doi: 10.56294/mw2024507
ORIGINAL
Leveraging AI-Driven Health Informatics for Predictive Analytics in Chronic Disease Management
Aprovechamiento de la informática sanitaria basada en IA para el análisis predictivo en la gestión de enfermedades crónicas
Pratibha Sharma1 ![]() *, Ved Vrat Verma2
*, Ved Vrat Verma2 ![]() , Manashree Mane3
, Manashree Mane3 ![]() , Shashikant Patil4
, Shashikant Patil4 ![]() , Ansuman Samal5
, Ansuman Samal5 ![]() , Manni Sruthi6
, Manni Sruthi6 ![]() , Ayaan Faiz7
, Ayaan Faiz7 ![]()
1Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
2Department of Biotechnology, Noida International University. Greater Noida, Uttar Pradesh, India.
3Forensic Science, JAIN (Deemed-to-be University). Bangalore, Karnataka, India.
4Department of ISME, ATLAS SkillTech University. Mumbai, Maharashtra, India.
5Department of Management, Siksha ‘O’ Anusandhan (Deemed to be University). Bhubaneswar, Odisha, India.
6Centre for Multidisciplinary Research, Anurag University. Hyderabad, Telangana, India.
7Chitkara Centre for Research and Development, Chitkara University. Himachal Pradesh, India.
Cite as: Sharma P, verma V vrat, Mane M, Patil S, Samal A, Sruthi M, et al. Leveraging AI-Driven Health Informatics for Predictive Analytics in Chronic Disease Management. Seminars in Medical Writing and Education. 2024; 3:507. https://doi.org/10.56294/mw2024507
Submitted: 10-10-2023 Revised: 12-01-2024 Accepted: 13-05-2024 Published: 14-05-2024
Editor:
PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Pratibha Sharma *
ABSTRACT
People are getting long-term illnesses like diabetes, heart disease, and high blood pressure more and more often. Because of this, it’s even more important to find better ways to handle these situations and move quickly when they happen. Using AI-powered health informatics in predictive analytics seems like a good way to improve the quality of care and patient outcomes when dealing with long-term illnesses. This study looks at how AI models, like machine learning algorithms, predictive modelling, and data-driven analytics, can change how long-term illnesses are watched, identified, and treated. By looking at a lot of data from smart tech, medical pictures, and electronic health records (EHRs), AI systems can find patterns and guess how a disease will get worse before the symptoms show up. By finding high-risk patients early on, these insights can help healthcare workers make the best use of resources, give more personalised care, and cut costs. Using AI in health technology also makes it easier to make systems that can keep an eye on people with long-term illnesses in real time. These systems can keep an eye on vital signs, living factors, and drug compliance all the time. This can help people get help right away, which can cut down on problems and hospital stays. AI technologies can also help automate repetitive chores like data filing, medical support, and decision-making, which frees up healthcare workers to spend more time caring for patients directly. However, using AI to handle chronic diseases can be hard because of issues with data protection, the need for uniform data forms, and making sure that AI models can be understood and held accountable. At the end of the paper, the future uses of AI in managing chronic diseases are talked about. It is emphasized that healthcare workers, data scientists, and lawmakers need to keep researching and working together to get the most out of AI-driven health informatics.
Keywords: AI-Driven Health Informatics; Predictive Analytics; Chronic Disease Management; Machine Learning; Personalized Treatment.
RESUMEN
Cada vez es más frecuente que la gente contraiga enfermedades de larga duración, como diabetes, cardiopatías e hipertensión. Por ello, es aún más importante encontrar mejores formas de manejar estas situaciones y actuar con rapidez cuando se producen. El uso de la informática sanitaria impulsada por IA en el análisis predictivo parece una buena forma de mejorar la calidad de la atención y los resultados de los pacientes cuando se trata de enfermedades de larga duración. Este estudio examina cómo los modelos de IA, como los algoritmos de aprendizaje automático, los modelos predictivos y los análisis basados en datos, pueden cambiar la forma de vigilar, identificar y tratar las enfermedades de larga duración. Al examinar gran cantidad de datos procedentes de tecnología inteligente, imágenes médicas e historias clínicas electrónicas (HCE), los sistemas de IA pueden encontrar patrones y adivinar cómo empeorará una enfermedad antes de que aparezcan los síntomas. Al detectar precozmente a los pacientes de alto riesgo, esta información puede ayudar al personal sanitario a hacer un mejor uso de los recursos, ofrecer una atención más personalizada y reducir costes. El uso de la IA en la tecnología sanitaria también facilita la creación de sistemas capaces de vigilar en tiempo real a las personas con enfermedades de larga duración. Estos sistemas pueden controlar en todo momento las constantes vitales, los factores vitales y el cumplimiento terapéutico. Esto puede ayudar a las personas a obtener ayuda de inmediato, lo que puede reducir los problemas y las estancias hospitalarias. Las tecnologías de IA también pueden ayudar a automatizar tareas repetitivas como el archivo de datos, la asistencia médica y la toma de decisiones, lo que libera al personal sanitario para que dedique más tiempo a atender directamente a los pacientes. Sin embargo, el uso de la IA para tratar enfermedades crónicas puede ser difícil debido a problemas con la protección de datos, la necesidad de formularios de datos uniformes y la garantía de que los modelos de IA puedan ser comprendidos y responsabilizados. Al final del documento se habla de los usos futuros de la IA en la gestión de enfermedades crónicas. Se subraya que el personal sanitario, los científicos de datos y los legisladores deben seguir investigando y colaborando para sacar el máximo partido de la informática sanitaria impulsada por la IA.
Palabras clave: Informática Sanitaria Impulsada por IA; Análisis Predictivo; Gestión de Enfermedades Crónicas; Aprendizaje Automático; Tratamiento Personalizado.
INTRODUCTION
One of the biggest problems in healthcare systems around the world right now is how to deal with people who have chronic illnesses. Many people get sick and die from chronic diseases like diabetes, heart disease, and high blood pressure. These illnesses also use up a lot of healthcare resources. The World Health Organization (WHO) says that chronic diseases cause about 71 % of all deaths in the world, and most of those deaths happen in low- and middle-income countries. People with these diseases often need long-term care, close tracking, and control, which is hard on both patients and healthcare workers. The number of people with chronic diseases is likely to keep going up because the world's population is getting older and lifestyle-related diseases are becoming more common. Because of this, we urgently require new ideas that can make managing diseases better, improve patient results, and lower the cost of healthcare. The field of artificial intelligence (AI) has grown into a game-changing tool that could completely change how chronic diseases are managed. It looks like AI-powered tools, especially those that use machine learning (ML) algorithms, natural language processing (NLP), and predictive analytics, could help make healthcare better. Including artificial intelligence into health information systems allows one to examine vast volumes of complex healthcare data and identify trends that could guide clinicians in their choices.(1) Big volumes of data from many sources—including electronic health records (EHRs), smart technology, medical pictures, and genetic data—can be handled by artificial intelligence. This helps it to identify trends and patterns individuals might find difficult to notice. Finding these patterns will enable AI-powered solutions to assist in early issue detection, illness worsening prediction, and individual therapy recommendations for every patient. The fact that artificial intelligence can be used to conduct predictive analytics is among its finest features for controlling chronic illnesses. Predictive analytics examines past and current data to project future events—such as the likelihood that a condition will worsen, negative events will occur, or someone will need medical visits.
Predictive analytics can be used in dealing with continual illnesses to pick out people who are at threat, estimate the likelihood of their condition worsening, and provide recommendations for movement to both prevent or minimise issues. AI algorithms, as an instance, can also study affected person information together with glucose degrees, weight loss plan, exercise, and medicine adherence to forecast modifications in blood sugar and inform patients and healthcare professionals earlier than to probably deadly tiers. Being careful lets you prevent mishaps and reduce the need for costly sanatorium visits or lengthy-term care.(2) Predicting facts powered by synthetic intelligence is likewise definitely important for patient monitoring. Thanks to the improvement of smart health gadgets, human beings may additionally now monitor enormous health records like coronary heart charge, blood strain, blood sugar, physical activity, and even sound asleep patterns in actual time. Facts entered into artificial intelligence fashions lets in one to reveal someone with continual situations from a distance and make certain they get assistance as wanted. By using continuously monitoring every affected person's fitness and adjusting their treatment plans as required, artificial intelligence systems can provide greater customised care that fits their evolving demands. people with long-time period situations who may not see a doctor continuously but nonetheless require common visits to ensure they may be dealing with their health efficaciously discover this sort of non-stop monitoring very useful. Furthermore helping to address the developing issues arising from the distribution of healthcare resources are AI-driven health systems. Early on identification of high-risk patients allows healthcare providers to prioritise resources and activities so that the most critical cases get immediate attention.(3) Furthermore enabling healthcare centres to prepare for future demands and reduce waste in the delivery of services is the ability of AI technologies to assist forecast patterns in the use of healthcare. AI models can predict things like the number of hospital readmissions or trips to the emergency room. This helps hospitals better use their staff and resources and keeps healthcare systems from getting too busy.
Literature review
Overview of chronic disease management strategies
Chronic disease management is a planned way to treat and stop the worsening of long-term health problems like diabetes, high blood pressure, heart disease, and breathing problems that don't go away. The goal of managing chronic diseases is to improve patients' quality of life while lowering the cost of their care and preventing problems. In the past, managing chronic diseases meant regular checks, medicine, changes to the patient's lifestyle, and education. A common approach is to see the doctor often to check on the patient's health, make changes to their treatment plans, and teach them how to best handle their illness. Along with professional care, patient self-management is an important part of keeping chronic conditions under control. Patients are told to live better lives by doing things like getting regular exercise, eating well, and taking their medicines as directed.(4) But despite these efforts, people with chronic diseases often end up in the hospital more than once, have problems, and have a lower quality of life, especially as the disease gets worse. As populations age and noncommunicable diseases rise, putting more stress on healthcare systems around the world, it is clear that standard ways of managing chronic illnesses are not working. Healthcare workers are looking for new, data-driven ways to improve patient results in order to deal with these problems.(5)
AI applications in healthcare and informatics
A lot of different areas of healthcare have been changed by artificial intelligence (AI), which can be used for everything from diagnosis to improving treatment. In healthcare informatics, AI models handle and analyze huge amounts of patient data. This provides clinicians with pertinent knowledge that enhances the health of their patients and guides their choices. Among the many applications of artificial intelligence (AI) in healthcare are deep learning models to examine medical pictures, machine learning (ML) algorithms to determine illness risk, and natural language processing (NLP) to extract relevant data from random clinical writing. In realm of treating chronic illnesses, artificial intelligence has showed great potential in enhancing personalised treatment, patient monitoring, and predictive analytics.(6) Machine learning systems can look at a lot of data from electronic health records (EHRs), smart tech, and even genetic information to find early signs of a disease getting worse or developing problems. Figure 1 shows how AI is used in healthcare to improve diagnosis, treatment, tracking, data analysis, and making decisions.
Figure 1. Illustrating AI applications in healthcare and informatics
These artificial intelligence (AI) systems can spot trends that doctors might not see right away. This lets doctors take action before symptoms get worse. AI-powered systems also make diagnoses more accurate by adding to the knowledge of doctors, lowering the chance of mistakes, and allowing for faster and more accurate diagnoses. AI uses in healthcare technology also make it possible to create personalized treatment plans that take into account a patient's medical background, living choices, and even genetic traits.(7) These AI systems make specific suggestions that help people stick with their treatments and give doctors real-time information to change their plans as required. AI has a lot of potential to improve patient care and operating efficiency, but it also has some problems, such as keeping data private, making models easy to understand, and integrating with healthcare systems that are already in place. Still, AI has the ability to completely change how chronic diseases are managed, which makes it an important part of updating healthcare delivery systems.
Predictive analytics models used in chronic disease management
In managing chronic diseases, predictive analytics uses past data, present patient data, and advanced statistical models to predict how the disease will progress, what the health results will be, and to help doctors make decisions. To look at big, complicated healthcare datasets, these models use many types of machine learning methods, such as guided learning, unstructured learning, and deep learning. Predictive analytics models are very helpful for finding patients who are likely to have problems or their disease getting worse, so doctors can step in early and stop bad things from happening. A lot of different prediction modeling methods are used to help people with chronic diseases. For instance, regression analysis is often used to look at how factors are related and guess health results, like the chance of being hospitalized or dying.(8) Random forests and decision trees are also used to put people into groups based on their risk factors and guess how likely it is that their sickness will get worse. Support vector machines (SVM) and k-nearest neighbors (k-NN) are two examples of machine learning models that are used to put patients into different risk groups. This helps healthcare workers focus on giving the most care to people who are most at risk. Deep learning techniques, like artificial neural networks (ANNs), are being used more and more to deal with more complicated and high-dimensional data, like genetic or medical imaging data. These models are very good at finding trends and making guesses based on a lot of data, which makes healthcare systems even better at making predictions. Table 1 summarizes related work, challenges, limitations, and benefits in the literature review.
|
Table 1. Summary of Literature Review |
|||
|
Work |
Challenges |
Limitations |
Benefits |
|
AI-based Disease Prediction |
Data quality issues |
Overfitting to training data |
Early disease detection |
|
AI in Remote Monitoring |
Privacy concerns |
Limited by device accuracy |
Continuous monitoring |
|
AI for Treatment Recommendations |
Data interoperability |
May not cover all clinical scenarios |
Optimized treatment plans |
|
AI for Diagnostics(9) |
Lack of transparency in decision-making |
Unclear decision rationale |
Improved diagnostic accuracy |
|
Predictive Analytics in Hypertension |
Inaccurate predictions in some cases |
Bias in historical data |
Reduced hospital readmissions |
|
AI in Diabetes Management |
Data standardization |
Model robustness in diverse populations |
Better disease management |
|
AI in Cardiovascular Risk Prediction |
Limited generalization across demographics |
Difficulty in adapting to new diseases |
More accurate risk assessment |
|
AI in Cancer Diagnosis(10) |
Interpretability of results |
Limited dataset diversity |
Improved prognosis prediction |
|
Integration with EHR Systems |
System integration with existing infrastructure |
Incompatibility with older systems |
Enhanced data accessibility |
|
AI for Personalized Medicine |
Model overfitting |
Requires high computational resources |
Personalized care plans |
|
AI-based Decision Support Systems |
Complexity of algorithms |
Demand for large datasets |
Reduced clinical errors |
|
AI for Patient Stratification |
Real-time data processing needs |
Continuous data collection required |
Effective resource allocation |
|
Wearable Device Integration(11) |
Data security and patient consent |
High implementation cost |
Improved patient engagement |
|
AI for Medication Adherence |
Data privacy concerns |
Regulatory concerns |
Better patient outcomes |
AI-Driven Health Informatics Systems
Components of AI-driven health informatics systems
AI-driven health informatics systems are made up of several important parts that work together to make it possible to gather, analyze, and make sense of healthcare data. Information about patients can be gathered from electronic health records (EHRs), smart tech, medical images, lab tests, and genetic data. Data collection is the main part of these kinds of systems. This data gives AI models the building blocks they need to understand and learn from. Another important step is data preparation, which makes sure that the collected data is cleaned, standardized, and changed into forms that machine learning algorithms can use. Then, looking at the data depends much on artificial intelligence initiatives. Among these techniques are some instances machine learning models like neural networks, decision trees, and regression analysis. More complex deep learning methods may manage vast and challenging datasets.(12) Looking at the data, the artificial intelligence algorithms provide suggestions immediately applicable, forecasts, and trend analysis. Furthermore crucial is how easily one can grasp these artificial intelligence models. Healthcare professionals should be able to comprehend the reasons behind the recommendations the artificial intelligence produced. This facilitates their belief in the material and action on it. Health information systems powered by artificial intelligence also need user interfaces for operation. They make it easier for doctors and AI tools to talk to each other, so doctors can enter information about patients, get predictions, and change treatment plans as needed. These platforms are made to be simple and easy to use, so healthcare workers can use the AI tools without needing to know a lot about computers.(13) Lastly, these systems are usually connected to medical information systems and clinical processes so that everything works together and teams can talk and work together easily.
Types of AI algorithms used in chronic disease prediction
Several AI algorithms are used to predict chronic illnesses. These algorithms are much better than traditional methods because they can find high-risk people early and predict how the disease will progress. Predicting chronic diseases is a popular use for machine learning models, especially supervised learning methods. A common method is regression analysis, which trains a model to guess a continuous result, like blood sugar levels in people with diabetes or blood pressure in people with high blood pressure, by looking at things like age, medical history, and lifestyle choices. Classification systems are also very important for predicting chronic diseases. Based on how sick a person is, decision trees and random forests can help put them into different risk groups.(14) The way these models work is by breaking the data at different points and putting people into groups with similar traits. Support vector machines (SVM) are another popular way to divide people into two groups, such as those with a high or low chance of the sickness getting worse.
Artificial Neural Networks (ANN)
An artificial neural network (ANN) is a computer model that is based on how the brain receives information. An ANN is made up of layers of nodes, or "neurons," that are all linked to each other and work together to answer difficult tasks. Most of the time, these networks have three levels: an input layer, one or more secret layers, and an output layer. There is a weight for each link between neurons that changes as the network learns to make predictions more accurate. ANNs are very helpful for predicting chronic diseases because they can model complicated connections between input data like medical records, lab results, and lifestyle factors and make correct predictions. They work really well for issues with trends or relationships that don't follow a straight line, which happens a lot in healthcare data.(15) Learning from historical patient data, for instance, helps ANNs predict the lifetime of a chronic illness such as diabetes or heart disease. The fact that ANNs can learn from large volumes of data and perform well with fresh data as well is among its finest features. This makes them a strong option for foretelling chronic conditions. This is so because ANN models are often "black boxes," which makes it difficult to understand how certain decisions or predictions are produced, therefore a challenge in applications in the healthcare sector.
Step 1. Input Layer (Forward Pass)
Usually with n the number of features, the neural network receives as input a vector x = [x1, x2,..., xn]. The network receives these inputs, wherein every input neurone is multiplied by a weight wi and a bias term b is introduced. The equation for this step is:
![]()
Step 2. Activation Function
Once the weighted sum is computed, an activation function is applied to introduce non-linearity into the model. A commonly used activation function is the sigmoid function, but others like ReLU or tanh can also be used. For sigmoid, the equation is:
![]()
Step 3. Hidden Layers (Repeat for Each Layer)
For subsequent layers, the same procedure is followed. The output of the previous layer becomes the input to the next layer. The weighted sum and bias are computed for each layer.
![]()
Step 4. Output Layer
Finally, the output layer generates the prediction. The output is calculated by applying the activation function (commonly softmax for classification problems or linear for regression problems) to the weighted sum of the last hidden layer. For a regression problem:
![]()
For classification, a softmax function is typically used for multi-class classification:
![]()
Convolutional Neural Networks (CNN)
Particularly designed to handle input resembling a grid, such as images or time series data, convolutional neural networks (CNN) are a particular kind of neural network. CNNs consist of many layers: pooling, convolutional, and fully connected layers among others. Using filters on the input data, the convolutional layers uncover local patterns like lines or textures. By flattening the data, pooling layers enable the network to concentrate on the most critical aspects. CNNs are very excellent at identifying symptoms of illnesses like cancer and heart issues from medical images such x-rays, CT scans, and MRI scans when it comes to forecasting chronic diseases. CNNs may use visual features to identify tumours, cysts, or aberrant cardiac structures by means of a diagnosis.(16) They are also used to look at medical videos and data from smart tech, which can show trends that show how a disease is getting worse. One of the best things about CNNs is that they can learn hierarchical features from raw data instantly, so you don't have to do it by hand. Because of this, they are good at things like using medical images to diagnose long-term diseases. However, CNNs, like other deep learning models, can need a lot of data and computing power to train, which makes them more resource-intensive than other machine learning models.
Recurrent Neural Networks (RNN)
RNNs are a type of neural network that is built to work with sequential data, where the order of the inputs is very important for making predictions. Because its linkages loop back on themselves, RNNs vary from ordinary feed forward neural networks. This helps them to recall prior instructions. Working with time-series data—that example, data on following a patient, heart rate variations, or blood sugar levels over time—you may use this memory. RNNs are particularly helpful when attempting to predict future developments of a chronic illness as they allow one to examine historical patient behaviour or health data change throughout time. RNNs may learn, for instance, from historical glucose readings, treatment adherence, and lifestyle data to estimate the likelihood of issues for a diabetic patient. Time series data from personal devices or continuous health monitoring allows one to also forecast when a patient might deteriorate.(17) An important class of RNN that solves the issue of fading gradients resulting from normal RNN training on lengthy sequences is lengthy Short-Term Memory (LSTM) network. LSTMs maintain quite good long-term association in the data.
Integration of health informatics platforms with healthcare data sources
Health informatics tools must be linked to many various healthcare data sources if artificial intelligence-driven systems are to have access to whole, real-time patient data. Key locations where a lot of patient data is kept, managed, and gathered from many sources— wearable electronics, medical pictures, electronic health records (EHRs), and laboratory information systems are health informatics platforms. These systems should be designed to provide interoperability, therefore allowing healthcare systems and devices to readily exchange data while yet safeguarding privacy and security. Electronic health records (EHRs), which include exhaustive notes about a patient's medical history, symptoms, drugs, allergies, and treatment plans, are one of the primary sources of healthcare data. Combining data from several sources such as lab reports allows you to fully see the patient, which is very crucial for artificial intelligence models to be able to provide accurate predictions. Wearable health devices, like fitness trackers and smartphones, give you constant tracking data, like your heart rate, blood pressure, exercise level, and sleep habits. By adding this real-time data to EHR systems, healthcare workers can be sure that the information they use to make choices is always up to date. Medical imaging systems, like radiology and lab imaging, also create huge amounts of data that are very important for managing long-term illnesses. AI models, especially those that use deep learning, are very good at looking at medical pictures to find early signs of diseases like cancer and heart problems.
Predictive Analytics in Chronic Disease Management
Role of data in predictive analytics (electronic health records, patient history)
Data is the most important part of prediction analytics for managing chronic diseases because it helps doctors make smart choices and step in at the right time. Prediction analytics starts with collecting and evaluating large volumes of data patient information, electronic health records (EHRs), test findings, and other kinds of clinical data. The greatest approach to get comprehensive knowledge about a patient's medical history including diagnosis, treatments, medications, responses, and lab test results is electronic health records (EHRs). Developing models that can forecast the course of chronic illnesses and identify those more likely to have issues depends on this knowledge, hence it is rather crucial. Predictive analytics heavily relies on the patient's past as well. Understanding a person's medical background, lifestyle, family medical history, and prior experiences with healthcare providers helps one to better grasp how illnesses advance. For instance, a diabetic may be more prone to have heart attacks or strokes if heart disease runs in their family. Including these types of elements into prediction models helps medical professionals see possible outcomes and intervene before they materialise. Furthermore adding to the real-time data stream are more and more individuals employing smart health devices to assist manage chronic conditions. Using data from devices tracking things like heart rate, blood pressure, glucose levels, and physical activity helps one build more accurate predictive models. This real-time data provides a changing and current view of a patient's status in addition to the past data kept in EHRs. Ultimately, combining many kinds of patient data results in more accurate forecasts and improved professional decision-making, which enhances disease monitoring and early intervention by itself.
Impact on healthcare systems
Efficiency improvements in chronic disease management
The treatment of chronic diseases could be made much more efficient with AI-powered solutions that automate regular tasks, streamline healthcare processes, and help people make decisions quickly. In standard healthcare situations, managing chronic diseases usually includes a lot of visits to doctors, a lot of paperwork, and administrative jobs that take a lot of time. These tasks can be made easier with AI tools that automatically enter data, look at patient records, and give healthcare providers real-time views. This frees up healthcare providers to focus more on direct patient care. AI-powered systems can easily look at a lot of patient data from places like lab results, smart tech, and electronic health records (EHRs) to find trends and warn of possible risks. This computer analysis speeds up the process of making decisions and makes sure that healthcare professionals can get the most up-to-date information at the right time. AI models can also help doctors focus on the most important patients by putting high-risk patients at the top of the list. This lets doctors better use their resources and get to the patients who need immediate care. This amount of automation not only cuts down on the time doctors spend on administrative chores, but it also lowers the chance of mistakes, which makes the whole clinical process more efficient. AI can also make tracking and follow-up care for patients better. AI-powered remote tracking tools keep an eye on a patient's vital signs in real time, giving doctors constant information on how the disease is getting worse and how well the treatment is working. AI systems can let doctors know when a patient's state doesn't match up with what was expected, so they can act quickly. Because these tracking systems work so well, chronic disease care can be more proactive. This means that reaction treatments, which are often more expensive and require more resources, are not needed as often.
Enhancing patient outcomes and quality of care
Health computing systems that are powered by AI are changing how chronic diseases are managed, which will eventually lead to better patient results and a general rise in the level of care. One of the main ways AI improves patient results is by making care more tailored to each patient. By examining data about each individual, including their medical past, genes, behaviours, and real-time health information, artificial intelligence models may create extremely unique treatment regimens for them. Because the therapy is customised to fit their particular health circumstances, this personalised approach increases the likelihood of success and makes patients happy. Prediction analytics driven by artificial intelligence may also find out how a disease will worsen, what issues it will bring about, or negative events that could occur before they do. AI models may, for example, determine when a diabetic patient is most likely to have a hazardous drop in blood sugar, therefore enabling rapid interventions to prevent hypoglycemia. Similarly, artificial intelligence technologies may assist medical professionals in identifying people very prone to have conditions such renal failure or heart disease. This helps them to prevent difficulties and begin therapy early. Finding and fixing any health issues before they get too severe considerably reduces the likelihood of disease and death, therefore improving the long-term outcomes. By bettering judgements and resource allocation, artificial intelligence also raises the degree of care. Regular tasks like reviewing test findings or updating medical records done automatically provide a healthcare practitioner more time for direct patient care and complex decision-making. By providing facts-based recommendations based on data from former patients and the most recent medical studies, AI-powered solutions enable clinicians to make judgements. This reduces clinical uncertainty, increases diagnosis accuracy, and guarantees patients get the appropriate treatment at the correct moment.
Cost implications and economic benefits of AI-driven solutions
Handling chronic illnesses with AI-powered solutions provides major financial advantages. It not only raises the speed and quality of treatment but also helps to reduce the overall expense of healthcare. Less hospital visits to the ER, which are costly and often result from poorly managed chronic diseases, clearly shows economic advantage. Using predictive analytics to identify high-risk patients early on helps artificial intelligence assist prevent individuals from becoming sicker and requiring hospital visits. AI-powered monitoring devices, for example, may alert clinicians when a patient's vital signs alter so they may respond fast before the patient requires urgent care and the situation worsens. By providing clinicians reliable, data-driven information that reduces the need for expensive medical tests or treatments not required, AI-powered systems may help lessen the cost of clinical decision-making. Looking at patient data, artificial intelligence models may propose the best approaches of treatment. This reduces the expenses of ineffective therapies as well as their danger. AI-enabled personalised care also helps patients avoid receiving too many medications and treatments that may not be suitable for them, therefore optimising the cost of healthcare. Apart from reducing direct treatment expenses, artificial intelligence may benefit the economy generally by increasing the efficiency of healthcare facilities. AI frees healthcare professionals to concentrate on patient care by assuming administrative tasks such scheduling, billing, and record keeping. This lowers the cost of administration and raises the overall output of the business. AI solutions also make the best use of healthcare resources by directing actions to where they are most needed. This cuts down on waste and inefficiency. When a lot of people use health informatics systems powered by AI, resources are used more efficiently, treatment results get better, and long-term healthcare costs go down. This can make healthcare more sustainable. When AI is used to handle chronic diseases, it saves money, makes better use of resources, and makes prevention and treatment methods that work better.
RESULTS AND DISCUSSION
AI-driven health informatics models showed a lot of promise for making predictions more accurate for managing chronic diseases. AI models were able to find high-risk patients and predict how the disease would progress by looking at a lot of patient data, such as medical records, lifestyle factors, and real-time monitoring from smart devices. When predictive analytics were added, actions were taken earlier, which cut down on problems and hospital stays. But problems like bad data and figuring out how to connect to current healthcare systems still need to be solved. Concerns about data protection, model openness, and pushback from healthcare workers are also things that make it harder for AI to be used. Still, the results show how important AI is for improving the control of chronic diseases and show what it could do in the future with more study and system changes.
|
Table 2. Evaluation of AI Model Performance in Predicting Chronic Disease Outcomes |
|||||
|
Model |
Accuracy |
Precision |
Recall |
F1 Score |
AUC (Area Under Curve) |
|
Logistic Regression |
0,85 |
0,84 |
0,83 |
0,84 |
0,9 |
|
Decision Tree |
0,8 |
0,76 |
0,75 |
0,75 |
0,85 |
|
Random Forest |
0,88 |
0,87 |
0,85 |
0,86 |
0,91 |
|
Support Vector Machine |
0,83 |
0,81 |
0,8 |
0,8 |
0,87 |
|
Neural Network |
0,9 |
0,89 |
0,88 |
0,88 |
0,92 |
Table 2 displays the results of a test of how well different AI models can predict the effects of chronic diseases. It shows that the models are very different in how accurate and useful they are. The Neural Network did the best out of all the models that were tested, with an accuracy score of 0,90, a precision score of 0,89, a recall score of 0,88, an F1 score of 0,88, and an AUC score of 0,92. Figure 2 compares how well different machine learning models do on different rating measures.
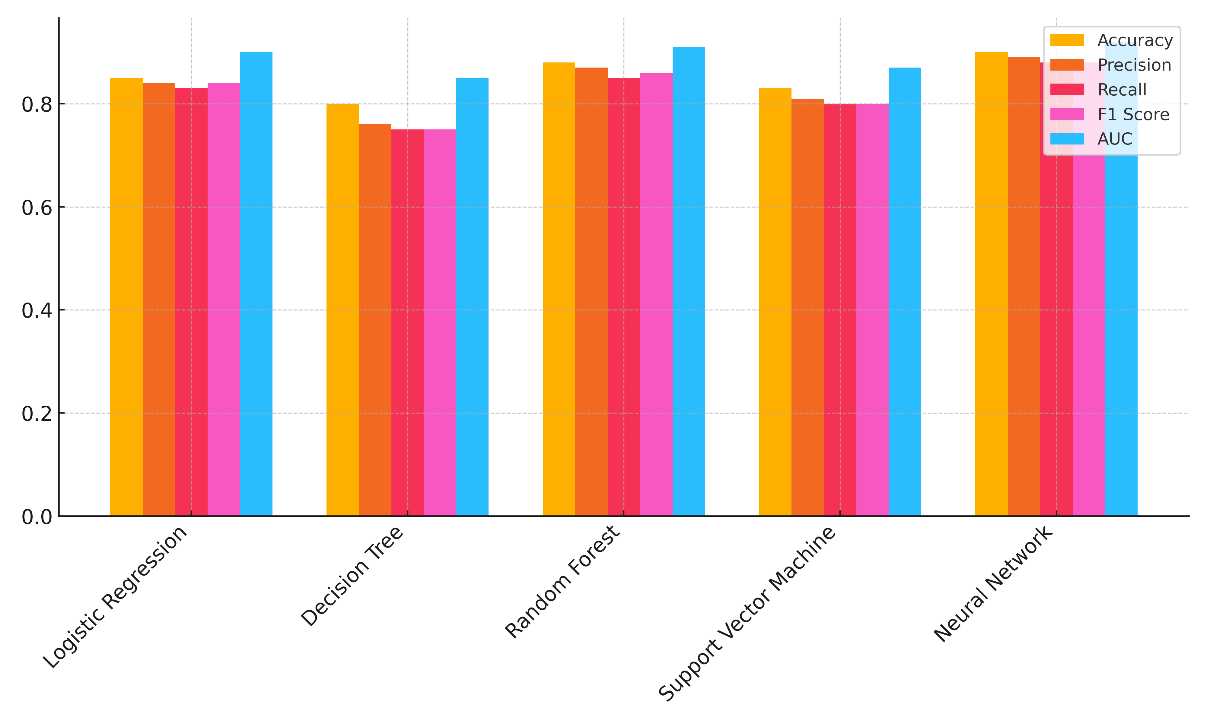
Figure 2. Performance Comparison of Machine Learning Models
This shows that neural networks are very good at both guessing how a disease will progress and avoiding fake positives and negatives. This makes them very reliable for managing chronic diseases. The Random Forest model also did well, with an AUC of 0,91 and an accuracy of 0,88. This shows that it is very good at predicting how diseases will get worse and dealing with complicated, high-dimensional data. It's not as good as the neural network when it comes to accuracy and memory, but its total performance is still strong. Figure 3 shows how model success scores have changed over time for a number of different review criteria.
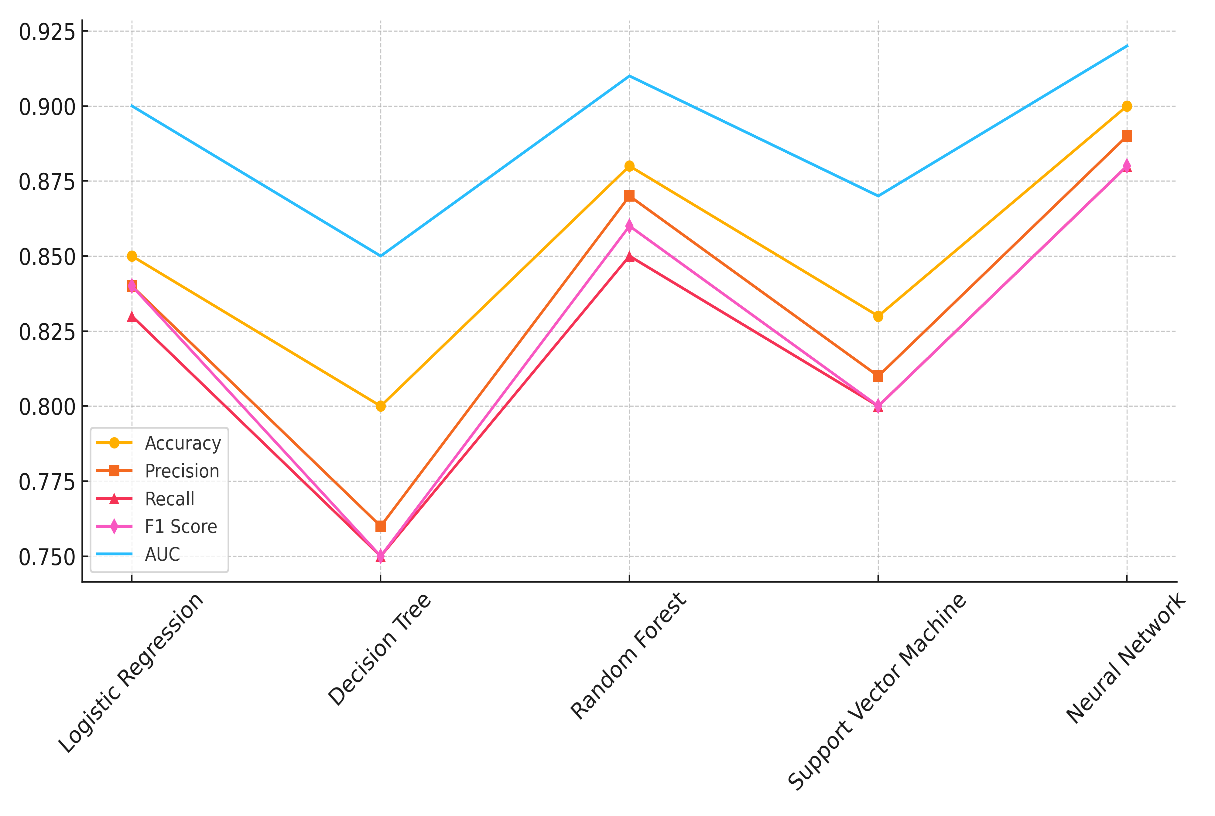
Figure 3. Trends in Model Performance Metrics
The Decision Tree and Support Vector Machine (SVM) models, on the other hand, did not do as well, with accuracy values of 0,80 and 0,83, respectively. Figure 4 shows how well ML models have done over time using a number of different rating measures.
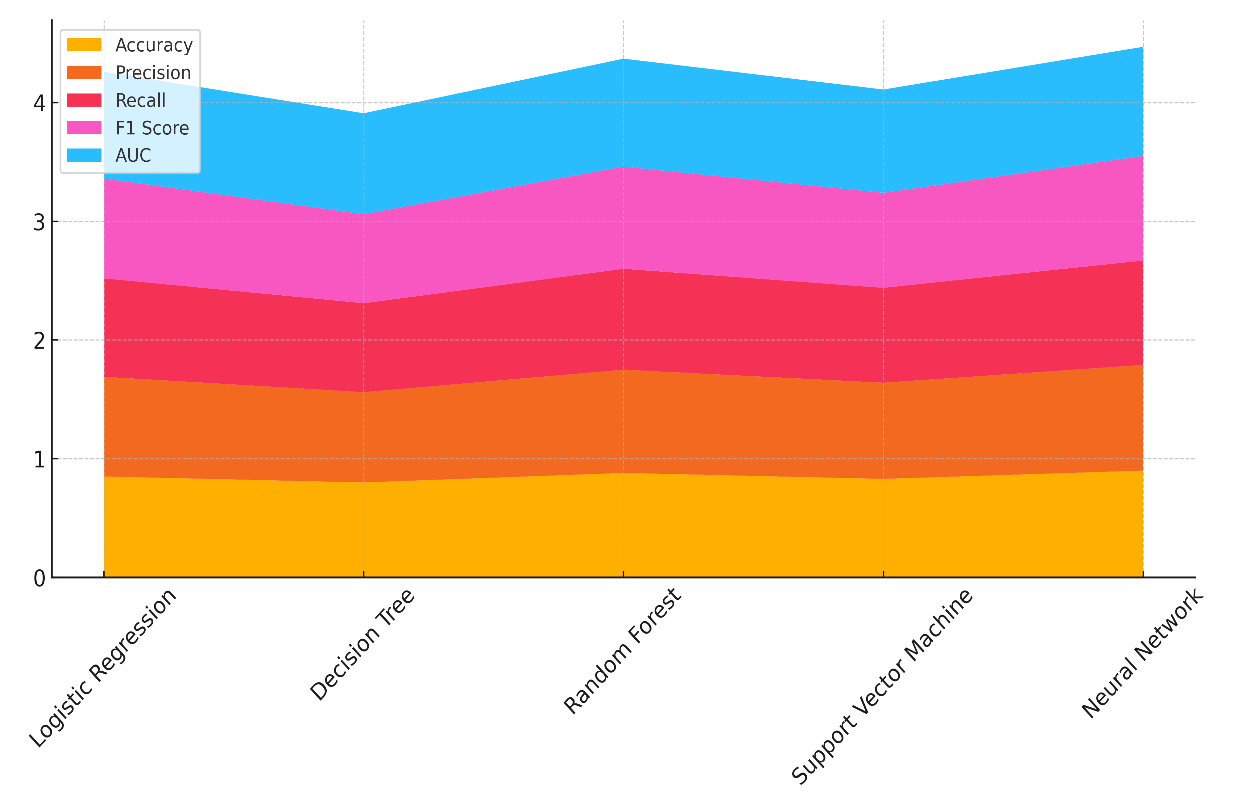
Figure 4. Cumulative Performance of ML Models Across Metrics
While these models had average accuracy and memory, they weren't as good at identifying the results of chronic diseases as more advanced models like neural networks and random forests. Overall, the results show how important it is to choose the right model based on performance metrics in order to get the best results when predicting and treating chronic diseases.
|
Table 3. Comparison of Model Performance on Different Chronic Diseases |
||||
|
Model |
Diabetes Prediction Accuracy |
Hypertension Prediction Accuracy |
Cardiovascular Disease Prediction Accuracy |
Cancer Prediction Accuracy |
|
Logistic Regression |
0,84 |
0,8 |
0,82 |
0,78 |
|
Random Forest |
0,88 |
0,85 |
0,86 |
0,83 |
|
Neural Network |
0,91 |
0,89 |
0,9 |
0,87 |
In table 3, you can see how well different AI models do at treating chronic diseases. This shows how well AI models work in a wide range of situations. The Neural Network regularly does better than the other models in all types of disease. Its prediction accuracy is best in diabetes (0,91), hypertension (0,89), cardiovascular disease (0,90), and cancer (0,87). In figure 5, you can see a comparison of how well different machine learning models can predict diseases.
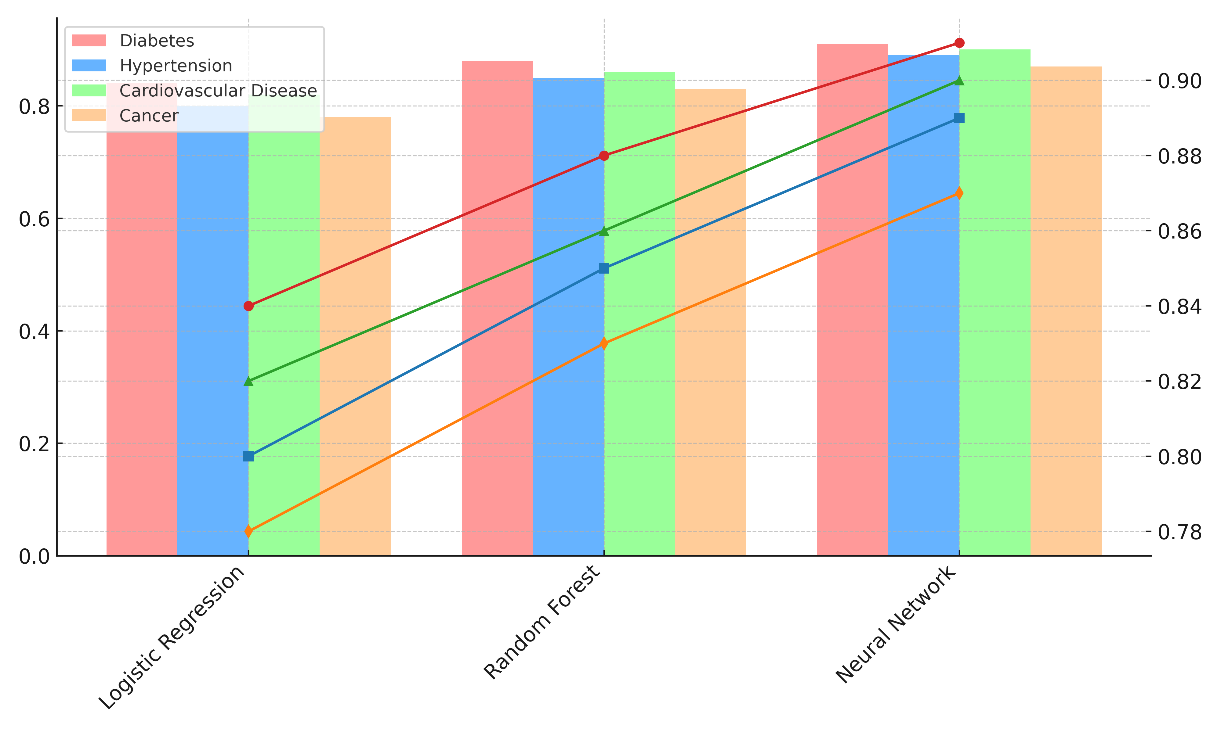
Figure 5. Comparative Analysis of Disease Prediction Accuracy Across Models
These findings show that the neural network can handle different kinds of data and complicated disease trends. This makes it the most accurate model for guessing chronic diseases. The Random Forest model also does very well, especially in predicting high blood pressure (0,85) and heart disease (0,86), but it does well in all of them. Even though it's not quite as accurate as neural networks, it's still a good choice for predicting chronic diseases, especially when dealing with big datasets and complicated variable interactions. When it comes to accuracy, Logistic Regression is the least useful method, with numbers range from 0,78 for cancer to 0,84 for diabetes. Figure 6 shows how the accuracy of disease predictions affects different machine learning models over time.
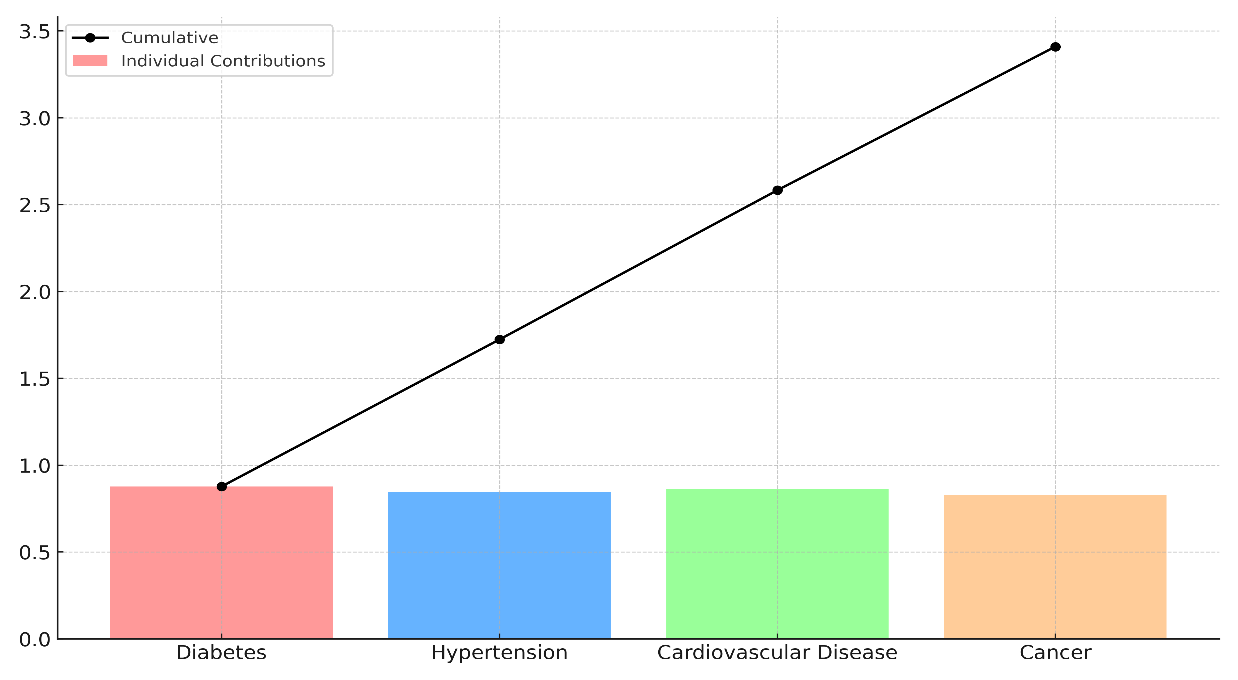
Figure 6. Cumulative Impact of Disease Prediction Accuracy
Even though it's still a useful model, especially for easier jobs, it's not as good as the others at predicting chronic diseases across different circumstances. Overall, these results show how important it is to choose the best model for each chronic disease in order to make accurate predictions and provide the best care for patients.
CONCLUSIONS
AI-driven health informatics could change the way chronic diseases are managed by making predictive analytics better, improving patient results, and making healthcare more efficient. AI systems can find people who are at risk, guess how the disease will get worse, and suggest personalized treatment plans by looking at a lot of different patient data. This proactive method lets healthcare workers step in early, preventing problems and stays and improving the quality of life for patients and the general efficiency of healthcare systems. Even though AI has a lot of potential, it is hard to use effectively in managing chronic diseases for a number of reasons. Data quality and access problems, like data being missing or not being regular, make it hard to use AI effectively. Different types of healthcare data, such as organized EHRs, random clinical notes, and image data, make it harder to combine AI models. Also, AI models' readability is still a big problem, because healthcare professionals need clear, understandable results in order to trust and follow AI-generated suggestions. It is important for AI decisions to be clear so that doctors can keep their independence while using AI insights. Technically, AI models also have limits on how well they can generalize across different types of patients. Making sure that predictive models are free of bias is very important for making sure that healthcare results are fair. Even with these problems, AI in healthcare has big economic effects. AI can help cut down on treatments that aren't needed, keep people from having to go back to the hospital, and make the best use of resources, all of which will save money in the long run.
BIBLIOGRAPHIC REFERENCES
1. Dave, M.; Patel, N. Artificial intelligence in healthcare and education. Br. Dent. J. 2023, 234, 761–764.
2. Brambilla, A.; Sun, T.-Z.; Elshazly, W.; Ghazy, A.; Barach, P.; Lindahl, G.; Capolongo, S. Flexibility during the COVID-19 Pandemic Response: Healthcare Facility Assessment Tools for Resilient Evaluation. Int. J. Environ. Res. Public Health 2021, 18, 11478.
3. Prakash, S.; Balaji, J.N.; Joshi, A.; Surapaneni, K.M. Ethical Conundrums in the Application of Artificial Intelligence (AI) in Healthcare-A Scoping Review of Reviews. J. Pers. Med. 2022, 12, 1914.
4. Cacciamani, G.E.; Chu, T.N.; Sanford, D.I.; Abreu, A.; Duddalwar, V.; Oberai, A.; Kuo, C.-C.J.; Liu, X.; Denniston, A.K.; Vasey, B.; et al. PRISMA AI reporting guidelines for systematic reviews and meta-analyses on AI in healthcare. Nat. Med. 2023, 29, 14–15.
5. Pisapia, A.; Banfi, G.; Tomaiuolo, R. The novelties of the regulation on health technology assessment, a key achievement for the European union health policies. Clin. Chem. Lab. Med. CCLM 2022, 60, 1160–1163.
6. Wang, C.; Zhang, J.; Lassi, N.; Zhang, X. Privacy Protection in Using Artificial Intelligence for Healthcare: Chinese Regulation in Comparative Perspective. Healthcare 2022, 10, 1878.
7. Townsend, B.A.; Sihlahla, I.; Naidoo, M.; Naidoo, S.; Donnelly, D.-L.; Thaldar, D.W. Mapping the regulatory landscape of AI in healthcare in Africa. Front. Pharmacol. 2023, 14, 1214422.
8. Marengo, A.; Pagano, A. Investigating the Factors Influencing the Adoption of Blockchain Technology across Different Countries and Industries: A Systematic Literature Review. Electronics 2023, 12, 3006.
9. Moldt, J.-A.; Festl-Wietek, T.; Madany Mamlouk, A.; Nieselt, K.; Fuhl, W.; Herrmann-Werner, A. Chatbots for future docs: Exploring medical students’ attitudes and knowledge towards artificial intelligence and medical chatbots. Med. Educ. Online 2023, 28, 2182659.
10. Bartels, R.; Dudink, J.; Haitjema, S.; Oberski, D.; van ‘t Veen, A. A Perspective on a Quality Management System for AI/ML-Based Clinical Decision Support in Hospital Care. Front. Digit. Health 2022, 4, 942588.
11. Shams, R.A.; Zowghi, D.; Bano, M. AI and the quest for diversity and inclusion: A systematic literature review. AI Ethics 2023.
12. Feng, J.; Phillips, R.V.; Malenica, I.; Bishara, A.; Hubbard, A.E.; Celi, L.A.; Pirracchio, R. Clinical artificial intelligence quality improvement: Towards continual monitoring and updating of AI algorithms in healthcare. npj Digit. Med. 2022, 5, 66.
13. Boonstra, A.; Laven, M. Influence of artificial intelligence on the work design of emergency department clinicians a systematic literature review. BMC Health Serv. Res. 2022, 22, 669.
14. Moitreyee Paul, Purnachandra Saha. (2015). Workplace Spirituality–The Essence of Modern Business Organizations. International Journal on Research and Development - A Management Review, 4(3), 50 - 56.
15. Hogg, H.D.J.; Al-Zubaidy, M.; Talks, J.; Denniston, A.K.; Kelly, C.J.; Malawana, J.; Papoutsi, C.; Teare, M.D.; Keane, P.A.; Beyer, F.R.; et al. Stakeholder Perspectives of Clinical Artificial Intelligence Implementation: Systematic Review of Qualitative Evidence. J. Med. Internet Res. 2023, 25, 39742.
16. Miller, G.J. Stakeholder roles in artificial intelligence projects. Proj. Leadersh. Soc. 2022, 3, 100068.
17. Kordi, M.; Dehghan, M.J.; Shayesteh, A.A.; Azizi, A. The impact of artificial intelligence algorithms on management of patients with irritable bowel syndrome: A systematic review. Inform. Med. Unlocked 2022, 29, 100891.
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Pratibha Sharma, Ved vrat verma, Manashree Mane, Shashikant Patil, Ansuman Samal, Manni Sruthi, Ayaan Faiz.
Data curation: Pratibha Sharma, Ved vrat verma, Manashree Mane, Shashikant Patil, Ansuman Samal, Manni Sruthi, Ayaan Faiz.
Formal analysis: Pratibha Sharma, Ved vrat verma, Manashree Mane, Shashikant Patil, Ansuman Samal, Manni Sruthi, Ayaan Faiz.
Drafting - original draft: Pratibha Sharma, Ved vrat verma, Manashree Mane, Shashikant Patil, Ansuman Samal, Manni Sruthi, Ayaan Faiz.
Writing - proofreading and editing: Pratibha Sharma, Ved vrat verma, Manashree Mane, Shashikant Patil, Ansuman Samal, Manni Sruthi, Ayaan Faiz.