, India.
5Centre for Multidisciplinary Research, Anurag University. Hyderabad, Telangana, India.
6Chitkara Centre for Research and Development, Chitkara University. Himachal Pradesh, India.
7Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
Cite as: Kemothi S, Jayakumar SS, Kolaventi SS, Satapathy P, Sudheer K, Ahluwalia G, et al. Advancing Patient-Centered Care through AI-Driven Medical Informatics and Real-Time Health Data Analysis. Seminars in Medical Writing and Education. 2024; 3:506. https://doi.org/10.56294/mw2024506
Submitted: 10-10-2023 Revised: 12-01-2024 Accepted: 13-05-2024 Published: 14-05-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Swati Kemothi *
ABSTRACT
In the quickly evolving sector of healthcare, the marriage of artificial intelligence (AI) with medical technology has drastically revolutionised the way patient-centered care is given. By real-time health data analysis, AI-driven solutions enable healthcare professionals to provide more individualised, effective, proactive treatment. By means of its applications in real-time health data analysis and medical computing, this study explores how artificial intelligence might support patient-centered care enhancement. Big volumes of patient data including information from smart devices, clinical records, and medical images are handled by artificial intelligence algorithms including predictive analytics, natural language processing, and machine learning models. Along with helping clinicians make better judgements, these instruments increase patient involvement, happiness, and likelihood of excellent outcomes. The key advantage of artificial intelligence-driven medical informatics is that it can provide real-time patient health information to healthcare professionals so they may respond fast on new medical problems or probable hazards. Predictive models, for instance, may recommend certain treatment regimens, forecast the course of an illness, and identify potential issues before they become very major. Particularly for those who live in remote or poor regions, AI may also enable telemedicine and online monitoring systems, therefore helping to make healthcare more accessible. Moving the emphasis from reactive care to focused, preventive care helps AI-driven solutions empower individuals to take control of their own health. Better healthcare outcomes follow from simpler patient and healthcare worker collaboration made possible by combined use of artificial intelligence and medical computers. Using these technologies does, however, also present challenges like concerns about data security, the need for consistent procedures, and ensuring ethical usage of artificial intelligence in medical environments.
Keywords: Artificial Intelligence; Patient-Centered Care; Medical Informatics; Real-Time Health Data; Predictive Analytics.
RESUMEN
En el sector sanitario, en rápida evolución, la unión de la inteligencia artificial (IA) con la tecnología médica ha revolucionado drásticamente la forma de prestar una atención centrada en el paciente. Mediante el análisis de datos sanitarios en tiempo real, las soluciones basadas en la IA permiten a los profesionales sanitarios ofrecer un tratamiento más individualizado, eficaz y proactivo. A través de sus aplicaciones en el análisis de datos sanitarios en tiempo real y la informática médica, este estudio explora cómo la inteligencia artificial puede contribuir a mejorar la atención centrada en el paciente. Los grandes volúmenes de datos de pacientes, incluida la información procedente de dispositivos inteligentes, historiales clínicos e imágenes médicas, se manejan mediante algoritmos de inteligencia artificial que incluyen análisis predictivos, procesamiento del lenguaje natural y modelos de aprendizaje automático. Además de ayudar a los médicos a tomar mejores decisiones, estos instrumentos aumentan la participación del paciente, su felicidad y la probabilidad de obtener resultados excelentes. La principal ventaja de la informática médica basada en la inteligencia artificial es que puede proporcionar a los profesionales sanitarios información sobre la salud del paciente en tiempo real, de modo que puedan reaccionar con rapidez ante nuevos problemas médicos o probables riesgos. Los modelos predictivos, por ejemplo, pueden recomendar determinados regímenes de tratamiento, pronosticar el curso de una enfermedad e identificar posibles problemas antes de que se agraven. Sobre todo para quienes viven en regiones remotas o pobres, la IA también puede permitir la telemedicina y los sistemas de seguimiento en línea, contribuyendo así a hacer más accesible la asistencia sanitaria. Al pasar de la atención reactiva a la atención centrada y preventiva, las soluciones basadas en la IA ayudan a las personas a tomar el control de su propia salud. La simplificación de la colaboración entre el paciente y el personal sanitario, posible gracias al uso combinado de la inteligencia artificial y los ordenadores médicos, mejora los resultados de la asistencia sanitaria. Sin embargo, el uso de estas tecnologías también plantea retos como la seguridad de los datos, la necesidad de procedimientos coherentes y la garantía de un uso ético de la inteligencia artificial en entornos médicos.
Palabras clave: Inteligencia Artificial; Atención Centrada en el Paciente; Informática Médica; Datos Sanitarios en Tiempo Real; Análisis Predictivo.
INTRODUCTION
The advancement of technology in the last several decades has greatly affected the way medical approaches have evolved. Among this technology influencing the maximum is artificial intelligence (AI). Its miles altering the manner scientific professionals treat their sufferers. Affected person-targeted care which places each affected person's needs, desires, and beliefs first forms the muse of modern-day healthcare processes. But, given the complexity of healthcare and the increasing affected person statistics, we should find clean tactics to enhance consequences and remedy. Clinical technology pushed by way of synthetic intelligence and real-time health facts evaluation cooperates to improve affected person-focused remedy. Healthcare structures therefore emerge as more individualised, proactive, and efficient. To collect and compare substantial volumes of patient records, artificial intelligence-driven clinical informatics makes use of many numerous technology and methods together with machine learning (ML), natural language processing (NLP), and predictive analytics. These contraptions enable clinicians to make better judgements by using assisting them become aware of patterns, forecast fitness worries, and provide them with knowledge approximately the most desirable strategies of affected person remedy. a number of the many databases AI can sift are digital fitness records (EHRs), scientific imaging, genetic records, and real-time sensor records. This allows clinicians to peer a patient's health holistically. Combining many information sources enables scientific employees to absolutely apprehend an affected person's clinical beyond, residing instances, and contemporary state of fitness. Setting up and seeing so much information is one of the primary demanding situations dealing with healthcare nowadays. Healthcare professionals should cope with loads of information regularly no longer organised or maintained in different systems given so many digital fitness statistics, clever fitness gadgets, and mobile health packages.(1) By way of rapidly managing records and extracting insightful analysis that can guide physicians' decisions, artificial intelligence can help to address those challenges. This no longer handiest ensures that the remedy received is tailored for every affected person, considering their unique necessities and goals, however it additionally helps sufferers make better, more fast selections. By means of figuring out illnesses early, forecasting fitness dangers, and providing tailor-made remedy options, synthetic intelligence utilised in healthcare might also let sufferers get better remedy.
Predictive analytics, for example, may identify those who are very likely to develop long-term conditions like diabetes or heart disease, therefore enabling early treatment and prevention. Similarly, machine learning techniques may assist with trend discovery in medical images, therefore enabling clinicians to make quicker and more accurate diagnoses. Data from smart devices included in real-time health data analysis allows physicians to constantly monitor patients, therefore improving the treatment.(2) Doctors can detect how illnesses are worsening, handle issues, and make necessary treatment plan adjustments via real-time patient observation, thereby improving patient outcomes. AI-run solutions may also enable patients to be more engaged and content. Figure 1 illustrates how artificial intelligence-powered medical informatics may examine real-time patient data to improve treatment.
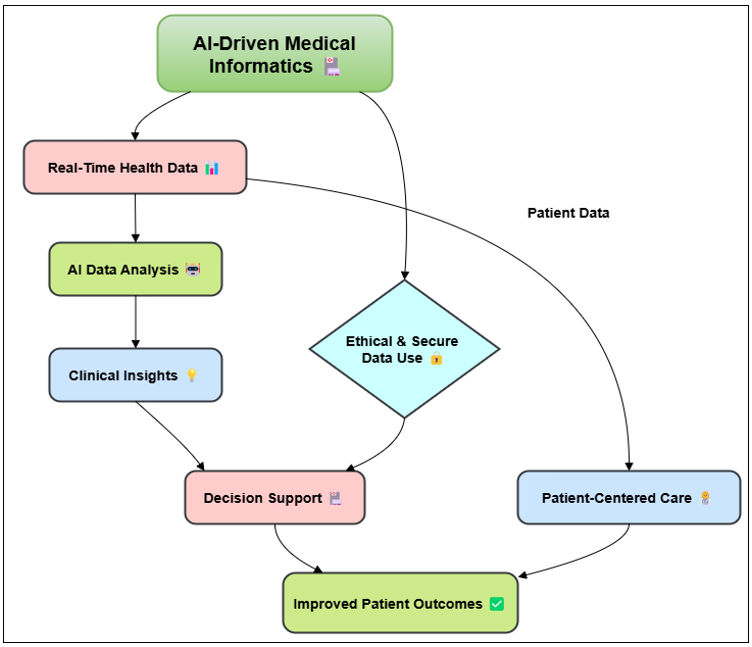
Figure 1. AI-Driven Medical Informatics and Real-Time Health Data Analysis
Through access to their health data and tailored recommendations via digital platforms, artificial intelligence empowers individuals to actively participate in managing their health. Managing a chronic illness particularly requires this as the greatest outcomes depend on keeping the patient active over time. AI may also let medical professionals keep an eye on patients' development, provide them more customised counsel, and improve their communication skills with regard to Patients and their care teams may benefit from this by working closer and with greater trust among one another. Although artificial intelligence-driven medical technology offers numerous advantages, several issues must be resolved before it may be generally used in patient-centered care.(3) Patient data is very private and must be kept secure from those who shouldn't have access to it or who could use it, hence data privacy and security is rather crucial. Common approaches for data sharing, teamwork, and model assessment help to ensure that artificial intelligence technologies may be readily included to healthcare systems. Furthermore, one has to give great consideration the moral consequences of artificial intelligence in the medical field. How to ensure, for instance, that AI decision-making procedures are transparent, fair, and responsible?
Background and literature review
Current challenges in patient-centered care
PCC, often known as patient-centered care, seeks to provide each individual patient with healthcare that honours their needs and preferences. Many people accept as true with that p.c is an essential issue of quality of living; but various issues complicate its implementation. The truth that healthcare services are not cooperating nicely is one of the principal troubles. Patients get treatment from many companies in several places which include hospitals, trendy care centres, specialized clinics, and network fitness tasks regularly simultaneously. This makes it difficult to create thorough, orderly, and customised treatment programs in addition to consistent care. The full-size volume of affected person information coming from several resources clinical imaging, test outcomes, smart technology, electronic health records (EHRs) is another important task.(4) Managing and evaluating this information in a manner that aids in top notch choice-making is a undertaking for lots medical practitioners. Information maintained separate across structures or unorganised could motive one to overlook possibilities for early analysis or preventative treatment, therefore affecting the affected person results. Inefficient scheduling and useful resource allocation also lead sufferers to regularly need to wait longer for treatment or secure with-up visits, which delays analysis or issue solving. Getting people more engaged in their care and ensuring them observe via is considered one of p.c's hardest tasks. Many patients battle to observe their complicated treatment programs, take their tablets as directed, and adjust their normal activities.(5) They can lack the records, sources, or help required to make clever selections about their health.
Evolution of medical informatics
Combining computer technology, information era, and health care, medical informatics combines over the past several decades, it has developed significantly. Medical informatics became largely involved on fundamental computer systems to automate mundane tasks such billing, coding, and file keeping. As healthcare became more and more complicated, but, the emphasis shifted to creating more state-of-the-art systems to manipulate scientific facts, help people in making better choices, and beautify affected person remedy. When they first emerged within the Nineties, electronic health records (EHRs) represented a huge advancement in clinical technology.(6) Doctors and nurses would possibly scan patient notes the use of EHRs, therefore facilitating storage, seek, and sharing of patient information. This circulate to virtual made it possible to create unmarried platforms from which extra related structures consisting of clinical, laboratory, imaging, and genetic records can be created. These trends enabled nurses and physicians to get complete affected person information at the time of treatment, consequently accelerating and enhancing scientific picks made through them. More and more clinical informatics has been using cutting aspect era such artificial intelligence (AI), machine learning (ML), and massive facts analytics to decorate healthcare service.(7) AI and ML have made coping with records in more complicated methods viable. This lets in us to discover styles, take look at large amounts in actual time, and challenge affected person behaviour.
The impact of AI in healthcare
By use of machine learning algorithms and deep learning approaches, artificial intelligence systems may identify patterns in this data and provide clinicians with insights sometimes invisible at first sight. On the one hand, physicians already employ artificial intelligence systems to assist with illness diagnosis including cancer, heart disease, and brain disorders. Diagnosis technologies powered by artificial intelligence can examine medical pictures like X-rays, MRIs, and CT scans to discover issues rather precisely. These instruments may detect early indicators of illnesses in non-symptomatic individuals, so therapy can begin earlier and patients could have better outcomes. In the same way, AI can help doctors guess how likely it is that a patient will get certain conditions or problems. This lets doctors make treatment plans for each patient that are specifically suited to their health.(8) AI is also a key part of improving patient-centered care by making telemedicine and distant tracking work better. Wearable tech driven by AI can keep track of a patient's vital signs, exercise levels, and sleep habits in real time, giving them and their doctor’s constant health information. This real-time data can help doctors make quick choices and change treatment plans as needed, which will make the whole care experience better. AI has also made progress in getting patients involved. Through personalized suggestions and prompts, AI has helped people better understand and take care of their health problems. From the history and literature study, Table 1 shows the methods, key results, obstacles, and scope.
|
Table 1. Summary of Background and Literature Review |
|||
|
Algorithm |
Key Findings |
Challenges |
Scope |
|
Random Forest |
High accuracy in disease classification |
Overfitting, feature selection |
Disease classification, risk prediction |
|
Support Vector Machine |
Effective in predicting patient outcomes |
Requires large datasets, difficult to interpret |
Patient outcome prediction, disease prognosis |
|
Logistic Regression |
Simple, interpretable, fast |
Limited to linear relationships |
Healthcare decision support |
|
Neural Networks |
High performance in large datasets |
Data pre-processing intensive |
Medical image processing, drug discovery |
|
K-Nearest Neighbors(9) |
Good for classification of small datasets |
Computationally expensive for large datasets |
Small dataset classification, diagnostic predictions |
|
Decision Trees |
Simple decision rules |
Risk of overfitting |
Medical diagnosis, classification tasks |
|
Naive Bayes |
Efficient in text classification |
Assumes feature independence |
Text classification in healthcare documents |
|
Deep Learning |
Effective for time-series data |
Requires a large amount of labeled data |
Time-series analysis in patient health monitoring |
|
Recurrent Neural Networks |
Good for sequence prediction |
Difficult to interpret results |
Sequence modeling for patient data |
|
Bayesian Networks |
Probabilistic model for prediction |
Assumes prior knowledge of model structure |
Predictive analytics in healthcare |
|
XGBoost(10) |
Effective in high-dimensional data |
Sensitive to noisy data |
Medical prediction, genomic data analysis |
|
Convolutional Neural Networks |
High precision in image recognition |
High resource consumption |
Medical image classification, diagnostic tools |
|
Principal Component Analysis |
Reduces dimensionality for faster processing |
Difficulty handling complex data structures |
Dimensionality reduction in genomics, EHR data |
|
Gradient Boosting |
Efficient in boosting predictive accuracy |
Sensitive to hyperparameters |
Ensemble learning for accurate healthcare predictions |
Ai-driven medical informatics
Definition and key components
In AI-driven medical informatics, artificial intelligence (AI) methods are used together with medical informatics to improve healthcare service, help doctors make better decisions, and make sure that each patient gets the care that they need. It uses complex algorithms, machine learning models, and data analytics to process, analyze, and make sense of huge amounts of medical data from many sources, like patient histories, medical images, lab results, smart tech, and electronic health records (EHRs).(11) The main goal of medical informatics that is driven by AI is to make healthcare systems more effective, approachable, and patient-centered by providing real-time information, the ability to predict the future, and personalized care suggestions.
Key components of AI-driven medical informatics include:
· Data Integration and Management: One of the most important skills in medical informatics is being able to combine and handle data from different sources, like EHRs, diagnostic tests, and health tracking devices. AI algorithms are used to process unorganized or siloed data and combine it into a single file that makes it easier to analyze and make decisions. Integrating data gives doctors a full picture of a patient's health, which is important for providing individualized care.
· Machine Learning and Predictive Analytics: Algorithms for machine learning (ML), like controlled, unstructured, and reinforcement learning, are used to find trends in patient data and guess how their health will turn out. Predictive analytics helps find diseases early, figure out who is at risk, and make treatments work better. By finding risk factors early on in a patient's health journey, AI models can predict problems like heart attacks or diabetic crises, which allows for quick treatments.(12)
· Natural Language Processing (NLP): NLP methods are used to get useful data from text files that aren't organized, like study papers, doctor's notes, and exit reports. NLP makes it possible for AI systems to understand and study free-text data, which has been hard for medical computing systems in the past. CDSS stands for clinical decision support systems. This will improve the level of care and cut down on mistakes made by people.
AI techniques used in medical informatics
Machine learning
Many times employed in medical computing to examine and make sense of vast volumes of healthcare data is a fundamental artificial intelligence technique known as machine learning (ML). Developing algorithms that can learn from data trends without explicit programming is the essence of machine learning (ML). This helps systems improve gradually. Looking through a lot of patient data medical records, lab findings, imaging data, vital signs ML models may identify trends and project patient behaviour. Supervised learning is one kind of machine learning that finds great use in medical computing. Under this approach, models are instructed to identify trends in designated data. For example, ML models may be trained on large databases including images of medical scenarios.(13) This helps them to precisely identify disorders such tumours or fractures. Conversely, unsupervised learning searches for unseen patterns in data that has not been labelled. This can help find insights or disease groups that weren't known before. Machine learning is used in healthcare to make diagnoses more accurate, predict how patients will do, make treatment plans more effective, and track patients' growth over time. For instance, ML algorithms can guess how likely it is that a person will need to go back to the hospital, help with specific drug suggestions, and guess how long it will take for long-term conditions like diabetes to get worse.(14)
Step 1: Data Collection
The first step is to gather the data that will be used to train the machine learning model. The dataset should be relevant to the problem you are solving, and it typically consists of features (input variables) and labels (output or target variables).
Mathematically:
Let X = [x1, x2, ..., xn] represent the feature vector of n samples.
Let y = [y1, y2, ..., yn] represent the corresponding labels or target values.
Step 2: Data Preprocessing
In this step, you clean the data, handle missing values, normalize or scale features, and convert categorical variables into numerical ones if needed. The goal is to prepare the data for training the machine learning model.
Mathematically:
Normalize or scale features: x_hat_i = (x_i - μ) / σ, where μ is the mean and σ is the standard deviation.
Handle missing values: Replace missing values using imputation techniques (mean, median, mode, etc.).
Step 3: Model Selection
Select the appropriate machine learning model based on the problem type (e.g., regression, classification). For example, if it's a classification task, you might use a decision tree, logistic regression, or a support vector machine (SVM).
Mathematically, for a linear regression model, the hypothesis hθ(x) can be represented as:
![]()
Where:
θ represents the parameters (weights) of the model.
x1, x2, ..., xn are the input features.
Step 4: Training the Model
In this step, you use the training data to optimize the model's parameters (weights) by minimizing a loss function. The most common loss function used in regression tasks is Mean Squared Error (MSE).
Mathematically, for linear regression, the loss function is:
![]()
Where:
m is the number of training samples.
hθ(xi) is the predicted value for sample i.
yi is the actual value for sample i.
To minimize this loss, you typically use gradient descent:
![]()
Where α is the learning rate.
Step 5: Model Evaluation
Once the model is trained, evaluate its performance using a test set (unseen data). Common evaluation metrics include accuracy (for classification) or RMSE (Root Mean Squared Error for regression).
Mathematically, for classification, accuracy is defined as: Accuracy = (Number of correct predictions) / (Total number of predictions).
For regression tasks, you can calculate RMSE:
![]()
Where:
yihat is the predicted value for sample i.
yi is the actual value for sample i.
Natural language processing
Natural Language Processing, or NLP, is an area of artificial intelligence that studies how machines and people talk to each other. NLP is used in medical computing to process and analyze large amounts of written data that is not organized, like medical books, exit reports, and clinical notes. A lot of healthcare data is in the form of free text, which has made it hard to study and add to organized systems in the past. NLP fills in this gap by letting machines understand, analyze, and create language in a way that looks and acts like a person. Getting valuable information from clinical texts like patient records, doctor's notes, and medical research publications depends on NLP in major part. Based on significant information like symptoms, diagnosis, therapies, and outcomes, NLP systems may automatically categorise free-text notes. This facilitates the locating and analysis of the material.(15) This improves treatment choices by allowing clinicians to rapidly access the data required about a patient. Large-scale clinical research publications provide valuable information, assist identify viable medication combinations, and enable one to understand patient attitudes on their mental health.
Step 1: Text Preprocessing
The first step in NLP is to preprocess the raw text. This typically involves steps like tokenization, stopword removal, stemming, and lemmatization. Preprocessing converts raw text into a structured format that can be analyzed.
Mathematically, tokenization can be represented as: Let T = [t1, t2, ..., tn] represent the tokenized words from the input text.
Stopwords removal: Let W = [w1, w2, ..., wn] be the list of stopwords, and remove them from the tokens.
Step 2: Text Representation
Once the text is preprocessed, the next step is to represent the words as numerical vectors that can be used in machine learning models. Common methods include Bag of Words (BoW), TF-IDF (Term Frequency-Inverse Document Frequency), and Word Embeddings (e.g., Word2Vec).
Mathematically, for TF-IDF, the term frequency (TF) for a word \( w_i \) in a document \( d \) is given by:
![]()
The inverse document frequency (IDF) for a word \( w_i \) across a collection of documents \( D \) is:
![]()
Where:
(N) is the total number of documents.
\(df(wi) \) is the number of documents containing \( wi \).
The TF-IDF weight for a word \( wi \) in document \( d \) is:
![]()
Step 3: Feature Extraction
After representing the text, feature extraction is performed to obtain relevant features for the NLP task (e.g., sentiment analysis, topic modeling). Techniques like N-grams, POS tagging, and Named Entity Recognition (NER) are often used for extracting features.
Mathematically, for N-grams, let a sequence of words \( w_1, w_2, ..., w_n \) be given, and an N-gram model creates a window of size \( N \) over the sequence:
![]()
Step 4: Model Training
In this step, you use the extracted features to train an appropriate machine learning model. Common algorithms include Naive Bayes, Support Vector Machine (SVM), and Recurrent Neural Networks (RNNs) for text classification and sentiment analysis.
Mathematically, for a text classification task, the model predicts the probability of class \( C \) given a document \( d \) with features \( x_1, x_2, ..., xn \):
![]()
Step 5: Model Evaluation
Once the model is trained, its performance is evaluated using appropriate evaluation metrics. For classification tasks, metrics such as accuracy, precision, recall, and F1-score are commonly used.
Mathematically, accuracy is defined as:
![]()
For precision and recall, for a binary classification (positive class \( P \) and negative class \( N \)):
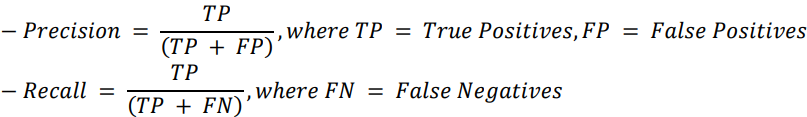
F1-score is the harmonic mean of precision and recall:
![]()
Predictive analytics
Using statistical techniques and machine learning, predictive analytics a subfield of artificial intelligence looks at previous data and projects future events. Medical computers heavily relies on predictive analytics, which forecasts probable health hazards, illness growth, and treatment effectiveness thus enhancing patient care. Looking at large datasets including patient information, clinical records, test findings, and lifestyle variables, predictive models may identify patterns showing how probable it is that anything negative will occur in the future.(16) Hospital settings use predictive analytics to identify illnesses early, categorise patients according on their risk, and provide individualised treatment plans. Predictive models, for example, may determine a person's likelihood of developing cancer, diabetes, or heart disease, which allows clinicians to intervene before symptoms present. Guessing what will happen with patients that are, how likely they are to get better, have issues, or need to return to the hospital after release is another very beneficial application for predictive analytics. Being able to guess possible risks lets doctors step in early, which improves patient results and lowers the cost of healthcare. Predictive analytics can also be used to make treatment plans work better.(17) Predictive models can help find the best treatments for each patient by looking at past treatment data and how patients responded to those treatments. This cuts down on the need for trial-and-error methods.
Benefits of AI in managing patient data
AI has the ability to completely change how patient data is handled, which would be very helpful for speed, accuracy, and personalized care. Using artificial intelligence to manage patient data is one of the finest benefits in that it can rapidly and accurately handle vast volumes of data. For healthcare systems, electronic health records (EHRs), medical imaging, lab findings, genetic data, and real-time sensor data from smart devices all provide an enormous volume of data. Much faster and more effectively than humans could, artificial intelligence can arrange, examine, and extract helpful ideas from this data. To provide a more complete picture of a patient's health, AI-powered systems may aggregate data from numerous sources. Combining many types of data enables clinicians to make more informed decisions those results in improved treatment plans, more accurate diagnosis, and better patient outcomes. AI systems may, for example, combine clinical data with genetic information to ensure that medicines are customised to every patient's particular DNA composition. This makes medications more precise and powerful. This is particularly beneficial in fields like cancer, where efficient treatment depends much on tailored therapy.(18) Another significant advantage of employing artificial intelligence to handle patient data is its ability to provide real-time improved decision-making for individuals. With AI, healthcare professionals can get the most up-to-date information, which lets them keep an eye on their patients' situations and make changes to their treatments as required. Figure 2 shows how AI can help manage patient data more quickly, which leads to better health results.
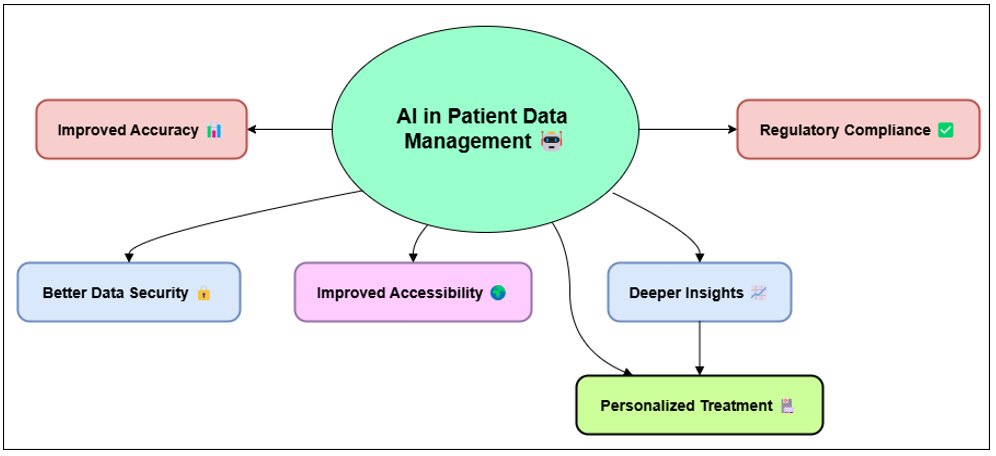
Figure 2. Illustrating the Benefits of AI in Managing Patient Data
A type of AI called predictive analytics can also help find early signs of problems, stop bad things from happening, and lower the number of times people have to go back to the hospital. AI can also help automate boring office chores like billing, filing, and scheduling. This makes healthcare run more smoothly and lets doctors focus more on caring for patients.
Real-time health data analysis
Overview of real-time health monitoring systems
Real-time health tracking systems are made to constantly gather, analyze, and make sense of health data from patients in real time. This gives doctors and decision-makers useful information that helps them act and make decisions quickly. These systems are very important in both hospital and home care settings because they let doctors keep an eye on their patients' health without having to physically check them all the time. Real-time monitoring is especially helpful for people who have long-term conditions like diabetes, high blood pressure, or heart disease because it lets doctors keep an eye on their vital signs and general health. These systems can keep an eye on many health factors by using related technologies, like blood pressure, heart rate, breathing rate, oxygen saturation, glucose levels, and physical exercise. The information is sent to healthcare workers through safe networks. They can view it in real time, which lets them check on a patient right away and make changes to their treatment plans as needed. For instance, in critical care units or emergency rooms, real-time health tracking devices help doctors spot early signs of worsening, so they can act quickly and lower the risk of serious consequences. One of the best things about real-time health tracking is that it lets healthcare go from being reactive to being proactive. These systems can find small changes in a patient's health that could mean new problems by constantly collecting data and keeping an eye on trends. This early spotting can help keep patients out of the hospital again, cut down on trips to the emergency room, and improve their health.
Technologies enabling real-time data collection (wearables, IoT)
The growth of smart tech and the Internet of Things (IoT) has changed how real-time health data is collected. Many people use wearable tech, like smartphones, exercise trackers, and wearable ECG monitors, to keep track of their health in real time. These gadgets have monitors that check things like blood oxygen levels, heart rate, sleep habits, and physical exercise. They then send this information to other gadgets that are linked, mobile apps, or healthcare platforms. Because these gadgets work in real time, they can be constantly checked on, which gives patients and doctors useful information about health trends. Linking these smart devices and sensors to healthcare systems is mostly dependent on IoT so that physicians and patients may quickly exchange data and communicate in real time. Wireless networks like Bluetooth or Wi-Fi bind IoT-enabled health devices together. They communicate patient data to health systems or cloud-based platforms so that only authorised medical professionals may access it. This link guarantees that medical personnel constantly have the most current information about their patients. This helps one to monitor their development, ensure they are adhering to their treatment programs, and act in an emergency should one be needed. More specialised areas of healthcare, such monitoring individuals with long-term diseases or assisting in recovery from surgery, also find use for wearables and Internet of Things (IoT) devices. For instance, smart insulin pumps can continuously monitor blood sugar levels and instantly adjust the dosage of insulin supplied. Likewise, constant blood pressure monitors allow physicians to alert them should a patient's blood pressure rise too much. More health data in real time as these devices develop smarter helps to enhance patient outcomes and enable more customised medical treatment by means of their gathering.
Patient-centered care and ai integration
Defining patient-centered care
PCC aims are to enhance the whole patient experience, improve health outcomes, and increase flexibility in healthcare so it may meet every patient's demand. PCC is aware that rather than just treating certain illnesses or ailments, one should grasp the full person including their social, psychological, and emotional requirements. Among the key concepts of patient-centered care include respecting the patient's decisions, organising and combining treatment, communicating information, and motivating the patient to assume leadership. Under this approach, medical professionals candidly communicate with patients and provide them easily available, unambiguous information about their diseases and course of treatment. Patients should be allowed to share their concerns, ask questions, and make informed decisions about their health based on correct knowledge. This combined approach enables physicians and patients to develop a closer relationship of trust and support, therefore improving general health outcomes and making the patients happier. PCC covers broader ground than just professional exchanges. It covers also patient involvement in long-term health management, continuity of care, and access to treatment. By establishing an environment in which the patient feels like an active participant, PCC hopes to provide not only scientifically sound but also compatible with the patient's own values and way of life. However, for this approach to be successful, innovative ideas—such as leveraging artificial intelligence and other modern technology to make treatment more specialised and on time, particularly for those with challenging, long-term diseases—are needed.
RESULTS AND DISCUSSION
Combining medical technology powered by AI with real-time health data analysis makes patient-centered care a lot better by allowing for personalized care, early disease discovery, and proactive health management. Through machine learning and predictive analytics, AI systems can get real-time information from a lot of different sources, which helps doctors make better decisions and patients get better care. Wearables and Internet of Things (IoT) devices make real-time tracking systems possible. These systems continuously record vital signs, which lets doctors act quickly and lower the risk of problems.
|
Table 2. AI Model Evaluation Results |
||
|
Evaluation Parameter |
AI Model 1 |
AI Model 2 |
|
Accuracy (%) |
92 |
87 |
|
Precision (%) |
89 |
84 |
|
Recall (%) |
94 |
90 |
|
F1-Score (%) |
91 |
87 |
|
AUC (%) |
93 |
89 |
The test results for AI Model 1 and AI Model 2 are shown in table 2. These results give us important information about how well they did in a number of important areas. In every rating metric, AI Model 1 always does better than AI Model 2. 92 % of the time, AI Model 1 is right, while 87 % of the time, AI Model 2 is right. Figure 3 shows a comparison of the performance of an AI model using different evaluation measures to see how well it works and how accurate it is.
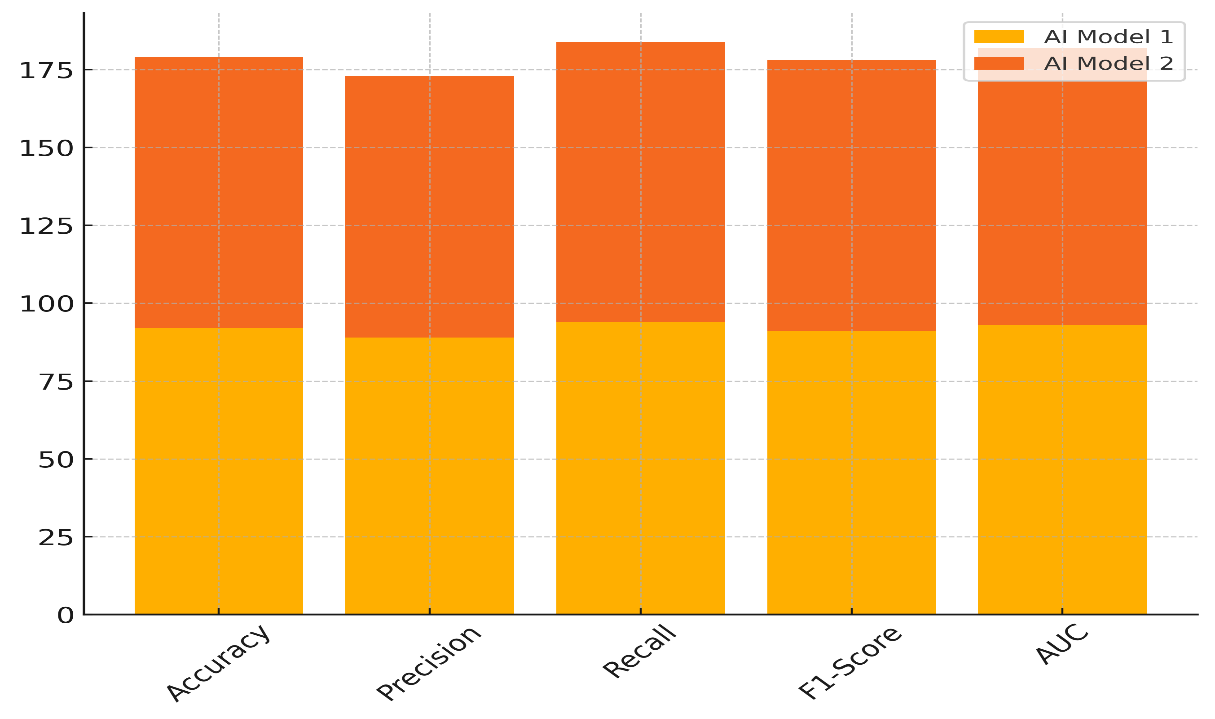
Figure 3. Comparison of AI Model Performance Across Evaluation Metrics
This means that Model 1 is more likely to be right about what will happen in the end. When it comes to accuracy, AI Model 1 still has a 5 % edge over Model 2, getting 89 % compared to 84 % for Model 2. This shows that Model 1 is better at reducing the number of fake positives. In figure 4, you can see how the success of AI models has changed over time by looking at different rating measures.
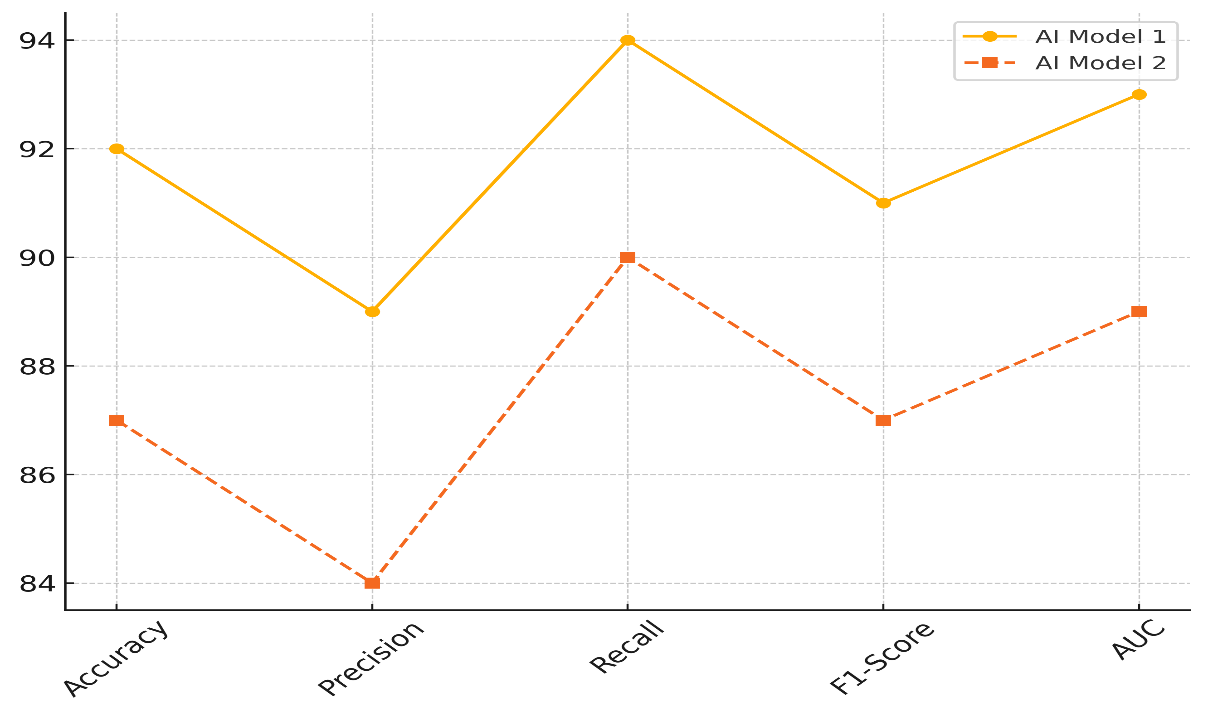
Figure 4. Performance Trends of AI Models Across Evaluation Metrics
Also, Model 1 does much better than Model 2 in recall, which checks how well it can find all the important cases (94 % vs. 90 % for Model 2). The F1-score, which compares accuracy to memory, also shows the same pattern. Model 1 gets a score of 91 %, while Model 2 only gets 87 %. Model 1 also does better on the AUC (Area Under the Curve) metric, which checks how well the model can tell the difference between groups, with a score of 93 % compared to 89 % for Model 2.
|
Table 3. Real-Time Health Data System Evaluation |
||
|
Evaluation Parameter |
System A |
System B |
|
Data Processing Speed (ms) |
45 |
50 |
|
Error Rate (%) |
2,1 |
2,7 |
|
Real-time Monitoring (%) |
98 |
95 |
|
Patient Engagement (%) |
85 |
80 |
The test results for System A and System B are shown in table 3 for a number of different factors. In every important way, System A does better than System B. It takes 45 ms for System A to process data compared to 50 ms for System B. This means that System A can handle and process data more quickly. This is very important for real-time programs that need to make decisions quickly. System A is also better than System B when it comes to mistake rate; System A's is 2,1 % and System B's is 2,7 %. This shows that System A is more precise and less likely to give wrong results, which is very important in healthcare settings where accuracy is key to keeping patients safe. Figure 5 shows how well System A and System B did on several important rating criteria.
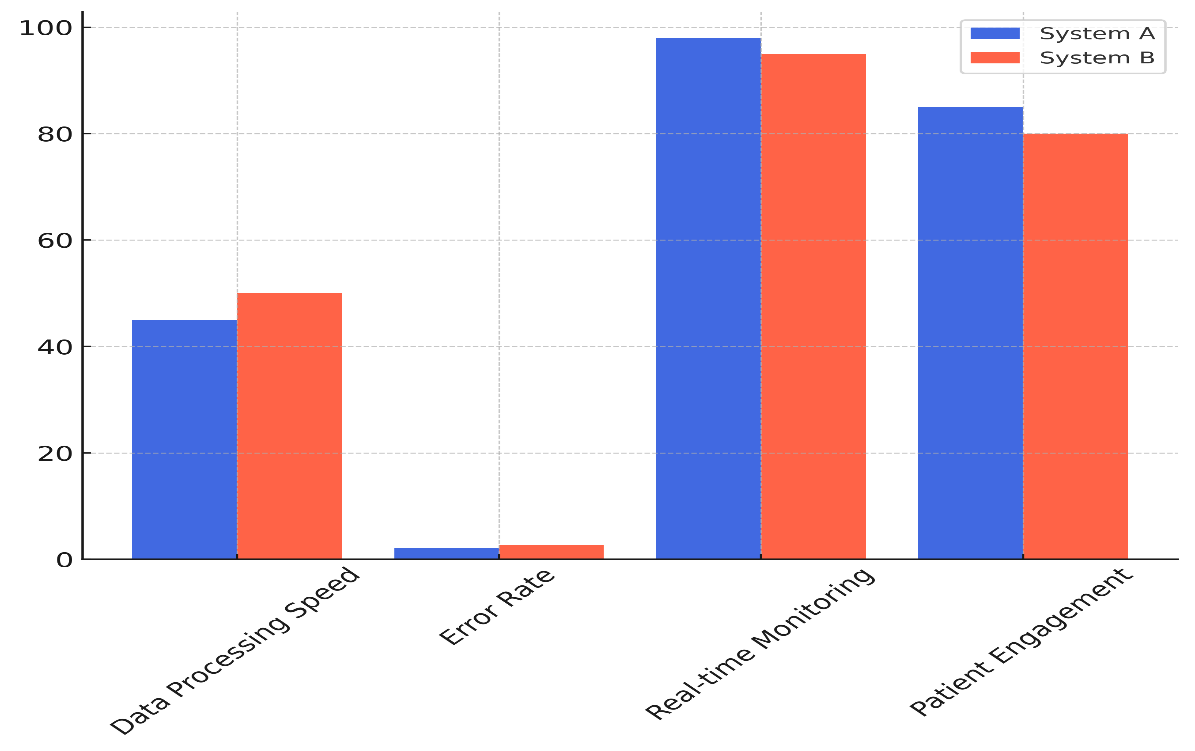
Figure 5. Performance Comparison of System A and System B Across Key Metrics
The 98 % of data in System A is monitored in real time, while only 95 % of data in System B is monitored in real time. Figure 6 shows how system performance has changed over time based on different measurement measures.
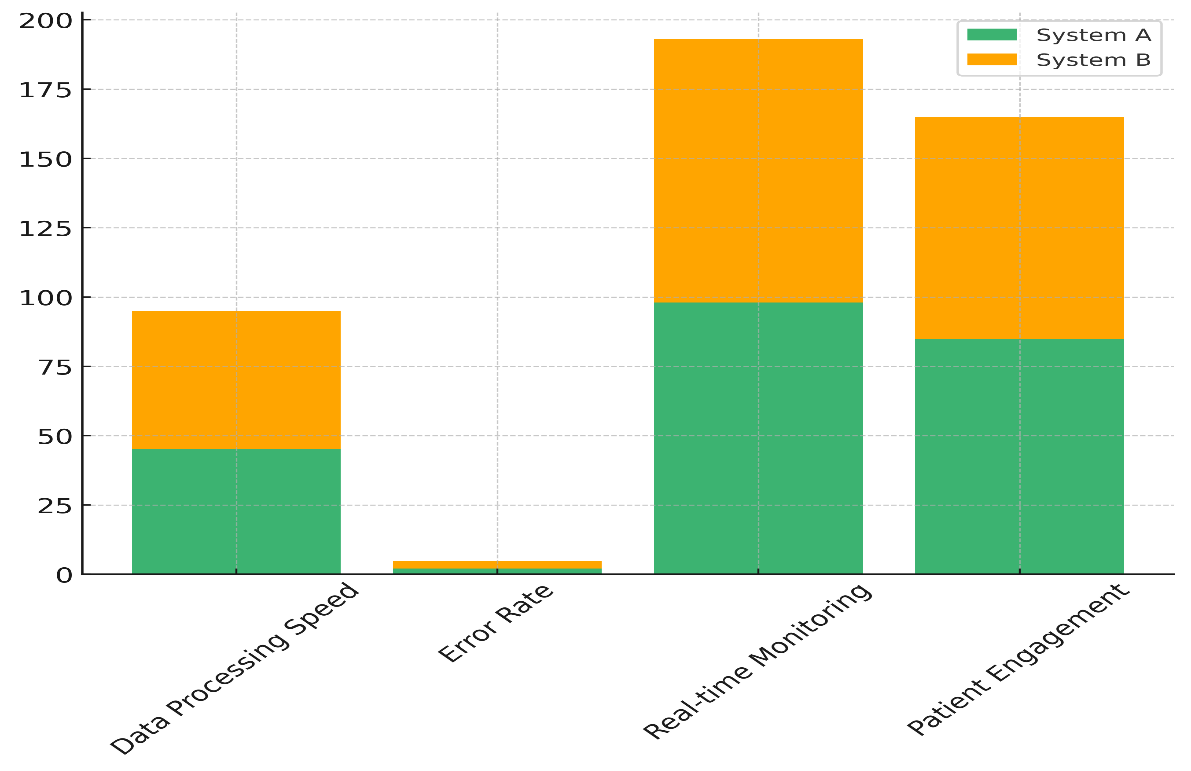
Figure 6. Cumulative Contribution of System Performance Across Evaluation Metrics
This means that System A gives healthcare workers more constant and up-to-date knowledge, which lets them act more quickly when they need to. Last but not least, System A has more engaged patients (85 %), while System B only has 80 %. This shows that System A is better at getting people to connect with their health data and stay involved in their care, which is very important for improving their health in the long run.
CONCLUSIONS
Combining medical technology powered by AI with real-time health data analysis has the ability to completely change care that is focused on the patient. Using cutting edge technology as machine learning, natural language processing, and predictive analytics, healthcare systems may provide more individualised, proactive, and efficient treatment that matches each patient's need. By managing enormous volumes of patient data and providing real-time information capable of significantly enhancing patient outcomes, artificial intelligence aids clinicians in making better judgements. Constant monitoring a patient's health is made feasible by wearable technology and the Internet of Things (IoT). This helps clinicians to respond fast and identify issues early on, therefore reducing the chance of negative consequences and hospital readmissions. Real-time health monitoring technologies help patients even more to take responsibility of their condition. Doctors may monitor their patients' vital signs, make hypotheses about possible health hazards, and modify their treatment plans as necessary by integrating artificial intelligence into these surveillance systems without any issues. Making healthcare more effective, lowering costs and increasing patient happiness all depend on this shift from responding to proactive treatment. Using artificial intelligence in patient-centered care does, however, present some challenges. Before AI-driven healthcare solutions can fully realise themselves, issues with data privacy and security as well as technical obstacles such data exchange and integration must be resolved. We also need to consider moral and legal issues like justice, transparency, and accountability to ensure that artificial intelligence is used sensibly in therapeutic environments.
BIBLIOGRAPHIC REFERENCES
1. Yang, D.-M.; Chang, T.-J.; Hung, K.-F.; Wang, M.-L.; Cheng, Y.-F.; Chiang, S.-H.; Chen, M.-F.; Liao, Y.-T.; Lai, W.-Q.; Liang, K.-H. Smart healthcare: A prospective future medical approach for COVID-19. J. Chin. Med. Assoc. 2023, 86, 138.
2. Dewangan, N.; Vyas, P.; Ankita; Mandal, S. Smart Healthcare and Intelligent Medical Systems. In Computational Intelligence and Applications for Pandemics and Healthcare; IGI Global: Hershey, PA, USA, 2022; pp. 205–228. ISBN 978-1-79989-831-3.
3. Dong, A.; Guo, J.; Cao, Y. Medical information mining-based visual artificial intelligence emergency nursing management system. J. Healthc. Eng. 2021, 2021, e4253606.
4. Abdulkareem, K.H.; Mohammed, M.A.; Salim, A.; Arif, M.; Geman, O.; Gupta, D.; Khanna, A. Realizing an Effective COVID-19 Diagnosis System Based on Machine Learning and IoT in Smart Hospital Environment. IEEE Internet Things J. 2021, 8, 15919–15928.
5. Gupta, N.S.; Kumar, P. Perspective of artificial intelligence in healthcare data management: A journey towards precision medicine. Comput. Biol. Med. 2023, 162, 107051.
6. Jayaraman, P.P.; Forkan, A.R.M.; Morshed, A.; Haghighi, P.D.; Kang, Y.-B. Healthcare 4.0: A review of frontiers in digital health. WIREs Data Min. Knowl. Discov. 2020, 10, e1350.
7. Kumar, A.; Gond, A. Natural Language Processing: Healthcare Achieving Benefits Via Nlp. Sci. Prepr. 2023, 2023, 2–14. [
8. Kumar, Y.; Koul, A.; Mahajan, S. A deep learning approaches and fastai text classification to predict 25 medical diseases from medical speech utterances, transcription and intent. Soft Comput. 2022, 26, 8253–8272.
9. Aggarwal, N.; Ahmed, M.; Basu, S.; Curtin, J.J.; Evans, B.J.; Matheny, M.E.; Nundy, S.; Sendak, M.P.; Shachar, C.; Shah, R.U.; et al. Advancing Artificial Intelligence in Health Settings Outside the Hospital and Clinic. NAM Perspect. 2020, 2020, 1–26.
10. Lee, D.; Yoon, S.N. Application of Artificial Intelligence-Based Technologies in the Healthcare Industry: Opportunities and Challenges. Int. J. Environ. Res. Public Health 2021, 18, 271.
11. Javed, A.R.; Saadia, A.; Mughal, H.; Gadekallu, T.R.; Rizwan, M.; Maddikunta, P.K.R.; Mahmud, M.; Liyanage, M.; Hussain, A. Artificial Intelligence for Cognitive Health Assessment: State-of-the-Art, Open Challenges and Future Directions. Cogn. Comput. 2023, 15, 1767–1812.
12. Maddula, R.; MacLeod, J.; McLeish, T.; Painter, S.; Steward, A.; Berman, G.; Hamid, A.; Abdelrahim, M.; Whittle, J.; Brown, S.A.; et al. The role of digital health in the cardiovascular learning healthcare system. Front. Cardiovasc. Med. 2022, 9, 1008575.
13. Sarker, I.H. AI-Based Modeling: Techniques, Applications and Research Issues Towards Automation, Intelligent and Smart Systems. SN Comput. Sci. 2022, 3, 1–20.
14. Sennott, S.C.; Akagi, L.; Lee, M.; Rhodes, A. AAC and Artificial Intelligence (AI). Top. Lang. Disord. 2019, 39, 389–403
15. G. Umamaheswararao . (2015). The Role of Securities & Exchange Board of India (SEBI) towards Regulating Indian Mutual Funds. International Journal on Research and Development - A Management Review, 4(3), 8 - 17.
16. Poalelungi, D.G.; Musat, C.L.; Fulga, A.; Neagu, M.; Neagu, A.I.; Piraianu, A.I.; Fulga, I. Advancing Patient Care: How Artificial Intelligence Is Transforming Healthcare. J. Pers. Med. 2023, 13, 1214.
17. Hosny, A.; Parmar, C.; Quackenbush, J.; Schwartz, L.H.; Aerts, H. Artificial intelligence in radiology. Nat. Rev. Cancer 2018, 18, 500–510.
18. Hossain, E.; Rana, R.; Higgins, N.; Soar, J.; Barua, P.D.; Pisani, A.R.; Turner, K. Natural Language Processing in Electronic Health Records in relation to healthcare decision-making: A systematic review. Comput. Biol. Med. 2023, 155, 106649.
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Swati Kemothi, Sujayaraj Samuel Jayakumar, Swarna Swetha Kolaventi, Pratyashi Satapathy, Kollathur Sudheer, Gunveen Ahluwalia, Ansh Kataria.
Data curation: Swati Kemothi, Sujayaraj Samuel Jayakumar, Swarna Swetha Kolaventi, Pratyashi Satapathy, Kollathur Sudheer, Gunveen Ahluwalia, Ansh Kataria.
Formal analysis: Swati Kemothi, Sujayaraj Samuel Jayakumar, Swarna Swetha Kolaventi, Pratyashi Satapathy, Kollathur Sudheer, Gunveen Ahluwalia, Ansh Kataria.
Drafting - original draft: Swati Kemothi, Sujayaraj Samuel Jayakumar, Swarna Swetha Kolaventi, Pratyashi Satapathy, Kollathur Sudheer, Gunveen Ahluwalia, Ansh Kataria.
Writing - proofreading and editing: Swati Kemothi, Sujayaraj Samuel Jayakumar, Swarna Swetha Kolaventi, Pratyashi Satapathy, Kollathur Sudheer, Gunveen Ahluwalia, Ansh Kataria.