doi: 10.56294/mw2024510
ORIGINAL
Personalized Health Informatics Platforms for Patient-Centric Remote Care and Telehealth Optimization
Plataformas informáticas sanitarias personalizadas para la teleasistencia centrada en el paciente y la optimización de la telesalud
Sarbeswar
Hota1 ![]() *,
Bodireddy Vamalatha2
*,
Bodireddy Vamalatha2 ![]() , Gourav Sood3
, Gourav Sood3
![]() , Simran Kalra4
, Simran Kalra4
![]() , Ajab Singh Choudhary5
, Ajab Singh Choudhary5
![]() , Manashree Mane6
, Manashree Mane6
![]() , Zuleika Homavazir7
, Zuleika Homavazir7
![]()
1Department of Computer Applications, Siksha ‘O’ Anusandhan (Deemed to be University). Bhubaneswar, Odisha, India.
2Centre for Multidisciplinary Research, Anurag University. Hyderabad, Telangana, India.
3Chitkara Centre for Research and Development, Chitkara University. Himachal Pradesh-174103 India.
4Centre of Research Impact and Outcome, Chitkara University. Rajpura- 140417, Punjab, India.
5School of Allied Health Sciences, Noida International University. Greater Noida, Uttar Pradesh, India.
6Forensic Science, JAIN (Deemed-to-be University). Bangalore, Karnataka, India.
7Department of ISME, ATLAS SkillTech University. Mumbai, Maharashtra, India.
Cite as: Hota S, Vamalatha B, Sood G, Kalra S, Choudhary AS, Mane M, et al. Personalized Health Informatics Platforms for Patient-Centric Remote Care and Telehealth Optimization. Seminars in Medical Writing and Education. 2024; 3:510. https://doi.org/10.56294/mw2024510
Submitted: 11-10-2023 Revised: 13-01-2024 Accepted: 14-05-2024 Published: 15-05-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Sarbeswar Hota *
ABSTRACT
Improving telemedicine services and making virtual care more patient-centered depend on personalised health informatics systems. These platforms leverage innovative technologies such artificial intelligence, machine learning, and data analytics as healthcare systems evolve to fit a digital-first world to provide tailored treatment plans, real-time monitoring, and future-use health information. With an eye towards how they may enhance patient outcomes, improve healthcare services, and reduce running costs, this article explores how tailored health information systems might be employed in telemedicine. These instruments help to give accurate, tailored treatment that is more effective and sensitive to each patient’s requirements by utilising knowledge on each patient’s medical history, genetics, habits, and real-time biometrics. Combining artificial intelligence with machine learning enables constant data analysis. This gives us predictive analytics that can find early signs of health problems and help us make better decisions about care. Personalised health informatics systems also encourage patient participation by giving them tools for self-monitoring and communicating with healthcare providers. This leads to better relationships between patients and providers and better obedience to treatment plans. As remote care gets better and easier to use, doctors and nurses can take care of more patients without lowering the level of care. Also, using safe ways to share data protects patients’ privacy and makes it easy for patients, carers, and healthcare teams to talk to each other. Even though there have been improvements, problems like data protection, interoperability, and following the rules are still stopping these platforms from being widely used. This paper talks about these problems and suggests ways to make them less severe. Personally tailored health information systems are a huge step forward in telemedicine. They could change the way online medical services are provided, making them more effective, easier to access, and focused on the patient.
Keywords: Personalized Health Informatics; Telehealth Optimization; Remote Care; Artificial Intelligence; Patient-Centric Care; Predictive Analytics.
RESUMEN
La mejora de los servicios de telemedicina y una atención virtual más centrada en el paciente dependen de sistemas informáticos sanitarios personalizados. Estas plataformas aprovechan tecnologías innovadoras, como la inteligencia artificial, el aprendizaje automático y el análisis de datos, a medida que los sistemas sanitarios evolucionan para adaptarse a un mundo digital, con el fin de ofrecer planes de tratamiento personalizados, seguimiento en tiempo real e información sanitaria de uso futuro. Con la vista puesta en cómo pueden mejorar los resultados de los pacientes, perfeccionar los servicios sanitarios y reducir los costes de funcionamiento, este artículo explora cómo pueden emplearse los sistemas de información sanitaria a medida en telemedicina. Estos instrumentos ayudan a administrar tratamientos precisos y personalizados, más eficaces y sensibles a las necesidades de cada paciente, gracias al conocimiento de su historial médico, su genética, sus hábitos y sus datos biométricos en tiempo real. La combinación de la inteligencia artificial con el aprendizaje automático permite un análisis constante de los datos. Esto nos proporciona análisis predictivos que pueden encontrar signos tempranos de problemas de salud y ayudarnos a tomar mejores decisiones sobre la atención. Los sistemas informáticos de salud personalizados también fomentan la participación de los pacientes al proporcionarles herramientas de autocontrol y comunicación con los profesionales sanitarios. Esto mejora las relaciones entre pacientes y proveedores y la obediencia a los planes de tratamiento. A medida que la teleasistencia mejora y se hace más fácil de usar, médicos y enfermeros pueden atender a más pacientes sin rebajar el nivel de atención. Además, el uso de métodos seguros para compartir datos protege la intimidad de los pacientes y facilita la comunicación entre pacientes, cuidadores y equipos sanitarios. Aunque se han producido mejoras, problemas como la protección de datos, la interoperabilidad y el cumplimiento de las normas siguen impidiendo el uso generalizado de estas plataformas. Este artículo habla de estos problemas y sugiere formas de hacerlos menos graves. Los sistemas de información sanitaria personalizados son un gran paso adelante en la telemedicina. Podrían cambiar la forma en que se prestan los servicios médicos en línea, haciéndolos más eficaces, de más fácil acceso y centrados en el paciente.
Palabras clave: Informática Sanitaria Personalizada; Optimización de la Telesalud; Teleasistencia; Inteligencia Artificial; Atención Centrada en el Paciente; Análisis Predictivo.
INTRODUCTION
Technology advances are causing a huge shift in healthcare, and personalised health information systems are becoming some of the most important parts of this change. Advanced data analytics, artificial intelligence (AI), and machine learning are used by these tools to make healthcare solutions that are specific to each patient's needs. Telehealth services have become more popular around the world, especially since the COVID-19 pandemic, because they are easier to get to and more handy than standard in-person healthcare. Personalised health information systems are very important for making remote care work better, improving the level of care for patients, and making health results better, especially for managing chronic diseases and preventative healthcare. Personalised health informatics systems are made to collect, handle, and analyse huge amounts of data from many places, like electronic health records (EHRs), smart tech, and data created by patients. Every patient who passes in real time should be shown fully and dynamically.(1) Using this data can help medical practitioners better understand the health issues and lifestyle circumstances of their patients, therefore enabling more tailored treatment strategies. These programs are more precise and practical as they are designed to meet every person's health, genes, even personal preferences. People are thus more likely to keep on their therapies and see improvement. These technologies are built on artificial intelligence, which also is fundamental in enabling data-driven judgements. Programmes in machine learning search for patterns in extremely big datasets. This allows clinicians to predict a patient's possible ailments, see early symptoms of sickness, and make forward treatment plans. By gathering data from gadgets a patient wears glucose meters, heart rate monitors, sleep tracks AI can also monitor their health. Healthcare personnel have the ability to respond fast thanks to this consistent flow of real-time data, therefore preventing major health issues before they start and reducing the hospital visit count.
Telehealth medical treatment delivered over the phone or online is another crucial component of personalised health informatics. Particularly in rural or underdeveloped regions, personalised health systems and telemedicine cooperate to make healthcare more accessible. Without having to travel a great distance, patients may consult their physicians via video conferences, get follow-up treatment from far away, and even participate in virtual health meetings.(2) This facilitates the access to healthcare facilities, therefore reducing wait times and lessening of stress in healthcare institutions. By providing tools enabling individuals to be more engaged in managing their own health, personalised health informatics systems may help increase patient participation. Easy for anybody to use platforms let patients access their health information, check on their condition, create objectives, and communicate directly to their healthcare providers. By concentrating on the patient, figure 1 demonstrates how tailored health systems enhance virtual care and enable improved performance of telemedicine.
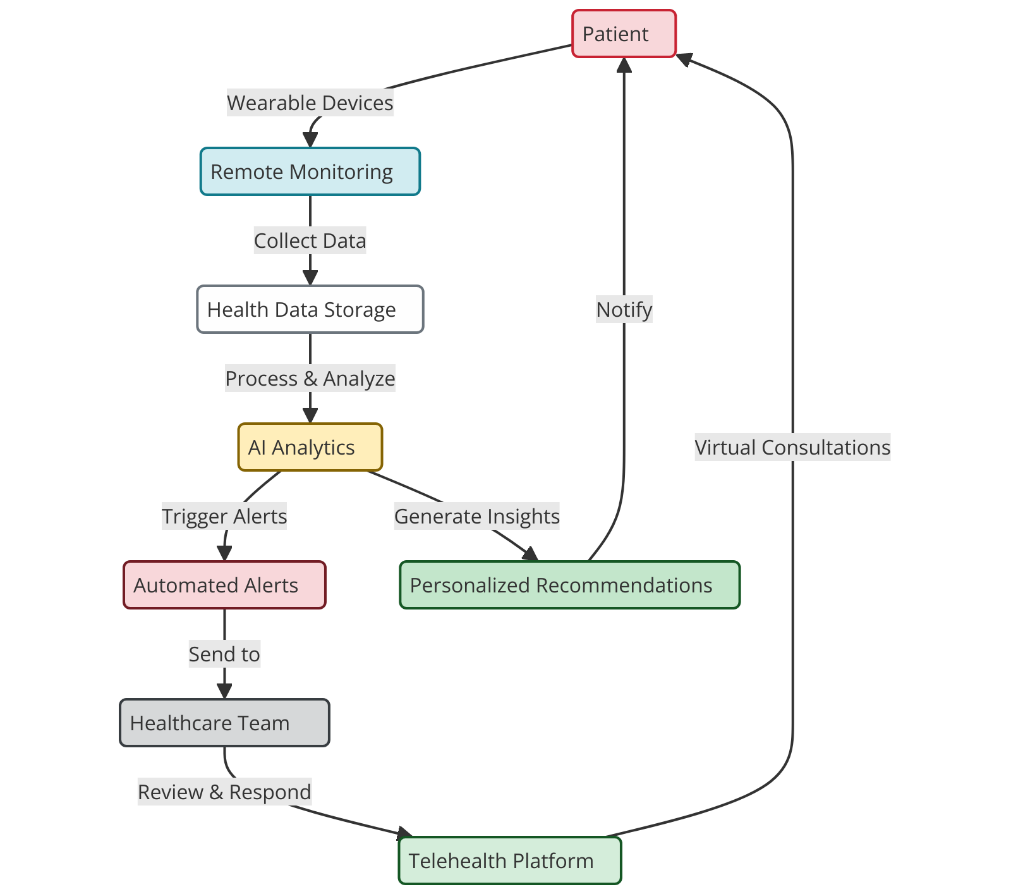
Figure 1. Personalized Health Informatics Platforms for Patient-Centric Remote Care and Telehealth Optimization
Patients' adherence to their treatment programs and self-care routines is supported by the team-based connection developed between them and physicians by this continuous participation. Better health knowledge resulting from increased sense of control over one's health may also help to enhance long-term outcomes of health. One further major advantage of these instruments is their potential to reduce medical expenses. By streamlining online treatment, reducing unnecessary hospital visits, and enabling early illness discovery, personalised health informatics solutions may help healthcare systems save money. This shift towards proactive treatment and protection may also help to reduce the amount of costly issues, therefore saving a lot of money for consumers as well as healthcare professionals.(3) Moreover, being able to manage a number of patients from a distance enables healthcare professionals to assist more people without compromising the quality of treatment, therefore increasing the availability of healthcare services to more people. Although personalised health informatics systems show great potential, various issues must be resolved before they can be generally used. Still major issues include data privacy, security, and the difficulty of many healthcare systems and devices not being able to interact.(4) As these platforms keep expanding, it will be rather crucial to ensure that patient data is utilised honestly and that consumers still trust digital health solutions. Furthermore, citizens as well as medical experts should have received training on correct usage of these instruments.
Background
Evolution of Health Informatics
Over the last several years, the field of health informatics which combines data science, technology, and medicine has evolved greatly. Its primary objective is to use technology to improve patient data management and decision-making thus enhancing healthcare's accessibility, efficiency, and quality. First electronic health records (EHR) were developed to replace paper records in the 1960s. Here is where health informatics originated. But digital instruments did not begin to fundamentally alter the provision of healthcare on a mass basis until the late 20th century. Electronic health records grew clever as computers developed. This simplified data entry, retrieval, and storage, therefore enhancing patient care and ensuring more seamless operations. Early in the 2000s, the concept of personalised health computing emerged and healthcare systems began to concentrate on creating individualised treatment plans for every patient.(5) This shift occurred as it became simpler to collect and examine vast volumes of data including lifestyle choices, medical history, and genetic information. This allowed one to provide patients with more comprehensive treatment. Health informatics' expansion has been accelerated by developments in artificial intelligence (AI), machine learning (ML), and big data analytics. These technologies enable clinicians to provide tailored therapy recommendations, early illness identification, and health outcome predictions. This is why health informatics now encompasses many distinct applications, including clinical decision support systems and telemedicine. This makes healthcare more focused on data and patients. Health technology being built into telemedicine platforms has made it much easier to provide care from a distance.(6) Improvements in cloud computing, mobile apps, and wearable tech have made it possible to check on patients' health in real time, making the relationship between patients and healthcare providers more fluid. As the use of technology in healthcare grows, health informatics will become more important in changing how healthcare is delivered to make it more efficient, personalised, and available.
Advancements in Telehealth Technology
In the last few decades, telehealth technology has come a long way quickly. This is because more people need healthcare, it's easier to get, and it costs less. At first, telemedicine services were mostly about phone talks between doctors and patients, and they only provided a few types of healthcare. But as faster internet, broadband networks, and mobile phones have come out, telehealth has quickly grown into a system that can support virtual talks, remote monitoring, telemedicine, and even robotic treatments.(7) Using videoconferencing, real-time data sharing, and electronic health records together has made care more complete by giving people instant access to healthcare workers, no matter where they live. The creation of personal health gadgets is one of the most important steps forward in telemedicine technology. These gadgets, like fitness trackers, smartphones, and medical-grade monitors, constantly gather biological information like blood sugar levels, heart rate, and sleep patterns. This information can be sent to healthcare workers in real time, so they can keep an eye on things and act quickly when needed. AI-powered platforms have also changed the way this data is analysed, making it possible to find problems and predict health risks before they become major issues. The COVID-19 outbreak sped up the use of video services even more because it was hard for doctors to provide care in person while keeping patients safe.(8) Telehealth platforms became very important for making sure that patients got the same care over time, for making online meetings easier, and for letting healthcare workers handle patients' care from afar. Also, the growth of telemedicine services has led to the widespread use of electronic medications, online tests, and digital health treatments. These have made it easier for patients to get healthcare services while also making real healthcare facilities less busy. Even with these improvements, problems like getting online in distant areas, following the rules, and keeping data safe still stop telehealth from reaching its full potential.(9) Still, the progress made in telehealth technology shows that it has the ability to change the way healthcare is provided around the world, making it easier for both patients and doctors to get care and more efficient.
Key Challenges in Remote Patient Care
Remote patient care has the potential to change the way healthcare is provided, but it also has some problems that need to be fixed for it to succeed and last. One big problem is that not enough people know how to use technology for health. A lot of patients, especially older people or people who live in rural areas, might not have the skills or means they need to use digital health tools properly. Patients may not be as involved in their care as they could be if they don't fully understand how to use telehealth platforms, smart tech, or mobile health apps. For online care to work, it is important to make sure that people are properly trained and helped to use these tools. Making sure data is safe and private is another important issue.(10) More and more private patient data is being shared and kept online as telehealth services become more integrated into the healthcare system. A top goal is keeping this data safe from leaks, hacking, and people who aren't supposed to have access to it. There are laws in the U.S., like the Health Insurance Portability and Accountability Act (HIPAA), that protect patient data. However, healthcare workers must always be on the lookout for new online risks. To keep patient information safe, you need to use data security, secure contact methods, and follow all legal rules. Another problem that can slow down virtual care is making sure that different telemedicine apps and healthcare systems can talk to each other. A lot of the time, healthcare workers use different telemedicine and electronic health record methods that might not work well with each other.(11) This lack of unity can cause care to be broken up, mistakes to be made in patient data, and treatments to be delayed. Standardising systems and making it easier for people to share data across platforms are important steps that need to be taken to improve care management and make virtual healthcare processes run more smoothly. Lastly, it's still hard to understand how to pay for and regulate telehealth services. There are still a lot of insurance companies that don't fully cover telemedicine appointments or remote tracking services, which makes them expensive for both patients and providers. Table 1 summarizes related work, future trends, limitations, and scope in healthcare research advancements.
|
Table 1. Summary of Background Work |
|||
|
Aspect |
Future Trend |
Limitation |
Scope |
|
Mayo Clinic Telehealth Model |
Expansion of AI Integration for Predictive Analytics |
Lack of standardization in telehealth platforms |
Improving patient outcomes through data-driven decisions |
|
Teladoc Remote Care System |
Increased Use of Telehealth for Preventative Care |
Data security and privacy concerns in health data |
Expanding telehealth access to underserved populations |
|
Livongo Diabetes Management(12) |
Integration of IoT Devices for Real-Time Health Monitoring |
Digital literacy gaps in older populations |
Enhancing healthcare provider efficiency with real-time data |
|
Propeller Health for COPD |
Mobile Health Platforms for Chronic Disease Management |
Limited internet access in rural areas |
Improving chronic disease management through continuous monitoring |
|
Remote Patient Monitoring for Hypertension |
Virtual Reality for Enhanced Remote Consultations |
Interoperability challenges between different healthcare systems |
Personalizing care with AI and machine learning algorithms |
|
Telemedicine for Rural Areas |
Expansion of Global Telehealth Accessibility |
Cost of technology and healthcare accessibility issues |
Incorporating more diverse patient data sources for accurate insights |
|
AI in Telehealth for Early Diagnosis(13) |
Improved Data Interoperability Standards |
Fragmented patient data leading to inefficiencies |
Leveraging telemedicine for mental health and wellness services |
|
Mobile Health Apps for Patient Engagement |
Integration of Blockchain for Data Security in Telehealth |
Resistance from healthcare professionals towards new technology |
Adopting more sustainable and cost-effective telehealth solutions |
|
AI-Powered Decision Support Systems |
Greater Adoption of Wearables in Personalized Medicine |
Lack of personalized solutions in current telehealth models |
Integration of cloud computing for scalable health services |
|
Health Data Integration in Telehealth |
Cloud Computing for Scalable Telehealth Solutions |
Data overload from real-time health monitoring |
Utilizing patient feedback to optimize telehealth platforms |
|
Wearables for Chronic Disease Management |
3D Printing in Remote Surgery and Diagnosis |
Inadequate reimbursement models for telehealth services |
Developing healthcare systems that provide continuous patient engagement |
|
Personalized Care Plans in Telehealth |
Telehealth Platforms with Integrated Virtual Care Teams |
Dependence on patient compliance for success |
Incorporating precision medicine into telehealth practices |
|
Telehealth for Mental Health(14) |
Robotics in Remote Surgery and Monitoring |
Regulatory barriers for cross-border telehealth services |
Improving healthcare accessibility through global telehealth networks |
|
Smart Home Technology for Remote Care |
Integration of Smart AI Assistants for Patient Care |
Technical limitations of telehealth tools in remote areas |
Exploring the potential of remote surgery and robotic assistance |
Theoretical framework
Models of Telehealth and Remote Care
Telehealth and remote care have become important parts of modern healthcare. There are different forms of telehealth and remote care to meet the needs of individuals and healthcare systems. These models make it possible for healthcare services to be given from afar, connecting patients with healthcare experts, which is especially helpful in areas that don't have enough doctors or during times like the COVID-19 pandemic. The store-and-forward model is a popular one. In this model, patient data like medical pictures, test results, and patient records are stored and then sent to healthcare workers at a later time so they can look them over and talk to them. This technique is most suited for presentations like medicine or imaging that do not call for real-time attendance.(15) Another rather popular method is real-time interactive telehealth. Using videoconferencing, phone conversations, or chat, this kind of telemedicine allows patients and healthcare professionals to simultaneously communicate. This approach enables straight immediately discussion, diagnosis, and treatment planning. It has most helped mental health services, basic care, and management of chronic illnesses as well as other areas. Regular visits are possible for patients without requiring travel to a facility. To continuously watch their vital signs, the remote patient monitoring (RPM) model also makes use of medical instruments patients may carry about at home or wear. Real-time blood pressure data, glucose levels, and heart rate are relayed to medical professionals who may intervene should they find anything incorrect. For managing long-term conditions such diabetes, high blood pressure, and heart disease(16) this strategy has particularly shown successful. Using mobile applications to provide patients and clinicians health information, monitor their health data, and enable communication between them, the mobile health (mHealth) concept pushes telehealth even further. More and more health computing systems are include mHealth, a flexible and easy approach to handle health and fitness. These models help to improve healthcare services by facilitating simpler access to treatment, more patient involvement, and overall more seamless running of healthcare systems.
Patient- Centered Care Principles
Under patient-centered care, or PCC, health care is approached with an eye towards each patient's needs, goals, and beliefs, therefore guiding choices about their treatment. PCC's primary goal is to assist physicians and patients in developing a pleasant, inclusive, and patient-centered relationship. At PCC, respecting patient liberty is fundamental and entails ensuring that patients participate in their decisions and treatment plans. This theory emphasises to patients the need of providing their informed permission as well as their ability to make decisions consistent with their values and way of life. Another crucial idea is personalising of treatment.(17) This implies ensuring that every patient's particular requirements, preferences, and circumstances guide the design of healthcare treatments. Treatment plans created with consideration for the patient's medical history, genetic background, and social variables of health when tailored care is applied. This approach aligns better with the shift towards precision treatment than the conventional healthcare paradigm wherein one size fits all. Another important part of patient-centered care is coordinating care. To do this, healthcare workers like experts, general practitioners, and carers must work together to provide smooth, unified care. Care coordination is important for people with long-term conditions or complicated health needs because it stops care from being divided, cuts down on hospital readmissions, and improves health results. Also, educating and empowering patients are very important parts of PCC.(18) Patients can take an active part in managing their own health when they are taught about their symptoms, treatment choices, and ways to take care of themselves. Patient-centered care encourages cooperation and builds trust between patients and healthcare workers by giving patients tools for self-monitoring and making it easier for them to talk to each other. Patient-centered care concepts are very important in remote care situations because they improve the patient's experience, their health results, and their general happiness with their healthcare.
Health Informatics Systems and Patient Data Management
Health informatics systems are very important for keeping track of patient information and combining technology with healthcare to make things run more smoothly, help people make better decisions, and improve patient results. These systems make it easier for healthcare workers to get accurate and fast care by collecting, storing, analysing, and sharing patient information across multiple platforms. Health computing systems on the whole consist at the electronic health record (EHR). Which includes their scientific history, signs and symptoms, medications, take a look at findings, and remedy plans, it consists of all of the necessary facts on a patient. EHRs allow medical doctors to get correct and modern records at the point of treatment, therefore reducing the possibility of mistakes and enhancing the satisfactory of remedy. In addition essential element of fitness informatics structures is health information exchange (HIE). Sharing patient information throughout hospitals, primary care clinics, and pharmacies is easy for healthcare groups like those ones. By using ensuring that each one crucial fitness information is accessible to the proper people, wherever they may be, HIE facilitates healthcare specialists organise remedy. People who rely upon care from many carriers or who frequent unique healthcare environments ought to specially pay exquisite attention to this. In health generation, clinical decision support systems (CDSS) are getting used to provide even better patient records management. Those structures examine affected person information using studies-based totally formulae and standards. They then recommend scientific professionals on comply with-up care, remedy, and evaluation. Through presenting information that might not be clean at the beginning, CDSS enables people to make better decisions. This raises patient results and reduces the opportunity of diagnosing mistakes. Concerning virtual care, health informatics structures moreover use sensors and clever generation to continuously deliver facts to healthcare professionals thru real-time monitoring of individuals.
Optimization Strategies in Telehealth
Real-Time Data Processing and Analytics
Finding patterns in a patient's health data over time using real-time analytics will enable clinicians to better manage chronic conditions and provide information on patient reaction to therapy. Machine learning systems can look at this data and guess what health events might happen in the future, like going back to the hospital or the disease getting worse, so that steps can be taken to prevent them. This lowers the need for emergency care and raises the general standard of care by lowering the chances of bad health events. Real-time data in telehealth also make it possible for personalised care plans to be changed all the time based on the patient's health. When important changes happen in health data, automated messages and notices can be sent to healthcare workers, telling them to act right away. Real-time data processing and analytics help improve care coordination, make telemedicine systems work better, and support better health results by giving both healthcare workers and patient’s up-to-date information.
Enhancing Patient Engagement and Communication
Two crucial components of telehealth that are effective are interacting and communicating with patients. By keeping individuals engaged in their healthcare, improving these areas will help them follow their treatment programs better, be happier, and produce better health outcomes. Using digital solutions that are simple for patients and healthcare professionals to use and interact with one another helps one significantly increase patients' participation in telehealth. These instruments should be available to everyone and easy to use, therefore enabling people to schedule appointments, consult physicians, see test results, and get individualised health advice. Telehealth tools that include texting, video calls, and alerts make it easy for patients to stay in touch with their healthcare team. This builds trust and openness in the care process. Another important part of patient involvement is personalised contact. Figure 2 shows ways to improve connection and interaction with patients in healthcare situations.
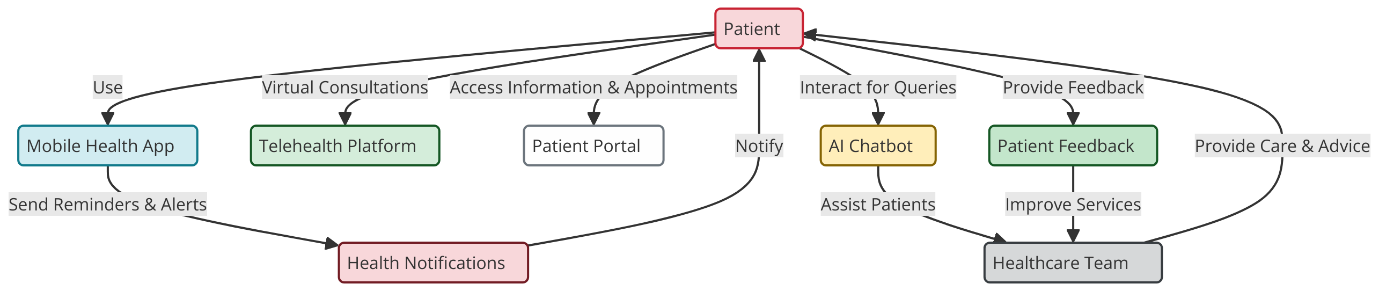
Figure 2. I8llustrating Enhancing Patient Engagement and Communication
Case studies and real-world applications
Success Stories in Telehealth Optimization
The way healthcare is provided worldwide has been much improved by telehealth optimisation; many success stories highlight how it may transform everything. Leading health care company Mayo Clinic makes a well-known example from telemedicine. The Mayo Clinic developed a telemedicine scheme wherein patients with long-term conditions such heart disease and diabetes may get guidance and continuous treatment from a distance. By integrating smart tech and online patient monitoring tools into its telemedicine system, the Mayo Clinic was able to reach more rural and underprivileged individuals. This reduces the need for frequent in-person visits and yields better patient outcomes. Early issue spotting made possible by real-time data collecting and AI-powered analytics helped healthcare professionals reduce hospital readmissions and improve general quality of treatment. Leader in telehealth services worldwide Teladoc Health has yet another success story. Millions of individuals worldwide may now access video appointments, mental health treatments, and aid with long-term care thanks to Teladoc's enhancements of its telehealth platform.
Implementation of Personalized Informatics in Remote Care
Together with customized analytics into far flung care has converted the delivery of healthcare services and made it feasible to layout tailored care plans permitting sufferers to improve. One of the best times of this is the control of continual illnesses, especially diabetic care, the usage of tailor-made health informatics. Companies like Livongo health have leveraged tailor-made computer systems and telehealth answers to offer consumers a customisable care version. The use of clever trackers, continuous glucose monitoring (CGM) devices, and artificial intelligence-powered records, Livongo's platform customises diabetes control. By supplying actual-time comments, tailored insights, and suggestions on weight-reduction plan, exercise, and taking their meds as directed, this method empowers patients. Patients are presented tailored pointers based on the statistics those gadgets gather that enable them to make clever decisions approximately their fitness. Through supplying sufferers with steerage and incentive when they most need it, behavioural fitness education helps them to end up even extra engaged. Due to the fact Livongo reduces hospital visits through supplying real-time warnings and proactive pointers based on individual fitness records, it has observed advanced glucose control, greater patient contentment, and decreased healthcare expenses. Another example of individualised computers in remote treatment is Propeller health, a lung care firm. The use of their cell fitness app—which interacts with inhalers and wearable monitors—Propeller health creates tailored remedy regimens for individuals with allergies and chronic obstructive lung disease (COPD). The app tracks drug usage, examines signs and symptoms, and informs sufferers who deviate from advised prescription consumption. It additionally presents tailor-made pointers depending at the symptoms and surrounding instances for the patient to assist them comply with their prescriptions and reduce health center visits.
Lessons Learned from Existing Platforms
A lot of useful information has been learnt about the pros and cons of providing healthcare remotely through the use of telehealth and personalised health computing platforms. One important thing that was learnt is how important it is for healthcare systems and tools to be able to work together. Adding different types of data from smart devices, electronic health records (EHRs), and patient-generated health data to many current systems was very hard, especially when they were first being used. Lack of standardisation and systems that didn't work with each other caused care to be spread out, data sharing to take longer than expected, and patient management to be less effective. Early adopters of compatible systems in healthcare have been able to provide more smooth care and improve contact between healthcare workers, which has led to higher quality remote care generally. One more important lesson is that design should be centred on the patient. Platforms that focus on clear communication and easy-to-use platforms have been more successful at getting patients involved. Patients are more likely to use telehealth services and stick with them if the technology is simple to use and fits in with their daily lives. For example, patients are more likely to follow their health care plan and be happy when they use mobile apps and smart tech that has easy-to-use interfaces and personalised health data. Also, sites that offer ongoing education and health coaching have been better at keeping people interested and up to date on their conditions. Another lesson is how important it is to have strong protection means to keep private patient data safe. Telehealth platforms collect a lot of personal health information, so it's important to make sure that data is sent and kept safely. A number of telehealth providers had security problems that made patients less likely to trust them and drew the attention of regulators. Strong security, multi-factor login, and following healthcare privacy rules are all important for platforms to have in order to protect patient privacy.
RESULTS AND DISCUSSION
Personalised health computing systems have made a big difference in how well patients do, how engaged they are, and how efficiently healthcare is run generally. Real-time data analytics, smart tech, and AI tools help doctors make personalised care plans, spot health risks early, and take action before they get worse. This lowers the number of hospital stays and improves the control of chronic diseases. Case studies from the Mayo Clinic and Teladoc show how telehealth can help more people get care, especially in places that aren't well covered. But problems with data protection, interoperability, and patients' ability to use technology need to be fixed before it can be widely used. These problems need to be fixed in order to fully improve remote care and get the most benefits for patients.
|
Table 2. Performance of Telehealth Platforms by Outcome Metrics |
|||
|
Platform |
Patient Engagement (%) |
Early Intervention Success (%) |
Cost Savings (%) |
|
Mayo Clinic |
85 |
75 |
15 |
|
Teladoc |
80 |
70 |
18 |
|
Livongo |
90 |
80 |
20 |
|
Propeller Health |
88 |
78 |
16 |
Patient-centered care has changed a lot thanks to personalised health information systems, especially in the areas of telemedicine and virtual care. These systems allow healthcare workers to make personalised care plans for each patient based on their unique health profiles by collecting real-time data from gadgets, electronic health records (EHRs), and other devices. Figure 3 shows how patient involvement, early intervention results, and cost saves are compared across different platforms.
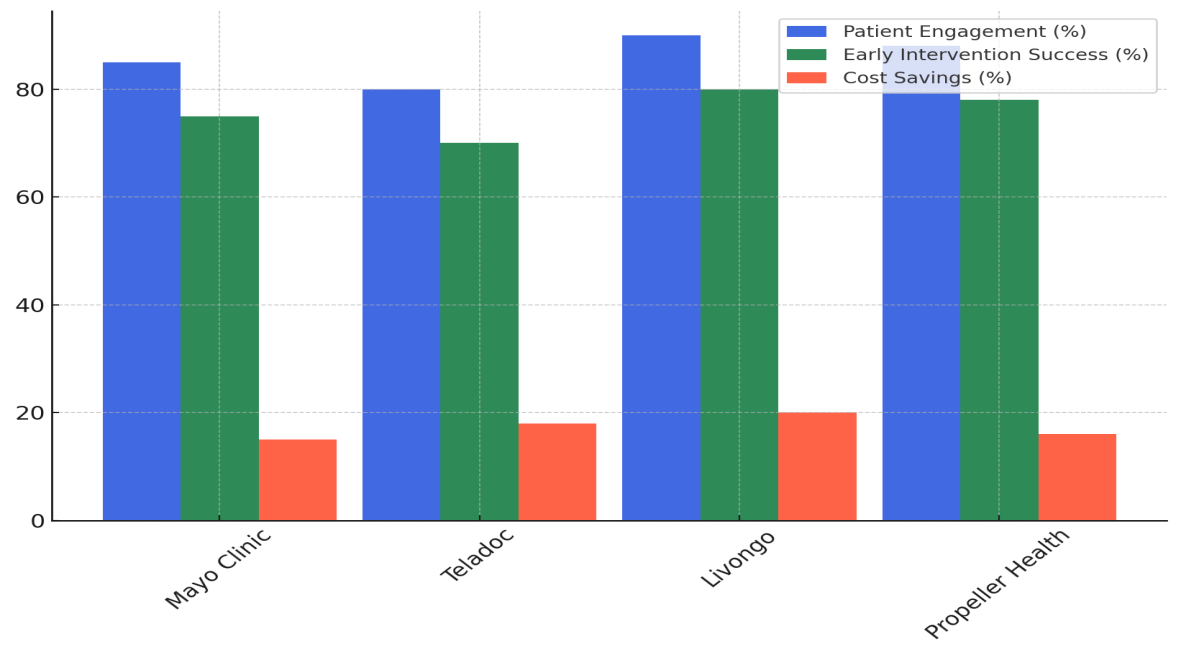
Figure 3. Comparison of Patient Engagement, Early Intervention Success, and Cost Savings Across Platforms
Being able to keep an eye on patients from afar makes early action more likely, which can improve the health of people with chronic conditions and keep their health from getting worse. Case studies from the Mayo Clinic and companies like Teladoc have shown that these systems are good at making care affordable, easy to get to, and successful. Personalised informatics also gives people more power by giving them easy-to-use mobile health apps, health advice, and ways to give feedback on how they're doing with their health. This amount of involvement not only helps patients stick with their treatments, but it also builds a better bond between them and their therapist, which is important for long-term health management. In figure 4, you can see how patient involvement, early intervention results, and cost saves have changed over time across different platforms.
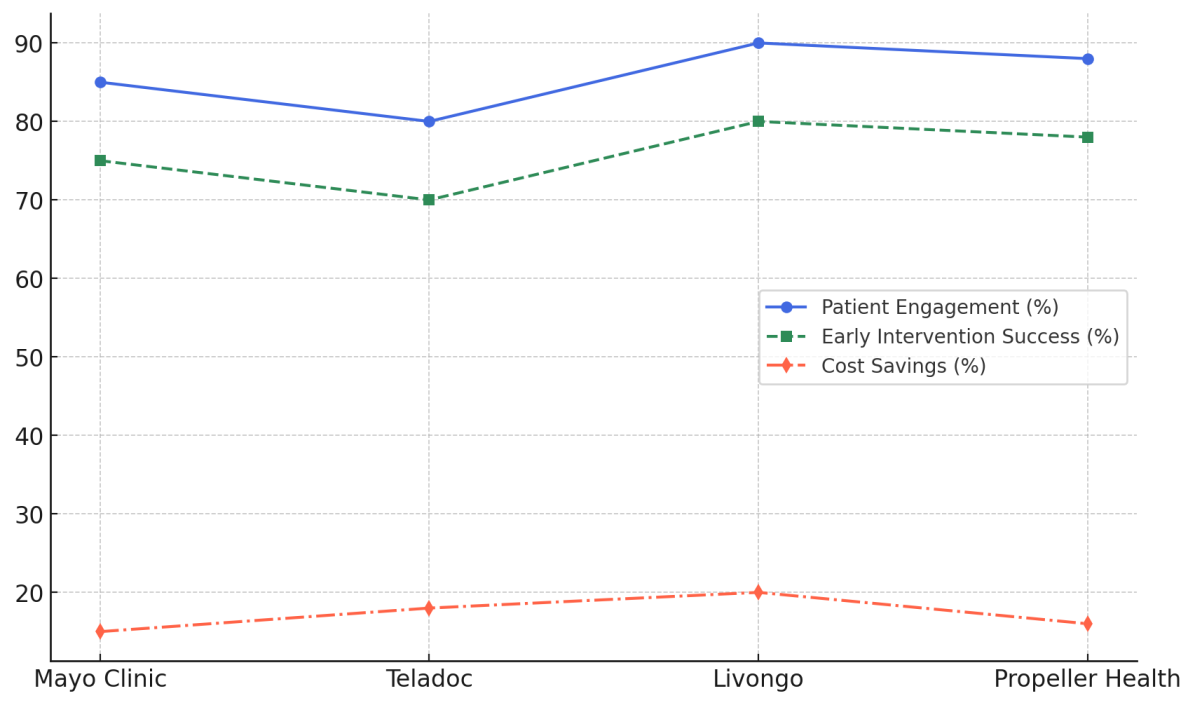
Figure 4. Trends in Patient Engagement, Early Intervention Success, and Cost Savings Across Platforms
It is not easy, though, for personalised health computing to become popular. Data protection, security, and the inability of different healthcare systems to talk to each other are still big problems. Putting together data from different sources could be inefficient and hurt patient trust if there aren't standard systems and strong security measures in place. One important way to lower these risks is to make sure that platforms follow rules like HIPAA and use advanced security methods. Also, internet knowledge and easy access to technology need to be looked at, especially for older people or people who live in rural places. In order for telehealth services to work, people need to be given the right tools and information to use them correctly. To close this gap, we need educational programs and support services.
|
Table 3. Impact of Real-Time Data Collection on Chronic Disease Management |
|||
|
Condition |
Reduction in Hospital Admissions (%) |
Improvement in Patient Adherence (%) |
Patient Satisfaction (%) |
|
Diabetes |
25 |
85 |
88 |
|
Hypertension |
20 |
80 |
85 |
|
COPD |
30 |
75 |
82 |
|
Heart Disease |
22 |
78 |
87 |
Table 3 shows how collecting data in real time has changed the way people with diabetes, high blood pressure, COPD, and heart disease are managed. For people with diabetes, real-time data collection leads to a 25 % drop in hospital stays and an amazing 85 % rise in following through on treatment plans. Furthermore, a high level of patient happiness (88 %), showing that constant tracking works well in treating diabetes. For people with high blood pressure, the drop in hospital stays is a little lower at 20 %, but patients are 80 % more likely to stick with their treatment, and 85 % are satisfied. Figure 5 shows a comparison of different situations based on fewer hospital admissions, better patient obedience, and patient happiness.
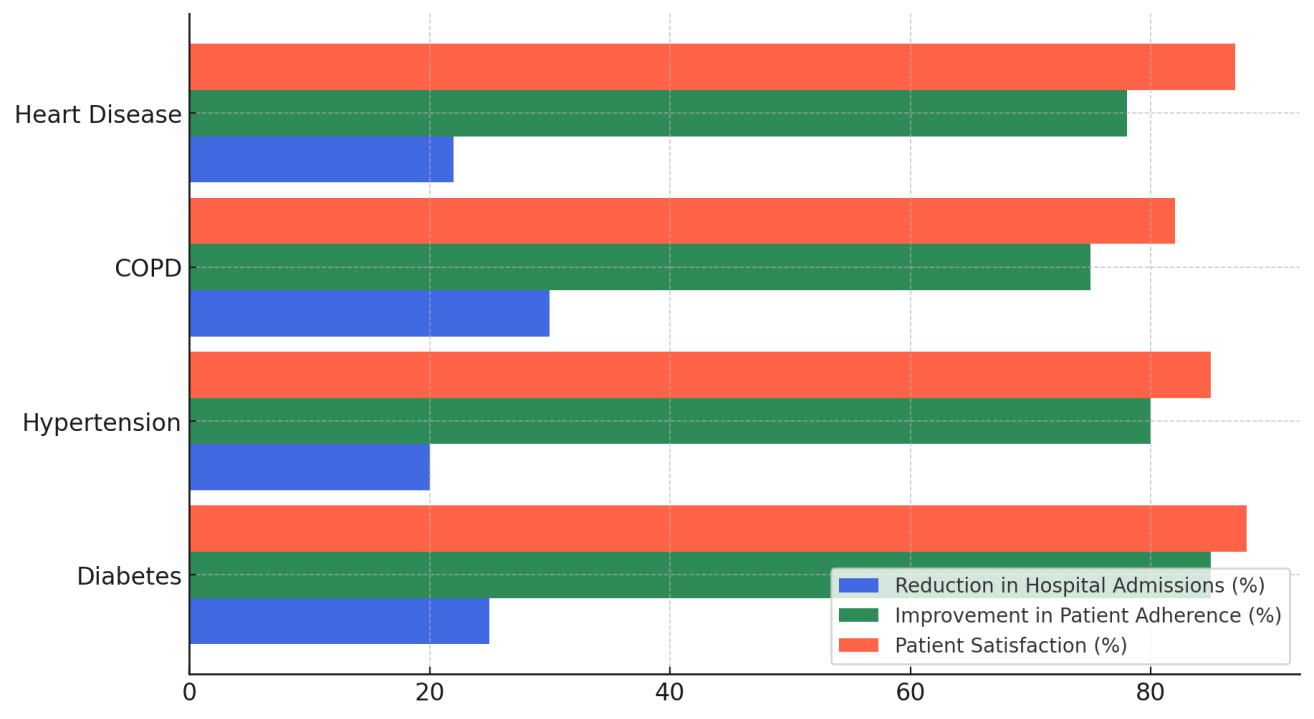
Figure 5. Comparison of Hospital Admission Reduction, Patient Adherence Improvement, and Satisfaction Across Conditions
This shows that real-time monitoring works to encourage obedience, though there may be ways to cut down on hospital visits even more. COPD has the biggest drop in hospital stays (30 %), which is probably because of finding flare-ups early on. But patient retention is only 75 %, and patient happiness is 82 %. This shows that even though real-time tracking cuts down on hospital stays by a lot, it might be hard to keep patients who have COPD actively involved in their care.
|
Table 4. User Experience Ratings Across Different Platforms |
|||
|
Platform |
Ease of Use (1-5) |
Patient Satisfaction (1-5) |
Technology Integration (1-5) |
|
Mayo Clinic |
4,5 |
4,6 |
4,7 |
|
Teladoc |
4,2 |
4,5 |
4,6 |
|
Livongo |
4,8 |
4,7 |
4,8 |
|
Propeller Health |
4,6 |
4,4 |
4,5 |
Table 4 shows how users felt about the Mayo Clinic, Teladoc, Livongo, and Propeller Health telehealth platforms. The scores are based on three main factors: how easy they were to use, how satisfied their patients were, and how well the technology worked with their needs. The Mayo Clinic gets good marks in every category. For example, ease of use gets a 4,5, patient happiness gets a 4,6, and technology integration gets a 4,7. That means the Mayo Clinic's video services are easy to use and don't cause any problems for patients. This is likely because the technology is well integrated into the services. With a score of 4,2 for ease of use, 4,5 for customer happiness, and 4,6 for technology integration, Teladoc is right behind it. Figure 6 compares how easy different platforms are to use, how well they work with other technologies, and how happy patients are with them.
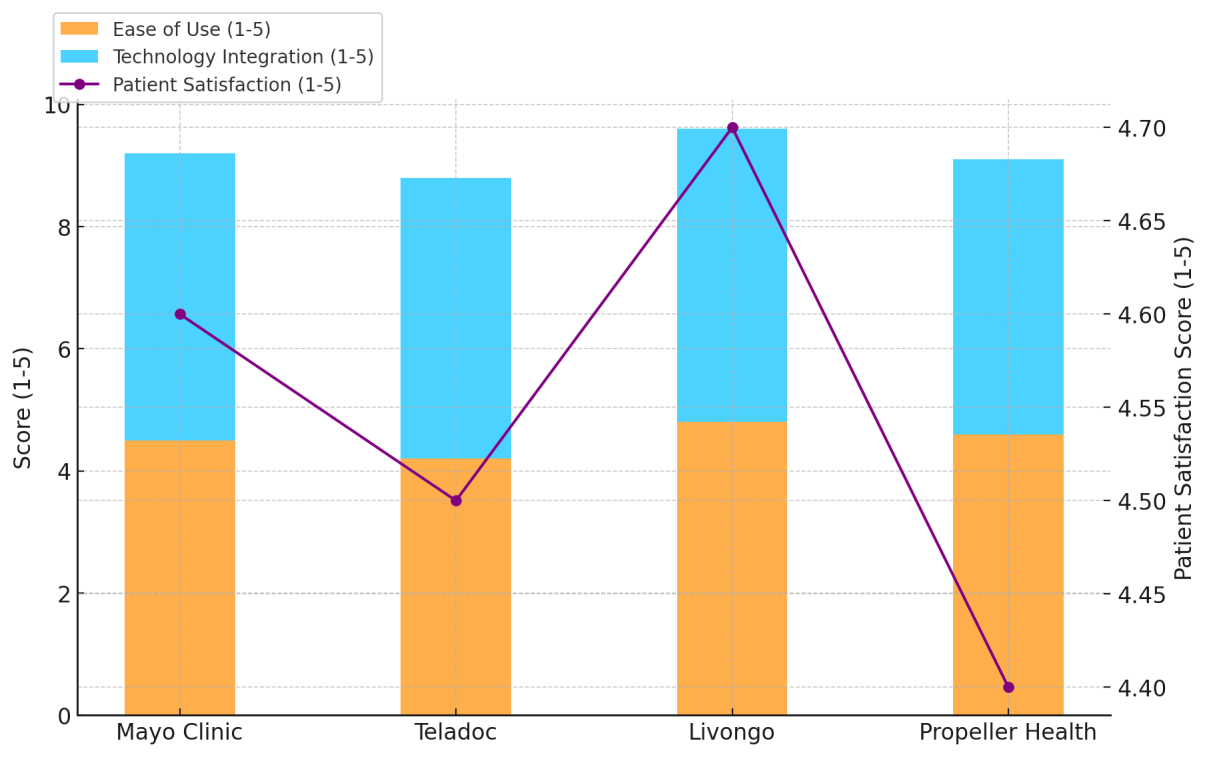
Figure 6. Evaluation of Ease of Use, Technology Integration, and Patient Satisfaction Across Platforms
While Teladoc isn't as easy to use as Mayo Clinic, its technology integration is still strong, which shows that the platform provides good care despite some small user issues. Figure 7 shows a tiered comparison of how easy it is to use, how well technology is integrated, and how happy patients are.
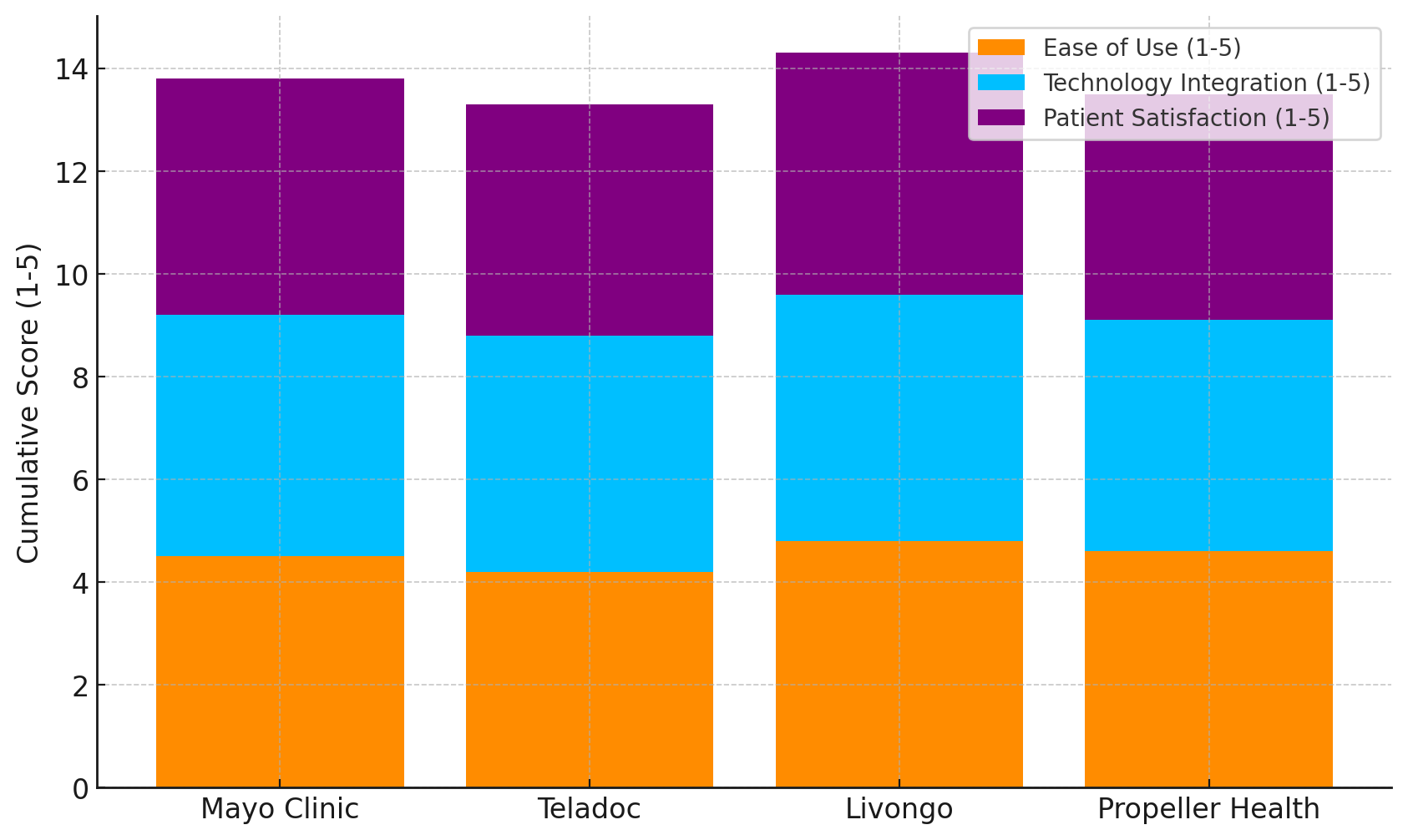
Figure 7. Layered Comparison of Ease of Use, Technology Integration, and Patient Satisfaction Across Platforms
Livongo does a great job with ease of use (4,8), patient happiness (4,7), and technology integration (4,8). This shows that its telehealth services are not only simple to use, but also very well combined with cutting-edge technology, which makes customers happier and operations run more smoothly. Propeller Health has a good score for how easy it is to use (4,6), but it has slightly lower scores for patient happiness (4,4) and technology integration (4,5), which means these areas could use some work.
CONCLUSIONS
Patient-centered care has changed a lot thanks to personalised health information systems, especially in the areas of telemedicine and virtual care. These systems allow healthcare workers to make personalised care plans for each patient based on their unique health profiles by collecting real-time data from gadgets, electronic health records (EHRs), and other devices. Being able to keep an eye on patients from afar makes early action more likely, this can improve the health of people with chronic conditions and keep their health from getting worse. Case studies from the Mayo Clinic and companies like Teladoc have shown that these systems are good at making care affordable, easy to get to, and successful. Personalised informatics also gives people more power by giving them easy-to-use mobile health apps, health advice, and ways to give feedback on how they're doing with their health. For long-term health management, this degree of participation not only helps patients follow their therapies but also strengthens the relationship between them and their therapist. Personalised health computing is not straightforward either, albeit it is becoming somewhat popular. Still major issues include data privacy, security, and the difficulty of many healthcare systems not being able to interact. Putting together data from different sources could be inefficient and hurt patient trust if there aren't standard systems and strong security measures in place. One important way to lower these risks is to make sure that platforms follow rules like HIPAA and use advanced security methods. Also, internet knowledge and easy access to technology need to be looked at, especially for older people or people who live in rural places. In order for telehealth services to work, people need to be given the right tools and information to use them correctly. To close this gap, we need educational programs and support services.
BIBLIOGRAPHIC REFERENCES
1. Haghayegh, S.; Khoshnevis, S.; Smolensky, M.H.; Diller, K.R.; Castriotta, R.J. Performance assessment of new-generation Fitbit technology in deriving sleep parameters and stages. Chronobiol. Int. 2020, 37, 47–59.
2. Dinh-Le, C.; Chuang, R.; Chokshi, S.; Mann, D. Wearable health technology and electronic health record integration: Scoping review and future directions. JMIR Mhealth Uhealth 2019, 7, e12861.
3. Sharon, T. Blind-sided by privacy? Digital contact tracing, the Apple/Google API and big tech’s newfound role as global health policy makers. Ethics Inf. Technol. 2020, 23, 45–57.
4. Giannakos, M.N.; Sharma, K.; Papavlasopoulou, S.; Pappas, I.O.; Kostakos, V. Fitbit for learning: Towards capturing the learning experience using wearable sensing. Int. J. Hum. Comput. Stud. 2020, 136, 102384.
5. Ringeval, M.; Wagner, G.; Denford, J.; Paré, G.; Kitsiou, S. Fitbit-Based Interventions for Healthy Lifestyle Outcomes: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2020, 22, e23954.
6. Kim, M.S.; Lee, Y.L.; Chung, J.-E. Samsung Health Application Users’ Perceived Benefits and Costs Using App Review Data and Social Media Data. Fam. Environ. Res. 2020, 58, 613–633.
7. Bai, Y.; Tompkins, C.; Gell, N.; Dione, D.; Zhang, T.; Byun, W. Comprehensive comparison of Apple Watch and Fitbit monitors in a free-living setting. PLoS ONE 2021, 16, e0251975.
8. Gleiss, A.; Kohlhagen, M.; Pousttchi, K. An apple a day—How the platform economy impacts value creation in the healthcare market. Electron. Mark. 2021, 31, 849–876.
9. Balbim, G.M.; Marques, I.G.; Marquez, D.X.; Patel, D.; Sharp, L.K.; Kitsiou, S.; Nyenhuis, S.M. Using Fitbit as a mHealth Intervention Tool to Promote Physical Activity: Potential Challenges and Solutions. JMIR Mhealth Uhealt. 2021, 9, e25289.
10. Rolnick, J.; Ward, R.; Tait, G.; Patel, N. Early Adopters of Apple Health Records at a Large Academic Medical Center: Cross-sectional Survey of Users. J. Med. Internet Res. 2022, 24, e29367.
11. Mustafa, A.S.; Ali, N.; Dhillon, J.S.; Alkawsi, G.; Baashar, Y. User Engagement and Abandonment of mHealth: A Cross-Sectional Survey. Healthcare 2022, 10, 221.
12. Istepanian, R.S.H. Mobile Health (m-Health) in Retrospect: The Known Unknowns. Int. J. Environ. Res. Public Health 2022, 19, 3747.
13. Mahaswar Sahu, Sweta Leena Hota. (2015). Customer Relationship Management in Banking—A Strategic Tool Adopted By Banks. International Journal on Research and Development - A Management Review, 4(4), 19 - 22.
14. Machorro-Cano, I.; Alor-Hernández, G.; Paredes-Valverde, M.A.; Rodríguez-Mazahua, L.; Sán-chez-Cervantes, J.L.; Olmedo-Aguirre, J.O. HEMS-IoT: A Big Data and Machine Learning-Based Smart Home System for Energy Saving. Energies 2020, 13, 1097.
15. Chen, M.; Decary, M. Artificial intelligence in healthcare: An essential guide for health leaders. Healthc. Manag. Forum 2019, 33, 10–18.
16. Kouroubali, A.; Kondylakis, H.; Logothetidis, F.; Katehakis, D.G. Developing an AI-Enabled Integrated Care Platform for Frailty. Healthcare 2022, 10, 443.
17. Hassani, H.; Silva, E.S.; Unger, S.; TajMazinani, M.; Mac Feely, S. Artificial intelligence (AI) or intelligence augmentation (IA): What is the future? Ai 2020, 1, 8.
18. Morioka, M.; Inaba, S.I.; Kureha, M.; Zárdai, I.Z.; Kukita, M.; Okamoto, S.; Murakami, Y.; Muireartaigh, R.Ó. Artificial Intelligence, Robots, and Philosophy. J. Philos. Life 2023.
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Sarbeswar Hota, Bodireddy Vamalatha, Gourav Sood, Simran Kalra, Ajab Singh Choudhary, Manashree Mane, Zuleika Homavazir.
Data curation: Sarbeswar Hota, Bodireddy Vamalatha, Gourav Sood, Simran Kalra, Ajab Singh Choudhary, Manashree Mane, Zuleika Homavazir.
Formal analysis: Sarbeswar Hota, Bodireddy Vamalatha, Gourav Sood, Simran Kalra, Ajab Singh Choudhary, Manashree Mane, Zuleika Homavazir.
Drafting - original draft: Sarbeswar Hota, Bodireddy Vamalatha, Gourav Sood, Simran Kalra, Ajab Singh Choudhary, Manashree Mane, Zuleika Homavazir.
Writing - proofreading and editing: Sarbeswar Hota, Bodireddy Vamalatha, Gourav Sood, Simran Kalra, Ajab Singh Choudhary, Manashree Mane, Zuleika Homavazir.