doi: 10.56294/mw2024532
Examining Advances Challenges and Patient Outcomes in Immunotherapy for Cancer Treatment
Examen de los avances, retos y resultados para los pacientes en inmunoterapia para el tratamiento del cáncer
Pragati
Aniket Manoli1 ![]() *,
Snigdha Pattnaik2
*,
Snigdha Pattnaik2 ![]() , Debanjana Prasad3
, Debanjana Prasad3 ![]() , Manashree Mane4
, Manashree Mane4 ![]() , Vinima Gambhir5
, Vinima Gambhir5 ![]() , C.Bharanidharan6
, C.Bharanidharan6 ![]() , Sumeet Kaur7
, Sumeet Kaur7 ![]()
1Department of Microbiology, KLE Jagadguru Gangadhar Mahaswamigalu Moorusaavirmath Medical College, Huballi KLE Academy of Higher Education and Research. Karnataka, India.
2Department of Pharmaceutical Sciences, Siksha ‘O’ Anusandhan (Deemed to be University). Bhubaneswar, Odisha, India.
3Department of Biotechnology, Noida International University. Greater Noida, Uttar Pradesh, India.
4Forensic Science, JAIN (Deemed-to-be University). Bangalore, Karnataka, India.
5Department of ISME, ATLAS SkillTech University. Mumbai, Maharashtra, India.
6Department
of artificial intelligence and data science, Panimalar engineering college.
Chennai, India.
7Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
Cite as: GAniket Manoli P, Pattnaik S, Prasad D, Mane M, Gambhir V, Bharanidharan C, et al. Examining Advances Challenges and Patient Outcomes in Immunotherapy for Cancer Treatment. Seminars in Medical Writing and Education. 2024; 3:532. https://doi.org/10.56294/mw2024532
Submitted: 10-11-2023 Revised: 26-02-2024 Accepted: 19-06-2024 Published: 20-06-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Pragati Aniket Manoli *
ABSTRACT
Immunotherapy has changed the way cancer is treated and given people with many types of cancer new hope. Immunotherapy works very well on some types of tumors, like melanoma, lung cancer, and blood diseases, by using the body’s immune system to find and attack cancer cells. This abstract talks about the progress made in immunotherapy, the problems that come up when it is used, and how it affects the results for patients. New developments in immunotherapy include immune checkpoint inhibitors, CAR T-cell treatment, and monoclonal antibodies. These have made a big difference in many patients’ chances of surviving and quality of life. These treatments can have long-lasting effects, even on cancer that is very far along, showing that long-term recovery is possible. Clinical studies have increased the conditions that these treatments can treat, which has led to the approval of a number of new drugs and combining tactics that make them work better. Even with these improvements, the area of immunotherapy still has a ways to go. The reaction of patients is very different; some people get big benefits, while others show little or no response. Tumor variety, the tumor microenvironment, and the presence of immune-suppressing processes are some of the things that affect this variation. Additionally, dealing with immune-related side effects is very hard. To reduce toxicity without losing therapy effectiveness, careful tracking and treatment plans are needed. Access to immunotherapy is still a problem because some people can’t get these medicines because they are too expensive, not available, or don’t meet certain requirements. Inequalities in access to care can lead to unequal results from treatment.
Keywords: Immunotherapy; Cancer Treatment; Patient Outcomes; Immune Checkpoint Inhibitors; Adverse Events; Treatment Response Variability.
RESUMEN
La inmunoterapia ha cambiado la forma de tratar el cáncer y ha dado nuevas esperanzas a las personas con muchos tipos de cáncer. La inmunoterapia funciona muy bien en algunos tipos de tumores, como el melanoma, el cáncer de pulmón y las enfermedades de la sangre, utilizando el sistema inmunitario del organismo para encontrar y atacar las células cancerosas. Este resumen habla de los avances en inmunoterapia, los problemas que surgen cuando se utiliza y cómo afecta a los resultados para los pacientes. Los nuevos avances en inmunoterapia incluyen los inhibidores del punto de control inmunitario, el tratamiento con células T CAR y los anticuerpos monoclonales. Estos tratamientos han supuesto una gran diferencia en las posibilidades de supervivencia y la calidad de vida de muchos pacientes. Estos tratamientos pueden tener efectos duraderos, incluso en cánceres muy avanzados, lo que demuestra que la recuperación a largo plazo es posible. Los estudios clínicos han aumentado las afecciones que pueden tratar estos tratamientos, lo que ha llevado a la aprobación de una serie de nuevos fármacos y a la combinación de tácticas que hacen que funcionen mejor. Incluso con estas mejoras, el área de la inmunoterapia aún tiene camino por recorrer. La reacción de los pacientes es muy diferente; algunas personas obtienen grandes beneficios, mientras que otras muestran una respuesta escasa o nula. La variedad del tumor, el microentorno tumoral y la presencia de procesos inmunosupresores son algunos de los factores que influyen en esta variación. Además, es muy difícil hacer frente a los efectos secundarios relacionados con el sistema inmunitario. Para reducir la toxicidad sin perder eficacia terapéutica, es necesario un seguimiento y unos planes de tratamiento cuidadosos. El acceso a la inmunoterapia sigue siendo un problema porque algunas personas no pueden obtener estos medicamentos porque son demasiado caros, no están disponibles o no cumplen ciertos requisitos. Las desigualdades en el acceso a la atención pueden dar lugar a resultados desiguales del tratamiento.
Palabras clave: Inmunoterapia; Tratamiento del Cáncer; Resultados en Pacientes; Inhibidores del Punto de Control Inmunitario; Efectos Adversos; Variabilidad de la Respuesta al Tratamiento.
INTRODUCTION
In the past few years, immunotherapy has become a revolutionary way to treat cancer, completely changing the field of oncology. This new treatment uses the immune system's power to find and kill cancer cells. It gives patients who may not react to standard treatments like radiation and chemotherapy a new option. The creation of new immunotherapeutic methods, such as safe checkpoint inhibitors, CAR T-cell treatment, and monoclonal antibodies, has enormously progressed persistent comes about, particularly for cancers that were once thought to be serious. Even though there has been a part of advance, there are still some issues that make immunotherapy less compelling and harder to get. The discovery of immune checkpoint drugs is one of the foremost critical steps forward in immunotherapy. These medicines work by halting proteins that halt the resistant system from reacting properly. This makes it less demanding for the body to discover and murder cancer cells. Drugs like pembrolizumab and nivolumab are exceptionally great at treating melanoma and non-small cell lung cancer, getting long-lasting reactions and raising survival rates.(1) Within the same way, CAR T-cell treatment has changed the way blood cancers are treated. Intense lymphoblastic leukemia and some sorts of lymphoma have been treated exceptionally effectively with CAR T-cell treatment, which changes a patient's possess T cells so they can spot and fight cancer cells. These enhancements have had a colossal effect on how well patients have done. Numerous individuals who had terrible guesses within the past are presently living longer and having way better quality of life. Immunotherapy has the control to not as it were get rid of tumors but moreover to give patients long-lasting remissions, as seen in cases where patients don't have cancer for years after treatment. Figure 1 shows the progress, problems, and results for patients in cancer treatment. It shows how immune checkpoint drugs, CAR-T cell treatment, and custom vaccinations have made progress. Toxicity and resistance are two problems. Immunotherapy has the ability to completely change how cancer is treated, as shown by its positive effects on survival rates and quality of life.
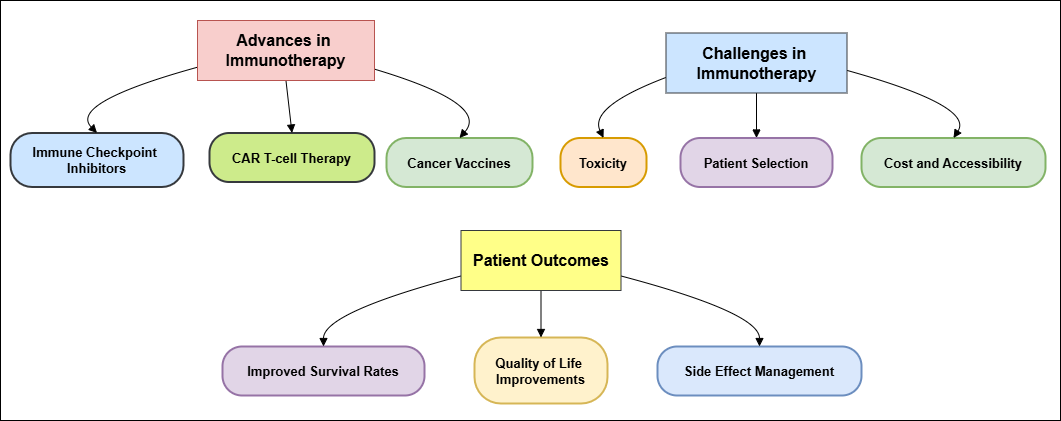
Figure 1. Advances, Challenges, and Patient Outcomes in Immunotherapy for Cancer Treatment
Cancer management has been revaluated in light of this worldview move in treatment. This shows how vital personalized medication is and how vital it is to form treatment plans that are interesting to each quiet and their illness. Indeed with these positive changes, there are still a few issues with putting immunotherapy into hone. One huge issue is that patients do not continuously react well to treatment. Be that as it may, whereas a few individuals have astounding impacts, others may not react at all. This instability is caused by a number of things, such as the distinctive sorts of tumors, the tumor's environment, and the patient's safe framework. To improve response rates and make treatment plans work superior, it's imperative to get it these things. Immunotherapy can cause the immune framework to react as well emphatically, which can have a number of side effects on the skin, GI tract, and endocrine organs, among other organs. These terrible things can happen now and then and are so terrible that they got to be taken note and managed with right absent. A very critical thing for specialists to think around is how to adjust the effectiveness of immunotherapy with how to handle its side impacts.(2) Another big issue is getting people get to immunotherapy. These medications can spare lives, but numerous patients can't get them since they are as well costly and got to be given and observed over by restorative experts in a certain way. Disparities can get more regrettable when individuals have different get to health care, particularly in neglected areas. It is important to fix these issues so that all cancer patients can gain from advance in care.
Background work
Immunotherapy is an important part of treating cancer that was made possible by decades of study into how the immune system can fight cancer. Surgery, chemotherapy, and radiation therapy were the main types of cancer treatments in the past, but they didn't always work and had a lot of bad side effects. In the late 20th century, researchers begun to realize that the safe framework can actually discover and kill abnormal cells. Finding immune checkpoints, which are control forms that keep safe tolerance and stop infection, could be a big step forward in this area. Finding proteins like CTLA-4 and PD-1 as imperative parts of these pathways driven to the improvement of modern medicines that try to stop these checkpoints. The discovery of resistant checkpoint inhibitors was a big step forward in the treatment of cancer. After clinical considers showed that drugs like ipilimumab (a CTLA-4 inhibitor) and pembrolizumab (a PD-1 inhibitor) worked, they were approved and included to standard care for a number of distinctive sorts of cancer. The creation of CAR T-cell treatment is another vital step forward in immunotherapy.(3) To utilize this strategy, the T cells of a persistent are hereditarily changed so that they create chimeric antigen receptors (CARs), which make them superior at focusing on particular tumor antigens. Since CAR T-cell treatment works so well, particularly for treating blood cancers like acute lymphoblastic leukemia and a few lymphomas, it has become a major change in how cancer is treated.
The reality that cellular treatments can cause long-lasting reductions in cancer patients who have attempted all other medicines has appeared how valuable they can be in oncology. The number of immunotherapeutic choices has moreover grown thanks to continuing investigate into tumor-infiltrating lymphocytes (TILs), monoclonal antibodies, and cancer medicines. Analysts examining the tumor microenvironment have learned how tumors stow away from the safe framework. This has driven to plans to alter the tumor environment to form the safe framework work superior. Indeed with these advancements, immunotherapy has had its share of issues along the way. Issues like harmful impacts of medications, conflicting quiet responses, and unequal get to care make it clear that more ponder and unused thoughts are required. For immunotherapy to move forward, we need to get it how these problems work. This will make medicines for cancer more effective and simpler for individuals to urge.(4) In general, the foundation work in immunotherapy appears how analysts from diverse areas have worked together to create big changes in how cancer is treated and how well patients do.
|
Table 1. Summary of Background Work |
|||
|
Study/Work |
Key Finding |
Challenges |
Impact |
|
Pembrolizumab in Melanoma |
Significant improvement in survival rates in advanced melanoma |
IrAEs (immune-related adverse events) leading to treatment discontinuation |
Enhanced survival and QoL, but with side effects limiting use |
|
Combination of Pembrolizumab & Chemo |
Higher 1-year survival in NSCLC compared to chemotherapy alone |
Increased rate of severe side effects and toxicity |
Improved survival, but need for better side effect management |
|
CAR T-Cell Therapy in ALL(5) |
High remission rates in relapsed/refractory leukemia patients |
High incidence of severe adverse events (e.g., cytokine release syndrome) |
Revolutionary treatment for blood cancers with long-term impact |
|
Atezolizumab in Bladder Cancer |
Increased survival in advanced bladder cancer patients |
Limited response in some patient subgroups |
Promising option, but less effective in certain populations |
|
Ipilimumab in Melanoma |
Durable responses in some melanoma patients |
Immune evasion by tumors, leading to resistance |
Potential for long-term remission in select patients |
|
Durvalumab in NSCLC |
Improved progression-free survival in combination with chemotherapy |
Cost and accessibility, plus possible immune-related toxicity |
Significant survival benefit, particularly in late-stage disease |
|
Nivolumab for Renal Cell Carcinoma(6) |
High efficacy in advanced renal cancer |
Development of resistance in long-term use |
Improved survival and quality of life for kidney cancer patients |
|
Combination Immunotherapy in Lung Cancer |
Combination of PD-1 inhibitors and chemotherapy improves survival |
High toxicity and risk of autoimmune diseases |
Better outcomes for advanced lung cancer with personalized care |
|
Tisagenlecleucel in Leukemia |
CAR T-cell therapy showed long-term remission in pediatric leukemia |
High risk of cytokine release syndrome and neurological toxicity |
Transformative treatment with curative potential for pediatric ALL |
|
Checkpoint Inhibitors in HNSCC |
Survival benefit in head and neck squamous cell carcinoma |
Inconsistent responses, need for biomarkers to predict efficacy |
Breakthrough in treatment for head and neck cancers |
|
Adoptive T-cell Therapy in Breast Cancer(7) |
Modest success in HER2-positive breast cancer |
Difficulty in expanding T-cells and tumor resistance |
Potential for targeted treatment, but still in early phases |
|
Immune Checkpoint Inhibitors in Colorectal Cancer |
Improved survival in mismatch repair-deficient colorectal cancer |
Low efficacy in mismatch repair-proficient tumors |
High promise in genetic-based therapies for specific cancers |
|
Vaccine Therapy in Prostate Cancer |
Vaccines show potential to stimulate immune response in prostate cancer |
Limited efficacy and difficulty in inducing strong immune responses |
Offers new direction in cancer immunotherapy, but needs refinement |
Advances in immunotherapy
Types of immunotherapy
Immunotherapy includes a wide range of cancer treatments that use the immune system to fight the disease. Immunotherapy comes in many forms, each with its own special effects and advantages. Some of the main ones are immune checkpoint inhibitors, CAR T-cell therapy, monoclonal antibodies, cancer vaccines, and oncolytic virus treatment.
CAR T-cell Therapy
Chimeric antigen receptor (CAR) T-cell treatment includes taking out and changing the genes of a patient's T cells so that they produce CARs that specifically target tumor proteins. This new way of treating blood cancers, like acute lymphoblastic leukemia and some lymphomas, has made a huge difference, and many patients now have completely cured their cancers after treatment.(8)
Monoclonal Antibodies
These molecules are made in a lab and can bind directly to cancer cells, telling the immune system to kill them. Some examples are rituximab, which is used to treat certain types of lymphomas, and trastuzumab, which is used to treat HER2-positive breast cancer. Monoclonal antibodies can also carry deadly drugs straight to cancer cells, which makes treatment more effective.
Cancer Vaccines
Unlike other vaccines, which aim to keep people from getting sick, cancer vaccines try to get the immune system to attack tumors that are already there. Some therapeutic vaccines, like sipuleucel-T for prostate cancer, have shown hope in getting the immune system to fight cancer cells.(9)
Oncolytic Virus Therapy
Oncolytic virus therapy is a new method that uses genetically modified viruses to target and kill cancer cells while also boosting the immune system. One example is Talimogene laherparepvec (T-VEC), which is allowed to treat cancer.
Recent developments in research
Recent progress in immunotherapy research has helped us learn a lot more about how to make immune reactions against cancer work better. Combination therapies, in which immunotherapy is used along with more common treatments like chemotherapy, radiation, or targeted therapy, are one of the most important changes. Studies have shown that immune checkpoint inhibitors and chemotherapy can work better together, especially in non-small cell lung cancer and triple-negative breast cancer. The goal of this approach is to use synergistic effects to make the immune system's reaction stronger and last longer. Finding predictive factors that can help doctors figure out which patients are most likely to benefit from certain immunotherapies is another area of study that looks very hopeful. Recent progress in genetic screening and tumor microenvironment research has led to the finding of biomarkers like PD-L1 expression and the number of mutations in a tumor.(10) These factors help doctors customize treatment plans so that patients get medicines that work best for their specific tumors. This improves results and reduces side effects that aren't needed. Additionally, there has been a rise in the study of how immunotherapy can be defeated. To make medicines that work better, we need to know why some people don't react to treatment or whose disease gets worse after the first response.
Case studies of successful immunotherapy applications
Multiple sorts of cancer have reacted exceptionally well to immunotherapy, as shown by a number of well-known case considers. As an case, pembrolizumab is utilized to treat progressed melanoma. It is an resistant checkpoint medicate that targets PD-1. A 45-year-old man with progressed melanoma was the subject of a case think about. After getting pembrolizumab, the tumor shrank significantly. This individual had attempted a few treatments in the past without much victory. But after beginning immunotherapy, they had a long-lasting response and have been cancer-free for over three a long time.(11) This case appears that checkpoint inhibitors may be able to help patients who have attempted all other medicines fall flat to get better. Hematological tumors can be treated with CAR T-cell treatment, which is another solid case. A case ponder of a 12-year-old boy with repeating intense lymphoblastic leukemia (ALL) appears how this strategy can alter things. The quiet failed typical treatment, so they had CAR T-cell treatment that focused on the CD19 marker. Inside some weeks, the patient had full recuperation, and after five a long time of long-term follow-up, there were no signs of return. In this case, the victory of CAR T-cell treatment in kids is appeared, together with its capacity to give long-lasting comes about in intense circumstances. Nivolumab, another PD-1 inhibitor, has been appeared to work well in strong tumors to treat non-small cell lung cancer (NSCLC). Imaging tests appeared that the development had shrunk a lot, and the patient said that their quality of life had gotten way better.(12) This case appears that immunotherapy can be a good choice indeed when the infection is exceptionally distant along, giving trust to individuals who do not have numerous other treatment options. These case studies appear how immunotherapy can alter the course of different types of cancer.
METHOD
Research design
When it comes to investigate planning, the choice between subjective and quantitative strategies includes an enormous effect on how a think about is done and what it finds. Each strategy is sweet for a distinctive kind of study address and serves a diverse reason. The most objective of subjective study is to discover out around and get it people's subjective feelings, reasons, and sees. A part of the time, interviews, center groups, and individual observations are utilized to induce deep and wealthy information for this reason. Analysts utilize these strategies to get subtle bits of knowledge that appear how complicated social occasions and human behavior are. For case, subjective research can be exceptionally accommodating when looking into how immunotherapy influences patients since it lets analysts discover individual stories, passionate responses, and things that make treatment harder. This level of information can offer assistance healthcare experts do their employments superior and make patient-centered care superior.(13) Quantitative study, on the other hand, involves gathering and analyzing numbers to discover designs, relationships, and factual noteworthiness. This way of doing things employments organized devices like surveys, tests, and statistical investigations to create beyond any doubt that that comes about are objective and can be repeated. Analysts can test speculations and draw conclusions from a bigger test estimate utilizing quantitative strategies, which grant them a bigger picture of an occasion. For occurrence, a quantitative consider might see at how well a certain immunotherapy treatment works for a enormous group of patients by using statistical strategies to look at treatment response and life rates. Patterns and associations can be found more effectively with this strategy, which makes a difference the development of evidence-based strategies.(14) A parcel of the time, the goals of the think about determine whether to utilize subjective or quantitative investigate.
Data collection methods
Clinical trial data
Clinical studies are an critical portion of restorative ponder, particularly when it comes to making and testing modern medications, like immunotherapy for cancer. These studies are carefully arranged to accumulate data that can offer assistance us get it how well, securely, and by and large modern medicines influence patient results.(15,16) There are diverse sorts of information that are assembled amid clinical studies, such as personal data, clinical goals, and safety reviews. When individuals take part in clinical thinks about, organized overviews and case report forms (CRFs) are frequently utilized to urge fundamental individual data like age, sex, race, and health history. This data helps analysts make sure that the study population is obvious and normal, so they can see at results for a run of ethnic groups.(17) Also, collecting clinical outcomes like total survival, progression-free survival, and reaction rates is very important for figuring out how well the intervention works as a treatment. A lot of the time, objective measures like imaging studies and lab tests are used to check for these goals because they give us measurable information about how well the treatment worked. Another important part of collecting data in clinical studies is making sure that the participants are safe. Adverse events connected to the intervention are carefully recorded and sorted by how bad they were and how they relate to the treatment. This information is very important for knowing the risk profile of a new treatment because it tells regulators and doctors about possible side effects and how to treat them. Patient-reported outcomes (PROs) are also often used in clinical studies to get subjects' individual thoughts on their quality of life, complaints, and treatment happiness.(18)
Patient surveys and interviews
Questionnaires and conversations with patients are important types of qualitative study that are used to learn more about how patients feel about their care, especially when it comes to immunotherapy for cancer. These methods give useful information that can be added to clinical results to get a fuller picture of the patient's journey and how care affects their quality of life. Surveys are organized tools that are used to get standard information from a big group of people. They can be given in a number of different ways, such as on paper, online, or over the phone. Most surveys have closed-ended questions that let you see at the numbers behind answers approximately treatment joy, overseeing side effects, and common wellbeing.(19) With built up devices just like the EQ-5D or the Utilitarian Appraisal of Cancer Treatment (Reality), analysts can discover out how immunotherapy influences patients' quality of life and how they can go approximately their everyday lives. On the other hand, interviews are a more individual way to gather information. They can be drained individual or online, and the open-ended questions make it easier for individuals to conversation approximately their sentiments, considerations, and encounters in more profundity. This qualitative strategy lets analysts see into complicated subjects like how individuals feel around treatment, what stops them from getting care, and how a cancer conclusion influences their mental wellbeing. Interviews can moreover uncover patterns that studies might miss. This gives analysts more data that can help them improve patient-centered care and professional practices. Overviews and discussions are both exceptionally critical for finding out what patients think and need approximately immunotherapy.(20) Analysts can get a more total picture of how treatment works by combining these qualitative methods with quantitative clinical information. This will inevitably lead to better patient results, more personalized treatment, and better communication between patients and healthcare workers.
Data analysis techniques
Statistical analysis
A key part of numerous research strategies is factual investigation. This is often particularly genuine in clinical studies, where it is utilized to analyze information and come to valuable conclusions. Utilizing distinctive factual strategies on numeric information from tests, polls, or clinical trials is what this handle is all about. It lets analysts see how variables are related, how they change, and what patterns they are appearing. The main reason of measurable examination is to discover data that can offer assistance specialists make decisions and offer assistance individuals superior get it how treatments work. Clear insights are one of the foremost imperative parts of factual investigation. They describe and organize information to grant a clear picture of the study group. Mean, median, mode, standard deviation, and recurrence conveyances are all sorts of expressive insights.(21) Researchers use these measures to get a fundamental idea of their information before moving on to more complicated considers. They help them see the main patterns and differences in the information. On the other hand, inferential statistics let analysts draw wide conclusions approximately a community from a little set of information. To discover out in case contrasts seen between bunches are factually critical, strategies like t-tests, chi-square tests, and ANOVA are frequently utilized. According to an illustration, analysts might utilize these tests to see if any changes in response rates are greater than what would be predicted by chance in clinical considers that test the viability of immunotherapy. Too, relapse examination could be a strong tool for looking at how factors are related to each other. This helps analysts discover factors that can foresee comes about and make sure that other components do not get within the way.
Step-wise process for Statistical Analysis
Step 1: Data Collection and Preparation
The first step involves collecting and preparing the data for analysis. This includes organizing the data, checking for missing values, and ensuring the data is in the correct format for the analysis.
Mathematical Representation: Let the dataset be represented as X = {x1, x2,...,xn}
Where:
xi represents individual data points.
n is the total number of observations.
Step 2: Descriptive Statistics Calculation
In this step, key statistical measures such as the mean, variance, and standard deviation are computed to summarize the dataset.
Mean:
The arithmetic mean μ of the data is calculated as:
![]()
Variance
The variance σ² is calculated as:
![]()
Standard Deviation
The standard deviation σ is the square root of variance:
![]()
Step 3: Hypothesis Testing
In hypothesis testing, the null hypothesis (H₀) is compared against an alternative hypothesis (H₁) to determine if there is enough evidence to reject H₀. A commonly used statistical test is the t-test, which compares means of two samples.
t-Test Statistic:
The t-statistic is calculated as:
Where:
· x̄₁, x̄₂ are the sample means,
· s₁², s₂² are the sample variances,
· n₁, n₂ are the sample sizes.
Step 4: Model Fitting and Regression Analysis
After hypothesis testing, the next step is to fit a statistical model to the data. Linear regression is often used for analyzing the relationship between independent and dependent variables.
Linear Regression Equation:
The relationship between the dependent variable y and independent variable x is modeled as:
![]()
Where:
· y is the dependent variable.
· x is the independent variable.
· β₀ is the intercept.
Thematic analysis for qualitative data
A lot of people use thematic analysis to look at qualitative data. It lets scholars find trends (themes) in the data and report on them in a structured way. This way works especially well in healthcare, where knowing patients' feelings, thoughts, and actions is important for making care and treatment better, especially when it comes to chemotherapy for cancer patients. Researchers can use thematic analysis on different kinds of qualitative data, like answers to open-ended surveys, interviews, and focus groups, because it is very flexible. One of the first steps in topic analysis is familiarization. This is when experts really look at the data and try to understand what it all means.(22) As a first step, read and reread the transcripts, making notes on your first thoughts and possible themes. After getting to know the data, researchers begin coding, which means organizing it in a way that makes sense and captures important traits that are relevant to the research questions. Coding can be done either straight from the data, which is called inductive coding, or based on ideas or models that already exist, which is called logical coding. After coding is done, experts move on to theme development, which is the process of putting together linked codes into bigger themes that cover the most important results. At this stage, researchers may need to go back and look at the data again to make sure that the themes they found are a good picture of the experiences of the subjects.
Challenges in immunotherapy
Mechanisms of resistance
Immunotherapy for cancer treatment has come a long way, but one of the greatest issues is still the forms of resistance that make these treatments less successful. Immunotherapy can be safe to a number of organic and microenvironmental components. These can make treatment less viable and make it harder for patients to get long-lasting results. One important way that resistance works is through the tumor microenvironment, which can make a setting that debilitates resistant responses and makes them less compelling. Tumors can discharge distinctive hormones and development variables that bring in administrative T cells (Tregs) and myeloid-derived silencer cells (MDSCs). These cells halt effector T cells from doing their work. This impact not as it were makes it harder for the safe framework to discover and kill cancer cells, but it can moreover offer assistance the tumor grows. Tumor heterogeneity is another imperative calculate that contributes to resistance. This implies that diverse cancer cells inside the same tumor have distinctive hereditary and phenotypic characteristics. Since of this assortment, bunches of cancer cells that are less likely to reply to immunotherapy may shape. For example, contrasts in how antigens are communicated on tumor cells might make it so that the resistant framework doesn't recognize and battle all cancer cells, which lets safe clones live and increase. Furthermore, changes in safe defense circuits can make treatment even less effective. Immune checkpoint inhibitors try to boost T cell activity by stopping proteins like PD-1 and CTLA-4. However, tumors may find other ways to avoid being found by the immune system. It's possible for different immunity checkpoints or co-inhibitory molecules to become more active, which can lower T cell reactions even when these treatments are present.
Adverse effects and patient safety
Immunotherapy has changed the way cancer is treated, but it also has some risks. Knowing about these risks is important for keeping patients safe. Bad effects can be mild to serious, and they can have a big effect on the patient's quality of life and ability to stick with their treatment. Some common side impacts of immunotherapy are tiredness, skin responses, and flu-like symptoms. With compassionate care, these impacts are frequently well controlled. The more critical issue with immunotherapy, though, is that it can cause immune-related adverse events (irAEs). These happen when the body's resistant system attacks sound cells by mishap, causing swelling and harm in numerous organs. Skin (causing rashes or skin inflammation), GI tract (causing colitis), endocrine glands (causing thyroiditis or adrenal disappointment), and lungs (causing pneumonitis) are a few of the foremost common places it influences. These reactions can run from mild symptoms that need to be observed to conditions that are life-threatening and need to be hospitalized and closely overseen. Due to the possibility of major side impacts, patients who are getting immunotherapy must be closely watched. Oncologists have to be educating their patients a part about possible side impacts and make beyond any doubt they have clear ways to induce in touch with them in case their side effects alter or get more regrettable. For irAEs to be overseen well, they ought to be found and treated rapidly. Regularly, corticosteroids or immunosuppressive drugs are required to ease indications and get the safe system back in adjust. When it comes to patient security, you also need to think almost conditions and the patient's general health. In case you already have an incendiary condition, you may be more likely to induce irAEs. This implies that you got to be carefully evaluated and your treatment plans may need to be changed.
Accessibility and cost issues
Immunotherapy has become a revolutionary way to treat cancer, but problems with access and cost make it hard to use by many people. Many patients can't get immunotherapy because it's so expensive. This means that treatment availability is different for people based on their income, insurance coverage, and where they live. Immunotherapy costs a lot of money in many ways. New immunotherapeutic drugs, like immune checkpoint inhibitors and CAR T-cell therapies, can cost more than a hundred thousand dollars for a full course of treatment. Often, these prices cover not only the medicines themselves, but also costs connected to them, like diagnostic tests, tracking, and possibly taking care of side effects. These financial requests can be too much for numerous individuals, particularly those who do not have enough insurance or who have a part of out-of-pocket costs. Since of this, some patients may not get care or may put it off, which could hurt their chances of getting better. Aside from the coordinate prices of treatment, contrasts within the framework of healthcare make it indeed harder for a few individuals to get offer assistance. It might be difficult for individuals in provincial or destitute places to induce to specialized locales that donate immunotherapy. Multidisciplinary groups are required to carry out and keep an eye on these medications. This takes more assets and information, which might not be accessible all over in healthcare. This injustice based on area can cause individuals to hold up longer for treatment and have worse health impacts.
Regulatory hurdles
Regulatory problems make it hard for immune treatments for cancer to get better and be available to more people. Before they can be cleared for clinical use, new treatments have to go through a lot of tests to make sure they are safe, effective, and of good quality. Regulatory bodies like the European Medicines Agency (EMA) and the U.S. Food and Drug Administration (FDA) have set up thorough ways to evaluate new treatments, which can make the clearance process long and hard to understand. One of the biggest problems with governmental approval is that new immunotherapies have to go through a lot of tests to show that they work and are safe. There are usually more than one part to these trials. Phase I trials check to see if the drug is safe, Phase II trials see if it works at first, and Phase III trials compare it fully to normal treatments. This multi-step process can take years to finish, which delays patients' access to treatments that could save their lives. Also, because immunotherapy is always changing, legal standards need to be updated all the time to reflect new ways that medicines work and the unique side effects that come with them. Another problem is that strong biomarkers need to be found and proven in order to predict how patients will respond to immunotherapy. Regulatory agencies need proof that certain biomarkers can accurately show which patients will gain most from a certain treatment. This condition could make the development process take longer while experts look for and confirm these marks.
Patient outcomes
Survival rates and long-term effects
Immunotherapy has made a big difference in how well cancer patients do, especially when it comes to survival rates and long-term effects. Immunotherapy has been shown in many studies to greatly improve both total survival and progression-free survival. This is especially true for cancers that didn't have many treatment choices in the past, like melanoma, lung cancer, and some types of blood cancer. For example, patients with advanced melanoma who were given immune checkpoint drugs like pembrolizumab and nivolumab have had very high rates of long-term mortality compared to past statistics. According to clinical studies, a lot of patients have long-lasting reactions, and some even have long-term remissions that last for years. This is different from standard treatments, which often didn't help people live for a long time. Immunotherapy has also shown potential in lung cancer, especially non-small cell lung cancer (NSCLC). Studies show that people who get combo treatments with checkpoint inhibitors have longer total mortality rates than people who only get regular chemotherapy.
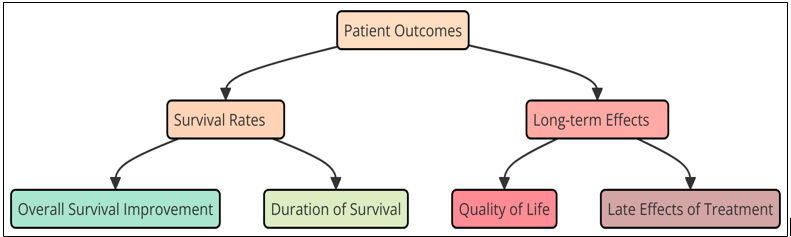
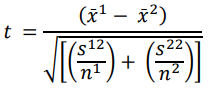
Figure 2. Patient Outcomes" with subcategories for "Survival Rates" and "Long-term Effects
Figure 2 shows how cancer patients do after treatment, with a focus on two main groups: Survival Rates and Long-Term Effects. It talks about how new treatments have led to higher survival rates and also looks at long-term effects like quality of life, lingering toxins, and prolonged recovery, giving a full picture of the therapeutic effect. But knowing the long-term benefits is very important for fully assessing how immunotherapy affects patient results. There are worries about the long-term presence of immune-related adverse events (irAEs), even though many patients report big improvements. Some people may have long-term side effects that lower their quality of life, like thyroid problems, skin problems, or stomach problems. To make sure that people keep up a good quality of life, these long-term effects need to be managed with ongoing follow-up and a multidisciplinary approach.
Quality of life considerations
Quality of life (QoL) is an important thing to think around when looking at distinctive cancer treatments, such as immunotherapy. It is well known that immunotherapy can increment mortality rates and cause tumor reactions. However, it is fair as vital to know how it influences patients' daily lives, mental health, and common happiness with their care. As immunotherapy gets to be more common, measuring QoL is important for making choices almost treatment and progressing care for patients. Managing side effects, particularly immune-related antagonistic occasions (irAEs), is an vital portion of moving forward the quality of life for individuals who are getting immunotherapy. These side impacts can be mellow to genuine, and they may happen in many organ frameworks, such as the skin, the stomach related framework, and the endocrine framework. The appearance of irAEs can have a enormous impact on a patient's wellbeing and capacity to do day by day errands. For illustration, digestive problems like colitis can be agonizing and make it difficult to eat right, and skin reactions can have an impact on self-esteem and social intuitive. So, taking great care of these side impacts is exceptionally important for moving forward patients' quality of life. It's too vital not to disregard around the mental and enthusiastic viewpoints of managing with cancer and getting treatment. Patients may feel on edge, discouraged, or uncertain almost their viewpoint, particularly on the off chance that they have to follow a complicated treatment arrange. Immunotherapy can make individuals feel a part of diverse feelings. Patients may be energized almost its guarantee whereas too having to bargain with the issues that come with the treatment.
RESULTS AND DISCUSSION
Immunotherapy has made a big difference in how well cancer patients do after treatment. This is shown by higher survival rates and long-lasting reactions in cancers like melanoma and non-small cell lung cancer. But there are still issues, such as ways to battle resistance, bad effects, and tall costs that can make it harder for a few individuals to induce what they require. Patient-reported results show how critical it is to oversee immune-related antagonistic events and improve quality of life in arrange to provide total care.
|
Table 2. Survival Rates of Immunotherapy Treatments |
|||
|
Treatment Type |
1-Year Survival Rate (%) |
2-Year Survival Rate (%) |
5-Year Survival Rate (%) |
|
Immune Checkpoint Inhibitors |
85 |
50 |
40 |
|
Immune Checkpoint Inhibitors |
70 |
40 |
25 |
|
CAR T-Cell Therapy |
90 |
80 |
60 |
|
CAR T-Cell Therapy |
80 |
60 |
50 |
|
Monoclonal Antibodies |
75 |
60 |
40 |
The mortality rates for different cancer medicines, especially immunotherapies, show how far cancer care has come and how hard it still is. Immune checkpoint drugs, like pembrolizumab and nivolumab, have shown promise in treating a number of cancers, with mortality rates of 70–85 % after one year. But these numbers drop a lot over time.
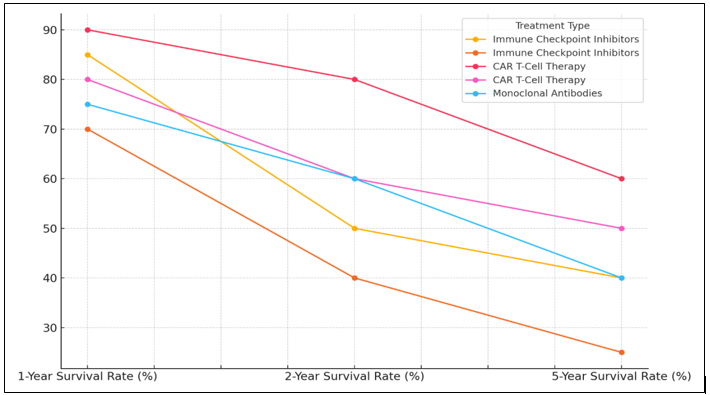
Figure 3. Survival Rate by Treatment Type Over Time
Figure 3 compares survival rates across different treatment types over time. It highlights variations in effectiveness, showcasing how advancements like targeted therapies and immunotherapies significantly improve long-term survival compared to conventional treatments. The 5-year mortality rate is between 25 and 40 percent. Long-term survival rates are going down, which brings up the problem of resistance. Cancers may be able to avoid immune monitoring after an initial reaction, so more study is needed to find signs that can help doctors choose better patients. Another cutting edge vaccine, CAR T-cell treatment, has shown great promise, especially in treating blood cancers like lymphoma and leukemia.
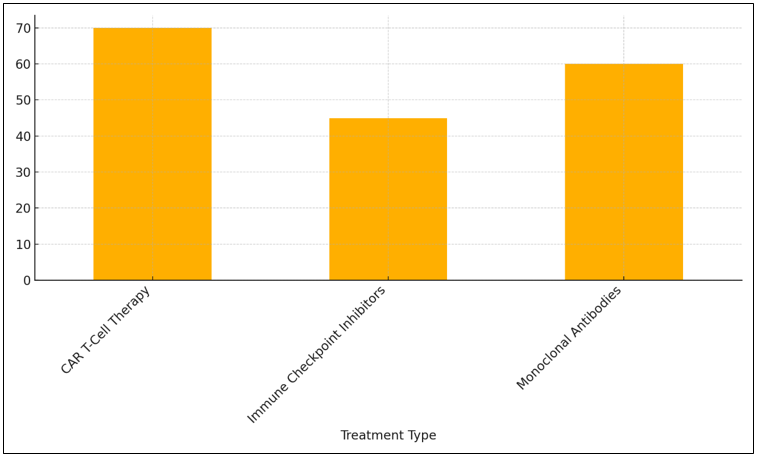
Figure 4. Overall Efficacy of Cancer Treatments
For one year, 80–90 % of people who receive CAR T-cell treatments will still be alive, and for two years, 60–80 % of people who receive immune checkpoint inhibitors will still be alive, as represent it in figure 4. But even CAR T-cell treatment has problems; only 50 to 60 % of people who get it survive 5 years. There are risks with these treatments, like cytokine release syndrome, which shows how important it is to carefully care for patients. Survival rates are about average with monoclonal antibodies, which are often used with other medicines. A 75 % survival rate after one year and a 40 % survival rate after five years show that monoclonal antibodies may not work as well or last as long as CAR T-cell treatment or immune checkpoint inhibitors.
|
Table 3. Adverse Events and Quality of Life Assessment |
||||
|
Cancer Type |
Treatment Type |
Incidence of IrAEs (%) |
Grade 3-4 Adverse Events (%) |
QoL Score Improvement (%) |
|
Melanoma |
Pembrolizumab |
20 |
8 |
15 |
|
NSCLC |
Pembrolizumab + Chemo |
25 |
10 |
18 |
|
ALL |
CAR T-cell Therapy |
30 |
15 |
30 |
|
Bladder Cancer |
Atezolizumab |
18 |
5 |
10 |
Different types of cancer and medicines have very different rates of immune-related adverse events (IrAEs) and differences in how bad they are.
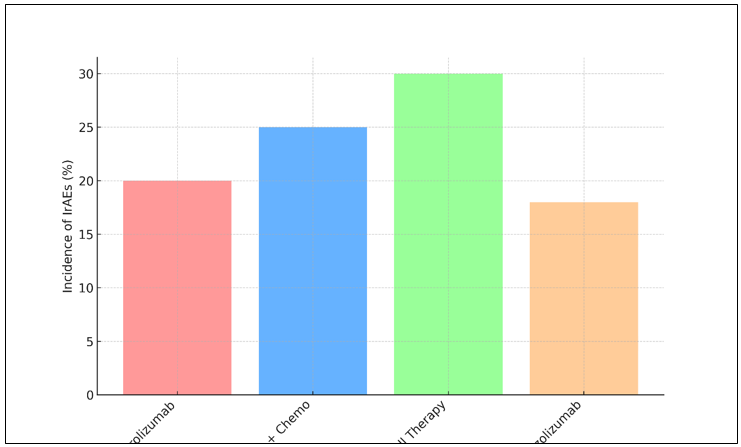
Figure 5. Incidence of Immune-Related Adverse Events (IrAEs)
They also have very different effects on quality of life (QoL) changes. 20 % of people with melanoma who are treated with pembrolizumab have IrAEs, and 8 % have Grade 3–4 adverse events. The figure 5 represent the Immune-Related Adverse Events.
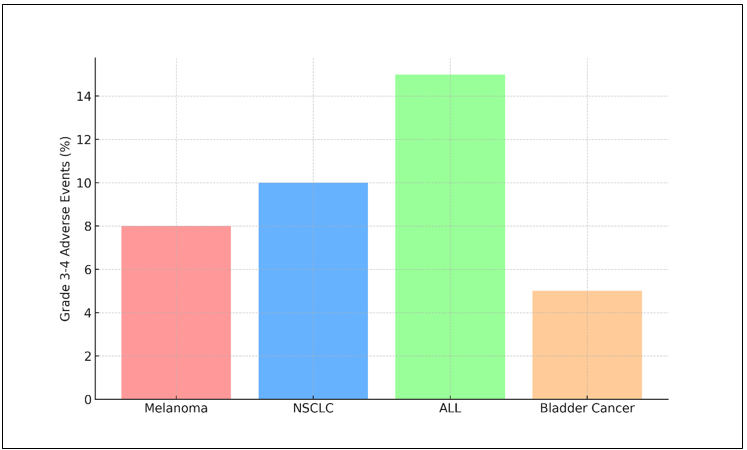
Figure 6. Grade 3-4 Severe Adverse Events by Cancer Type
Even with these problems, pembrolizumab raises QoL by 15 %, which suggests that for many patients, the benefits in terms of life and pain relief may be greater than the risks of side effects. Pembrolizumab and chemotherapy together cause a slightly higher rate of IrAEs (25 %) and more serious Grade 3–4 events (10 %) in people with non-small cell lung cancer (NSCLC), as comparison illustrate for Grade 3-4 Severe Adverse Events by Cancer Type in figure 6.
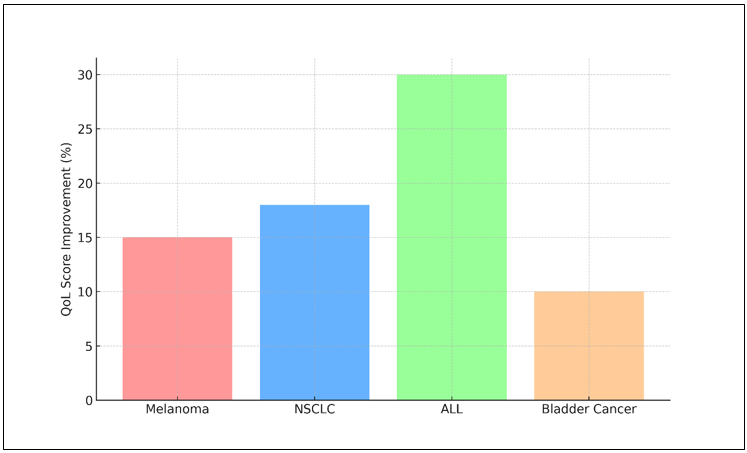
Figure 7. Quality of Life (QoL) Improvement by Cancer Type
But the increase in quality of life (18 %) is higher than what was seen in melanoma. This shows that combination treatment might help patients do better, even if the side effects are stronger. 30 % of people with acute lymphoblastic leukemia (ALL) who are getting CAR T-cell treatment will have an adverse event, and 15 % of those people will have a serious adverse event. However, the 30 % increase in QoL shows how much CAR T-cell treatment can improve life and general health, even though it comes with a higher chance of major side effects. The figure 7 shows how changes in Quality of Life (QoL) have been seen across different types of cancer. This shows how improved treatments have affected patients' health. The results show that QoL progress levels are not all the same. For some cancers, there were big gains in physical, mental, and social functioning. This shows how important it is to adapt treatment methods to deal with problems unique to cancer and improve total patient results.
CONCLUSIONS
Immunotherapy is a huge step forward in the way cancer is treated, giving many people new hope and better results. By using the immune system to find and kill cancer cells, immunotherapy has changed the way cancer is treated, especially for types of cancer that couldn't be cured before, like melanoma and non-small cell lung cancer. Immune checkpoint inhibitors, CAR T-cell treatment, and other new methods have been shown in clinical trials to improve life and cause reactions that last. This has changed what is expected in cancer. However, immunotherapy has had some rough spots along the way. Tumor ecosystem factors and tumor variability are two examples of mechanisms of resistance that can make treatment less effective, leading to different outcomes for each patient. It's also important to know that immune-related adverse events come with big risks and need good treatment plans to keep patients' quality of life as high as possible. To deal with these bad effects, we need a complete method that includes patient-reported results and makes sure that the social and mental parts of cancer care are understood and dealt with. There are also big problems with accessibility and cost that make it hard for immunotherapy to be widely used. The high prices of these new treatments can make care less fair, especially for groups that aren't getting enough of it. To make sure that all patients can benefit from these new treatments, it is important to find ways to improve insurance coverage, simplify governmental processes, and improve healthcare facilities. To get around the problems that come with immunotherapy, more study needs to be done. Looking into predicted factors can help make treatments more effective by adjusting them to each patient's needs.
BIBLIOGRAPHIC REFERENCES
1. Shiravand, Y.; Khodadadi, F.; Kashani, S.M.A.; Hosseini-Fard, S.R.; Hosseini, S.; Sadeghirad, H.; Ladwa, R.; O’Byrne, K.; Kulasinghe, A. Immune checkpoint inhibitors in cancer therapy. Curr. Oncol. 2022, 29, 3044–3060.
2. Zhang, Y.; Zhang, Z. The history and advances in cancer immunotherapy: Understanding the characteristics of tumor-infiltrating immune cells and their therapeutic implications. Cell. Mol. Immunol. 2020, 17, 807–821.
3. Hegde, P.S.; Chen, D.S. Top 10 Challenges in Cancer Immunotherapy. Immunity 2020, 52, 17–35.
4. Sanmamed, M.F.; Chen, L. A paradigm shift in cancer immunotherapy: From enhancement to normalization. Cell 2018, 175, 313–326.
5. Zhou, Y.; Tao, L.; Qiu, J.; Xu, J.; Yang, X.; Zhang, Y.; Tian, X.; Guan, X.; Cen, X.; Zhao, Y. Tumor biomarkers for diagnosis, prognosis, and targeted therapy. Signal Transduct. Target. Ther. 2024, 9, 132.
6. Grosser, R.; Cherkassky, L.; Chintala, N.; Adusumilli, P.S. Combination immunotherapy with CAR T Cells and checkpoint blockade for the treatment of solid tumors. Cancer Cell 2019, 36, 471–482.
7. Adir, O.; Poley, M.; Chen, G.; From, S.; Krinsky, N.; Shklover, J.; Roitman, J.S.; Lammers, T.; Schroeder, A. Integrating artificial intelligence and nanotechnology for precision cancer medicine. Adv. Mater. 2020, 32, e1901989.
8. Gonzalez, H.; Hagerling, C.; Werb, Z. Roles of the immune system in cancer: From tumor initiation to metastatic progression. Genes Dev. 2018, 32, 1267–1284.
9. Kim, S.K.; Cho, S.W. The evasion mechanisms of cancer immunity and drug intervention in the tumor microenvironment. Front. Pharmacol. 2022, 13, 868695.
10. Baxevanis, C.N. Immune checkpoint inhibitors in cancer therapy—How can we improve clinical benefits? Cancers 2023, 15, 881.
11. Ahmed, H.; Mahmud, A.R.; Siddiquee, M.F.; Shahriar, A.; Biswas, P.; Shimul, M.E.K.; Ahmed, S.Z.; Ema, T.I.; Rahman, N.; Khan, M.A.; et al. Role of T cells in cancer immunotherapy: Opportunities and challenges. Cancer Pathog. Ther. 2023, 1, 116–126.
12. Waldman, A.D.; Fritz, J.M.; Lenardo, M.J. A guide to cancer immunotherapy: From T cell basic science to clinical practice. Nat. Rev. Immunol. 2020, 20, 651–668.
13. Mavi, A.K.; Gaur, S.; Gaur, G.; Babita; Kumar, N.; Kumar, U. CAR T-cell therapy: Reprogramming patient’s immune cell to treat cancer. Cell. Signal. 2023, 105, 110638.
14. Wang, C.; Wang, J.; Che, S.; Zhao, H. CAR-T cell therapy for hematological malignancies: History, status and promise. Heliyon 2023, 9, e21776.
15. Liu, D.; Che, X.; Wang, X.; Ma, C.; Wu, G. Tumor Vaccines: Unleashing the Power of the Immune System to Fight Cancer. Pharmaceuticals 2023, 16, 1384.
16. Maleki, E.H.; Bahrami, A.R.; Matin, M.M. Cancer cell cycle heterogeneity as a critical determinant of therapeutic resistance. Genes Dis. 2023, 11, 189–204.
17. Krzyszczyk, P.; Acevedo, A.; Davidoff, E.J.; Timmins, L.M.; Berrios, I.M.; Patel, M.; White, C.; Lowe, C.; Sherba, J.J.; Hartmanshenn, C.; et al. The growing role of precision and personalized medicine for cancer treatment. Technology 2018, 6, 79–100.
18. Sharma, P.; Hu-Lieskovan, S.; Wargo, J.A.; Ribas, A. Primary, adaptive, and acquired resistance to cancer immunotherapy. Cell 2017, 168, 707–723.
19. Garg, P.; Malhotra, J.; Kulkarni, P.; Horne, D.; Salgia, R.; Singhal, S.S. Emerging Therapeutic Strategies to Overcome Drug Resistance in Cancer Cells. Cancers 2024, 16, 2478.
20. Enokida, T.; Moreira, A.; Bhardwaj, N. Vaccines for immunoprevention of cancer. J. Clin. Investig. 2021, 131, e146956.
21. Bilusic, M.; Madan, R.A. Therapeutic cancer vaccines: The latest advancement in targeted therapy. Am. J. Ther. 2012, 19, e172–e181.
22. Sordo-Bahamonde, C.; Lorenzo-Herrero, S.; Gonzalez-Rodriguez, A.P.; Martinez-Perez, A.; Rodrigo, J.P.; Garcia-Pedrero, J.M.; Gonzalez, S. Chemo-immunotherapy: A new trend in cancer treatment. Cancers 2023, 15, 2912.
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Pragati Aniket Manoli, Snigdha Pattnaik, Debanjana Prasad, Manashree Mane, Vinima Gambhir, C.Bharanidharan, Sumeet Kaur.
Data curation: Pragati Aniket Manoli, Snigdha Pattnaik, Debanjana Prasad, Manashree Mane, Vinima Gambhir, C.Bharanidharan, Sumeet Kaur.
Formal analysis: Pragati Aniket Manoli, Snigdha Pattnaik, Debanjana Prasad, Manashree Mane, Vinima Gambhir, C.Bharanidharan, Sumeet Kaur.
Drafting - original draft: Pragati Aniket Manoli, Snigdha Pattnaik, Debanjana Prasad, Manashree Mane, Vinima Gambhir, C.Bharanidharan, Sumeet Kaur.
Writing - proofreading and editing: Pragati Aniket Manoli, Snigdha Pattnaik, Debanjana Prasad, Manashree Mane, Vinima Gambhir, C.Bharanidharan, Sumeet Kaur.