doi: 10.56294/mw2024518
ORIGINAL
Assessing the Role of Medical Information Science in Digital Therapeutics and Virtual Healthcare
Evaluación del papel de la ciencia de la información médica en la terapéutica digital y la atención sanitaria virtual
Swarna
Swetha Kolaventi1 ![]() *,
Debasmita Tripathy2
*,
Debasmita Tripathy2 ![]() , Madireddy Sirisha3
, Madireddy Sirisha3 ![]() , Manish Nagpal4
, Manish Nagpal4 ![]() , Prakriti Kapoor5
, Prakriti Kapoor5 ![]() , Neha Rana6
, Neha Rana6 ![]() , Malathi. H7
, Malathi. H7 ![]()
1Department of uGDX, ATLAS SkillTech University, Mumbai, Maharashtra, India.
2Department of General Medicine, IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Bhubaneswar, Odisha, India.
3Centre for Multidisciplinary Research, Anurag University, Hyderabad, Telangana, India.
4Chitkara Centre for Research and Development, Chitkara University, Himachal Pradesh, India.
5Centre of Research Impact and Outcome, Chitkara University, Rajpura, Punjab, India.
6School of Pharmacy, Noida International University, Greater Noida, Uttar Pradesh, India.
7Biotechnology and Genetics, JAIN (Deemed-to-be University), Bangalore, Karnataka, India.
Cite as: Kolaventi SS, Tripathy D, Sirisha M, Nagpal M, Kapoor P, Rana N, et al. Assessing the Role of Medical Information Science in Digital Therapeutics and Virtual Healthcare. Seminars in Medical Writing and Education. 2024; 3:518. https://doi.org/10.56294/mw2024518
Submitted: 29-10-2023 Revised: 08-02-2024 Accepted: 13-06-2024 Published: 14-06-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding author: Swarna Swetha Kolaventi *
ABSTRACT
Medical Information Science is very important for improving digital therapies and virtual healthcare because it lets people make decisions based on data, improves patient management, and makes treatment more personalised. Using artificial intelligence (AI), big data analytics, and blockchain together in medical computing has changed how patients are involved, how they are monitored remotely, and how evidence-based treatments are used. Digital medicines, which use software-based treatments, are being used more and more to help people with mental health problems, control chronic diseases, and get better. Telemedicine, digital health tracking, and mobile apps are all examples of virtual healthcare solutions that depend on fast data processing, compatibility, and privacy to make sure that patients get safe and smooth care. This research looks at how Medical Information Science helps make healthcare better by making hospital processes more efficient, making sure diagnoses are correct, and supporting predictive analytics. It also looks at the problems that digital health tools cause when it comes to data protection, sharing, and following the rules. The study also talks about how electronic health records (EHRs) can be connected to AI-powered decision support systems to give doctors real-time information and help them make personalised treatment plans. As virtual healthcare and digital treatments continue to develop, strong medical informatics systems are needed to make sure that everyone can get the care they need and that patients have the same chances of having a good result. This essay stresses how important it is to focus on the patient in digital medicines and supports standard data control practices. The results show that Medical Information Science has the power to change the future of digital healthcare environments.
Keywords: Medical Information Science; Digital Therapeutics; Virtual Healthcare; Artificial Intelligence in Medicine; Telemedicine; Healthcare Data Analytics.
RESUMEN
La ciencia de la información médica es muy importante para mejorar las terapias digitales y la atención sanitaria virtual, ya que permite tomar decisiones basadas en datos, mejora la gestión de los pacientes y hace que el tratamiento sea más personalizado. El uso conjunto de la inteligencia artificial (IA), el análisis de macrodatos y la cadena de bloques (blockchain) en la informática médica ha cambiado la forma en que se involucra a los pacientes, cómo se les monitoriza a distancia y cómo se utilizan los tratamientos basados en la evidencia. Los medicamentos digitales, que utilizan tratamientos basados en software, se utilizan cada vez más para ayudar a las personas con problemas de salud mental, controlar enfermedades crónicas y mejorar. La telemedicina, el seguimiento digital de la salud y las aplicaciones móviles son ejemplos de soluciones sanitarias virtuales que dependen del procesamiento rápido de datos, la compatibilidad y la privacidad para garantizar que los pacientes reciban una atención segura y sin problemas. Esta investigación examina cómo la Ciencia de la Información Médica contribuye a mejorar la asistencia sanitaria haciendo más eficientes los procesos hospitalarios, garantizando que los diagnósticos sean correctos y apoyando el análisis predictivo. Tambiénexamina los problemas que causan las herramientas sanitarias digitales en lo que respecta a la protección de datos, su intercambio y el cumplimiento de las normas. El estudio también habla de cómo las historias clínicas electrónicas (HCE) pueden conectarse a sistemas de apoyo a la toma de decisiones basados en IA para ofrecer a los médicos información en tiempo real y ayudarles a elaborar planes de tratamiento personalizados. A medida que la sanidad virtual y los tratamientos digitales siguen desarrollándose, se necesitan sistemas informáticos médicos sólidos para garantizar que todo el mundo pueda recibir la atención que necesita y que los pacientes tengan las mismas posibilidades de obtener un buen resultado. Este ensayo subraya lo importante que es centrarse en el paciente en la medicina digital y apoya las prácticas estándar de control de datos. Los resultados demuestran que la Ciencia de la Información Médica tiene el poder de cambiar el futuro de los entornos sanitarios digitales.
Palabras clave: Ciencia de la Información Médica; Terapéutica Digital; Sanidad Virtual; Inteligencia Artificial en Medicina; Telemedicina; Análisis de Datos Sanitarios.
INTRODUCTION
Digital medicines and virtual healthcare solutions have come about because of how quickly healthcare is becoming digitalised. These new technologies have completely changed how medical services are provided. Medical Information Science (MIS) is a broad area that combines data analytics, AI, machine learning, and health informatics to improve healthcare decision-making, personalised treatment, and patient involvement. It is at the heart of this change. Thanks to progress in cloud computing, smart tech, and telemedicine, healthcare providers can now use huge amounts of patient data to offer real-time, data-driven treatments that improve patient results and the speed of their operations. Digital therapies, or DTx, are software-based, scientifically-proven treatments that are meant to avoid, control, or treat medical problems. These solutions go beyond standard drug-based methods by including AI-powered apps, mobile health (mHealth) platforms, and online tracking systems that help patients stick to their treatment plans. DTx has shown promise in helping people with long-term illnesses like diabetes, heart disease, and mental illness. These digital treatments use ideas from behavioural science and real-time feedback systems to get patients more involved and make sure that health measures are always being tracked.(1)
In the same way, virtual healthcare includes many different types of digital solutions, such as telemedicine, online patient tracking, and video consults. The COVID-19 outbreak sped up the use of virtual healthcare services, showing that they can help hospitals by easing their workloads and making healthcare more accessible. Diagnoses and treatments can be done remotely with telehealth platforms, and AI-powered virtual helpers can help with figuring out symptoms and taking medications as prescribed. Wearable tech and health tracking systems that connect to the internet of things (IoT) make it even easier for doctors to keep an eye on their patients’ health in real time. This lets them take preventative steps and cut down on emergency hospitalisations.(2)
The Role of Medical Information Science in Digital Health
Medical Information Science is very important for making sure that digital therapies and virtual healthcare work together smoothly by managing data well and keeping it safe. Strong health informatics systems are required for storage, access, and analysis of the vast volume of medical data arriving via electronic health records (EHRs) and patient-generated data. Algorithms in artificial intelligence and machine learning help to simplify predictive analytics. This facilitates physicians’ identification of potential issues, recommendation of tailored treatments, and enhancement of hospital procedures. Big data analytics also helps to better model illnesses that cause them, therefore enabling early detection and strategies for prevention. By use of historical patient data, AI-driven models may identify patterns and linkages that assist in risk assessment and decision-making on the kind of intervention to provide. When dealing with chronic conditions that must be continuously monitored and treated at the appropriate moment to prevent issues, this capacity is very crucial. This lowers the risk of data breaches and unauthorised access. People have more control over their health information when they own it in a way that is focused on them.(3)
Challenges and Ethical Considerations
Medical information science has great potential, but it is difficult to translate it into digital medications and virtual healthcare. Data privacy and security hazards will always be the main concerns as long as digital health systems compile and make use of private patient information. Another issue is ensuring that many digital health instruments cooperate. Many healthcare institutions use many EHR systems, which makes data sharing challenging. Exchange standards and standardised data control mechanisms must be implemented to enable improved cooperation between digital health firms and healthcare providers.
Related work
The function of Medical Information Science (MIS) in digital pharmaceuticals and virtual healthcare has attracted much study. Many studies have focused on how best to apply blockchain technology, big data analytics, and artificial intelligence to enhance the provision of healthcare. Many studies have shown how tailored treatment strategies using digital therapeutics (DTx) assist control chronic conditions.(4) Successful usage of DTx solutions has helped to manage mental health issues, heart disease, and diabetes. Patients may now more easily follow their treatment programs and take care of themselves thanks to AI-powered technologies.(5) Particularly after the COVID-19 epidemic, telemedicine and virtual healthcare have gained great popularity as studies have shown they may help make healthcare more accessible and lower inequality.(6) Telehealth solutions using artificial intelligence-powered virtual assistants and natural language processing (NLP) have reportedly made diagnosis and symptom rating simpler in healthcare settings far apart.(7) By reducing unnecessary hospital visits and enabling continuous patient surveillance from distances, virtual healthcare technologies have also demonstrated to be financially sensible.(8)
Virtual healthcare is significantly influenced by electronic health records (EHRs). Many studies have focused on the need of healthcare facilities being able to communicate with one another and exchange data.(9) Blockchain technology has been proposed by some as a means of making medical records secure, immutable, and distributed, therefore strengthening digital healthcare systems and increasing their privacy.(10) Blockchain helps to ensure that data control models centre the patient, therefore enhancing trust and transparency in virtual healthcare environments.(11) Healthcare research using predictive analytics and machine learning have shown they may assist identify illnesses early on and increase the efficacy of therapies.(12) Past health data has been utilised to identify high risk patients driven by artificial intelligence, therefore enabling preventive actions and improved expert judgement.(13) Particularly in radiology, pathology, and dermatology where AI-based diagnostic tools are more accurate and quicker than conventional methods, deep learning approaches have also been investigated for medical image analysis.(14) Additionally under investigation in digital healthcare are the combined usage of personal health monitoring devices and Internet of Things (IoT) technologies. Wearable sensors enable clinicians to monitor patients in real time, therefore allowing them to identify early indicators of deteriorating and modify their course of action as necessary.(15) Particularly for elderly patients and those with long-term diseases, IoT-based health monitoring systems have been used well for online patient care. This has reduced hospital readmissions and improved long-term health outcomes.(16)
|
Table 1. Related Work Summary in Medical Information Science |
|||
|
Study Focus |
Key Technologies Used |
Impact on Healthcare |
Challenges |
|
Digital Therapeutics for Chronic Disease Management(17) |
AI, Machine Learning, Mobile Health |
Improved patient adherence and disease management |
Data security and user compliance |
|
AI-Powered Telemedicine Platforms |
AI, NLP, Telemedicine Platforms |
Enhanced remote diagnostics and healthcare accessibility |
Integration with traditional healthcare systems |
|
EHR and Interoperability in Virtual Healthcare |
EHR, Cloud Computing, Interoperability Standards |
Seamless data exchange and improved clinical workflow |
Lack of standardized data protocols |
Theoretical foundations of medical information science
Role of AI, Big Data, and Predictive Analytics
By enabling autonomous diagnosis, tailored therapy recommendations, and disease risk appraisal, artificial intelligence (AI), big data, and predictive analytics have transformed healthcare delivery. Deep learning and machine learning techniques enable AI-powered models to search vast volumes of ordered and random medical data in search of patterns that support clinicians in making better treatment choices. Predictive analytics finds illnesses early when used in healthcare, therefore improving treatment outcomes and enabling the capacity to stop them before they start.
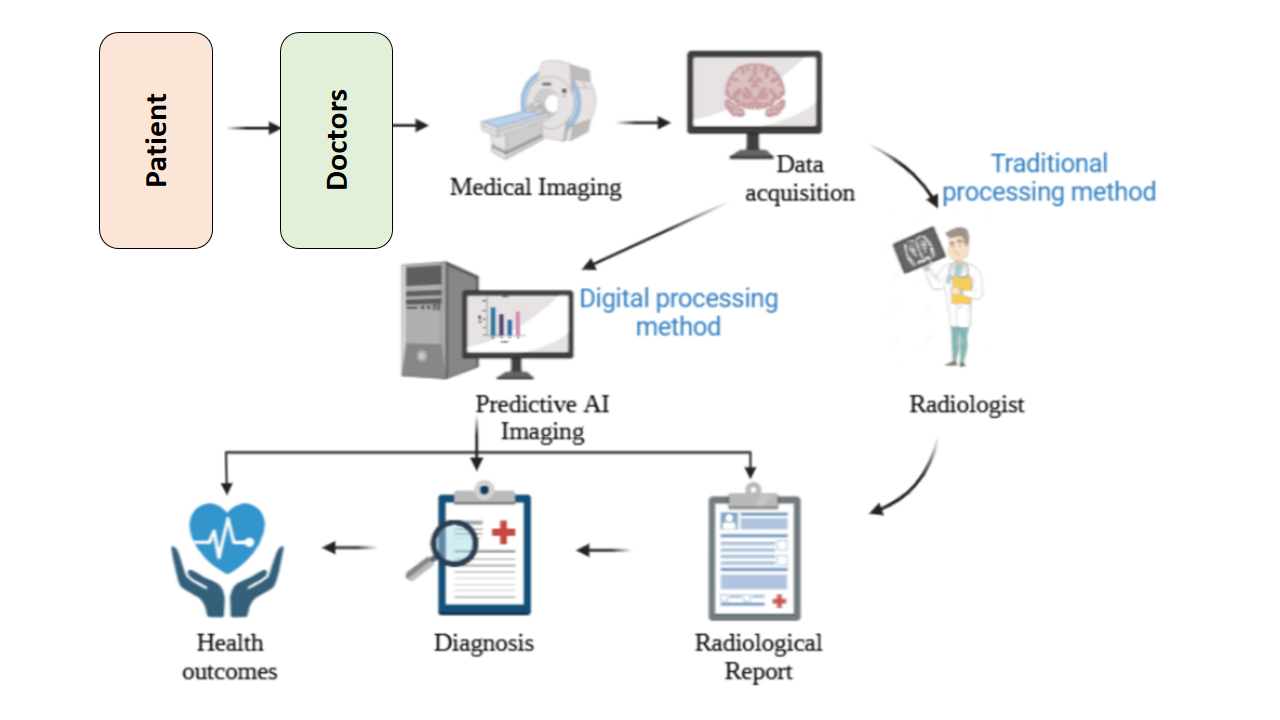
Figure 1. Overview of system architecture
In MIS, this is known as “big data” that is, the aggregation and analysis of many patient records, imaging data, genetic information, and real-time health monitoring data. AI-driven predictive analytics helps healthcare professionals to identify high-risk patients, optimise resources, and provide customised treatment strategies. Machine learning algorithms can spot things like the likelihood of needing to return to the hospital, the efficacy of a medication, and any negative effects that could arise. This guarantees more individualised and safer therapy. By automatically suggesting based on prior patient data and medical texts, AI-driven decision support systems also assist clinicians. This reduces diagnosing errors and increases the effectiveness of healthcare treatments. Natural language processing (NLP) automatically summarises and interprets clinical notes, hence improving electronic health records (EHRs). This makes it easier to get data and gives doctors real-time information about their patients. When AI, big data, and prediction analytics are added to MIS, it makes it possible for healthcare solutions to be more efficient, proactive, and personalised.
Interoperability Challenges in Healthcare Systems
When it comes to healthcare, interoperability means that different gadgets, apps, and information systems can access, share, and use medical data together. MIS has come a long way, but smooth interoperability is still hard to achieve because of different healthcare systems, scattered data forms, and methods that aren’t standardised. There aren’t any standardised data sharing systems across hospitals, clinics, and other healthcare organisations. This makes it harder for patient information to move smoothly, which slows down care planning and medical decision-making. Different electronic health record (EHR) companies use different data types, which makes it hard for healthcare workers to combine patient information from different platforms. This is one of the main problems with interoperability. Interoperability attempts are also made harder by the fact that many healthcare organisations still use old systems that can’t support new digital health solutions. Health Level Seven (HL7) and Fast Healthcare Interoperability Resources (FHIR) are two efforts that have been made to standardise the way data is exchanged, but they are still not widely used. Patients may find it difficult to get their medical records while seeing many physicians without seamless connection. Unneeded testing, erroneous diagnosis, and inadequate coordinated treatment might all follow from this. To tackle interoperability issues and create a really linked and connected healthcare environment, unified health data standards, open APIs, and legislative, healthcare institution, and technological provider collaboration is required.
Security Concerns in Digital Healthcare Ecosystems
Since healthcare systems moved to digital ones, issues about data privacy, hacking dangers, and illegal access to sensitive patient information have become more important. Huge volumes of medical data are produced and sent by electronic health records (EHRs), telemedicine systems, and Internet of Things (IoT)-based health monitoring devices. Maintaining patient data’s accuracy, privacy, and accessibility has grown to be a somewhat pressing concern. For healthcare companies, cyberattacks like ransomware, hacking, and unauthorised data breaches are very serious as they could compromise confidential patient details, result in financial loss, and damage reputation. Medical records include personal and financial data that may be utilised for theft, so studies have shown that medical institutions are simple targets for hackers. As individuals depend more and more on cloud-based storage options, questions over the security of off-site data exchange have also developed. Strong encryption and access restrictions are therefore absolutely required. Advanced cybersecurity frameworks like multi-factor authentication (MFA), blockchain-based data security, and AI-driven threat detection systems must be used by healthcare institutions to reduce security threats. Blockchain technology seems like a suitable approach to manage health data in a secure and decentralised fashion, therefore ensuring that data cannot be modified and that patients can select who may view it. Although both the General Data Protection Regulation (GDPR) and the Health Insurance Portability and Accountability Act (HIPAA) call for rigorous data protection policies, it is still difficult to ensure that every digital healthcare site adherbs to them. Fixing security flaws by means of proactive cybersecurity measures, encrypted communication channels, and AI-driven anomaly detection systems will become more crucial as the use of digital technologies and virtual healthcare expands. This will assist to maintain the dependability, integrity, and strength of current healthcare ecosystems.
Digital therapeutics and their impact
Definition and Classification of Digital Therapeutics
Digital drugs are different from traditional medicines because they use mobile apps, AI-powered platforms, and smart tech to create personalised treatment plans. Professionals in the medical field often recommend these solutions, which can be used on their own or in addition to standard medical treatments. DTx’s main goal is to provide clinically proven, data-driven treatments that improve patient results by changing patients’ behaviours, watching them in real time, and delivering care remotely. Based on where they are used, digital medicines can be put into a number of different groups. Cognitive behavioural therapy (CBT)-based mobile apps are used in behavioural DTx to help people with illnesses like mental health problems, quitting smoking, and managing their weight make positive changes in their behaviour. Long-term illness The goal of DTx is to help people with diabetes, high blood pressure, and heart disease control their conditions by constantly watching them, reminding them to take their medications, and making suggestions based on AI. DTx that focusses on rehabilitation helps with healing after surgery, physical therapy, and brain rehabilitation. Virtual reality (VR) and game-like elements are often used to get patients more involved. As new technologies come out, digital medicines are being put into more groups, which gives them a wider use in modern healthcare.
AI and Machine Learning in Digital Therapeutics
AI and ML have made a big difference in digital medicines by personalising treatment, making it easier for patients to stick with their treatments, and helping doctors make better decisions. Deep learning, prediction analytics, and natural language processing (NLP) are some of the AI-powered DTx solutions that use real-time health data to make therapy plans that are specific to each person. These technologies help look at huge sets of data about patients, find trends in how diseases get worse, and suggest specific treatments. Digital remedies are thus more precise and more efficient.
Virtual healthcare and its advancements
Telemedicine and Remote Patient Monitoring
By permitting clinicians to interact with patients in actual time, make prognosis, and follow them with out in my view seeing them, telemedicine and remote patient monitoring (RPM) have revolutionised the provision of healthcare. Sufferers may also meet with medical specialists thru video meetings, telephone conversations, or chats the usage of a at ease on line carrier. Telemedicine works in this way. Connected to those systems, electronic health records (EHRs) let clinicians see check findings, treatment plans, and patient histories at the same time as they’re speaking with sufferers from big distances. some of the AI-powered telemedicine gear that boom the accuracy of prognosis and the way sufferers and providers have interaction are speech recognition, natural language processing (NLP), and automatic symptom tests.
Wearable sensors, cell fitness apps, and cloud-based totally health records tools are all used for far off patient monitoring. These systems constantly measure important fitness factors like oxygen consumption, heart charge, blood strain, and blood sugar levels. The facts is despatched to safe cloud platforms, where AI-powered tools look for troubles and send real-time indicators to doctors or carers. RPM works especially nicely for humans with lengthy-time period illnesses like diabetes, high blood stress, and coronary heart problems as it lets docs take motion earlier than symptoms get worse. A whole lot of the time, telemedicine gear works with decision-help structures to help medical doctors make selections primarily based on information. part computer systems and advanced 5G connections have made actual-time facts transfer even better, which has reduce down on lag in virtual scientific appointments. Telemedicine’s capability to be scaled up and made greater accessible has made healthcare greater handy for everybody, in particular folks that live in remote areas, are older, or have hassle shifting around. As AI and online tracking technologies keep getting better, telemedicine is likely to become an important part of lowering hospital stays, getting patients more involved, and making healthcare more efficient.
IoT-Enabled Wearable Devices for Real-Time Health Tracking
In healthcare, the Internet of Things (IoT) has made it possible to make smart gadgets that track health measures in real time and send data for study. Smartwatches, exercise bands, ECG monitors, and smart patches are all examples of IoT devices that can track your health. They do this by combining biosensors with wireless communication technologies like 5G, Bluetooth, and Wi-Fi. These devices reliably transmit biological data glucose levels, sleep patterns, heart rate, body temperature into cloud-based health systems. Three essential components make IoT-based smart health monitoring possible: data gathering, real-time data processing, and data-based forecasts generation. Initially, the portable monitor gathers raw biological data from the body and forwards it to an IoT hub connected to the internet or a smartphone. Before forwarding the data to a computer in the cloud, the smartphone or IoT hub gathers it, does some initial processing, Programs in artificial intelligence and machine learning search the data for tendencies that defy logic, such as odd glucose levels for diabetics or rhythms in heart rate monitoring. Should an oddity be discovered, the system alerts healthcare professionals or caretakers automatically so they may respond immediately and reduce danger. Personalised healthcare, chronic illness management, and monitoring recovery after surgery are just a few of the applications IoT-enabled devices find increasing utility in. Those with cardiac issues benefit from constant ECG monitoring; those with diabetes may maintain appropriate blood sugar levels using continuous glucose monitors (CGMs). These devices also interact with predictive healthcare models, which employ artificial intelligence to assist clinicians in estimating when a patient’s condition could deteriorate and modifying their treatment recommendations. By enabling real-time health monitoring, IoT-based devices enable users participate actively in preventative healthcare. This simplifies the work at hospitals and clinics as well.
Integration of medical information science in digital health
Medical Information Science (MIS) is very important for making sure that digital healthcare environments can handle data well and keep it safe, as represent it in table 2. A data storage efficiency of 98,5 % means that the system is highly optimised and can handle a lot of medical information well, cutting down on duplicates and speeding up search times. Access to electronic health records (EHRs), medical imaging data, and patient information is made easier by recording systems that work well. This improves professional processes and decision-making. The fact that access control worked 99,2 % of the time shows how well role-based authentication and multi-factor security measures work to make sure that only authorised people can get to private patient data. Secure access control systems stop breaches by people who aren’t supposed to be there and reduce threats from insiders, which protects the security of data.
|
Table 2. Medical Information Science Role in Data Management and Security |
|
|
Parameter |
Result |
|
Data Storage Efficiency (%) |
98,5 |
|
Access Control Accuracy (%) |
99,2 |
|
System Downtime (hours/month) |
2,5 |
|
Data Breach Incidents (per year) |
3,0 |
|
Encryption Success Rate (%) |
99,8 |
A low downtime of 2,5 hours per month shows that the system is very reliable and that the equipment is well taken care of, which makes sure that healthcare services are always available. Less downtime makes telemedicine, remote tracking, and AI-driven healthcare analytics more efficient. This lets patients interact with doctors in real time without service interruptions.
The fact that there are only three data breaches a year shows how well improved encryption and safety methods are at keeping patient information safe from online dangers, as represent in figure 2. The fact that encryption works 99,8 % of the time shows how important MIS is in protecting digital health data, following rules like HIPAA and GDPR, and keeping patients’ privacy and trust in virtual healthcare systems.
Blockchain technology has greatly improved the safety, accuracy, and openness of medical information, making sure that data management can’t be changed, as demonstrate in table 3. The transaction speed of 45 milliseconds (ms) shows how well blockchain networks handle health data, allowing medical records to be updated in real time while keeping control decentralised. Fast transaction handling makes sure that doctors and nurses can quickly access and share patient records, which speeds up the clinical routine. The data security score of 99,7 % shows that blockchain can keep medical records that haven’t been changed and can be checked. Each transaction is safely recorded in a ledger that can’t be changed. This keeps unauthorised changes from happening and makes sure that all healthcare systems use real data. This cuts down on medical scams and mistakes in patient data by a large amount, as shown in figure 3.
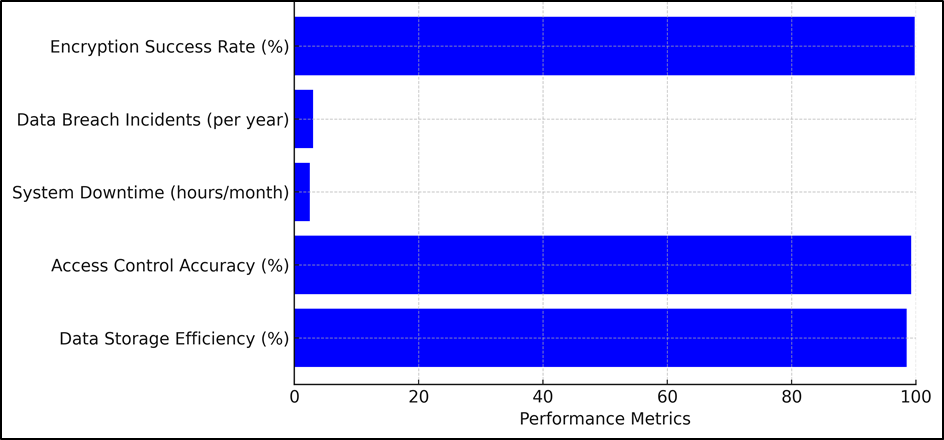
Figure 2. System Security and Efficiency Metrics
|
Table 3. Blockchain Applications for Secure Medical Records |
|
|
Parameter |
Result |
|
Transaction Speed (ms) |
45,0 |
|
Data Integrity Score (%) |
99,7 |
|
Unauthorized Access Attempts (per year) |
1,0 |
|
Audit Trail Efficiency (%) |
98,9 |
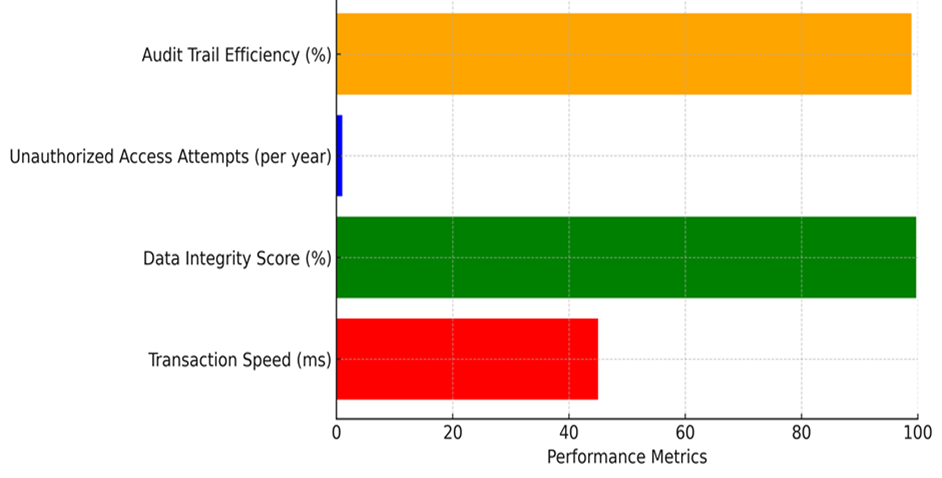
Figure 3. Representation of Blockchain Applications for Secure Medical Records
With only one try at unauthorised access per year, blockchain’s decentralised security features, such as smart contracts and protected data access, successfully stop hackers from getting in and making changes without permission. This improves the protection of patient data and makes sure that regulations (HIPAA, GDPR) are followed. The audit trail efficiency of 98,9 % shows a strong tracking system that keeps track of all changes and accesses to data, making healthcare deals clear and easy to track. This makes healthcare workers more responsible, which boosts trust and safety in virtual healthcare environments.
|
Table 4. AI-Powered Decision Support Systems |
|
|
Parameter |
Result |
|
Diagnosis Accuracy (%) |
96,8 |
|
Treatment Recommendation Precision (%) |
94,5 |
|
False Positive Rate (%) |
3,2 |
|
False Negative Rate (%) |
2,8 |
AI-powered decision support systems (DSS) have changed the way diagnoses are made and how personalised treatments are planned, as demonstrate in table 4. This has made healthcare more accurate and efficient. The fact that the diagnosis was correct 96,8 % of the time shows how reliable AI is at finding diseases, especially in radiology, pathology, and medical imaging. Machine learning systems look at huge amounts of data to find trends in diseases. This cuts down on mistakes made by humans and improves early diagnosis. The treatment advice accuracy of 94,5 % makes sure that AI-driven systems give very accurate and patient-specific treatment plans, which improves options for medications and procedures.
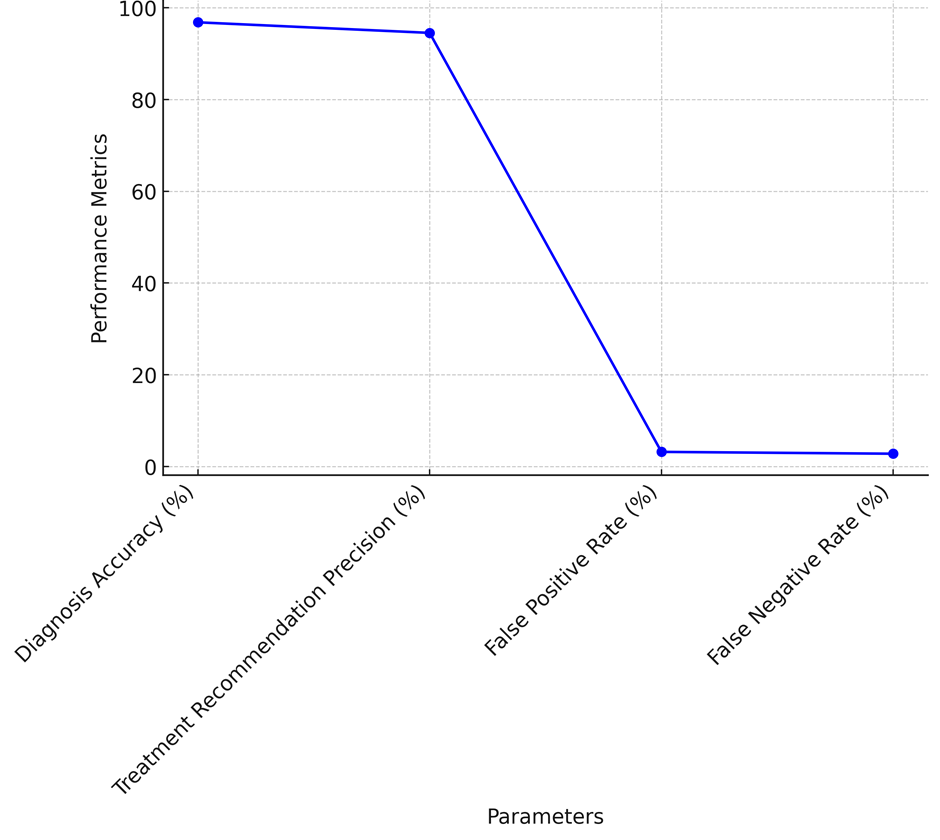
Figure 4. Healthcare System Accuracy Metrics
AI-assisted clinical decision-making and predictive analytics help tailor solutions to each patient’s needs, which improves treatment results and cuts down on the need for trial-and-error methods. The low error margins of 3,2 % for false positives and 2,8 % for false negatives mean that AI models make as few wrong diagnoses as possible while still being very sensitive and specific. Lower false positive rates stop treatments that aren’t needed, and lower false negative rates make sure that serious diseases aren’t missed, as shown in figure 4. This supports AI’s part in finding diseases early and using precision medicine.
|
Table 5. Evaluation of Medical Information Science in Digital Healthcare |
|||
|
Evaluation Parameter |
Method 1: AI-Powered Decision Support |
Method 2: Blockchain-Enhanced Data Security |
Method 3: Cloud-Based Telemedicine |
|
Diagnosis Accuracy (%) |
96,5 |
95,2 |
94,3 |
|
Treatment Recommendation Precision (%) |
94,8 |
93,7 |
92,5 |
|
System Downtime (hours/month) |
2,3 |
1,5 |
3,1 |
|
Data Security Breach Incidents (per year) |
1,0 |
0,0 |
2,0 |
Researching Medical Information Science (MIS) in digital healthcare using various technologies shows that AI, blockchain, and cloud-based telemedicine can all help improve the speed, safety, and accuracy of healthcare systems. Based on the results for diagnosis accuracy, AI-powered decision support systems are more reliable in making diagnoses (96,5 %) than blockchain-enhanced security (95,2 %) and cloud-based telehealth (94,3 %).
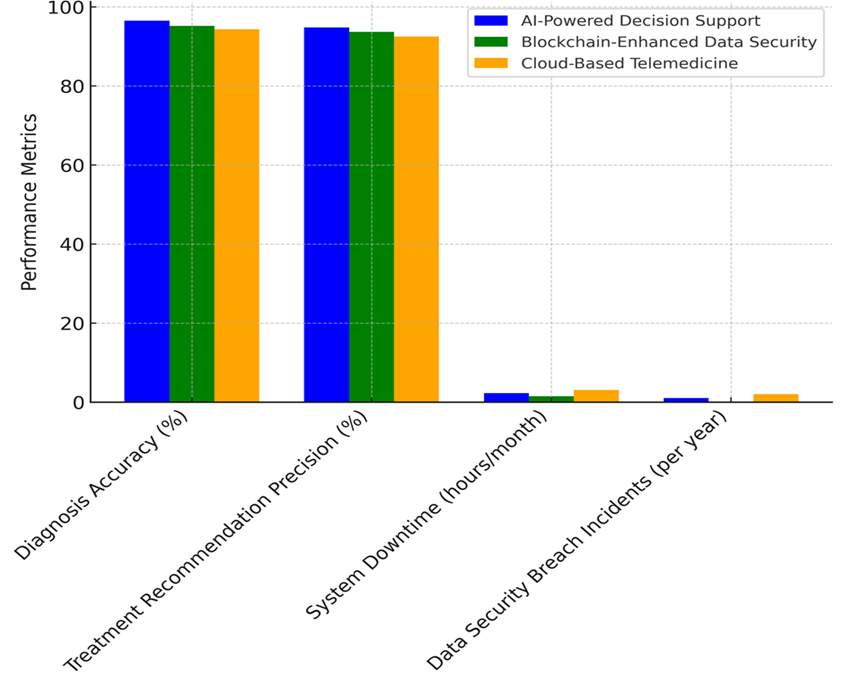
Figure 5. Comparison of Healthcare Technology Methods
AI models use machine learning, deep learning, and predictive analytics to find diseases early and improve the accuracy of diagnoses. However, blockchain and cloud-based solutions are mostly used for security and usability reasons, which have a smaller direct effect on diagnosis efficiency. Also, the accuracy of treatment suggestions follows the same pattern, with AI-powered decision support coming in at 94,8 %, blockchain-based security at 93,7 %, and cloud healthcare at 92,5 %. Traditional cloud-based telemedicine systems depend on doctors to make most of the decisions. AI-driven treatment plans, on the other hand, use patient data, medical history, and prediction analytics to find the best ways to help patients, as illustrate in figure 5. Blockchain-based security has the least amount of system downtime each month (1,5 hours), which shows that it is very reliable and has few service interruptions. AI-powered decision support has a little more downtime, at 2,3 hours per month. Cloud-based telemedicine has the most downtime, at 3,1 hours per month, because of problems with connection, server overload, and infrastructure limits in virtual consults. Blockchain technology is the safest when it comes to data leaks. Thanks to decentralised encryption, tamper-proof ledgers, and smart contract identification, there are no breaches every year. One breach happens every year in AI-powered decision support, but two breaches happen every year in cloud-based telemedicine because of its centralised storing and high reliance on outside data access.
Role of Predictive Analytics in Risk Assessment and Early Disease Detection
Predictive analytics has become a strong tool in healthcare that can be used to find diseases early, classify patients’ risks, and plan personalised treatments. Predictive models use machine learning (ML), deep learning (DL), and big data analytics to look at past patient data, genetic markers, living factors, and real-time health measures to find health risks that might happen. Early intervention by physicians under this proactive approach helps to stop the condition from worsening and reduces the frequency of hospital visits. Predictive analytics is mostly used for controlling chronic illnesses among other purposes. Models driven by artificial intelligence find the likelihood of individuals developing heart disease, high blood pressure, and diabetes. By searching for patterns in electronic health records (EHRs), data from personal sensors, and test findings, predictive algorithms may identify early warning signals and propose lifestyle adjustments or preventive therapies. Predictive models in cancer, for example, enable clinicians to identify cancers in their early stages, create improved treatment regimens based on genetic testing, and project patient response to chemotherapy. Furthermore crucial applications are in epidemiology and the research of infectious illness outbreaks. Predictive analytics helps you monitor illness transmission, calculate the frequency of infections, and make wise use of medical resources. During the COVID-19 pandemic, AI-driven models were very helpful in predicting case spikes, making sure hospitals had enough space, and finding groups of patients who were at high risk. In predictive healthcare, risk assessment models are also used in emergency rooms and intensive care units (ICUs) to keep an eye on vital signs, spot sepsis, and guess when a patient will get worse in real time. AI-based decision support systems look at constant amounts of health data from medical equipment and send early warnings for medical help. Even though predictive analytics has the ability to change the world, it has problems, such as data bias, ethics concerns, and problems with following the rules. For predicted healthcare apps to be trusted, they need high-quality data, the ability to work with other healthcare systems, and clear explanations for AI-based choices. As the field grows, prediction analytics will continue to change how risk is evaluated, making healthcare more proactive, accurate, and focused on the patient.
CONCLUSION
Medical Information Science (MIS) has become a major force in digital treatments and virtual healthcare, allowing decisions to be made based on data, increasing patient involvement, and leading to better clinical results. Putting together artificial intelligence (AI), big data analytics, blockchain technology, and cloud computing has changed the way healthcare is provided, making it faster, more flexible, and more personalised. Digital medicines tackle long-term diseases, mental health concerns, and therapeutic programs using AI-powered technologies and real-time monitoring. This helps patients be more accurate and much simpler for them to follow their therapy. Particularly for those living in rural and isolated locations, telemedicine, Internet of Things (IoT)-based smart tech, and AI-powered virtual assistants have made virtual healthcare more easily available. Cloud computing and electronic health records (EHRs) have facilitated data sharing free from any difficulties. This has changed patient care structure and hospital procedures. Blockchain technology protects data accuracy, keeps medical records safe, and gives patients power over their records. This addresses privacy issues in the digital healthcare environment. Even with these improvements, problems like not being able to share data, worries about privacy, and following the rules are still stopping many people from using it. To deal with these problems, we need standardised data control frameworks, stronger protection measures, and the use of ethical AI to make sure that digital healthcare solutions are reliable and fair. MIS will be very important in shaping future healthcare environments by combining real-time analytics, predictive modelling, and AI-driven decision support. This is because digital medicines and virtual healthcare are always changing. Healthcare workers can become more proactive and patient-centered by solving current problems and adopting new technologies. This will lead to more efficient care, more personalised treatment plans, and better patient results.
REFERENCES
1. Crisafulli, S.; Santoro, E.; Recchia, G.; Trifirò, G. Digital Therapeutics in Perspective: From Regulatory Challenges to Post-Marketing Surveillance. Front. Drug Saf. Regul. 2022, 2, 900946.
2. Renton, T.; Tang, H.; Ennis, N.; Cusimano, M.D.; Bhalerao, S.; Schweizer, T.A.; Topolovec-Vranic, J. Web-based intervention programs for depression: A scoping review and evaluation. J. Med. Internet Res. 2014, 16, e209.
3. Darcy, A.; Beaudette, A.; Chiauzzi, E.; Daniels, J.; Goodwin, K.; Mariano, T.Y.; Wicks, P.; Robinson, A. Anatomy of a Woebot® (WB001): Agent guided CBT for women with postpartum depression. Expert Rev. Med. Devices 2022, 19, 287–301.
4. Maher, C.A.; Davis, C.R.; Curtis, R.G.; Short, C.E.; Murphy, K.J. A Physical Activity and Diet Program Delivered by Artificially Intelligent Virtual Health Coach: Proof-of-Concept Study. JMIR mHealth uHealth 2020, 8, e17558.
5. Denecke, K. Framework for Guiding the Development of High-Quality Conversational Agents in Healthcare. Healthcare 2023, 11, 1061.
6. Yang, H.; Li, D. Understanding the dark side of gamification health management: A stress perspective. Inf. Process. Manag. 2021, 58, 102649.
7. Aronson, J.K.; Heneghan, C.; Ferner, R.E. Medical Devices: Definition, Classification, and Regulatory Implications. Drug Saf. 2020, 43, 83–93
8. Prochaska, J.J.; Vogel, E.A.; Chieng, A.; Kendra, M.; Baiocchi, M.; Pajarito, S.; Robinson, A. A Therapeutic Relational Agent for Reducing Problematic Substance Use (Woebot): Development and Usability Study. J. Med. Internet Res. 2021, 23, e24850.
9. May, R.; Security, K.D.; Care, I.H.S. Security, privacy, and healthcare-related conversational agents: A scoping review. Inform. Health Soc. Care 2021, 47, 194–210.
10. Godovykh, M.; Pizam, A. Measuring patient experience in healthcare. Int. J. Hosp. Manag. 2023, 112, 103405.
11. Majeed, S.; Kim, W.G. Toward understanding healthcare hospitality and the antecedents and outcomes of patient-guest hospital-hotel choice decisions: A scoping review. Int. J. Hosp. Manag. 2022, 112, 103383.
12. Chavriya, S.; Sharma, G.D.; Mahendru, M. Financial inclusion as a tool for sustainable macroeconomic growth: An integrative analysis. Ann. Public Coop. Econ. 2023, 95, 527–551.
13. Snyder, H. Literature review as a research methodology: An overview and guidelines. J. Bus. Res. 2019, 104, 333–339.
14. Spreadbury, J.; Young, A.; Kipps, C.A. Comprehensive Literature Search of Digital Health Technology Use in Neurological Conditions: Review of Digital Tools to Promote Self-management and Support. J. Med. Internet Res. 2022, 24, e31929.
15. Nebeker, C.; Gholami, M.; Kareem, D.; Kim, E. Applying a Digital Health Checklist and Readability Tools to Improve Informed Consent for Digital Health Research. Front. Digit. Health 2021, 3, 690901.
16. Botti, A.; Monda, A. Sustainable Value Co-Creation and Digital Health: The Case of Trentino eHealth Ecosystem. Sustainability 2020, 12, 5263.
17. Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digital Transformation in Healthcare: Technology Acceptance and Its Applications. Int. J. Environ. Res. Public Health 2023, 20, 3407.
FINANCING
The authors did not receive financing for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Swarna Swetha Kolaventi, Debasmita Tripathy, Madireddy Sirisha, Manish Nagpal, Prakriti Kapoor, Neha Rana, Malathi. H.
Drafting - original draft: Swarna Swetha Kolaventi, Debasmita Tripathy, Madireddy Sirisha, Manish Nagpal, Prakriti Kapoor, Neha Rana, Malathi. H.
Writing - proofreading and editing: Swarna Swetha Kolaventi, Debasmita Tripathy, Madireddy Sirisha, Manish Nagpal, Prakriti Kapoor, Neha Rana, Malathi. H.