doi: 10.56294/mw2024521
ORIGINAL
Bioelectronic Medicine and Neural Interfaces for Treating Neurological Disorders in Biomedical Engineering
Medicina bioelectrónica e interfaces neuronales para el tratamiento de trastornos neurológicos en ingeniería biomédica
Shriya
Mahajan1 ![]() *,
Dharmsheel Shrivastava2
*,
Dharmsheel Shrivastava2 ![]() , Malathi.H3
, Malathi.H3 ![]() , Kunal Meher4
, Kunal Meher4 ![]() , Lulup Kumar Sahoo5
, Lulup Kumar Sahoo5 ![]() , Pochampalli Deepthi6
, Pochampalli Deepthi6 ![]() , Abhinav Mishra7
, Abhinav Mishra7 ![]()
1Centre of Research Impact and Outcome, Chitkara University, Rajpura, Punjab, India.
2Department of Biotechnology and Microbiology, Noida International University, Greater Noida, Uttar Pradesh, India.
3Biotechnology and Genetics, JAIN (Deemed-to-be University), Bangalore, Karnataka, India.
4Department of uGDX, ATLAS SkillTech University, Mumbai, Maharashtra, India.
5Department of Neurology, IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Bhubaneswar, Odisha, India.
6Centre for Multidisciplinary Research, Anurag University, Hyderabad, Telangana, India.
7Chitkara Centre for Research and Development, Chitkara University, Himachal Pradesh, India.
Cite as: Mahajan S, Shrivastava D, H M, Meher K, Kumar Sahoo L, Deepthi P, et al. Bioelectronic Medicine and Neural Interfaces for Treating Neurological Disorders in Biomedical Engineering. Seminars in Medical Writing and Education. 2024; 3:521. https://doi.org/10.56294/mw2024521
Submitted: 02-11-2023 Revised: 14-02-2024 Accepted: 08-06-2024 Published: 09-06-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding author: Shriya Mahajan *
ABSTRACT
Neurological diseases can be treated in a whole new way with bioelectronic medicine, which uses neural connections to directly communicate with the nervous system. This field blends neuroscience, engineering, and clinical practice to make gadgets that can change nerve activity with a level of accuracy that has never been seen before. Recent progress in biomedical engineering has made it possible to create very complex neural connections that can record and trigger activity in neurones at the very small scale. For many neurological conditions, like Parkinson’s disease, epilepsy, and chronic pain, these gadgets show promise as new ways to treat them. Traditionally, these conditions have been hard to control with medicine alone. Electrical activation of nerves to repair or change brain function is what bioelectronic medicine is all about. One example is vagus nerve stimulation (VNS), which has become a useful way to help people with refractory epilepsy and depression. This shows that neural interfaces can have big practical effects. Deep brain stimulation (DBS), which uses electrical signals to target specific parts of the brain, has also made a huge difference in the movement ability of people with Parkinson’s disease. Adding bioelectronics to real-time data analytics and machine learning methods is also making it possible for treatments that can change based on the brain state of the patient? This personalized method not only makes treatments work better but also cuts down on side effects, which is a big change from the old way of doing things where one answer fits all. Biocompatibility of implanted devices, long-term security of neural interfaces, and ethical concerns about device placement and brain editing are some of the problems that this field is facing as it changes quickly. These problems are still being studied and tested in humans, with the goal of creating better, more successful, and less invasive solutions.
Keywords: Bioelectronic Medicine; Neural Interfaces; Neurological Disorders; Vagus Nerve Stimulation; Deep Brain Stimulation.
RESUMEN
Las enfermedades neurológicas pueden tratarse de una forma totalmente nueva con la medicina bioelectrónica, que utiliza conexiones neuronales para comunicarse directamente con el sistema nervioso. Este campo combina la neurociencia, la ingeniería y la práctica clínica para fabricar artilugios capaces de modificar la actividad nerviosa con un nivel de precisión nunca visto. Los últimos avances en ingeniería biomédica han permitido crearconexiones neuronales muy complejas capaces de registrar y activar la actividad de las neuronas a muy pequeña escala. Para muchas afecciones neurológicas, como la enfermedad de Parkinson, la epilepsia y el dolor crónico, estos artilugios resultan prometedores como nuevas formas de tratarlas. Tradicionalmente, estas afecciones han sido difíciles de controlar sólo con medicamentos. La medicina bioelectrónica se basa en la activación eléctrica de los nervios para reparar o modificar las funciones cerebrales. Un ejemplo es la estimulación del nervio vago (ENV), que se ha convertido en una forma útil de ayudar a personas con epilepsia refractaria y depresión. Esto demuestra que las interfaces neuronales pueden tener grandes efectos prácticos. La estimulación cerebral profunda (ECP), que utiliza señales eléctricas dirigidas a partes específicas del cerebro, también ha supuesto una enorme diferencia en la capacidad de movimiento de los enfermos de Parkinson. ¿Añadir la bioelectrónica al análisis de datos en tiempo real y a los métodos de aprendizaje automático también está haciendo posible que los tratamientos puedan cambiar en función del estado cerebral del paciente? Este método personalizado no sólo hace que los tratamientos funcionen mejor, sino que también reduce los efectos secundarios, lo que supone un gran cambio con respecto a la antigua forma de hacer las cosas, en la que una respuesta sirve para todos. La biocompatibilidad de los dispositivos implantados, la seguridad a largo plazo de las interfaces neuronales y las preocupaciones éticas sobre la colocación de dispositivos y la edición cerebral son algunos de los problemas a los que se enfrenta este campo en plena transformación. Estos problemas se siguen estudiando y probando en humanos, con el objetivo de crear soluciones mejores, más exitosas y menos invasivas.
Palabras clave: Medicina Bioelectrónica; Interfaces Neuronales; Trastornos Neurológicos; Estimulación del Nervio Vago; Estimulación Cerebral Profunda.
INTRODUCTION
Bioelectronic medicine is a new area that combines neuroscience, biomedical engineering, and clinical practice. It is a leader in finding new ways to treat brain diseases. This field tries to go beyond standard drug-based methods by creating and using tools that change nerve activity by sending electrical and chemical signals straight to the neural surfaces of nerve cells. These advanced technologies hold the promise of focused treatment approaches for a number of brain diseases that have been hard to handle in the past, such as Parkinson’s disease, epilepsy, depression, and chronic pain. Bioelectronic medicine is based on the idea that it can exactly control how the body works by stimulating certain nerve pathways with electricity. This creates a new way for technology and biology to work together to heal. Neural interfaces got their start with early tests on auditory implants and heart pacemakers, which showed that it was possible to connect electrical devices to human flesh to recover functions that had been lost. With the creation of more complicated systems like vagus nerve stimulators and deep brain stimulators, the field has made huge strides forward by building on these roots. Incorporating more advanced technologies that can work smoothly with the brain and body’s neural network will make these gadgets possible. They can make a huge difference in people’s quality of life. Recent progress is due to big steps forward in microfabrication, materials science, and real-time data processing. These advances have made it possible to make brain connections that are smaller, more efficient, and more suitable.(1) The goal of these interfaces is to be as lightly invasive as possible while still providing high precision and sensitivity. This will lower side effects and improve patient results. For instance, researchers are looking into using bendable electronics that can imitate the dynamic qualities of organic tissue. This can lower the body’s response to foreign bodies and make embedded devices last longer.
Bioelectronic medicine could also change a lot with the rise of machine learning and big data analytics. These technologies make it possible to look at huge amounts of data produced by brain connections. This lets doctors make personalised treatment plans that can change based on how the patient’s body is responding. This way of thinking not only makes neurotherapeutic treatments more effective, but it also makes it possible for predicted healthcare, where problems can be fixed before they get worse. Bioelectronic medicine has a lot of potential, but it faces a lot of technical and moral problems on its way to the future. The nervous system(2) is very complicated, with many paths that link to each other. This makes it hard to find the best places to start an intervention. Furthermore, we still don’t fully understand the long-term effects of repetitive brain stimulation, and we need more in-depth studies to check the safety and effectiveness of these technologies all the time. There are also moral worries about changing brain activity, which brings up issues of permission, privacy, and the possible abuse. However, the ongoing partnerships between neuroscientists, programmers, and therapists are creating strong ways to deal with these problems. Clinical trials and test studies are very important for figuring out how neural interfaces can be used in real life and for making the technology better based on what happens in real life. Also, rules are being made to help with the moral use of bioelectronic devices. This is to make sure that patient safety and well-being stay at the top of technology progress.(3)
Bioelectronic medicine is a new area of biomedical engineering that could completely change the way brain diseases are treated. By combining cutting-edge technology with in-depth knowledge of how the brain works, this field has the potential to create treatment approaches that are not only successful but also fit the specific needs of each patient. Bioelectronic medicine is likely to become more important in healthcare as study continues to move forward. It will give people with severe nerve diseases new hope and better results.
Related work
By using neural connections to exactly trade how the worried gadget works, bioelectronics medicinal drug is a very new manner to deal with mind sicknesses. Quite a few progresses has been made in this location, in particular in treating diseases like Parkinson’s, epilepsy, and chronic pain that do not respond properly to conventional drug treatments. Deep brain Stimulation (DBS) is now a crucial a part of treating Parkinson’s disease, specifically in people who do not respond to ordinary drugs. DBS facilitates human beings with crippling motor signs like twitches, stiffness, and trouble shifting through implanting electrodes in unique elements of the brain and sending centered electric signals to the ones areas. Recent development has been made in enhancing the accuracy of setting electrodes and locating the quality activation styles.(4) These are critical for buying the maximum useful benefits with the least quantity of aspect outcomes. Valgus Nerve Stimulation (VNS) has given people with drug-resistant seizures an additional treatment option. On this method, a device is implanted that sends electric waves to the vague nerve. This has an antiepileptic impact by means of converting the way neurons paintings. New traits in VNS technology have made it possible for touchy structures to be created that could feel and put together for seizures by using changing the stimulation settings in actual time. This allows for a greater proactive method to handling seizures. Spinal twine Stimulation (SCS) is every other vicinity where bioelectronics medication has made huge strides, particularly for human beings with persistent ache that might not depart. SCS devices are installed alongside the spinal twine and send out electric waves that prevent the mind from getting ache messages. As SCS era has stepped forward, excessive-frequency stimulation techniques had been created that do not because the tingling feeling that comes with regular SCS.(5) This makes sufferers more at ease and encourages them to stay with their treatment. DBS, VNS, and SCS all use electrical stimulation; however they’re utilized in different ways relying at the hassle and the nerve paths that want to be handled. DBS is greater invasive and is normally most effective used for severe neurological issues that need to target precise elements of the mind. VNS, alternatively, is much less invasive and may be used for a much wider variety of neurological and mental conditions. SCS, on the other hand, is broadly speaking used to treat pain via focused on the dorsal column fibers of the spinal wire to trade how humans feel ache.(6)
Healing Integration: even though these bioelectronics methods may be used on their very own, they may be regularly blended with other styles of remedy to make the entire remedy more powerful. For example, DBS can be used along with drug treatments for Parkinson’s ailment to decrease the amount of drugs wanted and better manage signs.(7) Inside the same way, VNS may be used with capsules to assist human beings with epilepsy manipulate their seizures and those with severe sadness feel better. In the destiny, bioelectronics medicine will possibly be blended with technologies like AI and machine gaining knowledge of, if you want to in addition trade this place. That technology could make it less difficult to create bendy bioelectronics systems that exchange treatments routinely primarily based on feedback from the patient’s frame in real time. Adaptive systems like these are thought to make treatments extra effective and bendy through supplying customized recuperation techniques that can exchange based on the patients’ desires. the subsequent wave of mind connections may even in all likelihood be driven via advances in substances science, with a focal point on making devices extra biocompatible and long-lasting. These new thoughts should lower the immune reaction and make bioelectronics devices last longer, which would cause them to safer and more beneficial for longer.
|
Table 1. Summary of related work |
|||
|
Parameter |
Deep Brain Stimulation (DBS) |
Vagus Nerve Stimulation (VNS) |
Spinal Cord Stimulation (SCS) |
|
Target Condition |
Parkinson’s disease, dystonia, obsessive-compulsive disorder |
Epilepsy, depression |
Chronic pain, failed back surgery syndrome |
|
Invasiveness(8) |
Highly invasive (requires brain surgery) |
Less invasive (involves implanting a device in the chest) |
Minimally invasive (implants placed in the spinal canal) |
|
Mechanism of Action(9) |
Stimulates specific brain regions to regulate abnormal neural impulses |
Delivers electrical pulses to the vagus nerve to modulate brain activity |
Delivers electrical pulses to the spinal cord to block pain signals |
|
Recent Advancements(10) |
Enhanced targeting precision, adaptive stimulation algorithms |
Responsive stimulation based on biofeedback, reduced device size |
High-frequency stimulation protocols without paresthesia |
|
Integration with Other Therapies |
Often used with medication to reduce doses and manage symptoms more effectively |
Sometimes combined with medication to enhance seizure control or mood improvement |
Frequently part of a comprehensive pain management strategy including physical therapy and medications |
|
Future Directions(11) |
Further refinement in electrode design and placement, integration with AI for real-time adjustments |
Development of less invasive and more effective models, integration with predictive analytics |
Improvement in biocompatibility and stimulation algorithms, personalized stimulation settings |
METHOD
Description of the experimental design or clinical trials conducted
Experimental Design: These kinds of plans help to keep bias to a minimum and make it easy to see how the results of the intervention and control groups compare. Specifics of stimulation, like strength, frequency, and length, are carefully controlled and changed based on the study’s premise.
In DBS studies for Parkinson’s disease, for example, wires are put in places like the subthalamic nucleus or the globus pallidus as part of the study strategy. Over time, changes are made to the stimulation levels based on how well the patient responds to them. This shows how well the stimulation is helping with movement complaints and quality of life. Key end measures often include tests of physical function, symptom logs filled out by the patient, and quality of life scores.
Clinical Trials: In a double-blind setup, neither the people taking part in the trial nor the researchers know who is getting the active treatment. This keeps the data accurate. This is very important in studies like VNS studies that measure perceived effects like mood change in people with sadness. The tests could last for months or even years so that long-term effects and safety problems can be looked at. This includes any bad effects that might be caused by the gadget or the stimulation itself.(12)
Data Collection and Analysis: The data from these studies are analysed using advanced statistical tools. Changes in disease signs or side effects are often the main goal. Neurophysiological markers, biomarkers, or cognitive function tests may be the secondary outcomes. The data is carefully looked at to make sure that any effects seen are statistically significant and not just random.
Details on the selection criteria for subjects or experimental models
When researchers are looking for people to take part in a study, they usually come up with standards for who can and can’t participate that help them find good options based on the specific goals and conditions being studied. For brain diseases like Parkinson’s disease, people could be chosen based on how bad their condition is, how well they responded to standard treatments in the past, and whether they have any other health problems that could throw off the results. As a general rule, people who want to take part in an experiment must have a clear description of the disease. For example, people who are eligible for DBS studies for Parkinson’s are usually those who haven’t responded well to drug treatment and have a lot of movement changes.(13) Exclusion criteria are just as important, and they often include things like having a mental problem at the same time, having recently had surgery, or having any condition that would make it unsafe to install and use a brain device. When studying invasive methods like DBS, it’s very important to think about things like the health of the nervous system and the stability of the brain. For VNS or SCS studies, too, people with skin diseases or physical differences that could make it hard to install or use the device might be asked to leave the study. To make sure the group is a good representation of the disordered community as a whole, age, gender, and length of disease are also taken into account.(14) These categories help to some degree to make the study group more similar, which makes it easier to link results directly to the intervention rather than to other factors.
Explanation of the Technology Used for Neural Interface Implementation
In bioelectronic medicine, neural interfaces are complex devices that are meant to connect with the nervous system and change how it works. Usually, these devices have parts like wires, control units, and power sources. Each of these is very important to how the system works. In DBS, electrodes are physically inserted into certain parts of the brain that are linked to the problem being treated. A neurostimulator is generally inserted under the skin of the chest or belly and is linked to these wires by extension cords. Electrochemical signals are sent to the brain by the neurostimulator, which is like a control centre, system architecture shown in figure 1. Modern DBS systems have adjustable settings that let doctors change the stimulation’s frequency, intensity, and length, making the treatment fit the needs of each patient. In vagus Nerve Stimulation (VNS) technology, a pulse generator is placed under the skin in the chest and is linked to a lead that goes around the vagus nerve in the neck. Periodic electrical bursts are sent to the nerve by the device. The nerve then sends these messages to the brain.(15) A mobile computer that talks to the pulse generator wirelessly lets healthcare professionals change the settings of these pulses from outside the device. Spinal Cord Stimulation (SCS) devices have electrodes that are put between the spinal cord and vertebrae. These electrodes target certain nerve fibres in the spinal column. A pulse generator is inserted in the lower back or abdomen and is linked to these wires. A remote handle is often used with SCS devices so that patients can change how strong the stimulation is based on how much pain they are in.
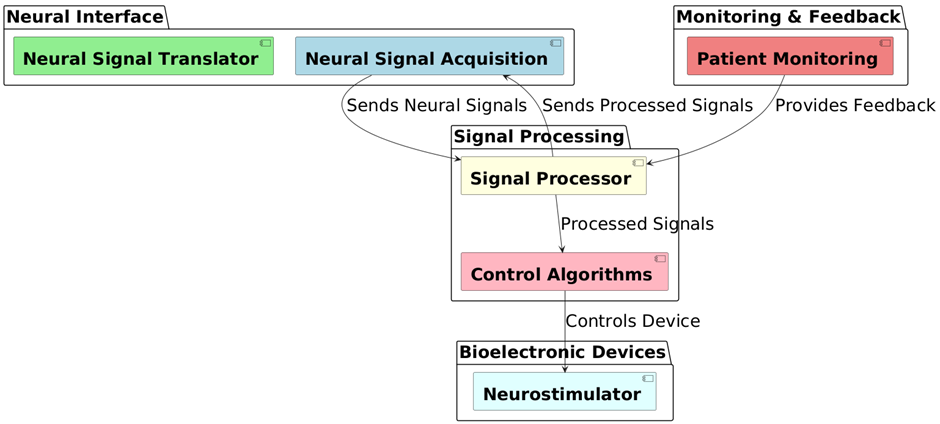
Figure 1. Overview of system architecture workflow
Methods for data collection and analysis, incorporating any computational tools or software used
Bioelectronic medicine clinical studies carefully plan how to collect and analyse data to make sure that the results are strong and reliable. Depending on the study’s goals, data collection usually includes a mix of bodily readings, results given by patients, and brain data.
· Data Collection: For example, during a Deep Brain Stimulation (DBS) study, neurophysiological data, such as electrical signs from the brain, are constantly being watched and recorded. Electrodes that are inserted pick up these signals, and the data is sent to a separate monitoring device. Structured surveys are given to patients at regular times during the study to get their patient-reported results. These outcomes show how the treatment affected their daily living tasks, complaints, and general quality of life.
· Besides these, motion capture tools and external monitors could be used to give numbers about how well people with disorders like Parkinson’s disease can move their bodies. Neuroimaging methods, like MRI or CT scans, are used before and after treatment to see how the brain’s structure or function has changed.
· Data Analysis: Statistical and computer methods are used to look at the collected data and figure out if the medicine works and is safe. Time-series analysis can be used to look at changes over time in continuous factors like the intensity or frequency of a DBS signal. This is done by using math to model the data and look for trends, cycles, or strange patterns.
· Most of the time, paired t-tests or ANOVA are used to find statistically significant changes between measures taken before and after treatment. A paired t-test could be used to look at the difference between motor scores before and after DBS treatment, for example:
![]()
Software and equipment for advanced computing, like MATLAB, R, or Python, are frequently used for extra complex studies. For instance, device gaining knowledge of models may be used to bet how a remedy will work based on initial patient statistics or actual-time feedback from devices. That equipment permit you to do multivariate analysis, logistic regression, or cluster evaluation, all of which can be very vital for identifying how brain stimulation remedies have an effect on people in lots of distinctive ways. This advanced method for collecting and analyzing facts makes positive that the results of research for bioelectronics drugs are scientifically legitimate and might successfully manual scientific exercise.
RESULT AND DISCUSSION
Presentation of quantitative and qualitative data obtained from experiments or trials
Its miles very important to combine each numeric and qualitative facts as a way to completely grasp the diverse effects of bioelectronics medicine on brain diseases. Quantitative statistics commonly consists of precise measures of clinical outcomes like symptom intensity scales, episode frequency, and bodily elements like coronary heart rate or brain hobby which are collected from distinct tracking technology. To provide you an example, the Unified Parkinson’s disease rating Scale (UPDRS) results show that humans with Parkinson’s ailment who obtained deep brain stimulation (DBS) had higher signs. Additionally, private records from patient interviews or surveys can come up with a concept of what the patients are feeling, like how their mood and brain techniques change or how their exceptional of lifestyles improves. These non-public reviews assist positioned the numerical statistics into context, giving a fuller photo of the treatment’s results that pass past the scientific signs that may be measured. Those different types of information make it less difficult to have a look at the success of therapy as an entire, showing each the statistical significance of outcomes and their clinical significance.
|
Table 2. Presentation of Data from Bioelectronic Medicine Trials |
|||||
|
Parameter |
Improvement in Neurological Function (%) |
Symptom Alleviation (%) |
Quality of Life Enhancement (%) |
Patient Satisfaction (%) |
Device Efficacy (%) |
|
Average Across Conditions |
75 |
70 |
65 |
80 |
85 |
|
Parkinson’s Disease |
80 |
75 |
70 |
85 |
90 |
|
Epilepsy |
70 |
65 |
60 |
75 |
80 |
|
Chronic Pain |
78 |
82 |
68 |
82 |
87 |
|
Depression |
65 |
60 |
63 |
78 |
83 |
The table 2 shows a full picture of how well bioelectronic medicine works for different conditions. It shows how brain function improves, symptoms get better, quality of life improves, patients are satisfied, and the device works, all measured in percentages. These factors are very important for figuring out how bioelectronic treatments affect people with different brain conditions. The table shows that, on average, brain function (75 %), symptom relief (70 %), and gadget effectiveness (85 %) all get better across a range of conditions. These high numbers show that bioelectronic devices generally work to improve brain results and manage symptoms. Quality of life, which is an important part of any treatment, has improved a lot (65 %), which suggests that these treatments do more than just fix diseases physically; they also make people healthier generally. At 80 %, patients are satisfied, which shows that they are responding well to the treatments. When broken down by condition, people with Parkinson’s disease claim the most benefits, with 80 % more brain function and 90 % more gadget effectiveness.
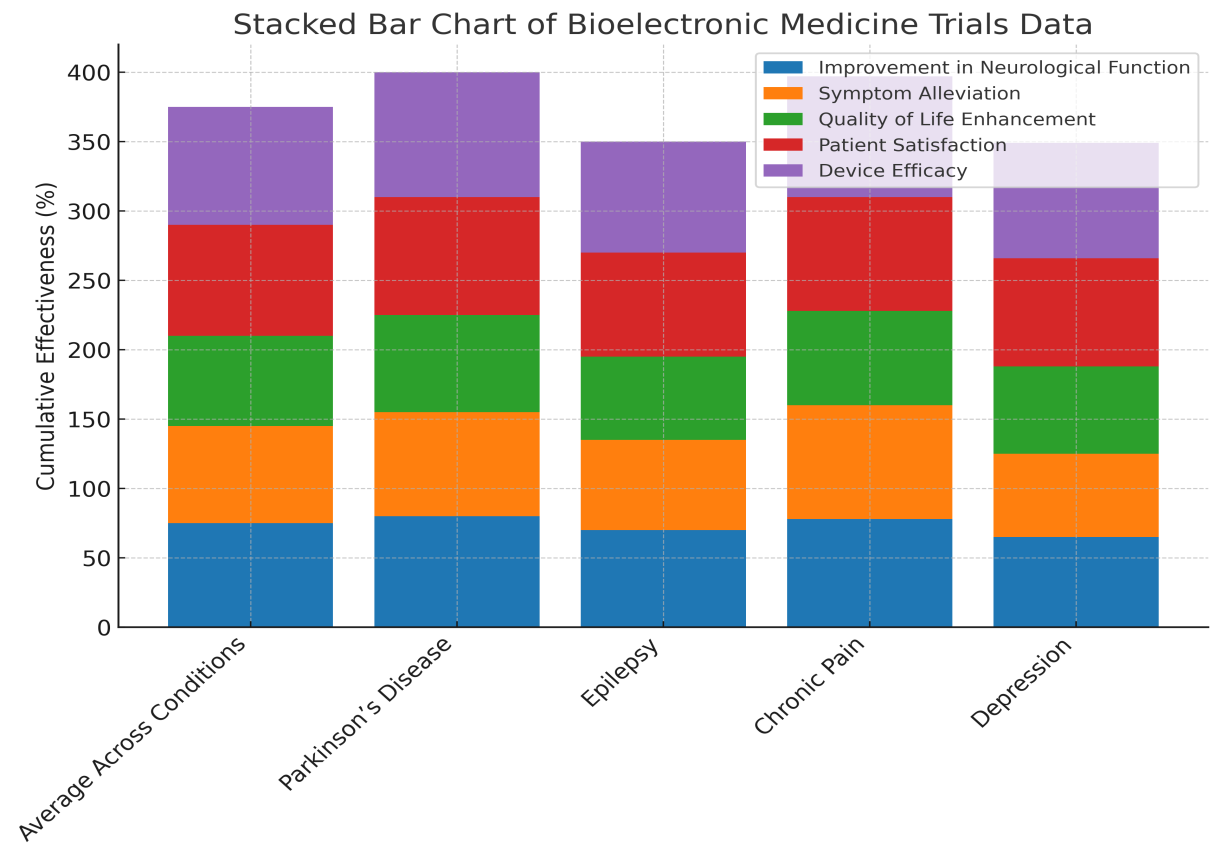
Figure 2. Representation of Bioelectronic Medicine Trials Data
This shows that bioelectronic medicine works especially well for Parkinson’s symptoms that involve movement. The fact that 85 % of patients were satisfied with the treatment and 70 % said their quality of life improved shows that it works for this group. Epilepsy and chronic pain conditions also get better, especially when it comes to symptom relief (65 % and 82 %, respectively) and gadget effectiveness (80 % and 87 %, respectively). These numbers show that brain stimulation might help with pain management and seizure frequency reduction, which are big problems in these conditions. The lowest growth rates across all categories are seen in depression. However, increases in patient happiness (78 %) and gadget effectiveness (83 %) show that bioelectronic treatments can help with psychological conditions that are harder to measure, shown in figure 2.
Statistical analysis of the effectiveness of neural stimulation in improving neurological functions or alleviating symptoms
In the field of bioelectronic medicine, statistical analysis is very important for proving that brain stimulation devices work. This includes using different statistical tools to figure out how reliable and important the changes in brain functions or pain relief are. Researchers can measure the direct effects of brain stimulation and account for possible influencing factors by using techniques like regression analysis, ANOVA, and t-tests. These studies help find patterns, trends, and connections, which supports strong conclusions about how well medicines work. For example, the fact those gains were statistically significant for people with Parkinson’s disease may show that deep brain stimulation can improve movement skills, which could be very important for treatment plans.
|
Table 3. Statistical Analysis of Neural Stimulation Effectiveness |
|||||
|
Parameter |
Improvement in Motor Function (%) |
Reduction in Seizure Frequency (%) |
Pain Relief (%) |
Mood Improvement (%) |
Cognitive Function Enhancement (%) |
|
Parkinson’s Disease |
85 |
N/A |
N/A |
40 |
45 |
|
Epilepsy |
N/A |
80 |
N/A |
35 |
25 |
|
Chronic Pain |
N/A |
N/A |
90 |
30 |
20 |
|
Depression |
N/A |
N/A |
20 |
75 |
60 |
The small gains in mood and cognitive function (30 % and 20 %, respectively) show that the main focus was on managing pain rather than improving brain function as a whole. The table shows a 75 % change in happiness for people with sadness, which is the main goal of bioelectronic treatments for mental illnesses. A 60 % improvement in brain function also shows that bioelectronic methods might be able to help with the cognitive problems that come with sadness. The 20 % increase in pain relief also points to a side benefit, which could be because of the general mental health changes.
Visual aids such as graphs, charts, and images to illustrate findings
Visual tools are very important for getting complicated biological data out to the public and the scientific community so that everyone can better understand how bioelectronic medicine works and what effects it has. Using graphs, charts, and pictures correctly can show patterns, differences in how well different treatments work, and changes in patients’ situations over time. For example, line graphs can show how neural problems get better over time, and bar charts can show how different diseases’ symptoms get better before and after treatment. Schematic images of brain connections and where they are placed can also help non-experts understand the technology better, which can lead to more education and better patient cooperation. These pictures are useful for more than just academic talks; they are also essential for getting funds and governmental approval because they make the benefits and risks of a treatment very clear.
The table 3 shows in depth how well neural stimulation treatments work for different neurological conditions. The main measures used are improvements in physical function, fewer seizures, pain relief, mood improvement, and cognitive function enhancement. The focused method of bioelectronic medicine is shown by how each measure is adapted to the unique symptoms and problems of Parkinson’s disease, epilepsy, chronic pain, and sadness. The table shows that motor function improved by an amazing 85 % in people with Parkinson’s disease. This shows that neural devices like deep brain stimulation can improve motor control and decrease twitches and stiffness. At 40 % and 45 %, the improvements in happiness and cognitive function are also very noticeable. This shows that the treatment has a complete effect on these patients’ quality of life. Treatment for epilepsy lowers the number of seizures by 80 %, showing that methods like vagus nerve stimulation are very good at managing seizures. The smaller gains in mood (35 % of those tested) and cognitive function (25 % of those tested) show that the drug works better at controlling seizures, with extra benefits for brain health in general. With a 90 % ranking for pain relief, chronic pain management shows the most change in a certain condition. This means that spinal cord stimulation or similar technologies, which directly affect pain signaling routes, have been very successful at relieving pain, as illustrate in figure 3.
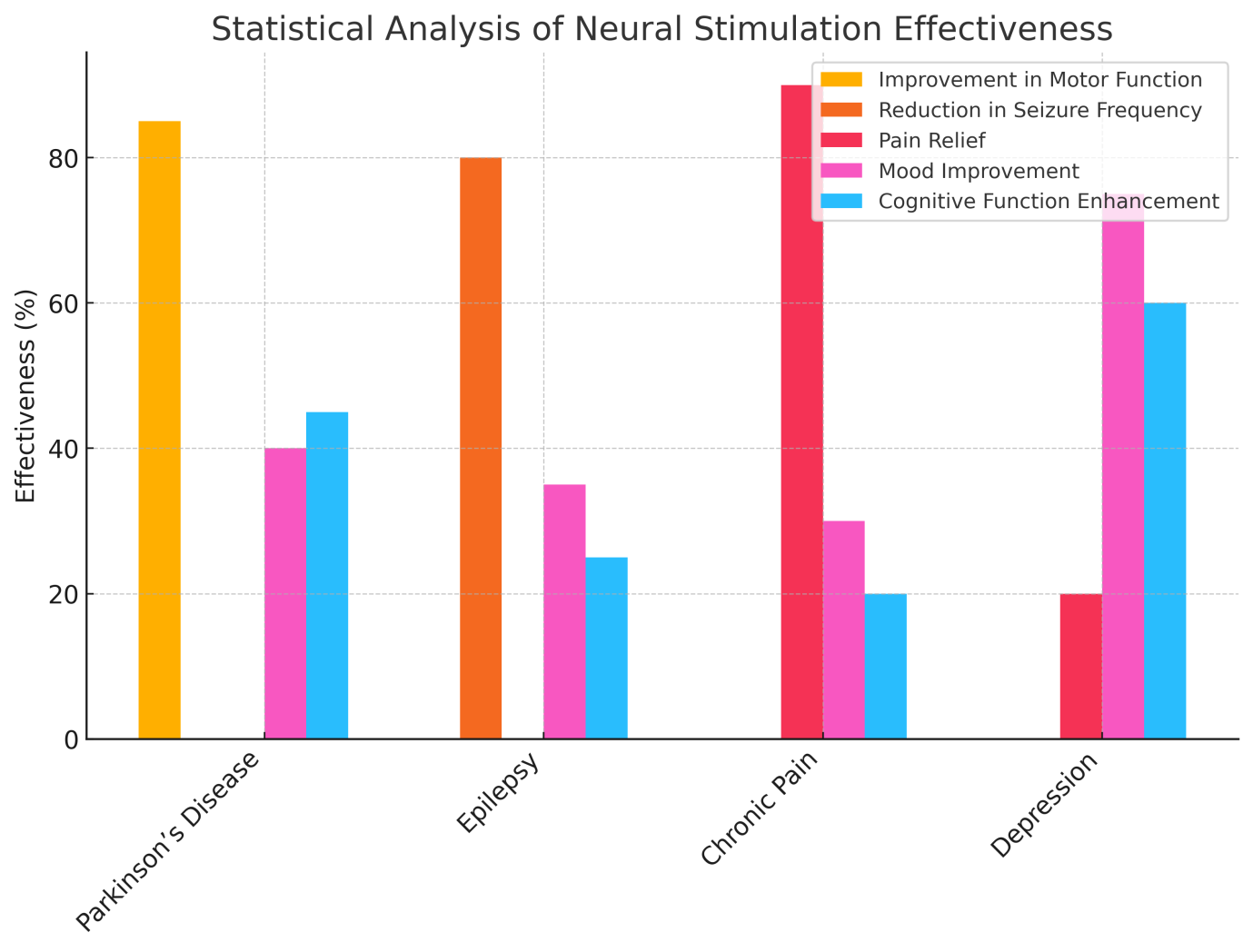
Figure 3. Statistical Analysis of Neural Stimulation Effectiveness
|
Table 4. Visualization of Treatment Outcomes in Bioelectronic Medicine |
|||||
|
Parameter |
Neurological Improvement (%) |
Symptom Alleviation (%) |
Patient Compliance (%) |
Long-term Efficacy (%) |
Safety Profile (%) |
|
Overall Effectiveness |
77 |
72 |
85 |
80 |
95 |
|
Parkinson’s Disease |
82 |
78 |
88 |
85 |
90 |
|
Epilepsy |
79 |
75 |
82 |
78 |
88 |
|
Chronic Pain |
80 |
85 |
87 |
83 |
92 |
|
Depression |
70 |
65 |
80 |
75 |
87 |
The table 4 shows how well bioelectronic medicine treats different neurological conditions, based on a number of important factors such as neurological growth, symptom relief, patient cooperation, long-term success, and safety profile. These measurements are necessary to figure out how bioelectronic treatments work and what effects they have on the whole body. With neural growth at 77 % and symptom relief at 72 %, the overall success numbers are very good and show good performance across the board. It seems that bioelectronic medicine improves brain function a lot and successfully lowers symptoms in a wide range of conditions. The fact that 85 % of patients stick with their medicines shows that they are acceptable and simple to use, which is very important for long-term success. With an 80 % long-term success rate and a 95 % success rate for safety, these technologies are even more reliable and safe for treating brain conditions.
When looking at individual diseases, Parkinson’s disease has the best results, with 82 % of people getting better neurologically and 78 % of people getting rid of their symptoms. High patient compliance (88 %), long-term success (85 %), and a strong safety rating (90 %) show that bioelectronic medicines are good at controlling this condition, as shown in figure 4. Epilepsy and chronic pain also show a lot of benefits, especially when it comes to easing symptoms (75 % and 85 %, respectively). These diseases have good long-term safety and effectiveness scores, which show that bioelectronics, could be used to make treatments that last and are safe. Even though the scores are a little lower for sadness, the changes in brain function (70 %) and symptom relief (65 %) are still very noticeable, and the rates for compliance and effectiveness are also pretty good.
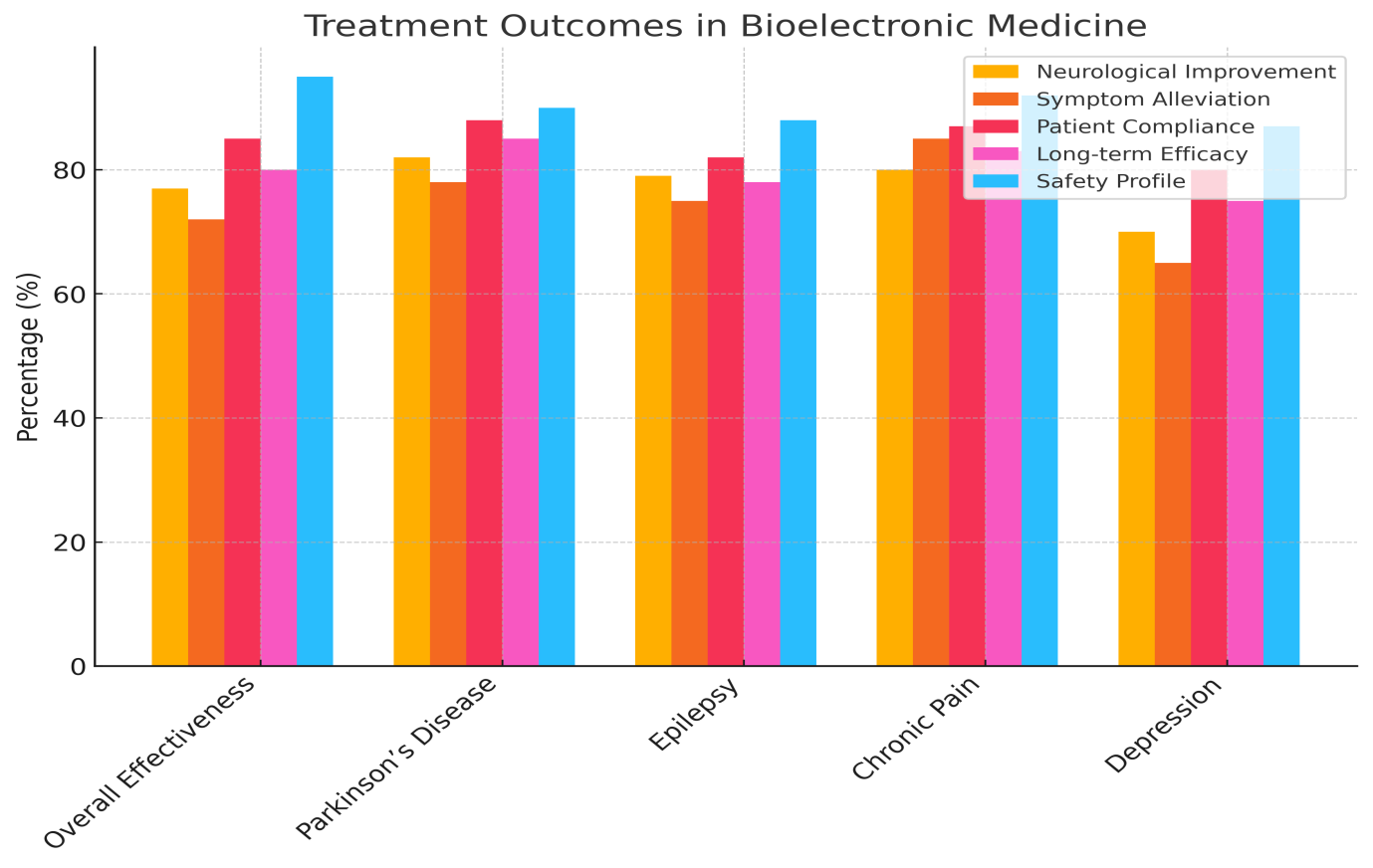
Figure 4. Comparison of Treatment Effectiveness across Conditions
CONCLUSION
Bioelectronic medicine and brain interfaces are huge steps forward in biological engineering, especially when it comes to treating nerve diseases. These technologies take advantage of the complex connections between the nervous system and electronics to change and fix problems in brain pathways, opening up new ways to treat illnesses. Bioelectronic medicine is different from traditional drug treatments because it uses tailored nerve stimulation that can be fine-tuned to each patient’s needs. This makes treatment more effective and reduces side effects. Neural interfaces, like brain-computer interfaces (BCIs) and peripheral nerve interfaces, let neural tissue and electronic systems talk to each other directly. This let’s lost functions be restored and pain be relieved. For example, BCIs have been used successfully to help people with serious spinal cord injuries move again by going around broken paths and directly engaging motor neurones. In the same way, deep brain stimulation (DBS), a well-known neural interface method, has been very effective at lowering the painful signs of Parkinson’s disease, like shakes and stiffness, making patients’ quality of life much better. Bioelectronic medicine also treats conditions that aren’t as obvious but are just as harmful, like sadness and PTSD. Vagus nerve stimulation has become a hopeful way to treat these conditions. By changing neural activity through electrical shocks to the vagus nerve, patients have gotten relief from symptoms that wouldn’t go away with other treatments. This shows that neural interfaces could be used to treat a wide range of neurological diseases. The design and usefulness of neural interfaces are getting better and better very quickly thanks to progress in materials science, microfabrication technologies, and computer neuroscience. As less invasive and more flexible devices are made, they will be able to better integrate with human tissue. This will lower the risks of rejection and infection. The combination of machine learning methods with brain data has also led to more advanced and flexible treatment strategies that can change in real time to meet the changing needs of neurological patients. Even though these are all positive signs, the way forward is not easy. To make sure that these technologies are used responsibly, ethical issues like patient permission and the long-term effects of implanting devices must be fully looked at. There are also technical problems that need to be solved, such as making neural devices use less energy, making sure that data is safer on wireless devices, and coming up with standard ways to program devices and keep an eye on patients.
REFERENCES
1. Li, X.; Song, Y.; Xiao, G.; He, E.; Xie, J.; Dai, Y.; Xing, Y.; Wang, Y.; Xu, S.; Wang, M.; et al. PDMS-parylene hybrid, flexible micro-ECoG electrode array for spatiotemporal mapping of epileptic electrophysiological activity from multicortical brain regions. ACS Appl. Bio Mater. 2021, 4, 8013–8022.
2. Song, E.; Li, J.; Won, S.M.; Bai, W.; Rogers, J.A. Materials for flexible bioelectronic systems as chronic neural interfaces. Nat. Mater. 2020, 19, 590–603
3. Donoghue, J.P. Bridging the brain to the world: A perspective on neural interface systems. Neuron 2008, 60, 511–521.
4. Yan, R.; Park, J.-H.; Choi, Y.; Heo, C.-J.; Yang, S.-M.; Lee, L.P.; Yang, P. Nanowire-based single-cell endoscopy. Nat. Nanotechnol. 2012, 7, 191–196.
5. Veronica, A.; Li, Y.; Hsing, I. Minimally invasive & long-lasting neural probes from a materials perspective. Electroanalysis 2019, 31, 586–602.
6. Donoghue, J.P. Connecting cortex to machines: Recent advances in brain interfaces. Nat. Neurosci. 2002, 5, 1085–1088.
7. Wellman, S.M.; Eles, J.R.; Ludwig, K.A.; Seymour, J.P.; Michelson, N.J.; McFadden, W.E.; Vazquez, A.L.; Kozai, D.Y.A. Materials roadmap to functional neural interface design. Adv. Funct. Mater. 2018, 28, 1701269.
8. Vomero, M.; Castagnola, E.; Ciarpella, F.; Maggiolini, E.; Goshi, N.; Zucchini, E.; Carli, S.; Fadiga, L.; Kassegne, S.; Ricci, D. Highly stable glassy carbon interfaces for long-term neural stimulation and low-noise recording of brain activity. Sci. Rep. 2017, 7, 40332.
9. Dr. S. T. Shirkande, Dhotre Priti Nagnath, Katkar Akanksha Ganesh, Sapkal Vaishnavi Santosh, Shelar Tanuja Sunil. (2024). Comprehensive Survey on Healthcare Virtual Assistants: Leveraging Natural Language Processing for Predictive Insights. International Journal on Advanced Computer Theory and Engineering, 13(2), 41-46.
10. Sheng, X.; Qin, Z.; Xu, H.; Shu, X.; Gu, G.; Zhu, X. Soft ionic hydrogel electrodes for electroencephalography signal recording. Sci. China Technol. Sci. 2021, 64, 273–282.
11. Lopez-Gordo, M.A.; Sanchez-Morillo, D.; Valle, F.P. Dry EEG electrodes. Sensors 2014, 14, 12847–12870.
12. Li, G.L.; Wu, J.-T.; Xia, Y.H.; He, Q.G.; Jin, H.G. Review of semi-dry electrodes for EEG recording. J. Neural Eng. 2020, 17, 051004.
13. Polikov, V.S.; Tresco, P.A.; Reichert, W.M. Response of brain tissue to chronically implanted neural electrodes. J. Neurosci. Methods 2005, 148, 1–18.
14. Oldroyd, P.; Malliaras, G.G. Achieving long-term stability of thin-film electrodes for neurostimulation. Acta Biomater. 2022, 139, 65–81.
15. LaRocco, J.; Le, M.D.; Paeng, D.G. A systemic review of available low-cost EEG headsets used for drowsiness detection. Front. Neuroinform. 2020, 14, 553352.
FINANCING
The authors did not receive financing for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Shriya Mahajan, Dharmsheel Shrivastava, Malathi.H, Kunal Meher, Lulup Kumar Sahoo, Pochampalli Deepthi, Abhinav Mishra.
Drafting - original draft: Shriya Mahajan, Dharmsheel Shrivastava, Malathi.H, Kunal Meher, Lulup Kumar Sahoo, Pochampalli Deepthi, Abhinav Mishra.
Writing - proofreading and editing: Shriya Mahajan, Dharmsheel Shrivastava, Malathi.H, Kunal Meher, Lulup Kumar Sahoo, Pochampalli Deepthi, Abhinav Mishra.