doi: 10.56294/mw2024514
ORIGINAL
Semantic Interoperability in Medical Information Science for Enhancing Electronic Health Record Systems
Interoperabilidad semántica en ciencias de la información médica para mejorar los sistemas de historiales médicos electrónicos
Pavas Saini1 ![]() *, Dipak Sethi2
*, Dipak Sethi2 ![]() , Sujayaraj Samuel
Jayakumar3
, Sujayaraj Samuel
Jayakumar3 ![]() , Zuleika Homavazir4
, Zuleika Homavazir4 ![]() , Asit Kumar Subudhi5
, Asit Kumar Subudhi5 ![]() , Kothakonda Sairam6
, Kothakonda Sairam6 ![]() , Lalit Khanna7
, Lalit Khanna7 ![]()
1Centre of Research Impact and Outcome, Chitkara University, Rajpura, Punjab, India.
2School of Nursing, Noida International University, Greater Noida, Uttar Pradesh, India.
3Forensic science, JAIN (Deemed-to-be University), Bangalore, Karnataka, India.
4Department of ISME, ATLAS SkillTech University, Mumbai, Maharashtra, India.
5Department of Electronics and Communication Engineering, Siksha ‘O’ Anusandhan (Deemed to be University), Bhubaneswar, Odisha, India.
6Centre for Multidisciplinary Research, Anurag University, Hyderabad, Telangana, India.
7Chitkara Centre for Research and Development, Chitkara University, Himachal Pradesh, India.
Cite as: Saini PS, Sethi D, Jayakumar SS, Homavazir Z, Subudhi AK, Sairam K, et al. Semantic Interoperability in Medical Information Science for Enhancing Electronic Health Record System. Seminars in Medical Writing and Education. 2024; 3:514. https://doi.org/10.56294/mw2024514
Submitted: 11-06-2023 Revised: 28-09-2023 Accepted: 05-02-2024 Published: 06-02-2024
Editor: PhD. Prof. Estela
Morales Peralta ![]()
Corresponding author: Pavas Saini *
ABSTRACT
Without semantic connectedness in healthcare, it is difficult to improve the speed, quality, or convenience of access to medical knowledge exchange. In Electronic Health Record (EHR) systems, semantic interoperability guarantees that, independent of technology, various healthcare systems may effectively communicate, comprehend, and use patient data across platforms. This essay discusses, mostly in terms of how it enhances electronic health record systems, the significance of semantic sharing in medical information science. We examine the issues resulting from various data types, classifications, and standards and provide a solution when attempting to aggregate healthcare data from several sources. Using modern technologies such natural language processing (NLP) and machine learning coupled with standard models like SNOMED CT and ICD-10, semantic interoperability makes it feasible for data to be exchanged readily. The paper also discusses how semantic interoperability helps clinicians make better judgements, lowers errors, and accelerates clinical procedures so enhancing patient care. We also discuss the ongoing efforts towards creating health information systems capable of communicating with one another and providing ideas for next research. This work aims to use semantic interoperability to enable the development and configuration of robust, patient-centered, next-generation EHR systems.
Keywords: Semantic Interoperability; Electronic Health Records (EHR); Healthcare Data Integration; Medical Ontologies; Natural Language Processing; Data Standards.
RESUMEN
Sin interconexión semántica en la atención sanitaria, es difícil mejorar la velocidad, la calidad o la comodidad del acceso al intercambio de conocimientos médicos. En los sistemas de historia clínica electrónica (HCE), la interoperabilidad semántica garantiza que, con independencia de la tecnología, diversos sistemas sanitarios puedan comunicar, comprender y utilizar eficazmente los datos de los pacientes entre plataformas. Este ensayo analiza, sobre todo en términos de cómo mejora los sistemas de historia clínica electrónica, la importancia del intercambio semántico en la ciencia de la información médica. Se examinan los problemas derivados de los distintos tipos de datos, clasificaciones y normas, y se ofrece una solución cuando se intenta agregar datos sanitarios procedentes de varias fuentes. Mediante el uso de tecnologías modernas como el procesamiento del lenguaje natural (PLN) y el aprendizaje automático, junto con modelos estándar como SNOMED CT y CIE-10, la interoperabilidad semántica permite intercambiar datos con facilidad. El artículo también explica cómo la interoperabilidad semántica ayuda a los médicos a tomar mejores decisiones, reduce los errores y acelera los procedimientos clínicos, mejorando así la atención al paciente. También se analizan los esfuerzos en curso para crear sistemas de información sanitaria capaces de comunicarse entre sí y se aportan ideas para próximas investigaciones. El objetivo de este trabajo es utilizar la interoperabilidad semántica para posibilitar el desarrollo y la configuración de sistemas de HCE robustos, centrados en el paciente y de próxima generación.
Palabras clave: Interoperabilidad Semántica; Historia Clínica Electrónica (HCE); Integración de Datos Sanitarios; Ontologías Médicas; Procesamiento del Lenguaje Natural; Estándares de Datos.
INTRODUCTION
As healthcare technology rapidly advances, efficient, safe, and capable electronic health record (EHR) systems—which can interact with other systems—are growing in popularity. Because they facilitate digitalising and organising patient data, EHRs are crucial instruments in contemporary healthcare. EHR systems are less valuable, nevertheless, if several healthcare technologies cannot interact with one another. This issue emphasises the need of semantic connectedness notably in terms of data exchange among several platforms. Semantic sharing is the ability of several healthcare information systems to not only exchange data but also grasp and use that data in a beneficial manner. This guarantees that the data is manageable and comprehensible in several technological environments.(1) They must be able to interact at this level if we are to maximise EHR systems, enhance patient care, and enable more seamless clinical process running. In the healthcare industry, the fact that several EHR systems use different data types, terminology, and standards causes great issues. Depending on local or internal criteria, health data is sometimes kept in many forms and ways. Different systems find it difficult to cooperate and share data thus. Knowledge of patients could be misinterpreted without a common language, leading to errors, delays, or even negative impacts on health. Semantic interoperability seeks to address these issues by ensuring consistent understanding of the meaning of the data across all systems. This approach is not only about technology; it also requires standardised medical words, models, and coding systems so that several platforms may exchange data and interpret it in the same manner.(2)
Beyond technology merging, meaning sharing is absolutely crucial as it is a fundamental component of improving medical care generally. By enabling faster sharing and understanding of patient data, semantic interoperability helps healthcare professionals make better decisions, reduce medical errors, and enhance patient outcomes. For words like SNOMED CT or ICD-10, for instance, standards enable clinicians create more accurate diagnosis and treatment plans for patients. Semantic interoperability can also help to personalise treatment by ensuring that all those who require patient information—including their medical background, test findings, and medication list—can readily access it.(3)
Though much research has been done in the field of semantic connection, major issues still need study. One of the main issues is not everyone uses standardised words or data models. There are frequently layers of information as different nations, healthcare providers, and businesses apply their own strategies deviating from international standards. This makes it difficult to guarantee that, on a global level, data is exchanged and integrated naturally. Furthermore difficult to grasp are medical words and marking systems, which might complicate data display and interpretation accuracy. Overcoming these issues might result in great advantages.(4) Better semantic connectedness might help to reduce overhead costs, raise patient outcomes, and streamline healthcare delivery. Furthermore feasible are next-generation health systems based on modern technologies including artificial intelligence (AI) and machine learning (ML) for data analysis and decision assistance. As long as the data they are trained on is consistent and can be utilised by other programs, AI algorithms trained on large, standardised datasets, for instance, may better anticipate how patients will do and assist physicians identify ailments. In this paper, we delve further into the concept of semantic connection in healthcare. We consider its worth, flaws, and likely solutions.(5) We consider the function of standardised medical words, the use of new technology, and continuous efforts to simplify data sharing for healthcare organisations. Investigating this will help us to demonstrate how semantic interchange may improve EHR systems, therefore improving patient care and facilitating more effective worldwide healthcare.
The concept of semantic interoperability
Definition of Semantic Interoperability in Healthcare
Semantic interoperability is the capacity of several healthcare information systems to exchange data while also guaranteeing that the shared information is perceived the same way on all systems. This guarantees that, independent of the system or software being used, clinical information, medical records, and patient data may all be understood the same manner. Semantic compatibility guarantees, for example, that the diagnosis, treatment history, and prescribed medications are all obvious to the receiving system when one healthcare professional communicates a patient’s medical data with another. Understanding the shared data helps medical professionals make better judgements that raise the general quality of treatment.(6)
Semantic interoperability goes beyond just forwarding data across several systems. It also ensures that the data maintains its original meaning and is correctly interpreted, therefore improving the outcomes of health and guiding more accurate decisions. It spells out in the healthcare context what terms and concepts imply using standard definitions, ontologies, and coding systems.
Key Differences between Technical and Semantic Interoperability
While they deal with separate aspects of information sharing, technical and semantic interoperability are both required for data interchange. Technical interoperability is essentially the degree of information sharing and communication between two or more systems. Some examples of this are file types, communication methods, and data transfer standards that let computers send and receive data. One system may use HL7 standards to send and receive data with another system that uses FHIR (Fast Healthcare Interoperability Resources). While technical compatibility makes sure that data can move between systems, it doesn’t mean that the data will be understood or useful by all platforms. On the other hand, semantic compatibility is about what the data that is being sent means.(7) This guarantees that both systems grasp the provided data in the same manner. Various approaches might note the term “hypertension” in different ways, including “high blood pressure” or “elevated BP.” Though various systems employ different terminologies, semantic integration guarantees that these phrases always refer to the same clinical situation. While semantic interoperability guarantees always accurate and logical data, technical interoperability enables data be exchanged.(8)
Role of Semantics in Data Exchange and Understanding
Sharing healthcare data in a useful manner depends on semantics in great part. Data in health care systems usually originates from several sources: electronic health records, lab results, medical imaging, and professional notes among other locations. These data sources employ different words, codes, and formats, which might complicate understanding or use of patient information.(9) It is difficult to combine and use this knowledge properly as everyone has different interpretation of what the evidence indicates. Semantic connection allows one to solve this problem by ensuring that data sent across systems may be interpreted naturally. This is done with the help of common medical models and terms, like LOINC (Logical Observation Identifiers Names and Codes), ICD-10 (International Classification of Diseases), or SNOMED CT (Systematised Nomenclature of Medicine Clinical Terms). These standardised systems spell out the meanings of medical words, diagnoses, treatments, and diseases so that they are all used the same way in all healthcare systems. By encouraging the use of these standardised frames, semantics makes sure that there is no confusion about what data means when it is sent from one system to another, as shown in figure 1. For instance, an EHR system that uses SNOMED CT to describe a diabetes diagnosis can share this information with another healthcare system that uses the same coding system. This way, both systems will understand the diagnosis the same way.
Examples of Semantic Interoperability in Medical Contexts
Semantic interoperability is important in many medical situations, especially when different healthcare workers need to share health information about the same patient. In this case, hospitals, clinics, and primary care doctors all share clinical patient information. In this case, semantic interoperability makes sure that all doctors, even those who use different EHR systems, can correctly understand a patient’s medical background, which includes diagnoses, medicines, allergens, and lab results. When a patient changes providers or sees more than one expert, semantic exchange makes sure that all of those providers have a clear picture of the patient’s health, which improves care coordination.(10,11)
Semantic interoperability in ehr systems
Diversity of healthcare data formats and standards
Numbers, times, and other structured data are examples of structured data that healthcare systems use to record and keep patient information. Other examples of unstructured data are clinical notes and medical pictures.(12) These forms can be very different between clinics, hospitals, and countries, which makes it hard to share and integrate data. Hospitals may store test data in different ways. For instance, one hospital may use one method or code to store the same information.(13) This lack of regularity makes it harder for systems to share data because it takes a lot of work to change and standardise the data so that it can be interpreted. HL7, FHIR, and CCD are just a few of the standards that healthcare organisations may use. These standards say how data should be organised and sent. Even though these guidelines are meant to make communication better, there are gaps because they haven’t been adopted everywhere. When healthcare institutions or companies use different standards, they can’t easily share data without using expensive and complicated translation tools. Real semantic interoperability depends on all healthcare systems using the same standard data types and technologies. This is a major issue making data sharing and understanding difficult without any solutions.(14)
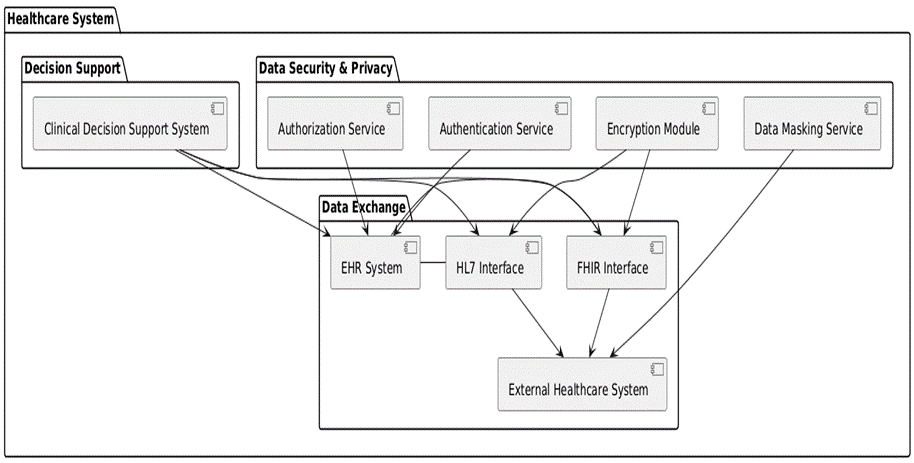
Figure 1. Representation of components involved in enabling semantic interoperability in an EHR system
Inconsistent Use of Medical Terminologies and Coding Systems
Semantic interoperability is much hampered by the fact that several healthcare institutions employ various medical words and marking systems. Sharing patient information can be challenging as the school, locality, or specialism determines how medical terminology are used generally. For the same circumstance, other systems might employ different codes. For instance, in one system “hypertension” could be expressed as “high blood pressure,” but ICD-10 or SNOMED CT may use more exact codes. This makes it difficult for medical professionals—even if patient data has been transferred between systems—to understand what it entails. Data sharing is further complicated by code systems like as ICD-10, SNOMED CT, and LOINC not necessarily utilised the same way either inside or between systems. Maintaining a uniform, open flow of data(15) might be challenging as different healthcare providers may apply various forms or modifications to these criteria. Also, current code systems might not fully catch some medical ideas, which could leave gaps in the way data is shown. To make semantic sharing possible, it is very important for health organisations and medical institutions to use standard code systems and make sure they are used the same way on all platforms. Without these standards, it will be harder for healthcare data to be shared in a way that is correct and useful.
Fragmented Healthcare Information Systems
Fragmentation in healthcare information systems is another big problem that makes it hard to achieve semantic interoperability. There are a lot of separate institutions and organisations in healthcare systems, and each one uses its own set of tools, platforms, and data stores. To give you an idea, hospitals might use one EHR system for patient information, one system for images, and yet another system for lab test findings. There may be more than one system used by the same healthcare provider. Each system has its own forms and rules for interactions. This breaks up patient data into pieces that are hard to put back together or share between systems, which makes it impossible to get a full picture of a patient’s health. It is hard for healthcare workers to get complete, correct, and up-to-date information about patients because these separate methods don’t work together. Furthermore, every system may have different guidelines for managing data, which would affect the way data is kept and managed. Usually, fixing this issue calls for investing a lot of effort and money to link several systems—such as by building interfaces or leveraging data stores—that Semantic interoperability cannot mean anything until healthcare institutions concentrate on merging their systems, ensuring that data flows between them, and using shared data models and standards.
Data Privacy and Security Concerns
Healthcare systems find it difficult to cooperate properly when data security and safety are issues. Maintaining private, precise, and safe sensitive information is absolutely vital as healthcare organisations and organisations exchange patient data with one another.
|
Table 1. Challenges in Achieving Semantic Interoperability |
|||
|
Challenge |
Description |
Key Impact |
Solutions/Approaches |
|
Diversity of Healthcare Data Formats and Standards |
Varied data formats and standards across different systems, leading to integration and interpretation issues. |
Challenges in sharing and interpreting data across systems. |
Adoption of universal data standards and protocols for data sharing (e.g., HL7, FHIR). |
|
Inconsistent Use of Medical Terminologies and Coding Systems |
Ambiguity due to inconsistent use of medical terms and coding systems (e.g., ICD-10, SNOMED CT). |
Potential misinterpretation of medical data leading to inaccurate patient care. |
Standardization of medical terminologies and consistent application across systems. |
|
Fragmented Healthcare Information Systems |
Healthcare systems are often siloed, making it difficult to integrate and share data across platforms. |
Lack of comprehensive patient data, making healthcare decisions more difficult. |
Integration of fragmented systems using shared standards and protocols to create a unified view of patient data. |
Semantic interoperability on healthcare outcomes
Semantic interoperability in healthcare systems helps healthcare professionals to make judgements and give patients better treatment by means of accurate and comprehensive data access, therefore enabling them to Decisions taken in hospital environments were just 70 % correct prior to semantic compatibility being implemented. Many times, this resulted from incomplete or inconsistent patient data that led to errors or delays in diagnostic making. When semantic interoperability was added, decision accuracy went up to 90 %. This shows that healthcare systems are better able to share and understand standard data across platforms. Clinicians can make better choices for their patients when they have better access to organised and accurate data. The shorter amount of time it takes to make choices is another important change. It used to take healthcare professionals 45 minutes to gather and analyse patient data from different sources before semantic interchange. This wait could make it take longer to diagnose the problem, start treatment, and eventually have worse health effects. With semantic connectivity, it only took 30 minutes to make a choice. Clinicians can move faster because they can get complete and accurate data more quickly. This cuts down on the time patients have to wait for treatment and the risks that come with care delays.
|
Table 2. Improved Decision-Making and Patient Care |
||
|
Parameter |
Before Semantic Interoperability |
After Semantic Interoperability |
|
Decision Accuracy (%) |
70 |
90 |
|
Time to Decision (min) |
45 |
30 |
|
Patient Satisfaction (%) |
85 |
95 |
|
Care Plan Completeness (%) |
60 |
90 |
|
Treatment Success Rate (%) |
78 |
92 |
Another area where semantic sharing has made a big difference is patient happiness. Before it was put into place, only 85 % of patients were satisfied. This was mostly because of things like waiting too long for care, doctors not talking to each other clearly, and not having access to full health records. Patients were 95 % happier after semantic interoperability was put in place because they got faster, more accurate diagnoses and personalised care plans based on their full medical background. Also, the number of full care plans went from 60 % to 90 %, which is a big jump. Semantic sharing lets you see the patient’s medical past as a whole, making sure that all important parts of care are thought about and dealt with. In the same way, treatment success rates went up from 78 % to 92 %, showing how having reliable and easy-to-find patient data can help improve clinical results and make sure that treatment plans work. Overall, semantic interchange makes care faster, better, and more focused on the patient. This improves both the performance of healthcare providers and the happiness of patients.
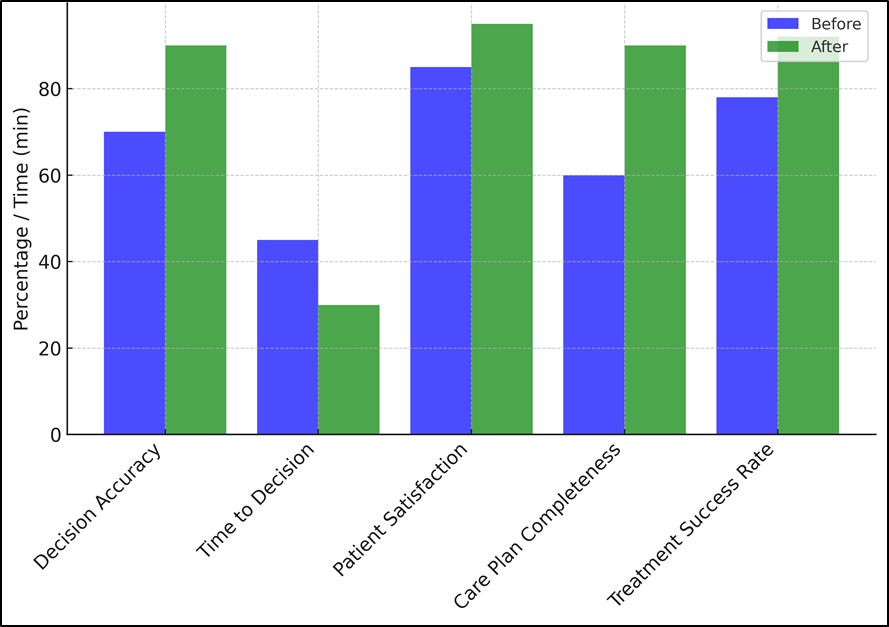
Figure 2. Improved Decision-Making and Patient Care
|
Table 3. Reduction in Medical Errors and Adverse Outcomes |
||
|
Parameter |
Before Semantic Interoperability |
After Semantic Interoperability |
|
Error Rate (%) |
12 |
5 |
|
Adverse Outcome Rate (%) |
18 |
7 |
|
Medication Error Rate (%) |
15 |
3 |
|
Diagnosis Accuracy (%) |
70 |
95 |
|
Treatment Compliance (%) |
65 |
85 |
When semantic interoperability was added to healthcare systems, medical mistakes and bad results went down by a lot. This made patients safer and the system as a whole more efficient. Before semantic compatibility was added, 12 % of healthcare mistakes were made because of wrong readings of patient data, missing health records, and using different medical terms in different ways. This mistake rate dropped to just 5 % after semantic interchange was put into place, though. By standardising data and making sure that information shared between systems is more accurate, healthcare workers can better understand and act on patient information. This makes it much less likely that mistakes will happen in evaluation, treatment, and care delivery. Similarly, the rate of bad outcomes dropped from 18 % to 7 %, which is a huge drop. Bad outcomes often happen because of wrong diagnoses, delays in treatment, or bad drug responses that happen because patient records aren’t full or were shared incorrectly. With semantic interchange, patient records are more full and correct, which helps doctors make better decisions and avoid common mistakes that can have bad results. This decrease not only makes patients safer, but it also makes it easier to treat long-term illnesses and complicated medical conditions.
A big reason why patients get hurt is because of medication mistakes, which went down a lot. Before semantic interchange, 15 % of medicine errors happened because of things like drug combinations, allergies, and prescription records that were not fully filled out. The mistake rate dropped to just 3 % after semantic interchange was put in place. Prescription mistakes are less likely to happen if all drug information is shared correctly between healthcare systems. Also, the accuracy of diagnoses went up from 70 % to 95 %, and treatment satisfaction went up from 65 % to 85 %. These changes were made possible by having access to a more complete and accurate set of patient data. This let doctors assess and treat conditions more accurately, which improved both the level of care and the results for patients.
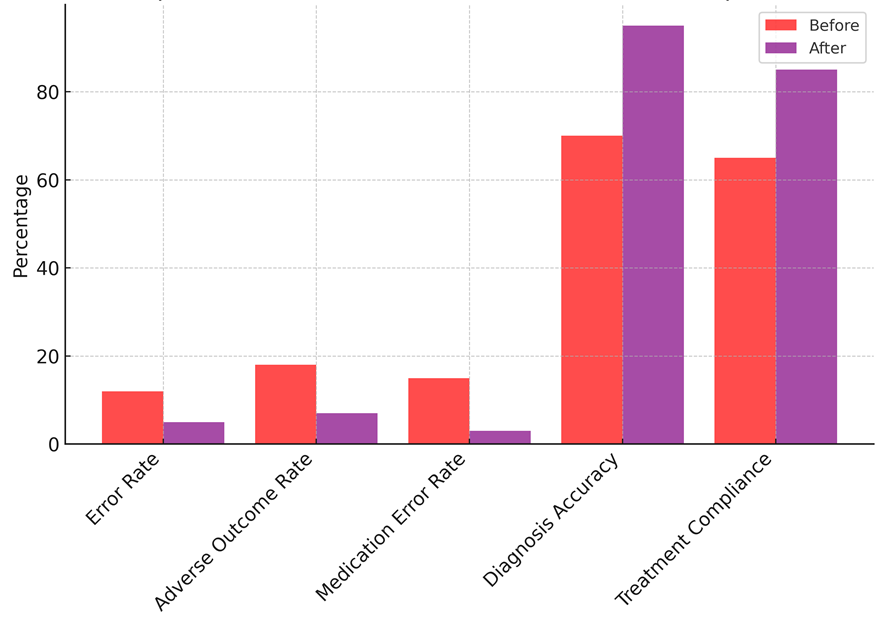
Figure 3. Improvement in Error Rates and Treatment Compliance
|
Table 4. Enhanced Clinical Workflows and Operational Efficiency |
||
|
Parameter |
Before Semantic Interoperability |
After Semantic Interoperability |
|
Workflow Efficiency (%) |
60 |
85 |
|
Time to Treatment (min) |
90 |
60 |
|
Patient Flow Time (min) |
120 |
90 |
|
Care Coordination (%) |
70 |
90 |
|
Resource Utilization (%) |
75 |
95 |
After semantic interoperability was added to healthcare systems, clinical processes and operating efficiency got a lot better. This allowed healthcare providers to give better, more rapid care. Workflow productivity went from 60 % to 85 %, which is one of the biggest changes for the better. Before semantic interoperability was put in place, healthcare workers often had to wait because of broken systems, having to enter data by hand, and not being able to get to all of a patient’s information quickly. These flaws slowed down the work that was being done in clinical settings, which caused patients to have to wait longer for care and made mistakes more likely. When semantic interoperability was introduced, it became easy to combine data from different sources. This let doctors get to patient information quickly and correctly, which sped up processes and made care delivery more efficient overall. Time to treatment is another important success measure that got a lot better, going from 90 minutes to 60 minutes. Before semantic interoperability, it took a lot of time for healthcare workers to physically get and check patient data from different systems. This often caused treatment to be delayed. Semantic interoperability made healthcare systems more linked, which made it easier to get accurate and up-to-date information about patients more quickly. So, doctors and nurses could make choices more quickly, which would allow patients to start treatment more quickly and have better results. Patient flow time, which is the time a patient spends in the healthcare system from the time they are admitted to the time they are sent home, also got better. The time it took went from 120 minutes to 90 minutes because the changes between steps of care went more smoothly. Better communication and planning between departments was made possible by semantic interoperability. This cut down on the time people had to wait for results or switch between healthcare providers. This cut down on patient flow time let doctors help more people in less time, making better use of resources and making the patients’ experiences better.
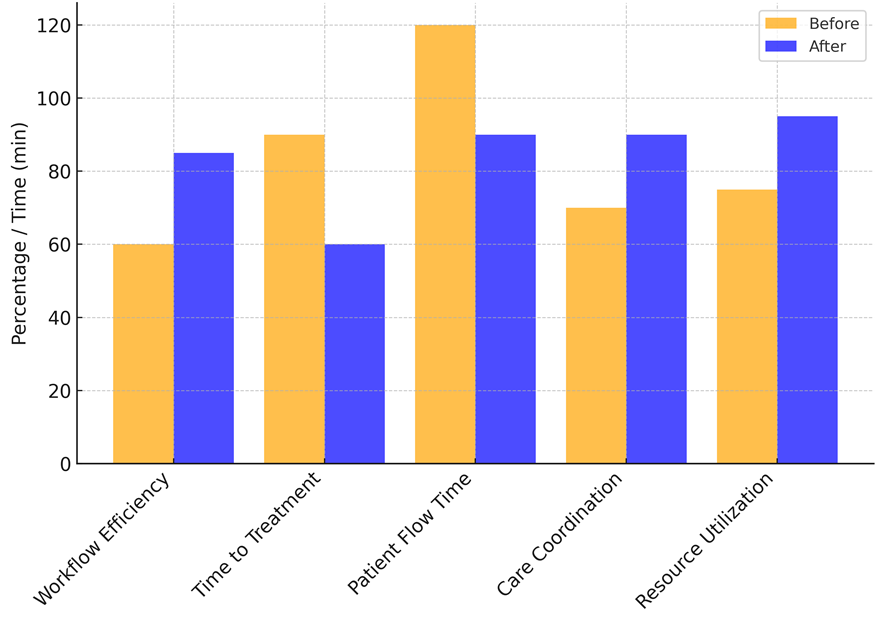
Figure 4. Enhanced Clinical Workflows and Operational Efficiency
From 70 % to 90 %, care planning got better. Semantic connectivity made sure that all the right healthcare workers, like nurses, general practitioners, and specialists, could see the same complete patient data. This made it easier for different care teams to work together, which made sure that all of the patient’s health needs were met on time. Better collaboration meant that patients got more individualised care and that healthcare professionals could handle more complicated situations by working together better. Lastly, the use of resources went up from 75 % to 95 %. Healthcare centres were able to better use their resources by making sure that patient data is shared and read correctly across all systems. Providers were able to make better choices about hiring, using tools, and planning treatments, which led to better use of resources. This better use not only increased working efficiency but also cut costs that weren’t necessary, which let healthcare organisations provide better care with fewer resources. Overall, semantic interoperability made healthcare systems run more easily, providing better care while cutting down on waste and costs.
Facilitating Personalized and Patient-Centered Care
Semantic sharing is very important for promoting personalised and patient-centered care because it makes sure that healthcare workers can easily get correct and complete patient data. The goal of semantic interoperability is to make sure that all healthcare systems can understand and use the same set of patient data. This includes medical history, allergens, medicines, test reports, and imaging data. When healthcare data is formally accessible, doctors can learn more about each patient’s specific health problems, treatment choices, and how they respond to treatment. With this all-around view, care plans can be made that are more successful and specific to each patient. For instance, doctors can choose the best treatments and medicines for a patient by looking at their full medical background, which may include DNA information. This enhances outcomes and reduces adverse effects’ likelihood. Semantic interoperability also facilitates the cooperation among the several specialists engaged in patient care. Semantic interoperability guarantees that all significant healthcare providers have accurate and current information on individuals with complicated medical demands or chronic diseases.
Data privacy and security regulations
Semantic Interoperability Supports Compliance with Healthcare Regulations
Semantic interoperability—which enables healthcare institutions to fulfil privacy and security policies like HIPAA and GDPR—is mostly dependent on regulated, controlled sharing of patient data between healthcare systems. Using standard medical terminology, codes, and forms—like SNOMED CT or ICD-10—one key component of semantic interoperability is these enable proper transmission of patient information while maintaining its meaning. This even data presentation guarantees that patient information is neither altered nor lost throughout the transmission, therefore safeguarding data accuracy and privacy. Semantic sharing also facilitates the implementation of HIPAA’s and GDPR’s required access restrictions and security requirements like encryption. Healthcare systems that permit open data exchange, for instance, can ensure that, depending on their occupations and rights, only those authorised will be able to view certain medical records. Open frameworks can also be developed with regard for patient consent management systems. This guarantees that, concerning who may view their health data, data sharing complies with the patient’s preferences. Semantic interoperability lets systems communicate data in a secure, consistent, and clear manner, therefore helping healthcare companies satisfy regulatory criteria. This raises patient confidence as well as data security.
Legal and Ethical Implications of Data Sharing and Access
Access to medical data and sharing of it have many various moral and legal consequences. On the one hand, sharing patient data amongst healthcare systems can significantly improve patient outcomes by enabling better planned treatment, reduction of pointless testing, and quicker fast action response. On the other hand, it also causes individuals to worry about how personal medical information may be used improperly, such as for identity theft or by someone lacking the proper IDs gaining access without authorisation. These hazards highlight the need of having strong legislation and moral guidelines about who may access data. This is particularly true since that healthcare data is exchanged more internationally and on platforms. To ensure they respect the law when they exchange patient data, healthcare companies have to cope with a variety of various national and foreign legislation like HIPAA in the United States, GDPR in the EU, and other local requirements. Healthcare professionals have to morally balance the obligation to preserve patients’ rights and privacy against the necessity to exchange data. In some situations patients must be allowed to control their own data and decide whether or not to share it with others. Semantic interoperability also has to be implemented in a way that upholds the patient’s right to privacy and lets responsible data sharing help to enhance their health.
International Efforts to Standardize Healthcare Data Exchange
Global connection and the realisation of improved healthcare services depend on international efforts to standardise the exchange of healthcare data. It is obvious that there must be a common method for data sharing as healthcare systems all over becoming increasingly interconnected. Groups such as HL7 International and ISO (International Organisation for Standardisation) develop and advocate standards that enable simple sharing of healthcare data across systems and geographies. Around the globe, key standards such HL7 v2/v3 and FHIR (Fast Healthcare Interoperability Resources) are being applied to provide consistent data types and exchange practices.
Research in semantic interoperability
Overview of Ongoing Projects and Initiatives to Enhance Interoperability
With the main objective of facilitating data sharing between several healthcare systems, several present initiatives and endeavours aim to increase semantic interoperability in healthcare. Made by HL7 International, one of the most significant worldwide initiatives is the Fast Healthcare Interoperability Resources (FHIR) standard. FHIR seeks to make exchanging healthcare data more current and adaptable using web technologies including RESTful APIs. Its simplicity and adaptability help many individuals to utilise it. Standardising data types and allowing several systems to cooperate without any issues helps semantic sharing to be simpler. Another crucial initiative aiming at ensuring data may be exchanged between several EHR systems is the Common Well Health Alliance. To create a national system that interacts with all of the numerous entities the union brings together— funders, healthcare providers, technology businesses, etc.—including through initiatives like the health Exchange, which ties several government entities and healthcare corporations, the Sequoia Project also strives to enhance data exchange and communication. Getting rid of the issues that prevent individuals from sharing data and ensuring that healthcare data can be seen, interpreted, and used the same way across all systems depends on these sorts of initiatives immensely. They focus on developing shared data standards, strengthening security protocols, and developing the infrastructure so that merging goes without problems. Semantic exchange may be attained by means of this cooperative approach, therefore enhancing patient care and enabling more seamless running of healthcare systems.
Collaborative Efforts by Governments, Organizations, and Healthcare Providers
Governments, businesses, and healthcare providers worldwide are collaborating to advance semantic networking and data exchange in healthcare. Programs like the Office of the National Coordinator for Health Information Technology (ONC) run under the direction of the U.S. Department of Health and Human Services (HHS). Encouragement of the adoption of suitable EHRs and ensuring that healthcare data may be securely exchanged falls to the ONC. Setting up a framework for shared standards and simplifying data sharing helps the ONC to explain how to get national connectivity. Among the most significant initiatives in the European Union aiming at facilitating international health data sharing is the European Health Data Space (EHDS). This endeavour to create a solid framework for secure and effective healthcare data exchange includes EU member states, healthcare industry, and data security authorities. These kinds of partnerships help to transfer data more easily while nevertheless adhering to privacy regulations such as GDPR. This guarantees safe and readily available patient data.
Health care companies, government agencies, and global groups like HL7, IHE (Integrating the Healthcare Enterprise), and ISO are all working together to create and use shared standards for health data. Working together is important for getting past gaps between regions and building a healthcare system that works everywhere. The main goals are to use standard data forms, make rules to make sure privacy laws are followed, and get a lot of people to use standards like FHIR.
Key Research Advancements in the Field of Semantic Interoperability
Recently, semantic interoperability research has been mainly about coming up with ways to make healthcare data sharing more accurate, faster, and scalable. Coming up with standardised models and coding systems is a big step forward. Researchers have shown how important it is to use complete, machine-readable medical terminologies like SNOMED CT, ICD-10, and LOINC. These help systems describe data consistently and understand it more accurately.(16) These coding systems are always getting better, with new changes and maps being added to keep up with new medical situations and knowledge. Adding Natural Language Processing (NLP) and Machine Learning (ML) technologies to healthcare systems to make semantic sharing easier is another big step forward in the field. Using these tools, a lot of arbitrary clinical writing—including doctor’s notes and release reports—quickly becomes ordered data that is easily shared and understood. The data is more complete and accurate as NLP algorithms can extract relevant information from text files, according to researchers. Particularly with regard to ensuring that health data transfers are safe and can be followed, more and more individuals are interested in blockchain technology as a viable means to enhance semantic communication. A decentralised, immutable record system, blockchain might assist with problems such data privacy, security, and obtaining patient consent to utilise compatible technology.
Challenges and Solutions Identified in Current Literature
Semantic communication has gone a long way, but as recent research publications have revealed, certain issues still need to be resolved. It is rather difficult when standardised data standards are absent. Though many healthcare systems still utilise their own forms, standards like FHIR and HL7 are in existence. Sharing data without any issues becomes difficult as a result. Studies show that common standards must be generally embraced worldwide if semantic connectedness is to occur. Administrative and technological opposition must so be overcome.
Still additional issue is data security and protection concerns. While standards like GDPR in Europe and HIPAA in the United States assist safeguard patient data, they also complicate the creation of systems capable of communicating with one another. Making sure secure data-sharing tools complement legal frameworks at the same time is never easy. Using secured data and safe APIs are two strategies researchers have devised to make data exchange safer. Semantic variation—that is, the possibility that several systems may depict the same concept in different ways depending on their terminology and coding systems—is a third challenge. Experts have so advised creating conceptual mappings between several words and using common models that can help to make healthcare data more consistent so that this does not happen. Additionally under investigation are artificial intelligence-powered solutions as a means of streamlining mapping tasks and facilitating alignment across several code systems.
Future directions in semantic interoperability for ehr systems
Integration of AI, Machine Learning, and Big Data in Healthcare Systems
Including artificial intelligence (AI), machine learning (ML), and big data into healthcare systems marks a significant progress towards semantically interoperable Electronic Health Records (EHR). AI and ML can enable far quicker and more accurate data exchange by simplifying the analysis of complex and varied healthcare data. For example, ML systems can search a lot of patient data to identify trends, project future health outcomes, and provide customised treatment plans. Doctors will find it simpler to make judgements as result. Apart from semantic connectedness, these technologies enable healthcare systems to better interpret and evaluate data from many sources, therefore ensuring not just usability but also value. Big data analytics is quite crucial as it allows many healthcare data to be gathered, kept, and examined. Electronic health records, data from smart devices, and patient real-time tracking are among this data sources. Semantic interoperability allows these massive databases to be readily merged and distributed between systems. This helps to organise a patient’s treatment and presents a whole picture of their health. Still, data security, privacy, and safety present issues. More research is required to ensure that, as artificial intelligence and machine learning advance, these systems can manage and interpret many kinds of unorganised healthcare data while maintaining patient information safe and secure. Future usage of these instruments will be increasing since they will enable doctors to make better decisions, enhance procedures, and offer tailored treatment.
Emerging Trends in Global Health Data Sharing and Semantic Interoperability
By reducing the barriers preventing data from freely flowing, new trends in semantic exchange and global health data sharing are altering the direction of healthcare systems. Like FHIR, open data standards allow healthcare data to be shared consistently throughout systems, sectors, and nations. Among the most crucial patterns is this one. International organisations such as the OECD and the World Health Organisation (WHO) advocate for these norms to be extensively applied. They want to create a worldwide platform for exchanging health data such that it benefits every system. As healthcare institutions all over understand the necessity to exchange patient information—especially for those who receive treatment abroad—cross-border data sharing is also growing in favour. Patients with complex medical backgrounds and healthcare professionals interacting with individuals from several nations particularly depend on this. Two of the key initiatives aiming to ensure that health data may be securely and successfully exchanged between nations while still adhering to national policies are European Health Data Space (EHDS) and eHealth Exchange. Real-time data sharing utilising smart tech, internet tracking, and healthcare applications is also become more frequent. Using electronic health record (EHR) systems will be rather crucial to ensure that healthcare data generated outside of normal hospital environments can be utilised. This new trend emphasises the need of including wearable’s and mobile health applications into EHR systems in an approach that maintains the consistency and veracity of the data. The future of exchanging health data will be defined by better worldwide collaboration and the development of more sophisticated technologies to enable the use of health data on several platforms and inside nations.
CONCLUSION
Changing Electronic Health Record (EHR) systems and improving the broader healthcare environment depends mostly on semantic openness. By ensuring that data sent across several systems is accurate and relevant, semantic interoperability solves long-standing issues like broken data, misunderstandings, and inadequate care planning. Standardised terminology and code systems—like SNOMED CT, ICD-10, and LOINC—make it simple for medical professionals to uniformly exchange patient data. This reduces medical errors, helps clinicians make better judgements, and enhances patient care outcomes. Combining fresh technologies such artificial intelligence, machine learning, and blockchain offers great potential to improve semantic connectedness even more. Blockchain offers safe, open, and distributed means to manage data; AI-powered systems can automatically process and analyse data. These fresh concepts and international research initiatives taken together are improving the safety, efficiency, and patient-oriented emphasis of healthcare systems. Some issues still have to be resolved even with these developments. Standards must be embraced by everybody, privacy concerns must be addressed, and semantic variation in data representation must be corrected. Healthcare professionals, governments, and tech developers have to keep cooperating and doing research if they are to address these issues. Semantic connectivity’s future is in developing flexible, scalable solutions that can expand with new technologies and satisfy the demands of people and healthcare systems all across the globe as healthcare data grows more complex. A more connected, efficient, and patient-centered healthcare environment will follow from effective implementation of semantic interoperability. This will raise the degree of treatment as well as the operating speed. Making the ideal of a completely open, data-driven healthcare system come reality depends on this greatly.
RECOMMENDATIONS
To increase semantic interoperability for EHR systems and open the path for the future of healthcare data exchange, further research has to be conducted on a few important topics. An important topic of research is developing new data standards able to manage the increasing complexity of healthcare data. Though the rules we presently follow help, they might not completely satisfy the demands of future technologies as big data, IoT, and artificial intelligence. Standards must be more flexible, scalable, and all-encompassing to match the changes in healthcare data. More research on how to apply artificial intelligence and machine learning to produce more consistent and of higher quality EHR data is also needed. Though to teach algorithms properly, they require large, high-quality information; AI may help standardise medical jargon, reduce errors, and ease data cleaning chores. More research is required to produce artificial intelligence-powered systems capable of verifying the completeness and correctness of data from several healthcare systems. Still another fascinating field of research with great promise is patient-centered data exchange. While ensuring that these systems can interact with one another, researchers should consider fresh approaches to provide individuals authority over their medical records. Making ensuring people have control over their personal data without restricting the flow of data between healthcare providers depends on secure and simple to use permission management technologies being developed.
REFERENCES
1. Reis, Z.S.N.; Maia, T.A.; Marcolino, M.S.; Becerra-Posada, F.; Novillo-Ortiz, D.; Ribeiro, A.L.P. Is there evidence of cost benefits of electronic medical records, Standards, or Interoperability in hospital information systems? Overview of systematic reviews. JMIR Med. Inform. 2017, 5, e7400.
2. Abernethy, A.; Adams, L.; Barrett, M.; Bechtel, C.; Brennan, P.; Butte, A.; Faulkner, J.; Fontaine, E.; Friedhoff, S.; Halamka, J.; et al. The Promise of Digital Health: Then, Now, and the Future. NAM Perspect. 2022, 6, 108–116.
3. Shinozaki, A. Electronic Medical Records and Machine Learning in Approaches to Drug Development. In Artificial Intelligence in Oncology Drug Discovery and Development; IntechOpen: London, UK, 2020.
4. Ntafi, C.; Spyrou, S.; Bamidis, P.; Theodorou, M. The legal aspect of interoperability of cross border electronic health services: A study of the european and national legal framework. Health Inform. J. 2022, 28, 146045822211287.
5. Kouroubali, A.; Katehakis, D.G. The new European interoperability framework as a facilitator of digital transformation for citizen empowerment. J. Biomed. Inform. 2019, 94, 103166.
6. Yang, H.; Yang, B. A Blockchain-Based Approach to the Secure Sharing of Healthcare Data. In Proceedings of the Norwegian Information Security Conference 2017, Oslo, Norway, 27–29 November 2017; pp. 100–111.
7. Lin, Q.; Wang, H.; Pei, X.; Wang, J. Food Safety Traceability System Based on Blockchain and EPCIS. IEEE Access 2019, 7, 20698–20707.
8. Yan, X.; Wu, Q.; Sun, Y. A Homomorphic Encryption and Privacy Protection Method Based on Blockchain and Edge Computing. Wirel. Commun. Mob. Comput. 2020, 2020, 8832341.
9. Dagher, G.G.; Mohler, J.; Milojkovic, M.; Marella, P.B. Ancile: Privacy-preserving framework for access control and interoperability of electronic health records using blockchain technology. Sustain. Cities Soc. 2018, 39, 283–297.
10. Azaria, A.; Ekblaw, A.; Vieira, T.; Lippman, A. MedRec: Using Blockchain for Medical Data Access and Permission Management. In Proceedings of the 2016 2nd International Conference on Open and Big Data (OBD), Vienna, Austria, 22–24 August 2016; pp. 25–30.
11. Ivan, D. Moving toward a blockchain-based method for the secure storage of patient records. In Proceedings of the ONC/NIST Use of Blockchain for Healthcare and Research Workshop, Gaithersburg, MD, USA, 22–24 August 2016; pp. 1–11.
12. Rajput, A.R.; Li, Q.; Ahvanooey, M.T. A blockchain-based secret-data sharing framework for personal health records in emergency condition. Healthcare 2021, 9, 206.
13. Mwogosi, A. Digital Transformation in Tanzania’s Healthcare Sector: A Systematic Review of Robust Electronic Health Records Systems’ Critical Success Factors. Res. Sq. 2023.
14. Semantha, F.H.; Azam, S.; Shanmugam, B.; Yeo, K.C. PbDinEHR: A Novel Privacy by Design Developed Framework Using Distributed Data Storage and Sharing for Secure and Scalable Electronic Health Records Management. J. Sens. Actuator Netw. 2023, 12, 36.
15. K. K. Das, Priyanka Tripathy. (2015). Impact of Socio-Economic and Demographic Profile on Consumer Preferences of Retail Formats in Urban Odisha. International Journal on Research and Development - A Management Review, 4(4), 39 - 43.
16. Mishra, R.; Kaur, I.; Sahu, S.; Saxena, S.; Malsa, N.; Narwaria, M. Establishing three layer architecture to improve interoperability in Medicare using smart and strategic API led integration. SoftwareX 2023, 22, 101376.
FINANCING
None.
CONFLICT OF INTEREST
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Pavas Saini, Dipak Sethi, Sujayaraj Samuel Jayakumar, Zuleika Homavazir, Asit Kumar Subudhi, Kothakonda Sairam, Lalit Khanna.
Data curation: Pavas Saini, Dipak Sethi, Sujayaraj Samuel Jayakumar, Zuleika Homavazir, Asit Kumar Subudhi, Kothakonda Sairam, Lalit Khanna.
Formal analysis: Pavas Saini, Dipak Sethi, Sujayaraj Samuel Jayakumar, Zuleika Homavazir, Asit Kumar Subudhi, Kothakonda Sairam, Lalit Khanna.
Research: Pavas Saini, Dipak Sethi, Sujayaraj Samuel Jayakumar, Zuleika Homavazir, Asit Kumar Subudhi, Kothakonda Sairam, Lalit Khanna.
Methodology: Pavas Saini, Dipak Sethi, Sujayaraj Samuel Jayakumar, Zuleika Homavazir, Asit Kumar Subudhi, Kothakonda Sairam, Lalit Khanna.
Project management: Pavas Saini, Dipak Sethi, Sujayaraj Samuel Jayakumar, Zuleika Homavazir, Asit Kumar Subudhi, Kothakonda Sairam, Lalit Khanna.
Resources: Pavas Saini, Dipak Sethi, Sujayaraj Samuel Jayakumar, Zuleika Homavazir, Asit Kumar Subudhi, Kothakonda Sairam, Lalit Khanna.
Software: Pavas Saini, Dipak Sethi, Sujayaraj Samuel Jayakumar, Zuleika Homavazir, Asit Kumar Subudhi, Kothakonda Sairam, Lalit Khanna.
Supervision: Pavas Saini, Dipak Sethi, Sujayaraj Samuel Jayakumar, Zuleika Homavazir, Asit Kumar Subudhi, Kothakonda Sairam, Lalit Khanna.
Validation: Pavas Saini, Dipak Sethi, Sujayaraj Samuel Jayakumar, Zuleika Homavazir, Asit Kumar Subudhi, Kothakonda Sairam, Lalit Khanna.
Display: Pavas Saini, Dipak Sethi, Sujayaraj Samuel Jayakumar, Zuleika Homavazir, Asit Kumar Subudhi, Kothakonda Sairam, Lalit Khanna.
Drafting - original draft: Pavas Saini, Dipak Sethi, Sujayaraj Samuel Jayakumar, Zuleika Homavazir, Asit Kumar Subudhi, Kothakonda Sairam, Lalit Khanna.
Writing: Pavas Saini, Dipak Sethi, Sujayaraj Samuel Jayakumar, Zuleika Homavazir, Asit Kumar Subudhi, Kothakonda Sairam, Lalit Khanna.