doi: 10.56294/mw2024524
ORIGINAL
Myofibroblast Activity in Diabetic Wound Healing: Unravelling the Diabetes Connection and Therapeutic Interventions
Actividad miofibroblástica en la cicatrización de heridas diabéticas: Desentrañando la Conexión con la Diabetes e Intervenciones Terapéuticas
Harsh Bhati1 ![]() *, Manashree Mane2
*, Manashree Mane2 ![]() , Vinima Gambhir3
, Vinima Gambhir3 ![]() , Jyoti Prakash Samal4
, Jyoti Prakash Samal4 ![]() , Vundela Swathi5
, Vundela Swathi5 ![]() , Jagmeet Sohal6
, Jagmeet Sohal6 ![]() , Saksham Sood7
, Saksham Sood7 ![]()
1Noida International University, Department of General Surgery. Greater Noida, Uttar Pradesh, India.
2JAIN (Deemed-to-be University), Department of Forensic Science. Bangalore, Karnataka, India.
3ATLAS SkillTech University, Department of ISME. Mumbai, Maharashtra, India.
4IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University), Department of Onco-Medicine. Bhubaneswar, Odisha, India.
5Centre for Multidisciplinary Research, Anurag University. Hyderabad, Telangana, India.
6Chitkara Centre for Research and Development, Chitkara University. Himachal Pradesh, India.
7Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
Cite as: Bhati H, Mane M, Gambhir V, Samal JP, Swathi V, Sohal J, et al. Myofibroblast Activity in Diabetic Wound Healing: Unravelling the Diabetes Connection and Therapeutic Interventions. Seminars in Medical Writing and Education. 2024; 3:524. https://doi.org/10.56294/mw2024524
Submitted: 04-11-2023 Revised: 17-02-2024 Accepted: 15-06-2024 Published: 16-06-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Harsh Bhati *
ABSTRACT
Diabetic wound healing poses a significant clinical challenge due to the impaired regenerative capacity observed in individuals with diabetes. Diabetes causes a dysregulated wound healing process that is multidimensional and involves intricate interactions between cellular and molecular processes. This paper reviews discuss the activity of myofibroblasts in the context of diabetic wound healing. Myofibroblasts are specialized cells with contractile capabilities that are essential for developing scars and tissue healing. They are one of the main participants in this complex process. Wound healing is a multifaceted and ever-changing biological response involving several interrelated systems. Enzymes responsible for the control of the extracellular matrix (ECM) are tissue inhibitors of metalloproteinases (TIMPs) and matrix metalloproteinases (MMPs). The ECM is essential for wound healing, reconstruction of tissues, and other bodily processes. Diabetes and myofibroblast apoptosis have a complicated and multidimensional interaction. Diabetes is a chronic illness that needs to be managed continuously since it fails to go away on the own. This strategy has strained interest in a number of areas, including wound healing. Certain academics have looked at the possibility of repurposing medications for wound care applications, even if this could not be typical. Dipeptidyl peptidase 4, metformin, and propranolol are used in the reusing of medications for the purpose of promoting wound healing. This review provides information on the influence of diabetes on myofibroblast function and fibroblast differentiation, as well as potential treatment options associated with the affected pathways.
Keywords: Martix Metalloproteinases (MMPs); Extracellular Matrix (ECM); Tissue Inhibitors Metalloproteinases (TIMPs); Dipeptidyl Peptidase 4 (DPP4).
RESUMEN
La cicatrización de heridas diabéticas plantea un importante reto clínico debido a la capacidad regenerativa alterada que se observa en las personas con diabetes. La diabetes causa un proceso de cicatrización de heridas desregulado que es multidimensional e implica intrincadas interacciones entre procesos celulares y moleculares. En este artículo se analiza la actividad de los miofibroblastos en el contexto de la cicatrización de heridas diabéticas. Los miofibroblastos son células especializadas con capacidades contráctiles esenciales para el desarrollo de cicatrices y la curación de tejidos. Son uno de los principales participantes en este complejo proceso. La cicatrización de heridas es una respuesta biológica polifacética y en constante cambio en la que intervienen varios sistemas interrelacionados. Las enzimas responsables del control de la matriz extracelular (MEC) son los inhibidores tisulares de las metaloproteinasas (TIMP) y las metaloproteinasas de matriz (MMP). La MEC es esencial para la cicatrización de heridas, la reconstrucción de tejidos y otros procesos corporales. La diabetes y la apoptosis de miofibroblastos tienen una interacción complicada y multidimensional. La diabetes es una enfermedad crónica que hay que controlar continuamente, ya que no desaparece por sí sola. Esta estrategia ha despertado el interés en diversos ámbitos, como la cicatrización de heridas. Ciertos académicos han estudiado la posibilidad de reutilizar medicamentos para aplicaciones en el cuidado de heridas, aunque no sea lo habitual. La dipeptidil peptidasa 4, la metformina y el propranolol se utilizan en la reutilización de medicamentos con el fin de promover la cicatrización de heridas. Esta revisión proporciona información sobre la influencia de la diabetes en la función de los miofibroblastos y la diferenciación de los fibroblastos, así como las posibles opciones de tratamiento asociadas a las vías afectadas.
Palabras clave: Martix Metaloproteinasas (MMPs); Matriz Extracelular (ECM); Inhibidores Tisulares de las Metaloproteinasas (TIMPs); Dipeptidil Peptidasa 4 (DPP4).
INTRODUCTION
A systemic disease called diabetes causes hyperglycemia that could be caused by organs and cells becoming resistant to insulin or an inadequate amount of the protein in the blood. In the throughout the globe, diabetic wounds over time represent a significant public health threat.(1) Individuals with diabetes have 10–20 times higher risk of limb owing to persistent ulcers than the rest of the population. The intricate reaction of biological and molecular processes that occurs during healing of wounds in diabetes is reflected in all phases of the healing procedure.(2) Typically, tissue remodeling, development, and inflammatory are the stages that wound healing through. It's a complicated procedure, and several situations involving tissue healing capacity result from any failure.(3) Extracellular Matrix (ECM), enhance the structural integrity of tissues following injury, and wound healing where cells proliferate and reshape.(4) Different progenitor cells are the source of lymphocytes.(5) According to exploratory and clinical data, diabetes-related healing of wounds can affect the development of myofibroblasts from precursor cells, which could result in inadequate ECM deposition, decreased wound contraction, and increased proteolytic enzymes operation as well as a dearth of proliferating cells.(6) Based on existing laboratory and clinical investigations, the study will discuss and assess the effects that diabetes has on myofibroblast biology, therapeutic methods for wound healing and pertinent signalling networks.(7)
An approach for understanding how diabetes affects the process of healing wounds, particularly myofibroblast activity.(8) Diabetes results in poor healing because of its complex pathophysiology, which includes immunological, nerve-related, blood vessels and physiological elements. Tissue oxygenation is reduced by delayed circulation and microvascular dysfunction brought by enhanced vessel stiffness linked to hyperglycaemia.(9) Peripheral nerve injury can cause tingling and reduced response to pain, if left untreated can culminate in the occurrence of long-term wounds. The traits mentioned are particularly important for the lower limbs, especially the foot, which is more susceptible to chronic conditions due to its greater exposure, even from minor lesions.(10) Table 1 depicts the summary of the review.
|
Table 1. Summary of the review |
||||
|
Writer |
Year |
Methods |
Findings |
Conclusion |
|
Eitner A et al.(11) |
2019 |
ELISA |
Plumbagin administration improved wound healing and showed potential as an antidiabetic and anti-inflammatory agent, according to the study results. |
Plumbagin's antidiabetic and wound healing mechanisms and the active principle involved can contribute to developing effective therapeutic strategies for diabetic wound treatment. |
|
Yan Y et al.(12) |
2020 |
PZH |
Topical Pazopanib Hydrochloride (PZH) outperformed systemic administration in enhancing wound closure and improving healing quality in the in vivo study. |
To promised progress in developing a topical PZH dosage for diabetic wound healing. |
|
Braunwald E (13) |
2019 |
T2DM |
The interplay among Type 2 Diabetes Mellitus (T2DM), heart failure, and renal dysfunction, creating harmful cycles. |
The described vicious circles here illustrate the progression of T2DM, with cardiovascular and renal complications often leading to disability and death. |
|
La Sala L et al. (14) |
2020 |
DPP |
To clarify the molecular pathways in obesity-related processes that contributes to the development of chronic diseases like diabetes and its complications. |
To highlight key aspects of diabetes prevention in overweight/obesity, with a focus on surgical interventions.
|
|
Kato M et al.(15) |
2019 |
DKD |
Early detection of epigenetic events in Diabetic Kidney Diseas (DKD) could aid timely diagnosis and prevent progression to end-stage renal disease. |
It explores the possibilities of certain methylation variables and non-coding RNAs as diagnostic and therapeutic targets, highlighting the rising relevance of genetics and epigenomics research in DKD. |
Diabetic wound healing
Myofibroblasts are specialized cells that are necessary for tissue regeneration and wound healing. With characteristics of both soft tissue and fibroblast cells, these cells represent a special hybrid.(16) Alpha-smooth muscles action and other electromechanical amino acids, which allow these cells to apply force and take part in tissues shrinkage, are characteristics of lymphocytes. When tissue injury first occurs, skeletal muscle cells are drawn to the damaged area to aid in the healing process by forming granulation tissue and helping wounds to close.(17) As a result of their contractile qualities, the wounded region shrinks and the wound contracts. Diabetes has an impact on skeletal muscle cells at all stages of the complex wound healing process.(18) Its effects are felt during the initiation, inflammation, cell proliferation, and maturing phases and a result has a significant effect on the entire course of tissue recovery. Figure 1 shows the myofibroblasts healing process.
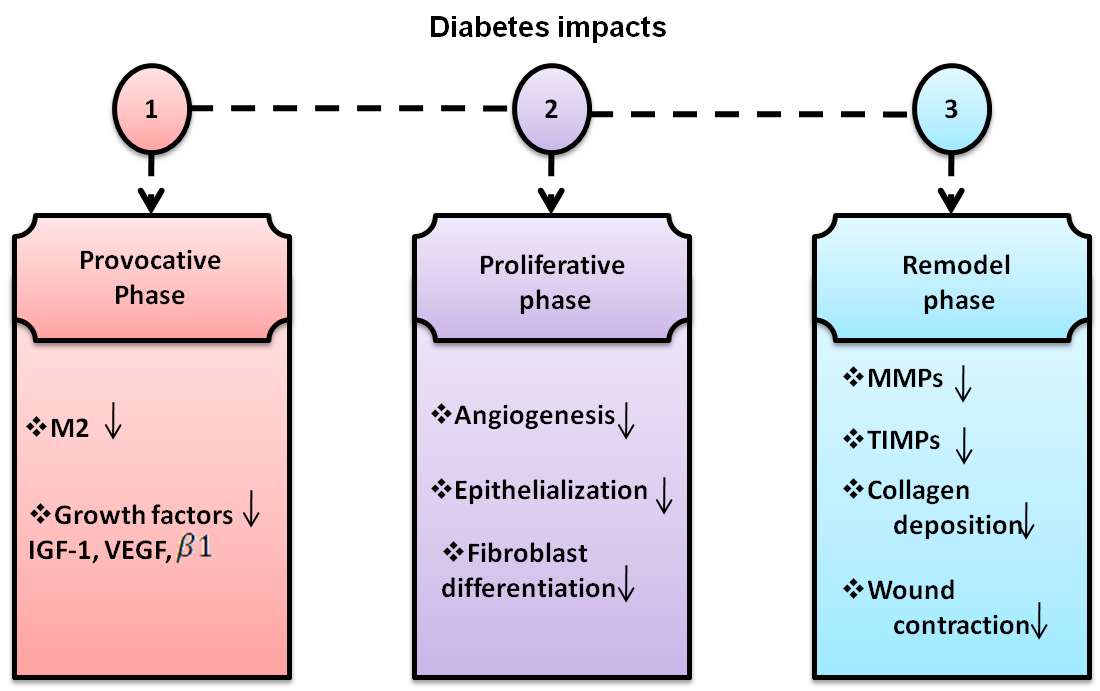
Figure 1. Diabetes impacts
Diabetes's effects on myofibroblast apoptotic
Myofibroblasts are highly particular cells that develop early in the recovery process and eliminated during the tissue-granulation phase when they are operating regularly. Diabetes causes myofibroblast maturation to be delayed in the beginning stages of repair phase.(19) However, it was shown in diabetic mice that were given a substance known as the number of myofibroblasts increased at later 15-day time periods. Particularly in the diabetic wounds was seen a prolonged retention for many days following the granulation phase and a delay in enlistment at the start of the process of wound healing.(20) Numerous in vitro experiments have demonstrated how hyperglycemia modifies the physiology of fibroblasts, including apoptosis, RETIREMENT and granular resistance. The healing of chronic diabetes wounds is significantly influenced by the mitochondrial behavior. Through the use of db/db mice, it was shown that diabetic wounds had notably elevated levels of TNF-α, fibroblast death, the caspase enzyme-3/7 operation and an increase in the pro-apoptotic transcription element FOXO1.(21) Recent findings indicate that in diabetic rats, adjusting TNF-α can decrease death and boost cell proliferation and myofibroblast densities and the healing of oral wounds in db/db mice and individuals that received glucocorticoid treatments.(22) In terms of molecular makeup, wounds in diabetic mice displayed a substantial increase in TUNEL-labeled apoptotic cells compared to wounds in control animals.(23) These changes were significant at 7 and 14 days following the creation of the wounds. Further analysis showed that some of these cells had died in fact scaffolds. Further studies should be used to investigate the relationship between diabetes and the apoptotic properties of fibroblasts, even though the precise mechanism is unclear.(24) Interaction between cells depends on gap junctions, which also support signs of cell death, such as fibrosis ablation. Gap junction amino acid over expression can result in deadly signaling errors and particularly common in wounds caused by diabetes.
Diabetes's effects on MMPs and TIMPs
This high ratio in wounds associated with diabetes sets off a series of harmful events: low TIMP levels trigger unchecked MMP activity, which in turn causes excess extracellular matrix (ECM) destruction. Moreover, other studies have shown, the elevated MMP protein concentrations worsen the disability by upsetting the well planned process of ECM formation.(25) A key component of the pathogenesis of diabetic wounds is revealed by the complex interaction between MMPs and TIMPs, which also identifies possible targets for therapeutic therapies meant to restore the delicate balance in the injury's environment.(26) Further research using db mice confirmed these results by revealing a significant reduction in the production of vascular endothelial growth factor (VEGF) in conjunction with increased activity of matrix metalloproteinase-9 (MMP-9) and hence a strong pro-degradative effect on cellular function.(27) In the context of urethral scarring, this multimodal investigation offers significant insights into the complex interactions between molecular variables controlling responses from cells . Table 2 depicts the impacts of MMPs and TIMPs.
|
Table 2. MMPs and TIMPs impacts |
||
|
Factor |
MMPs |
TIMPs |
|
MMP Expression |
Increased expression in diabetes |
Altered expression levels |
|
MMP Activity |
Elevated activity contributes to tissue remodeling and fibrosis |
Can be decreased in diabetic conditions |
|
Role in Complications |
Involved in diabetic complications (e.g., retinopathy, nephropathy) |
Helps regulate MMP activity, potentially protective |
|
Balance Disruption |
Imbalance leads to tissue degradation |
Disruption could exacerbate diabetic complications |
|
Therapeutic Targets |
MMP inhibitors considered for treatment |
TIMP modulation as a therapeutic approach |
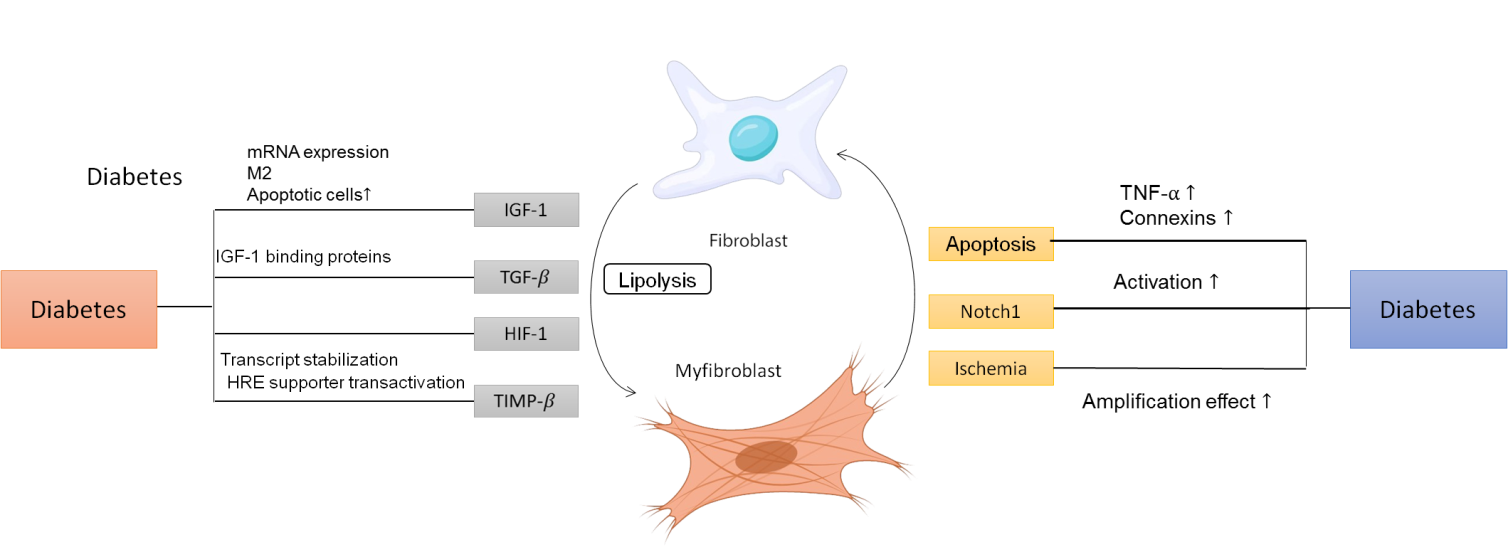
Figure 2. Diabetes's effects on many signaling pathways involved in healing wounds, including myofibro blastfunctioning
The mechanisms of healing in wounds
The physiological process of wound healing is a complex phenomenon initiated by the loss of skin integrity, impacting its barrier functions.(28) Given the skin's significant exposure to external irritants and the need to prevent infection, a rapid defense mechanism is often activated. Although the skin typically regains around 70 % of its original tensile strength, it can ultimately return to its natural state through physiological healing.(29) Usually, this process is divided into three phases: an inflammatory, a proliferative, and the reconstruction phase.
Repair in diabetes
The healing of wounds, leukocyte migration through disrupted extracellular matrix, processing of numerous cytokines and growth factor participation are few of the components that make up the procedure for recovery.(30) Preventing the disintegration of the foundations essential to the best possible wound healing requires maintaining the proper balance between MMPs and TIMPs. A synthetic, graphic depiction illustrating the sequence of events under typical and prolonged circumstances is presented in figure 3.
Statistical analysis
Before structural analysis and measurement, several preliminary analyses were approved using Statistical Package for the Social Sciences (SPSS) version 25.0 to rule out the possibility of value omissions and clear lines. Descriptive statistics are used by the researchers to examine the participant outcomes. All demographic information has been combined into a single table to illustrate the demographic components and SPSS is used to do a quantitative analysis of frequency. The basic framework is scrutinized after this inquiry in light of the information that was produced.
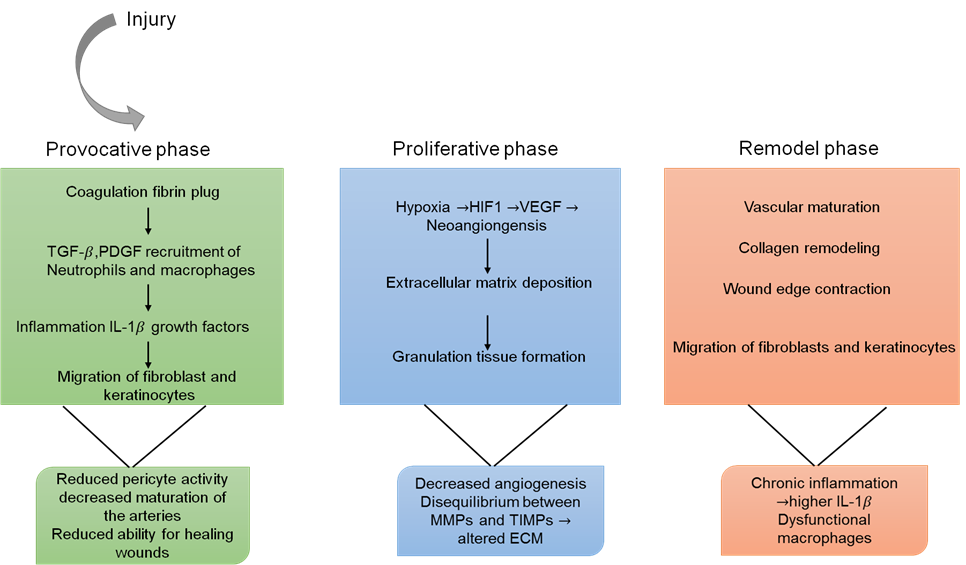
Figure 3. The chronological occurrence of events in physiological wound healing
Insulin
The innovative multicenter, international randomized trial known as Outcome Reduction with Initial Glargine Intervention (ORIGIN) was designed to target people with diabetes, especially those who were at a higher risk of cardiovascular disease and had early-stage Type 2 Diabetes Mellitus (T2DM). This large-scale was to assess and contrast the benefits of early low-insulin therapy with the standard regular care usually provided to high-risk group.(31) The experiment showed that glycemic management, which maintains HbA1c at or above 6,5 %, avoids diabetes development for five years and reduces the microangiopathy in those with HbA1c >6,4 %. Results from the Diabetes Prevention Program Outcome Study (DPPOS) demonstrate a significant 56 % decrease in the incidence of diabetes among high-risk persons who are able to return their pre-disposition glucose levels, emphasizing the critical importance of starting medication early and effectively.(32) It is noteworthy, that the inquiry does not offer precise information about the strategies or techniques used to accomplish this effective return to baseline glucose levels.
Metformin
Biguanide metformin is frequently administered as the first pharmacological intervention for the management of type II diabetes. It is widely accepted as a cornerstone in the therapeutic armament. Its impressive antihyperglycemic properties are supported by a complex mechanism that includes decreased absorption of glucose in the intestines, suppression of hepatic insulin synthesis and enhancement of the absorption of glucose and usage by body's various organs. Metformin's pharmacological profile contains new aspects that have been revealed by empirical findings, exhibiting unique pleiotropic effects. These include increasing the number and caliber of endothelium progenitor cells, which strengthens their defense function in preserving critical organs like the heart and kidneys. Furthermore, as recent research has shown, metformin has antioxidant qualities, inhibits fibrotic processes, and has an anti-proliferative effect.(33) Metformin known by its brand name Glucophage, acts pharmacologically by blocking electron transport at complex 1 of the mtdna chain, which is a crucial process in the synthesis of energy in cells. The complex interactions between these biochemical processes highlight the medication's effectiveness in treating hyperglycemia and suggest that could be useful in treating more general issues related to organ preservation and vascular health. This complex activity makes insulin a potentially effective treatment that goes much beyond its main function in controlling blood sugar levels. It also suggests that metformin can have a role in the overall health of a number of biological processes.
Statins are drugs
Statins possess diverse impacts on biological systems that go beyond their well-known inhibition of wound healing of farnesyl pyrophosphate (FPP) and cortisol synthesis. These drugs prevent the production of these inhibitory substances, but they also regulate the fundamental processes, resulting in a generalized suppression that lessens the accumulation of obesity. Furthermore, the complex physiological profile of statins, keratinocyte progression is inhibited, which places limitations on epithelial growth via binding to glucocorticoid receptors.(34) These substances have significant antibacterial, antioxidant and anti-inflammatory properties by nature, which gives a wide range of medical advantages. Furthermore, it is imperative to emphasize that statins have a noteworthy ability to augment endothelial function, thus promoting beneficial results in tissue repair. The wide-ranging and adaptable characteristics of statins emphasize their usefulness in a variety of therapeutic contexts, underscoring their importance beyond the domain of cholesterol control and highlighting their critical role in regulating diverse processes in cells for enhanced health benefits.
Phenytoin
Approximately 50 % of individuals receiving treatment for phenytoin experience gingival tissue development, a frequent adverse effect of the anticonvulsant medication. Although voltage-dependent Na+ channel blockage is the method by which phenytoin controls seizures nothing is known about the cellular process behind gum thickening. Due to the obvious gingival hypertrophy, phenytoin was directly tested in experimentally produced gingival wounds initially, leading to a rapid transition to skin reparative processes. However, research was done on the molecular mechanisms underlying the effects that were observed. The damaged area becomes stronger as a result of phenytoin's stimulation of granulation tissue development, inhibition of the collagenase movement, and promotion of collagen synthesis and deposition.(35) Lowering the bacterial load in the wound confers antibacterial properties but also requires a careful examination to determine if this impact is an independent result or a byproduct of addressing the inflammatory response, which is shown by a decrease in edema and exudate. Additionally, there is scientific data to bolster the claim that phenytoin injection leadership demonstrates a noteworthy ability to regulate VEGF and FGF at the lesion site, but sets off a critical series of events that are essential for angiogenesis. This complex mechanism that phenytoin orchestrates sets the stage for the start and stimulation of angiogenic processes, which in turn results in the formation of developing blood vessels. A detailed analysis of wound tissue that was treated with phenytoin subsequently provides strong evidence of a reduced inflow of inflammatory cells, an increased level of collagenization, and the coordinated formation of new vascular structures, all of which highlight the therapeutic utility of phenytoin in promoting tissue renewal and repair.
Inhibitors of dipeptidyl peptidase 4 (DPP4)
The transdermal serine aminopeptidase DPP4, often referred to as CD26, cleaves N-terminal the dipeptides in the presence of proline, the hydroxyproline and tyrosine. Its primary known function is the disintegration of enteric-released incretins that regulate the release of insulin. DPP4 quickly deactivates the insulin-releasing function of GLP-1 by specifically cleaving its N-terminal dipeptide. It's interesting to note that DPP4 targets a variety of receptors instead than just GLP1. When the blood sugar goal is not reached after a period of three months of metformin therapy, DPP4 antagonists and GLP1 analogs are two additional therapeutic alternatives that can be added to the program. DPP4 inhibition extends the insulin-secretagogue action of GLP1.(36) Specially beneficial because they are regarded as weight neutral (DPP4 inhibitors) or even have the ability to cause weight reduction (GLP1 analogs) and cause low rates of hypoglycemia. Furthermore, DPP4 is a widely distributed molecule with pleiotropic effects, which makes an appealing target for therapeutic intervention outside of the traditional usage of inhibitors of DPP4 such as antiglycemic medicines.
Recycling drugs to treat and heal wounds
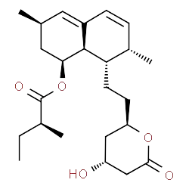
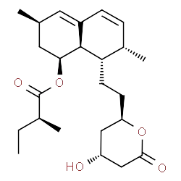
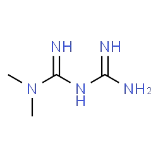
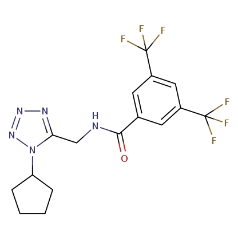
Its recognized function as a reactive material scavenger has led to application in creative wound dressings including naturally produced materials.(37) When compared to the biomaterial used, this combination of substances had a greater wound-repair effect. In addition to the medications listed, there appear to be a number of additional medications in use, which have demonstrated some activity in the wound healing process.(38) In this specific setting, shall focus on a few pharmaceutical classes, including those treat diabetes. Extensive genetic data, in addition to preclinical and clinical trials, supports the potential usefulness of these medications in encouraging successful healing of wounds. Table 3 lists all of their chemical formulae and structure.
|
Table 3. Chemical formulae and structure |
||
|
Chemical organization |
Name |
Chemical Procedure |
|
|
Statins |
C24H36O5 |
|
|
Phenytoin |
C15H11N2NaO2 |
|
|
Metformin |
C4H11N5 |
|
|
DDP-4 inhibitors |
C16H15F5N5O |
The crystalline structure and chemical composition of a drug called the inaugural statin available for sale are displayed.(39) Atorvastatin, Fluvastatin, Pravastatin, Simvastatin, The drug in question is readily available, other medications in the statin class.(40)
CONCLUSIONS
Myofibroblasts are essential for wound healing because they help to constrict the wound and form extracellular matrix (ECM). Diabetes affects how myofibroblasts function, which slows down the healing process in general. Hyperglycemia exacerbates hypoxia-induced harm dysregulates lipolysis, and tampers with the expression of cytokines. This obstacle impedes the complex process of myofibroblast development, which is critical to tissue regeneration and reconstruction. This causes problems with the extracellular matrix's proper adjustment, which is an essential framework that controls the behavior of cells and the architecture of tissues. By generating the required damaged wound conditions for restoration, a comprehension of the role, the cells known as in wound healing for diabetics helps improve the handling of wounds from diabetes that do not heal. There is a noticeable lack of study regarding the activation of myofibroblasts in diabetic wounds, indicating a substantial knowledge gap. Further research is desperately needed to decipher the complex mechanisms by which diabetes affects human myocytes and to clarify the intricate relationship between diabetes and myofibroblast stimulation in the context of wound healing.
BIBLIOGRAPHIC REFERENCES
1. Martinez-Moreno JM, Fontecha-Barriuso M, Martin-Sanchez D, Guerrero-Mauvecin J, Goma-Garces E, Fernandez-Fernandez B, Carriazo S, Sanchez-Niño MD, Ramos AM, Ruiz-Ortega M, Ortiz A. Epigenetic modifiers as potential therapeutic targets in diabetic kidney disease. International journal of molecular sciences. 2020 Jun 9;21(11):4113. DOI: https://doi.org/10.3390/ijms21114113
2. Zullo A, Mancini FP, Schleip R, Wearing S, Klingler W. Fibrosis: Sirtuins at the checkpoints of myofibroblast differentiation and profibrotic activity. Wound Repair and Regeneration. 2021 Jul;29(4):650-66. https://doi.org/10.1111/wrr.12943
3. Dong J, Chen L, Zhang Y, Jayaswal N, Mezghani I, Zhang W, Veves A. Mast cells in diabetes and diabetic wound healing. Advances in therapy. 2020 Nov;37(11):4519-37.DOI: https://doi.org/10.6084/m9.figshare.12911561
4. Bai Q, Han K, Dong K, Zheng C, Zhang Y, Long Q, Lu T. Potential applications of nanomaterials and technology for diabetic wound healing. International journal of nanomedicine. 2020 Dec 3:9717-43. https://doi.org/10.2147/IJN.S276001
5. Lasocka I, Jastrzębska E, Szulc-Dąbrowska L, Skibniewski M, Pasternak I, Kalbacova MH, Skibniewska EM. The effects of graphene and mesenchymal stem cells in cutaneous wound healing and their putative action mechanism. International journal of nanomedicine. 2019 Apr 1:2281-99. https://doi.org/10.2147/IJN.S190928
6. Retamal I, Hernández R, Velarde V, Oyarzún A, Martínez C, Julieta González M, Martínez J, Smith PC. Diabetes alters the involvement of myofibroblasts during periodontal wound healing. Oral Diseases. 2020 Jul;26(5):1062-71. https://doi.org/10.1111/odi.13325
7. Monika P, Waiker PV, Chandraprabha MN, Rangarajan A, Murthy KN. Myofibroblast progeny in wound biology and wound healing studies. Wound Repair and Regeneration. 2021 Jul;29(4):531-47. https://doi.org/10.1111/wrr.12937
8. Poznyak A, Grechko AV, Poggio P, Myasoedova VA, Alfieri V, Orekhov AN. The diabetes mellitus–atherosclerosis connection: The role of lipid and glucose metabolism and chronic inflammation. International journal of molecular sciences. 2020 Mar 6;21(5):1835.DOI: https://doi.org/10.1016/j.actbio.2020.03.035
9. Wang A, Lv G, Cheng X, Ma X, Wang W, Gui J, Hu J, Lu M, Chu G, Chen JA, Zhang H. Guidelines on multidisciplinary approaches for the prevention and management of diabetic foot disease (2020 edition). Burns & trauma. 2020;8:tkaa017. https://doi.org/10.1093/burnst/tkaa017
10. Wong SK, Rangiah T, Bakri NS, Ismail WN, Bojeng EE, Abd Rahiman MA, Soliman AM, Ghafar N, Das S, Teoh SL. The effects of virgin coconut oil on fibroblasts and myofibroblasts on diabetic wound healing. Medicine And Health. 2019 Jan 1;14:132-41. https://doi.org/10.17576/MH.2019.1402.12
11. Eitner A, Culvenor AG, Wirth W, Schaible HG, Eckstein F. Impact of diabetes mellitus on knee osteoarthritis pain and physical and mental status: data from the osteoarthritis initiative. Arthritis care & research. 2021 Apr;73(4):540-8.DOI: https://doi.org/10.1016/j.lfs.2019.04.048
12. Yan Y, Liu X, Zhuang Y, Zhai Y, Yang X, Yang Y, Wang S, Hong F, Chen J. Pien Tze Huang accelerated wound healing by inhibition of abnormal fibroblast apoptosis in Streptozotocin induced diabetic mice. Journal of Ethnopharmacology. 2020 Oct 28;261:113203. DOI: https://doi.org/10.1016/j.jep.2020.113203
13. Braunwald E. Diabetes, heart failure, and renal dysfunction: the vicious circles. Progress in cardiovascular diseases. 2019 Jul 1;62(4):298-302.DOI: https://doi.org/10.1016/j.pcad.2019.07.003
14. La Sala L, Pontiroli AE. Prevention of diabetes and cardiovascular disease in obesity. International journal of molecular sciences. 2020 Oct 31;21(21):8178.DOI: https://doi.org/10.3390/ijms21218178
15. Kato M, Natarajan R. Epigenetics and epigenomics in diabetic kidney disease and metabolic memory. Nature Reviews Nephrology. 2019 Jun;15(6):327-45.DOI: https://doi.org/10.1038/s41581-019-0135-6
16. Wan R, Weissman JP, Grundman K, Lang L, Grybowski DJ, Galiano RD. Diabetic wound healing: The impact of diabetes on myofibroblast activity and its potential therapeutic treatments. Wound Repair and Regeneration. 2021 Jul;29(4):573-81.DOI: https://doi.org/10.1111/wrr.12954
17. Jiang R, Wu S, Fang C, Wang C, Yang Y, Liu C, Hu J, Huang Y. Amino acids levels in early pregnancy predict subsequent gestational diabetes. Journal of Diabetes. 2020 Jul;12(7):503-11.DOI: https://doi.org/10.1111/1753-0407.13018
18. Ghiulai R, Roşca OJ, Antal DS, Mioc M, Mioc A, Racoviceanu R, Macaşoi I, Olariu T, Dehelean C, Creţu OM, Voicu M. Tetracyclic and pentacyclic triterpenes with high therapeutic efficiency in wound healing approaches. Molecules. 2020 Nov 26;25(23):5557. https://doi.org/10.3390/molecules25235557
19. Apolzan JW, Venditti EM, Edelstein SL, Knowler WC, Dabelea D, Boyko EJ, Pi-Sunyer X, Kalyani RR, Franks PW, Srikanthan P, Gadde KM. Long-term weight loss with metformin or lifestyle intervention in the diabetes prevention program outcomes study. Annals of internal medicine. 2019 May 21;170(10):682-90.DOI: https://doi.org/10.7326/M18-1605
20. Guillon C, Ferraro S, Clément S, Bouschbacher M, Sigaudo-Roussel D, Bonod C. Glycation by glyoxal leads to profound changes in the behavior of dermal fibroblasts. BMJ open diabetes research & care. 2021 Apr 26;9(1). DOI: https://doi.org/10.1136%2Fbmjdrc-2020-002091
21. Wilkinson HN, Hardman MJ. Wound healing: cellular mechanisms and pathological outcomes. Open biology. 2020 Sep 30;10(9):200223.DOI: https://doi.org/10.1098/rsob.200223
22. Ma Y, Chen Z, Tao Y, Zhu J, Yang H, Liang W, Ding G. Increased mitochondrial fission of glomerular podocytes in diabetic nephropathy. Endocrine Connections. 2019 Aug 1;8(8):1206-12. DOI: https://doi.org/10.1530/EC-19-0234
23. Bai L, Gao J, Wei F, Zhao J, Wang D, Wei J. Therapeutic potential of ginsenosides as an adjuvant treatment for diabetes. Frontiers in pharmacology. 2018 May 1;9:423. https://doi.org/10.3389/fphar.2018.00423
24. Kalan LR, Meisel JS, Loesche MA, Horwinski J, Soaita I, Chen X, Uberoi A, Gardner SE, Grice EA. Strain-and species-level variation in the microbiome of diabetic wounds is associated with clinical outcomes and therapeutic efficacy. Cell host & microbe. 2019 May 8;25(5):641-55.
25. Afonso AC, Oliveira D, Saavedra MJ, Borges A, Simões M. Biofilms in diabetic foot ulcers: impact, risk factors and control strategies. International journal of molecular sciences. 2021 Jul 31;22(15):8278. https://doi.org/10.3390/ijms22158278
26. Burr SD, Stewart Jr JA. Extracellular matrix components isolated from diabetic mice alter cardiac fibroblast function through the AGE/RAGE signaling cascade. Life Sciences. 2020 Jun 1;250:117569.DOI: https://doi.org/10.1016/j.lfs.2020.117569
27. Makrilakis K. The role of DPP-4 inhibitors in the treatment algorithm of type 2 diabetes mellitus: when to select, what to expect. International journal of environmental health research. 2019 Aug;16(15):2720.DOI: https://doi.org/10.3390/ijerph16152720
28. Larouche J, Sheoran S, Maruyama K, Martino MM. Immune regulation of skin wound healing: mechanisms and novel therapeutic targets. Advances in wound care. 2018 Jul 1;7(7):209-31. https://doi.org/10.1089/wound.2017.0761
29. Polerà N, Badolato M, Perri F, Carullo G, Aiello F. Quercetin and its natural sources in wound healing management. Current Medicinal Chemistry. 2019 Sep 1;26(31):5825-48. https://doi.org/10.2174/0929867325666180713150626
30. Wei P, Zhong C, Yang X, Shu F, Xiao S, Gong T, Luo P, Li L, Chen Z, Zheng Y, Xia Z. Exosomes derived from human amniotic epithelial cells accelerate diabetic wound healing via PI3K-AKT-mTOR-mediated promotion in angiogenesis and fibroblast function. Burns & Trauma. 2020;8:tkaa020. https://doi.org/10.1093/burnst/tkaa020
31. Wolak M, Staszewska T, Juszczak M, Gałdyszyńska M, Bojanowska E. Anti-inflammatory and pro-healing impacts of exendin-4 treatment in Zucker diabetic rats: effects on skin wound fibroblasts. European Journal of Pharmacology. 2019 Jan 5;842:262-9. https://doi.org/10.1016/j.ejphar.2018.10.053
32. Sugimoto K, Murakami H, Deguchi T, Arimura A, Daimon M, Suzuki S, Shimbo T, Yagihashi S. Cutaneous microangiopathy in patients with type 2 diabetes: Impaired vascular endothelial growth factor expression and its correlation with neuropathy, retinopathy and nephropathy. Journal of diabetes investigation. 2019 Sep;10(5):1318-31. DOI: https://doi.org/10.1111/jdi.13020
33. Maloney A, Rosenstock J, Fonseca V. A model‐based meta‐analysis of 24 antihyperglycemic drugs for type 2 diabetes: comparison of treatment effects at therapeutic doses. Clinical Pharmacology & Therapeutics. 2019 May;105(5):1213-23. https://doi.org/10.1002/cpt.1307
34. Ma Q, Li Y, Li P, Wang M, Wang J, Tang Z, Wang T, Luo L, Wang C, Zhao B. Research progress in the relationship between type 2 diabetes mellitus and intestinal flora. Biomedicine & pharmacotherapy. 2019 Sep 1;117:109138. DOI: https://doi.org/10.1016/j.biopha.2019.109138
35. Spampinato SF, Caruso GI, De Pasquale R, Sortino MA, Merlo S. The treatment of impaired wound healing in diabetes: looking among old drugs. Pharmaceuticals. 2020 Apr 1;13(4):60. https://doi.org/10.3390/ph13040060
36. Long M, Cai L, Li W, Zhang L, Guo S, Zhang R, Zheng Y, Liu X, Wang M, Zhou X, Wang H. DPP-4 inhibitors improve diabetic wound healing via direct and indirect promotion of epithelial-mesenchymal transition and reduction of scarring. Diabetes. 2018 Mar 1;67(3):518-31. https://doi.org/10.2337/db17-0934
37. Drankowska J, Kos M, Kościuk A, Marzęda P, Boguszewska-Czubara A, Tylus M, Święch-Zubilewicz A. MMP targeting in the battle for vision: Recent developments and future prospects in the treatment of diabetic retinopathy. Life sciences. 2019 Jul 15;229:149-56. DOI: https://doi.org/10.1016/j.lfs.2019.05.038
38. Kant V, Jangir BL, Sharma M, Kumar V, Joshi VG. Topical application of quercetin improves wound repair and regeneration in diabetic rats. Immunopharmacology and immunotoxicology. 2021 Sep 3;43(5):536-53. https://doi.org/10.1080/08923973.2021.1950758
39. Ayele AA, Tegegn HG, Ayele TA, Ayalew MB. Medication regimen complexity and its impact on medication adherence and glycemic control among patients with type 2 diabetes mellitus in an Ethiopian general hospital. BMJ open diabetes research & care. 2019 Jun 28;7(1).DOI: https://doi.org/10.1136%2Fbmjdrc-2019-000685
40. Oguntibeju OO. Medicinal plants and their effects on diabetic wound healing. Veterinary world. 2019 May 11;12(5):653. DOI: https://doi.org/10.14202%2Fvetworld.2019.653-663
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Harsh Bhati, Manashree Mane, Vinima Gambhir, Jyoti Prakash Samal, Vundela Swathi, Jagmeet Sohal, Saksham Sood.
Data curation: Harsh Bhati, Manashree Mane, Vinima Gambhir, Jyoti Prakash Samal, Vundela Swathi, Jagmeet Sohal, Saksham Sood.
Formal analysis: Harsh Bhati, Manashree Mane, Vinima Gambhir, Jyoti Prakash Samal, Vundela Swathi, Jagmeet Sohal, Saksham Sood.
Drafting - original draft: Harsh Bhati, Manashree Mane, Vinima Gambhir, Jyoti Prakash Samal, Vundela Swathi, Jagmeet Sohal, Saksham Sood.
Writing - proofreading and editing: Harsh Bhati, Manashree Mane, Vinima Gambhir, Jyoti Prakash Samal, Vundela Swathi, Jagmeet Sohal, Saksham Sood.