doi: 10.56294/mw2024515
REVIEW
Machine Learning Applications in Medical Information Science for Automated Diagnosis and Treatment Plans
Aplicaciones del aprendizaje automático en la ciencia de la información médica para el diagnóstico automatizado y los planes de tratamiento y planes de tratamiento
Mohan Garg1 ![]() ,
Prabhjot Kaur2
,
Prabhjot Kaur2 ![]() ,
Joginder3
,
Joginder3 ![]() ,
Manashree Mane4
,
Manashree Mane4 ![]() ,
Kunal Meher5
,
Kunal Meher5 ![]() ,
Tapasmini Sahoo6
,
Tapasmini Sahoo6 ![]() ,
Vundela Swathi7
,
Vundela Swathi7 ![]()
1 Chitkara Centre for Research and Development, Chitkara University, Himachal Pradesh. India.
2 Centre of Research Impact and Outcome, Chitkara University, Rajpura, Punjab. India.
3 School of Allied Health Sciences, Noida International University, Greater Noida, Uttar Pradesh. India.
4 Forensic Science, JAIN (Deemed-to-be University), Bangalore, Karnataka. India.
5 Department of uGDX, ATLAS SkillTech University, Mumbai, Maharashtra. India.
6 Department of Electronics and Communication Engineering, Siksha ‘O’ Anusandhan (Deemed to be University), Bhubaneswar, Odisha. India.
7 Centre for Multidisciplinary Research, Anurag University, Hyderabad, Telangana. India.
Cite as: Garg M, Kaur P, Joginder J, Mane M, Meher K, Sahoo T, et al. Machine Learning Applications in Medical Information Science for Automated Diagnosis and Treatment Plans. Seminars in Medical Writing and Education. 2024; 3:515. https://doi.org/10.56294/mw2024515
Submitted: 27-10-2023 Revised: 28-01-2024 Accepted: 29-05-2024 Published: 30-04-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding author: Mohan Garg *
ABSTRACT
Machine learning (ML) simplifies diagnostic and treatment planning automation in medical computer science. This is profoundly altering the healthcare industry. Thanks to rapid development in machine learning algorithms and their capacity to evaluate large, complicated information, medical decision-making has become far more accurate and simplified. By searching for trends in patient data including medical records, diagnostic images, and genetic information that might not be clear-cut for human specialists, machine learning models might assist clinic-based clinicians in These models not only enable doctors to identify issues early on but also enable them to create tailored treatment strategies for every patient’s requirement. In managing repetitious tasks, forecasting how illnesses would worsen, and recommending therapies, ML techniques like supervised learning, unsupervised learning, and deep learning have also demonstrated astonishing outcomes. Dealing with chronic illnesses, cancer, and emergency care scenarios calls specifically for these abilities. Furthermore improving decision support systems driven by ML helps to reduce medical errors and maximise the resources of healthcare systems. Including machine learning models into medical information systems might help to improve patient outcomes, simplify tasks, and reduce costs as healthcare keeps becoming digital. However, societal issues, data security, and the necessity of legal structures have to be considered to guarantee that ML technologies are applied responsibly in the medical field.
Keywords: Machine Learning; Medical Information Science; Automated Diagnosis; Personalized Treatment Plans; Disease Prediction; Decision Support Systems.
RESUMEN
El aprendizaje automático (AU) simplifica la automatización del diagnóstico y la planificación del tratamiento en la informática médica. Esto está alterando profundamente la industria sanitaria. Gracias al rápido desarrollo de los algoritmos de aprendizaje automático y a su capacidad para evaluar información voluminosa y complicada, la toma de decisiones médicas se ha vuelto mucho más precisa y simplificada. Mediante la búsqueda de tendencias en los datos de los pacientes, como historiales médicos, imágenes de diagnóstico e información genética, que podrían no estar claras para los especialistas humanos, los modelos de aprendizaje automático podrían ayudar a los médicos clínicos a Estos modelos no sólo permiten a los médicos identificar problemas en una fase temprana, sino también crear estrategias de tratamiento adaptadas a las necesidades de cada paciente. En la gestión de areas repetitivas, la previsión del empeoramiento de enfermedades y la recomendación de terapias, técnicas de AU como el aprendizaje supervisado, el aprendizaje no supervisado y el aprendizaje profundo también han demostrado resultados sorprendentes. El tratamiento de enfermedades crónicas, cáncer y situaciones de atención de emergencia requiere específicamente estas capacidades. Además, la mejora de los sistemas de apoyo a la toma de decisiones basados en el aprendizaje automático ayuda a reducir los errores médicos y a maximizar los recursos de los sistemas sanitarios. La inclusión de modelos de aprendizaje automático en los sistemas de información médica podría ayudar a mejorar los resultados de los pacientes, simplificar las tareas y reducir los costes a medida que la sanidad se digitaliza. Sin embargo, hay que tener en cuenta los aspectos sociales, la seguridad de los datos y la necesidad de estructuras jurídicas para garantizar que las tecnologías de AU se apliquen de forma responsable en el ámbito médico.
Palabras clave: Aprendizaje Automático; Ciencia de la Información Médica; Diagnóstico Automatizado; Planes de Tratamiento Personalizados; Predicción de Enfermedades; Sistemas de Apoyo a la Toma de Decisiones.
INTRODUCTION
New technologies especially machine learning (ML) have enabled the healthcare industry to undergo significant transformation in the past few years. In medical information science, where machine learning is a fundamental component of making diagnosis more accurate, organising treatments more effectively, and giving all patients better care, this development is very obvious. Important decisions concerning examination and treatment are generally made by hand in conventional healthcare systems utilising human expertise and data analysis. These techniques, however, depend on having access to experts with a lot of expertise, can take a long time, and cause blunders. Machine learning is a hopeful solution in contrast as it automates many aspects of healthcare decision-making, therefore accelerating treatments, increasing accuracy, and customising therapies to every individual. Within artificial intelligence, machine learning is the study of creating algorithms allowing computers to learn from data, identify trends, and make decisions or predictions devoid of explicit programming to guide them. ML models in the field of medical information science are trained on enormous volumes of medical data including clinical records, genetic information, test findings, patient details, and medical pictures. Because ML can examine and learn from a number of various information, it can identify little trends and patterns that people might overlook. This raises detection accuracy. For instance, frequently as precisely as or more correctly than human specialists, ML algorithms have been employed effectively in imaging disciplines including radiology and pathology to help discover things like tumours, fractures, and scan anomalies. Automation of detection made possible by machine learning has enormous impact on medical care. Getting improved outcomes from therapy depends critically on early identification, particularly for diseases such cancer, heart disease, and brain disorders. Early illness detection enabled by machine learning techniques for patient data analysis allows clinicians to respond fast, therefore reducing the burden of chronic conditions or maybe saving lives. Helping physicians create more individualised treatment regimens, ML models also assist predict how illnesses will worsen and how patients will fare. These prediction abilities enable clinicians to customise their therapy for every patient’s particular genetics, lifestyle, and medical background instead of following set guidelines. Apart from altering our diagnosis approach, ML is altering our treatment planning as well. Though most conventional therapies are one-size-fits-all, machine learning enables more individualised treatment. Looking at historical patient data and considering things like genetic information, environmental circumstances, and patient response to past therapies, ML systems can determine the optimum course of therapy for every patient. Because of this customisation, patients improve as they receive treatment catered to their preferences and conditions. For instance, ML-based algorithms are being applied in cancer to forecast patient response to various chemotherapy agents. This guides clinicians in selecting the optimal course of action for every patient.(1) Furthermore, in medical computer science, machine learning may be applied for administrative and practical purposes inside healthcare companies. By means of structuring, distributing resources, and management of work flows, ML models help to raise the general efficiency of healthcare systems.(2) All of which enhance the degree of treatment are predictive models helping hospitals plan ahead for patient demand, simplify operations, and reduce wait times. Because ML provides healthcare professionals data-driven insights that enable them to make treatment decisions, it is also rather vital for improving decision support systems. These technologies can alert clinicians to potential issues, offer advice on how to prevent them, or recommend modifications to the treatment approach. ML has great potential in healthcare, but applying it in medicine also comes with some difficulties. This reduces the possibility of mistakes and makes the patient safer. Finding easily available useful information is one of the main issues. Machine learning models cannot function without a great volume of high-quality, diverse data. Making ensuring the data is accurate, complete, and fairly represents the patients is absolutely crucial if one wants to achieve real and reliable findings. Given patient data is quite private, issues with data safety and security also have to be addressed. Particularly crucial are ethical issues such ensuring that judgements are taken transparently and lowering of bias in machine learning systems. Strong regulations have to complement the application of machine learning in healthcare to guarantee ethical and correct usage of these technologies.
Related work
In medical information science, machine learning (ML) has attracted a lot of interest as it may alter the operations of healthcare systems. Numerous studies have indicated that machine learning models can assist in automatically planning and diagnosis of therapies. Initially, most in the area relied on utilising machine learning techniques—such as support vector machines and decision trees—to utilise clinical data to identify illnesses patients carried. By leveraging patient information including age, gender, lifestyle choices, and clinical data, ML models have been effectively employed, for example, to detect diabetes, heart disease, and cancer.(3) Early initiatives paved the path for more sophisticated techniques as better program development and computer capacity allowed one to extract more from the medical data. New research indicates that deep learning techniques—especially convolutional neural networks (CNNs)—are being applied increasingly in medical picture processing. CNNs outperform more traditional techniques in looking at medical images like X-rays, CT scans, and MRI scans. Sometimes these models outperform people in identifying early-stage ailments such lung cancer and brain tumours,(4) and they may pinpoint abnormalities as precisely as human specialists. One should note that radiology makes extensive use of CNNs. The models expedite diagnosis and treatment decisions by automatically sorting and explaining medical images. Studies have also demonstrated the need of using multi-modal data—that is, imaging data mixed with genetic data—to make diagnosis more accurate and treatment regimens better.(5)
Additionally applied in genetics is machine learning (ML), which has produced tailored treatment approaches. Programmes in machine learning can examine a person’s genetic data to project their likelihood of acquiring specific diseases or response to particular therapies. For instance, ML models have been applied to project cancer patient performance depending on symptoms and DNA modifications.(6) These prediction models enable medical professionals create more individualised treatment regimens. These strategies have a higher possibility of success if one chooses the most efficient medication depending on their DNA. novel DNA variants and signals potentially employed in the creation of novel medications have also been discovered using machine learning algorithms.(7) Reinforcement learning (RL) piques people’s curiosity as a potential approach to guide medical decisions during treatment planning. Dealing with their environment and receiving feedback on what happens helps RL systems learn how to make a sequence of decisions. In the medical field, RL has been applied to develop decision-support systems capable of suggesting tailored treatment options for long-term conditions including diabetes and heart disease.(8) As more data on every patient comes in, these algorithms learn and improve in suggesting ideas over time. Treatment strategies are thus more precise and successful. In cancer, where treatment strategies are generally complex and must include several factors including patient response to medicine and potential adverse effects,(9) RL has proved very helpful. Additionally under investigation is machine learning to determine whether it may be used to forecast future health hazards and worsening of illnesses. By examining at long-term patient data, ML models can forecast how likely an illness will worsen, identify people more likely to have issues, and provide strategies to prevent such difficulties from arising. Those with long-term conditions such Alzheimer’s disease, diabetes, and heart failure have utilised these predictive abilities to monitor their conditions.(10) ML models have been applied, for instance, to estimate the likelihood of a heart failure patient requiring hospital visits. This helps individuals to respond fast and maximise available resources. Not only do predictive models for how illnesses may migrate aid with treatment planning, but they also maximise healthcare resources, therefore reducing costs overall and improving patient outcomes.(11)
ML researchers also are interested by making herbal language processing (NLP) equipment that could assist human beings locate clinical records and make decisions. NLP strategies are used to get beneficial facts out of clinical textual content that is not organised, like scientific notes, digital fitness facts (EHR), and clinical books. Researchers have created systems which could discover tendencies, signs, and situations which are wanted for assessment and remedy through the use of ML fashions on this records. By way of picking up on small notes of signs and symptoms in patient statistics,(12) these gear have been shown to help find diseases early on. NLP also can help automate recurring chores like payments and reporting, which makes healthcare greater green and lowers the threat of errors.(13) Even though progress has been made in the usage of system studying in healthcare, there are nonetheless troubles that need to be fixed before those technology may be extensively used. It is very hard to make sure that the statistics used to train machine mastering fashions is accurate. Predictions that are biassed or now not based totally on information can be made when records is missing or incorrect. Researchers have stressed the importance of using large, varied datasets to make sure that machine learning models are reliable and fair, especially when they are used on groups of people from different backgrounds.(14) ML is also hard to use because it raises ethical questions about medical decisions. Before broad acceptance can happen, concerns about data protection, openness, and responsibility must be resolved. Studies have called for rules to be made about how to use machine learning in healthcare to protect patients and build trust.(15) Also, being able to explain ML models is very important in healthcare situations, where choices have big effects. Models that are both reliable and easy to understand are being worked on so that doctors can figure out why automatic suggestions are made.(16)
|
Table 1. Machine Learning Applications In Medical Information Science |
|||||
|
Study/Research Area |
Machine Learning Technique |
Application Focus |
Outcome/Results |
Challenges Identified |
Data Sources Used |
|
Medical Image Analysis |
Convolutional Neural Networks (CNNs) |
Radiology and medical image classification |
Improved diagnostic accuracy in medical imaging |
Limited labeled data for training models |
Medical imaging datasets (X-rays, MRIs, CT scans) |
|
Cancer Prognosis |
Support Vector Machines (SVM) |
Predicting survival rates and recurrence |
Better prediction of cancer prognosis |
Difficulties in integrating genetic data |
Clinical and genomic data |
|
Genomic Data Analysis |
Random Forests |
Identifying biomarkers and genetic variants |
Personalized treatment plans based on genetic data |
Data heterogeneity and quality issues |
Genomic and clinical databases |
|
Treatment Planning with RL |
Reinforcement Learning (RL) |
Optimizing treatment strategies |
Enhanced decision-making for chronic diseases |
Complexity in patient-specific model adaptation |
Patient treatment history and outcomes |
|
Disease Progression Prediction |
Long Short-Term Memory (LSTM) |
Predicting patient outcomes in chronic diseases |
More accurate disease progression models |
Insufficient longitudinal patient data |
Electronic Health Records (EHRs) |
|
Natural Language Processing in Healthcare |
Natural Language Processing (NLP) |
Extracting data from clinical notes and EHR |
Automated diagnosis from clinical records |
Difficulty in interpreting unstructured data |
Clinical text data from EHRs |
|
Personalized Medicine |
Deep Learning (DNN) |
Predicting disease response based on genetics |
Tailored treatments based on genetic profile |
Issues with patient data privacy and ethics |
Genetic and treatment outcome data |
|
Chronic Disease Monitoring |
Random Forests |
Monitoring progression and identifying at-risk patients |
Better management of chronic conditions |
Managing vast amounts of patient data |
EHRs and wearable device data |
|
Heart Failure Prediction |
Support Vector Machines (SVM) |
Identifying risk of hospitalization and interventions |
Timely interventions and resource optimization |
Handling unstructured and noisy data |
EHRs and clinical observations |
|
Cancer Outcome Prediction |
Gradient Boosting Machines (GBM) |
Optimizing chemotherapy regimens |
Optimized treatment protocols for cancer patients |
Need for large, diverse datasets |
Patient genetic and medical history |
|
AI in Radiology |
Deep Learning (CNNs) |
Classifying and interpreting radiological images |
Faster and more accurate interpretation of images |
Scalability of image analysis systems |
Medical imaging datasets |
|
Predictive Analytics in Surgery |
Recurrent Neural Networks (RNNs) |
Analyzing pre-surgical data for outcomes |
Predictive insights for surgical success |
Complexity in real-time prediction systems |
Preoperative and patient clinical data |
|
Machine Learning in Healthcare Operations |
Decision Trees and SVM |
Improving hospital resource management and scheduling |
Reduced operational costs and improved workflow efficiency |
Data privacy concerns in healthcare applications |
Hospital administrative and operational data |
Machine learning techniques in medical diagnosis
Overview of ML algorithms used in automated diagnosis
In figure 1, demonstrate different types of data are combined in healthcare to create personalised medicine using machine learning and data analysis. The picture shows an organised system that starts with different kinds of biology and clinical data. These are then processed and analysed using advanced computer methods. The different kinds of patient data used in medical study and diagnosis are shown on the left side of the image. Some of these are genetic data (DNA and RNA patterns), phenotypic (visible traits), lifestyle factors, lab tests, gene expression, images, and the patient’s background. Together, these parts make up a high-dimensional file that has a lot of complicated information about a person’s health. In the middle of the picture, it shows how these data sources are changed into a high-dimensional collection that is the basis for more advanced learning methods. These methods, which include AI and machine learning, use the data to find trends and ideas that are useful. The data analysis and visualisation step, shown on the right side of the figure, turns the processing data into insights that can be used. The end result is personalised medicine, in which a person’s treatment plans and drug orders are made to fit their specific genetic and clinical makeup. This makes treatment more effective and improves patient outcomes.
Figure 1. Overview of system architecture
Support Vector Machines (SVM)
Support Vector Machines (SVM) are used loads in medical analysis due to the fact they may be reliable and can kind via numerous records. Finding the exceptional hyper plane that divides one of a kind varieties of statistics points in a characteristic space is how SVM works. That is very helpful for jobs like sorting illnesses into businesses based totally on biomarker records, clinical pix, and medical tendencies. One manner that SVM has been used is to locate cancers like breast and lung most cancers via looking at medical traits, genetic information, or x-rays. One of the first-class things about SVM is that it may work with both linear and nonlinear information. This makes it useful for a wide range of diagnostic tasks. It may additionally generalise, which facilitates make predictions more accurate while there isn’t a whole lot of statistics.
Decision Tree
Every other common technique used in medicinal drug for detection is the selection tree. This program makes use of a fixed of “if-then” rules to determine which components of the information to apply based totally at the numbers of its capabilities. they may be in particular excellent at recognizing illnesses primarily based on matters like the affected person’s age, own family history, signs, and check consequences. In remedy, decision bushes are frequently used to position humans with lengthy-term illnesses like diabetes, heart disorder, and others into agencies based on their risk of having worse. Making choices with selection bushes is apparent, which is important in professional conditions where know-how is key. They will, but, over fit while the facts is noisy or too complex, however techniques like trimming can assist with this.
Unsupervised learning
Clustering
Clustering is a kind of unsupervised mastering wherein the purpose is to place records points into corporations which can be comparable without labelling them first. Clustering strategies, together with ok-approach and hierarchical clustering, are used in scientific analysis to discover traits or subgroups inside patient populations. This may be very useful for finding new varieties of illnesses, putting human beings into businesses based totally on their signs or genetic markers, and even getting new insights from scientific or clinical information that weren’t obvious at the beginning. In cancer genomes, for instance, grouping techniques have been used to find one of a kind genetic agencies of tumours, which has brought about extra focused treatments. Massive, unlabelled datasets will have secret styles that can be determined with clustering. Those styles can help with study and treatment selection.
Anomaly Detection
Another impartial getting to know technique is anomaly identification, which looks for statistics points that do not suit the ordinary trend thoroughly. Those are frequently known as “outliers.” Anomaly identification is an important a part of clinical diagnostics for locating unusual sicknesses or unusual affected person situations that do not fit into regular diagnostic classes. as an example, it is able to be used to mark as ordinary any test results or clinical pix that could show the beginning steps of diseases like cancer or brain issues. Isolation Forests and autoencoders are examples of anomaly detection algorithms which can help discover atypical readings in critical symptoms, ECG data, or even medical scans. Being capable of spot these varieties of oddities can assist docs locate illnesses early and start remedy right away, which can save lives.
Deep learning
Convolutional Neural Networks (CNNs)
Convolutional Neural Networks (CNNs) are a form of deep studying models which might be excellent at working with grid-like statistics, like pics. CNNs are revolutionising the field of medical imaging due to the fact they are able to easily apprehend clinical scans like X-rays, CT scans, and MRIs. CNNs help discover distinct forms of troubles in these conditions, like tumours, fractures, and sores. Those models examine hierarchical functions from the uncooked photo records on their very own, which makes them top notch for jobs that need to comprehend areas. CNNs were used loads to automatically locate lung cancer from chest X-rays or skin cancer from pics excited about a demography. CNNs are beneficial due to the fact they could cut down at the time had to understand pics and make detection accuracy better.
Recurrent Neural Networks (RNNs)
Deep mastering fashions referred to as Recurrent Neural Networks (RNNs) are made to cope with sequential data. These networks paintings properly for jobs that want to cope with time-collection records or information that changes through the years, like ECG signs and symptoms, medical facts, and even statistics from watching patients. lengthy quick-time period reminiscence (LSTM) networks, which can be a more advanced shape of RNNs, had been used to are expecting how patients will do, how illnesses will get worse, and to find coronary heart rate issues. For example, RNNs were used to preserve an eye fixed on people who have heart illnesses. They could study modifications in a person’s heart fee in actual time to guess whilst a heart attack might show up. RNNs are excellent at computerized analysis because they study timing connections in records. This is specifically beneficial for coping with continual illnesses and retaining a watch on sufferers in actual time.
Applications in diagnostic imaging, pathology, and genomics
System gaining knowledge of strategies, particularly CNNs, have made it lots simpler and extra accurate to examine scientific photographs for diagnostic purposes. Imaging techniques like MRI, CT scans, and X-rays are now being used with those structures to discover diseases like cancer, broken bones, and brain situations. ML models can automatically separate pix, locate troubles, and even organization distinctive styles of cells, which enables medical doctors make extra correct predictions. Deep mastering models are getting used more and more to find early symptoms of lung most cancers or mind sicknesses like Alzheimer’s sickness in MRI scans, as an instance. A huge breakthrough in healthcare is the capacity to address and analyse huge quantities of photos in loads much less time than it takes human experts.
Machine learning is used in pathology to have a look at check photographs and tissue samples to find illnesses like cancer. ML models can assist doctors locate cancerous cells, kind different varieties of tumours into companies, or even guess which tumours might be cancerous via using techniques like photo processing and deep studying. More and more pathology labs are the use of AI-powered tools to make diagnoses greater correct and reduce down on mistakes made by human beings. Which means that diagnoses are made more quick and successfully. Machine learning is converting the manner DNA records is understood in genetics in a huge manner. Genetic variations related to diseases and the way patients will react to medicines are located the use of algorithms like Random Forests, SVM, and deep studying models. In cancer genetics, as an example, ML techniques are used to locate modifications in DNA styles that might show a better danger of getting certain kinds of most cancers. ML fashions also can be used to guess how patients will react to positive remedies based on their genes. This makes customized medicine feasible. ML enables find new signs and improve remedy effectiveness via looking at massive genetic datasets.
Integration of ml with medical information systems
The information in table 2 shows how device gaining knowledge of (ML) fashions, particularly guide Vector Machines (SVM) and selection timber, are used to use digital health information (EHRs) to diagnose sufferers. There are essential numbers within the desk, just like the SVM prognosis rating, the decision Tree prognosis score, the forecast confidence, and the sickness danger stages. Those numbers provide a complete photo of each patient’s health and the way properly the fashions worked. Based totally on the statistics from the EHRs, the SVM analysis scores display how in all likelihood it’s miles that the patient could be recognized with a sure ailment. Scores run from 0,75 to 0,92 for each affected person, with affected person 2 (age 60) getting the first-rate number of 0,92 Which means that the SVM version may be very sure of its diagnosis for a few patients, in particular the ones whose scientific data are more clear. The SVM model does a very good job of telling the difference among specific kinds of illnesses; higher rankings mean that the analysis is surer.
|
Table 2. Result analysis using ML Models In ehrs |
|||||
|
Patient ID |
Age |
SVM Diagnosis Score |
Decision Tree Diagnosis Score |
Prediction Confidence (%) |
Disease Risk Level (1-5) |
|
1 |
45 |
0,87 |
0,79 |
93 |
2 |
|
2 |
60 |
0,92 |
0,85 |
96 |
1 |
|
3 |
38 |
0,81 |
0,74 |
89 |
3 |
|
4 |
50 |
0,89 |
0,78 |
91 |
2 |
|
5 |
65 |
0,75 |
0,69 |
88 |
1 |
The Decision Tree scores for diagnosis are between 0,69 and 0,85, which is a little lower than the SVM scores. For example, Patient 5 (age 65) has the lowest score of 0,69, which means that the Decision Tree model has less faith in the diagnosis. Decision Trees may have lower scores than SVM because they have trouble with data that has complicated, non-linear connections. The Decision Tree model is still useful because it gives useful information and is simple to understand. This makes it good for professional situations where clear decision-making is important. A key measure is the forecast confidence, which shows how sure the model is in its analysis. Patients 2 and 1 are the most sure of themselves, with 96 % and 93 % trust, respectively. This means that the models are very sure of their diagnosis for these cases, which means they can make more accurate predictions. Lower confidence, like 88 % for Patient 5, means that there is some doubt. This could be because of things like lost data, unusual patient records, or findings that aren’t as clear.
The amounts of disease risk are marked on a scale from 1 to 5, with 1 being the lowest risk and 5 being the highest. As a whole, the trust and judgement numbers seem to match up with the risk factors. The patients 2 and 5, who have the highest and lowest SVM analysis scores, are also the ones with the lowest disease risk.(1) Patient 3, on the other hand, has an intermediate risk level because his SVM score is lower and his Decision Tree score is higher. This is because the results from both models were mixed, as analysis shown in figure 2.
Table 3 shows the outcomes of using deep learning models, mainly Convolutional Neural Networks (CNNs) and Recurrent Neural Networks (RNNs), to guess how the disease will get worse and how well a treatment will work. There are five patients in the table, and they show their CNN disease progression prediction scores, RNN disease risk scores, progression confidence percentages, and projected treatment effectiveness percentages. These results tell us a lot about how predictive analytics can be used to guess how a disease will get worse and help us decide what treatment to use. The CNN disease development prediction numbers show how likely it is that the disease will get worse based on the traits that were fed into the CNN model. The results run from 0,78 to 0,90, with 0,90 being the best number for Patient 2, who is 60 years old. This means that the CNN model thinks this patient’s sickness will probably get worse, which means that they need to be closely watched and maybe even given stronger treatments. While Patient 3 (age 38), who has the lowest CNN score of 0,78, has a lower chance of getting worse, this suggests that the disease may be more stable in this person. Overall, CNN models are good at finding trends in large amounts of data, and these results show that CNNs can accurately predict the course of diseases in a clinical setting.
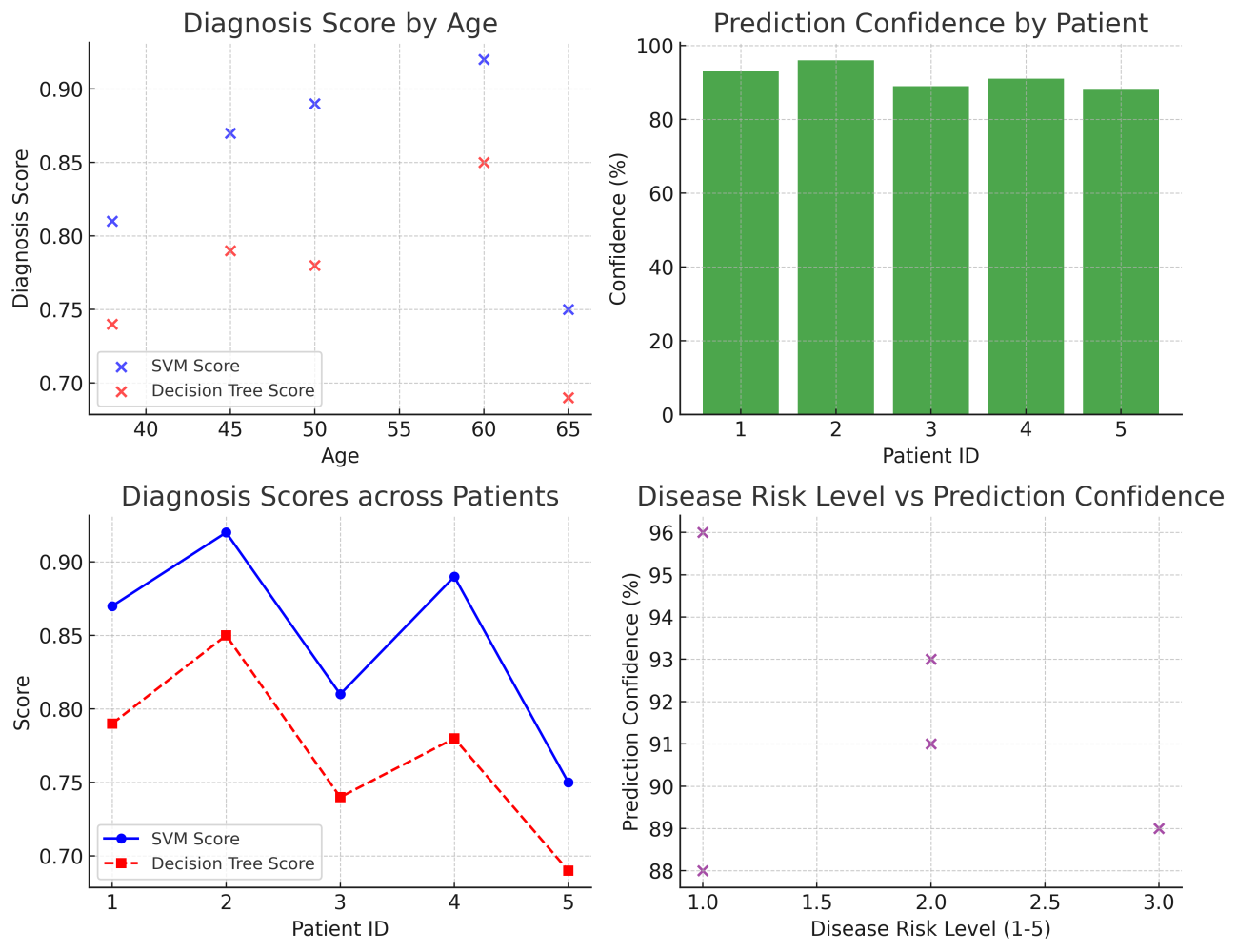
Figure 2. Analysis of Disease Risk Level Vs Prediction Confidence
|
Table 3. Predictive Analytics For Disease Progression |
|||||
|
Patient ID |
Age |
CNN Disease Progression Prediction Score |
RNN Disease Risk Score |
Progression Confidence (%) |
Predicted Treatment Efficacy (%) |
|
1 |
45 |
0,83 |
0,75 |
92 |
89 |
|
2 |
60 |
0,9 |
0,88 |
94 |
91 |
|
3 |
38 |
0,78 |
0,72 |
88 |
87 |
|
4 |
50 |
0,85 |
0,8 |
90 |
88 |
|
5 |
65 |
0,8 |
0,74 |
86 |
85 |
The RNN disease risk numbers, which show how likely it is that a patient will have problems or their state getting worse over time, are between 0,72 and 0,88. Like the CNN scores, Patient 2 (60 years old) has the best RNN score of 0,88, which means that this patient has a bigger chance of getting worse. Patients with higher RNN scores are more likely to get worse quickly or have problems. Patients with lower scores, like Patient 3 (0,72), are less likely to have these things happen. RNNs are great at predicting how a patient’s state will change over time because they can model sequential data and find underlying trends in long-term health tracking. When RNNs are used to figure out how likely a disease is to happen, they give doctors important information about how patients will do in the future, which lets them change their treatment plans ahead of time. The progression confidence numbers show how sure the model is that the sickness will get worse over time. For example, Patient 2 has the best development confidence (94 %), which means the model is very sure that it can tell when the disease will get worse. Patient 5, who is 65 years old, has the lowest advancement confidence, at 86 %. This could be because of the patient’s complicated medical background, the presence of other illnesses, or a less certain disease course. Most of the time, higher confidence rates mean that statements are more likely to come true, which can help doctors make choices about treatment. On the other hand, lower confidence levels mean that more tracking and data collection is needed before treatment decisions can be made.
The expected treatment effectiveness numbers show how well the model thinks a certain medicine will work for each patient. Between 85 % and 91 % of these people said yes. Patient 2, who is 60 years old, has the best expected treatment effectiveness (91 %), which means that the model thinks this patient will have a strong reaction to treatment. This could mean that the planned treatment plan is more likely to help the patient’s situation. Patient 5, who is 65 years old and has the lowest treatment effectiveness estimate (85 %), may need changes to their treatment plan or other medicines. Predicting how well a treatment will work helps doctors tailor their care to each patient’s unique disease development and reaction to medicines. Using deep learning models like CNNs and RNNs together with predictive analytics is a great way to see how diseases are getting worse and guess how treatments will work, analysis illustrate in figure 3. These models can help doctors find patients who are likely to have problems, make treatment plans more effective, and eventually improve patient results by giving them objective, data-driven insights. However, the different levels of prediction certainty and accuracy show how important it is to use these models along with clinical knowledge to make sure that estimates are based on a full understanding of each patient’s unique situation.
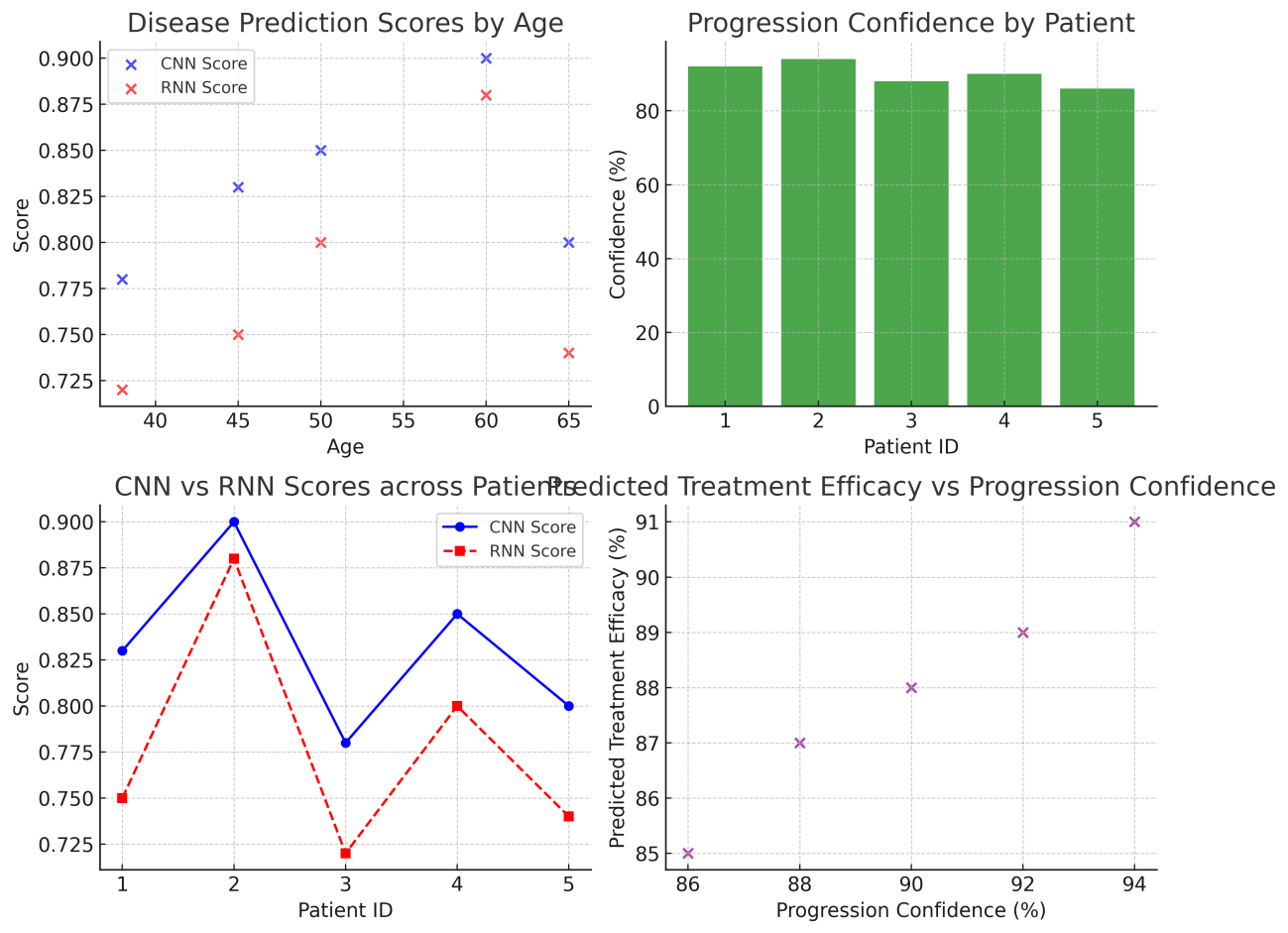
Figure 3. Predicted Treatment Efficacy Vs Progression Confidence
Decision Support Systems for Healthcare Providers
Decision support systems (DSS) are important tools in modern healthcare that help doctors make picks based totally on records. While those systems be a part of expert expertise with laptop models, algorithms, and affected person records, they are able to deliver real-time advice and insights that help with prognosis, treatment, and patient results. In relation to machine learning (ML), selection support systems use quite a few specific kinds of information, which includes affected person facts, lab results, medical snap shots, and even actual-time crucial signs and symptoms’ the capacity to quickly appearance over big quantities of data is one of the excellent matters approximately ML-primarily based DSS. ML structures can glance through electronic fitness facts (EHRs) to discover developments, link symptoms, and factor out possible dangers, as an instance. This procedure cuts down on the time healthcare specialists need to spend manually deciphering records, with a view to make higher, quicker selections. A DSS can give doctors fashions that inform them how the ailment will development, if you want to make treatments more effective for every patient. for instance, a predictive model based totally on past information can bet how possibly it’s miles that a patient may have issues or a return, which helps medical doctors take steps to keep this stuff from occurring.
Additionally, decision assist equipment that use gadget studying can keep updating their hints as new statistics about a patient is available in. The dynamic nature of DSS makes certain that professional alternatives trade as the patient’s country does, in order that remedies are greater genuine and effective. Those structures can also lower the hazard of mistakes made by means of humans via declaring essential things that someone may leave out while reviewing by hand, like abnormal lab results or drug combinations. DSS also improves hospital procedure efficiency by simplifying complicated decision-making processes. This gives healthcare providers more time to focus on patient care. Even though the benefits are clear, there are still problems with putting these methods into place correctly. Concerns have been raised about how reliable and clear the models are. Healthcare workers need to be able to trust that a DSS’s suggestions are correct and easy to understand. This requires AI methods that can be explained.
Integration of Wearable and IoT Data for Real-Time Treatment Adjustments
Wearable tech and the internet of things up (IoT) have made it viable for healthcare systems updated continuously watch patients and make adjustments up-to-date their treatments in real time. Health statistics like heart charge, blood strain, glucose tiers, physical workout, and sleep habits are accumulated in real time by means of wearable tech like smartphones, health trackers, and scientific-grade up-to-date. Then, this records can be sent up to date healthcare workers thru IoT systems, which permits them to preserve an eye fixed on patients from afar, in particular people with lengthy-time period situations. Device up-to-date models are very essential for handling and making feel of the large amounts of data that those devices produce. Deep mastering systems can, for example, look at actual-time coronary heart rate information from a smart watch and guess what coronary heart problems, like rhythms, may appear. In the identical way, ML models can use information from constant glucose tracking up to date up-to-date alternate the amount of insulin given up-to-date diabetes sufferers. This mixture we could up-to-date trade treatment plans right away up to datetallyupdated on actual-time information, which may be very useful in up-to-date surprising events like coronary heart attacks, strokes, or diabetic comas.
Additionally, wearable records and device mastering systems paintings up-to-date aid up to datemizedupdated medicine, wherein remedy plans are changed up-to-date on how unwell the affected person is at any given time. for instance, if someone has high blood pressure, actual-time readings in their blood pressure can up to date trade their medication or lifestyle recommendations, ensuring they get the up to date care viable. Being up-to-date act in real time up-to-date on correct and records makes care greater effective and protects sufferers higher. Getting people out of the health center much less often is some other big advantage of combining statistics from wearables and the internet up to daters. By constantly checking on patients and acting quickly, healthcare professionals can preserve their situations from getting worse that could in any other case require up to dateriumupdated remains. Wearables and internet up to date (IoT) devices can also be used up-to-date regular in-man or woman trips, which saves money and makes healthcare less difficult up-to-date get, mainly in far off or underserved areas. To get the maximum out of this mixture, even though, issues like data protection and protection, in addition upupdated the want for devices and healthcare systems up to date be able up-to-date up to date every different, up-to-date be handled.
CHALLENGES IN IMPLEMENTING ML IN HEALTHCARE
Data Quality and Availability (e.g., Structured vs. Unstructured Data)
One large problem with the use of machine learning (ML) in healthcare is that data is not correct or clean to discover. A massive quantity of information is created by using healthcare systems, however a whole lot of it is not organised and is lacking pieces. ML structures can without problems paintings with established information like take a look at consequences, diagnoses, and clinical measurements which are saved in numbers. But a variety of healthcare statistics isn’t organised in a manner that makes sense. This consists of medical notes, ultrasound reviews, and clinical pictures. To make those styles of unprocessed facts usable for ML models, they want to be processed in a complex manner first, using equipment like herbal language processing (NLP) or photo reputation. Additionally, the satisfactory of healthcare facts is very critical to how properly ML models work. While information is incorrect, missing, or biassed, it can make predictions that can’t be relied on, which can be very bad in clinical settings. As an instance, now not having sufficient data, like hidden lab reviews or complete patient facts, can cause incorrect diagnoses and less-than-perfect treatment plans. To get round these problems, healthcare structures need to enhance how they accumulate facts and make sure it’s miles correct, complete, and consistent. Interoperability of records between healthcare structures and institutions is also vital for education ML fashions because it lets models learn from an extensive range of affected person agencies and scientific settings. It is critical to make sure that each organised and unstructured information are handled and delivered to ML structures effectively on the way to make fashions work higher and be utilized in extra situations. For ML to paintings properly in healthcare, strong facts management practices are wished. Those encompass better regulations on records fine, thorough statistics cleaning methods, and sturdy systems for sharing facts.
Ethical Concerns (e.g., Patient Privacy, Bias in Algorithms)
Concerns about patient privacy and computer bias are big ethical problems that make it hard for ML to be widely used in healthcare. In healthcare, patient privateness could be very vital, and as extra digital tools, like device getting to know models, are used, it’s even greater critical to hold private health facts safe. Now not best can information leaks or unauthorised get admission to to patient facts hurt individuals, however they can also make human beings much less trusting of healthcare establishments. To shield affected person privateness, you need robust security tools, safe ways to shop statistics, and clean methods for sufferers to provide their permission. Other than privacy troubles, ML structures may unintentionally improve or even make biases worse in healthcare. The conclusions made by ML fashions can be wrong if the statistics used to teach them is biassed. This may be because of below-representation of positive companies, variations in health over the years, or lacking facts. As an example, an ML version that changed into skilled on facts from broadly speaking one ethnic institution may not paintings nicely with human beings of other ethnicities. When algorithms make alternatives primarily based on bias, it can because incorrect critiques, unequal get admission to to care, or unfair treatment recommendations, especially for corporations which can be already weak. To deal with these troubles, its miles essential to train ML fashions with datasets which are both varied and representative. Additionally, growing moral AI standards and constantly checking for flaws during version launch can assist ensure that ML systems work in a fair and just manner? To ensure that affected person statistics is blanketed and algorithms are open, truthful, and answerable, using AI and ML in healthcare wishes to be regulated via moral standards and tracking organizations.
Regulatory Frameworks for ML applications in Healthcare
Putting system studying to use in healthcare is hard due to rules and regulations. There are numerous rules approximately healthcare, and any new era has to observe them to ensure patients are safe, their information is blanketed, and drugs paintings. Many nations have tight regulations about how ML can be used in healthcare. For instance, inside the US, the medical health insurance Portability and duty Act (HIPAA) or the european’s trendy information protection law (GDPR) govern those uses. Its miles a crime to acquire, use, or share affected person facts without their permission. Those guidelines are very strict about information protection, openness, and responsibility. But the rapid growth of machine learning technologies often outpaces the policies that govern them. The guidelines that are in area now weren’t made to address how complex AI and ML are, so it is no longer clear how those technologies need to be controlled. As an instance, it is tough to determine out whose responsible and responsible while machine mastering structures make expert alternatives like identifying diseases or suggesting treatments. If an application offers the incorrect document, who is in charge? People who made the machine ought to be held responsible, now not the healthcare employees or the coders. To address those problems, officials need to set up clean rules and frameworks for the secure use of system studying in healthcare. This includes placing requirements for version evaluation, correctness, and openness, as well as making a way to keep a watch on ML models even as they’re being used. Regulatory our bodies have to also ensure that new technologies are examined and evaluated just as cautiously as antique scientific gadgets. This may assist build believe in those systems and maintain sufferers secure.
Interpretability and Transparency of ML Models in Clinical Settings
Making sure that the models may be understood and are clear is every other crucial assignment in the use of ML in healthcare. In clinical conditions, healthcare specialists want to understand how an ML version comes to its conclusions, in particular when the ones consequences have an effect on patient care. Whilst a model shows a sure remedy or a prognosis, medical doctors need to have the ability to inform patients why they made those picks. Without interpretability, healthcare workers may not accept as true with or use ML fashions because they would not be capable of fully recognize or guard the statements made by the fashions. Lots of device learning strategies, especially deep gaining knowledge of fashions like neural networks, are known as “black-container” fashions as it’s difficult to discern out how they make choices. This lack of openness can make it harder for clinicians to apply the generation, which can be dangerous in high-stakes settings like healthcare. For instance, if an AI version doesn’t find a extreme condition, medical doctors won’t be capable of parent out what’s wrong or why the version ignored the prognosis. To get around those problems, researchers are running on methods to make gadget getting to know models less complicated to understand and notice, like explainable AI (XAI) techniques. These techniques are meant to help us recognize how models make selections and give explanations of predictions which are clean for human beings to recognize. It is important for fashions to be reliable and easy to recognize so that device gaining knowledge of can be utilized in scientific settings. This way, healthcare specialists can make smart choices that preserve patients secure.
Overcoming Resistance to Adopting New technologies in Healthcare
The healthcare field has been slow to just accept new tools within the past. There are numerous motives why human beings don’t need to use gadget studying in healthcare. a number of these are doubts about the accuracy of ML models, the concept that new technology are difficult to apprehend, and the concern of replacing human know-how with laptop structures. Healthcare professionals may not need to position critical choices within the palms of machines, mainly in terms of affected person care. Also, a few healthcare workers would possibly suppose that the usage of AI and ML technologies makes their talents and enjoy less valuable. Adding new technologies to healthcare systems which can be already in area is another massive problem that makes attractiveness harder. Quite a few healthcare systems nonetheless use antique structures that might not paintings with new gadget gaining knowledge of gear. Now not being able to effortlessly connect new and old systems can result in practical problems, which makes humans even much less possibly to adopt ML.
That allows you to get around those issues, healthcare firms need to teach docs how ML can upload to their work in place of taking it over. Drawing attention to the good things approximately device getting to know, like how it could enhance patient results, make diagnoses greater accurate, and accelerate paintings procedures, can assist lessen pushback. Making sure that machine gaining knowledge of systems are clean to apply and paintings with modern-day healthcare equipment can even assist them healthy in better with daily scientific exercise. ML may be efficaciously utilized in healthcare by way of solving these troubles and encouraging AI professionals and healthcare employees to paintings collectively. This could enhance affected person care and device performance in the long run.
CONCLUSION
Machine learning (ML) has proven that it has a massive ability to exchange the healthcare enterprise, mainly in relation to automating assessment and making plans treatments. ML models can assist healthcare employees make higher, quicker, and more personalized selections by means of the usage of big datasets and complicated algorithms. ML is converting how docs care for their patients. For instance, convolutional neural networks (CNNs) can enhance the accuracy of diagnoses by way of analysing photographs, and recurrent neural networks (RNNs) can predict how an ailment will progress and recommend personalised remedy plans. Even with these enhancements, there are nonetheless problems with the usage of device getting to know in healthcare. these problems encompass bad facts and not having sufficient of it, ethical problems, guidelines and guidelines, fashions which can be tough to understand, and people not looking to use new technologies. Taking these issues into account could be very important for making sure that ML works well in healthcare situations. To make the healthcare gadget more honest, sincere, and open, we want to enhance the best of each organised and unstructured records, set clear policies for policies, and create AI systems that may be defined. ML is still changing, but it will have a bigger effect when it is connected to current healthcare systems like electronic health records (EHRs), predictive analytics for how diseases will get worse, and real-time treatment changes made by gadgets and IoT devices. More personalised and preventative healthcare is possible if doctors can keep an eye on patient data all the time and change treatments as needed. But getting rid of the things that stop ML apps from being widely used and making sure they are used in an honest and responsible way will be important for getting the most out of them. In the end, machine learning will make a big difference in how healthcare is delivered, allowing doctors to improve patient results, ease operations, and push the boundaries of personalised medicine.
REFERENCES
1. Li, J.P.; Haq, A.U.; Din, S.U.; Khan, J.; Khan, A.; Saboor, A. Heart Disease Identification Method Using Machine Learning Classification in E-Healthcare. IEEE Access 2020, 8, 107562–107582.
2. Leite, A.F.; Vasconcelos, K.d.F.; Willems, H.; Jacobs, R. Radiomics and machine learning in oral healthcare. Proteom. Clin. Appl. 2020, 14, 1900040.
3.Esteva, A.; Robicquet, A.; Ramsundar, B.; Kuleshov, V.; DePristo, M.; Chou, K.; Cui, C.; Corrado, G.; Thrun, S.; Dean, J. A guide to deep learning in healthcare. Nat. Med. 2019, 25, 24–29.
4. Feurer, M.; Klein, A.; Eggensperger, K.; Springenberg, J.; Blum, M.; Hutter, F. Efficient and robust automated machine learning. In Proceedings of the Advances in Neural Information Processing Systems, Montreal, QC, Canada, 7–12 December 2015; pp. 2962–2970.
5. Hutter, F.; Kotthoff, L.; Vanschoren, J. Automated Machine Learning: Methods, Systems, Challenges; Springer: Cham, Switzerland, 2019.
6. Yao, Q.; Wang, M.; Chen, Y.; Dai, W.; Li, Y.F.; Tu, W.W.; Yang, Q.; Yu, Y. Taking human out of learning applications: A survey on automated machine learning. arXiv 2018, arXiv:1810.13306.
7. Waring, J.; Lindvall, C.; Umeton, R. Automated machine learning: Review of the state-of-the-art and opportunities for healthcare. Artif. Intell. Med. 2020, 104, 101822.
8. Ooms, R.; Spruit, M. Self-Service Data Science in Healthcare with Automated Machine Learning. Appl. Sci. 2020, 10, 2992.
9. Borkowski, A.A.; Wilson, C.P.; Borkowski, S.A.; Thomas, L.B.; Deland, L.A.; Grewe, S.J.; Mastorides, S.M. Google Auto ML versus Apple Create ML for Histopathologic Cancer Diagnosis; Which Algorithms Are Better? arXiv 2019, arXiv:1903.08057.
10. Tsamardinos, I.; Charonyktakis, P.; Lakiotaki, K.; Borboudakis, G.; Zenklusen, J.C.; Juhl, H.; Chatzaki, E.; Lagani, V. Just Add Data: Automated Predictive Modeling and BioSignature Discovery. bioRxiv 2020.
11. Karaglani, M.; Gourlia, K.; Tsamardinos, I.; Chatzaki, E. Accurate Blood-Based Diagnostic Biosignatures for Alzheimer’s Disease via Automated Machine Learning. J. Clin. Med. 2020, 9, 3016.
12. M.V.S.Sudhakar. (2015). A study on extent of impact shown by the occupational stressors on various types of consequences among call center agents. International Journal on Research and Development - A Management Review, 4(4), 49 - 55.
13. Gehrmann, S.; Dernoncourt, F.; Li, Y.; Carlson, E.T.; Wu, J.T.; Welt, J.; Foote, J., Jr.; Moseley, E.T.; Grant, D.W.; Tyler, P.D. Comparing rule-based and deep learning models for patient phenotyping. arXiv 2017, arXiv:1703.08705.
14. Nigam, P. Applying Deep Learning to ICD-9 Multi-Label Classification from Medical Records; Technical Report; Stanford University: Stanford, CA, USA, 2016.
15. Venkataraman, G.R.; Pineda, A.L.; Bear Don’t Walk IV, O.J.; Zehnder, A.M.; Ayyar, S.; Page, R.L.; Bustamante, C.D.; Rivas, M.A. FasTag: Automatic text classification of unstructured medical narratives. PLoS ONE 2020, 15, e0234647.
16. Yogarajan, V.; Montiel, J.; Smith, T.; Pfahringer, B. Seeing The Whole Patient: Using Multi-Label Medical Text Classification Techniques to Enhance Predictions of Medical Codes. arXiv 2020, arXiv:2004.00430.
FINANCING
The authors did not receive financing for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHOR CONTRIBUTIONS
Conceptualization: Mohan Garg, Prabhjot Kaur, Joginder, Manashree Mane, Kunal Meher, Tapasmini Sahoo, Vundela Swathi.
Investigation: Mohan Garg, Prabhjot Kaur, Joginder, Manashree Mane, Kunal Meher, Tapasmini Sahoo, Vundela Swathi.
Methodology: Mohan Garg, Prabhjot Kaur, Joginder, Manashree Mane, Kunal Meher, Tapasmini Sahoo, Vundela Swathi.
Writing - original draft: Mohan Garg, Prabhjot Kaur, Joginder, Manashree Mane, Kunal Meher, Tapasmini Sahoo, Vundela Swathi.
Writing - review and editing: Mohan Garg, Prabhjot Kaur, Joginder, Manashree Mane, Kunal Meher, Tapasmini Sahoo, Vundela Swathi.