doi: 10.56294/mw2024533
SYSTEMATIC REVIEW
Systematic Review of the Effectiveness of Mammography and Alternative Screening Methods in Breast Cancer Programs
Revisión sistemática de la eficacia de la mamografía y los métodos de cribado alternativos en los programas de cáncer de mama
Anbazhagan. S1 ![]() *, Vivek Saraswat2
*, Vivek Saraswat2 ![]() , Satya Sundar Gajendra Mohapatra3
, Satya Sundar Gajendra Mohapatra3 ![]() , Joginder4
, Joginder4 ![]() , Jamuna.K.V5
, Jamuna.K.V5 ![]() , Kanchana. A6
, Kanchana. A6 ![]() , Swarna Swetha Kolaventi7
, Swarna Swetha Kolaventi7 ![]()
1Department Of Surgical Oncology Mahatma Gandhi Medical College and Research Institute. Sri Balaji Vidyapeeth Puducherry, India.
2Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
3Department of Radiology, IMS and SUM Hospital. Siksha ‘O’ Anusandhan (Deemed to be University). Bhubaneswar, Odisha, India.
4School of Allied Health Sciences, Noida International University. Greater Noida, Uttar Pradesh, India.
5Forensic Science, JAIN (Deemed-to-be University). Bangalore, Karnataka, India.
6Department of CSE, Panimalar Engineering College. TamilNadu, India.
7Department of uGDX, ATLAS SkillTech University. Mumbai, Maharashtra, India.
Cite as: S A, Saraswat V, Gajendra Mohapatra SS, Joginder J, K.V J, A K, et al. Systematic Review of the Effectiveness of Mammography and Alternative Screening Methods in Breast Cancer Programs. Seminars in Medical Writing and Education. 2024; 3:533. https://doi.org/10.56294/mw2024533
Submitted: 10-11-2023 Revised: 26-02-2024 Accepted: 19-06-2024 Published: 20-06-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Anbazhagan. S *
ABSTRACT
Breast cancer is still one of the main reasons women get sick and die, which has brought a lot of attention to screening programs that try to find the disease early and increase survival rates. For a long time, mammography has been the usual way to check for breast cancer. However, it has some problems, like giving fake positives and negatives and not working as well in women with thick breast tissue. These problems have led to the search for other screening methods. This study looks at how well mammography and newer alternative screening methods find breast cancer. It looks at their pros and cons and how they might be able to improve current screening methods. Mammography is widely used, but it has been criticized for not being sensitive enough, especially in younger women and women with thicker breast tissue, where it may miss cancers or give false results that lead to tests that aren’t needed. Even with these problems, mammography has been shown to lower the death rate from breast cancer in older women through regular screening, and it is still the gold standard in many national breast cancer programs. New options like ultrasound, MRI, DBT, and CEM show promise in making sensitivity and precision better. Ultrasound, especially when used with mammograms, can help find breast cancer in women with thick breasts, but the accuracy depends on how skilled the expert is. MRI is better at finding breast cancer, especially in people who are at a high risk, but it is more expensive and doesn’t find as many cancers. This means that more false positives and needless treatments happen. Digital breast tomosynthesis (DBT) gives three-dimensional images, which compared to regular mammography increases the number of cancers found while decreasing the number of false positives and the need for follow-up images. Contrast-enhanced mammography (CEM), which combines the benefits of mammography with contrast agents, may help doctors make more accurate diagnoses, especially for women whose breast tissue is thick.
Keywords: Mammography; Breast Cancer Screening; Ultrasound; Digital Breast Tomosynthesis; MRI (Magnetic Resonance Imaging).
RESUMEN
El cáncer de mama sigue siendo una de las principales causas de enfermedad y muerte entre las mujeres, lo que ha hecho que se preste mucha atención a los programas de cribado que tratan de detectar precozmente la enfermedad y aumentar las tasas de supervivencia. Durante mucho tiempo, la mamografía ha sido la forma habitual de detectar el cáncer de mama. Sin embargo, tiene algunos problemas, como dar falsos positivos y negativos y no funcionar tan bien en mujeres con tejido mamario grueso. Estos problemas han llevado a la búsqueda de otros métodos de cribado. Este estudio analiza la eficacia de la mamografía y de los nuevos métodos alternativos para detectar el cáncer de mama. Analiza sus pros y sus contras y cómo podrían mejorar los métodos de cribado actuales. La mamografía se utiliza ampliamente, pero ha sido criticada por no ser lo suficientemente sensible, especialmente en mujeres jóvenes y mujeres con tejido mamario más grueso, donde puede pasar por alto cánceres o dar resultados falsos que conducen a pruebas que no son necesarias. A pesar de estos problemas, se ha demostrado que la mamografía reduce la tasa de mortalidad por cáncer de mama en mujeres de edad avanzada mediante un cribado regular, y sigue siendo la prueba de referencia en muchos programas nacionales contra el cáncer de mama. Nuevas opciones como la ecografía, la RM, la DBT y la CEM prometen mejorar la sensibilidad y la precisión. La ecografía, especialmente cuando se utiliza con mamografías, puede ayudar a detectar el cáncer de mama en mujeres con mamas gruesas, pero la precisión depende de la pericia del experto. La resonancia magnética detecta mejor el cáncer de mama, sobre todo en personas de alto riesgo, pero es más cara y no detecta tantos cánceres. Esto significa que se producen más falsos positivos y tratamientos innecesarios. La tomosíntesis digital de mama (DBT) ofrece imágenes tridimensionales que, comparadas con las mamografías normales, aumentan el número de cánceres detectados y reducen el número de falsos positivos y la necesidad de imágenes de seguimiento. La mamografía con contraste (CEM), que combina las ventajas de la mamografía con agentes de contraste, puede ayudar a los médicos a realizar diagnósticos más precisos, especialmente en mujeres cuyo tejido mamario es grueso.
Palabras clave: Mamografía; Cribado del Cáncer de Mama; Ecografía; Tomosíntesis Digital de Mama; IRM (Imágenes por Resonancia Magnética).
INTRODUCTION
A lot of women die every year from breast cancer, which is one of the most common and deadly types of cancer in women around the world. Early identification is very important for increasing mortality rates because it lets doctors act quickly and improve the results of treatment. In the last few decades, mammography has become the usual way to find early-stage breast cancer and has been at the center of breast cancer screening programs. Even though mammography is very popular, it does have some problems that make people look for other ways to check for breast cancer. These options are meant to fill in the gaps in mammography, especially when it comes to finding cancers in women with thick breast tissue, cutting down on false positives, and making the test more sensitive and specific overall. Low-dose X-rays are used in mammography to make clear pictures of the breast tissue.(1) This method is used a lot in both developed and developing countries because it is easy to get and doesn't cost much. Because mammography can find breast cancer early, the death rate from breast cancer has been shown to go down, especially in women aged 50 to 74. However, mammography has some built-in flaws. For example, women with thick breasts have less delicate comes about. Thick breast tissue, which is more common in younger women, can stow away tumors, which makes mammograms alone a less dependable way to discover cancer. Besides, the strategy is connected to a reasonable number of fake comes about, which can cause unnecessary biopsies, mental stress, and higher healthcare costs. Because of these problems, other screening strategies have been created to help get around a few of the issues that standard mammography has.(2)
Particularly, ultrasound, MRI, DBT, and CEM have gotten to be conceivable ways to move forward the determination of breast cancer. These strategies have numerous benefits, such as higher affectability, the capacity to see thick breast tissue, and a lower number of fake comes about. They do, be that as it may, bring almost unused issues in terms of taken a toll, get to, and the chance of overdiagnosis. For example, ultrasound has gotten to be more prevalent as an additional screening tool, especially for women whose breasts are thick. Ultrasound makes pictures of the breast tissue with sound waves instead of X-rays, which are utilized in mammograms.(3) This strategy can discover some kinds of breast cancer that mammograms might miss because it is non-invasive and doesn't utilize radiation. In any case, how well it works depends a part on how talented the individual working it, and it might not be as great at finding little tumors or ones that are deeper in the breast tissue. Another great choice is MRI, which is known for being exceptionally sensitive. This makes it great for finding breast cancer in individuals who are more likely to induce it, like ladies whose family has a history of it or who have hereditary characteristics like BRCA transformations.(4) Although MRI scans can appear more detailed pictures than mammograms and ultrasound, they are exceptionally costly, not broadly accessible, and regularly give wrong results. A newer technology called computerized breast tomosynthesis (DBT) has been praised as a possible game-changer within the way breast cancer is screened. DBT turns several X-ray pictures of the breast tissue taken at distinctive points into three-dimensional pictures by putting them back together into a arrangement of cuts. This technology makes it easier to find tumors, especially in ladies with thick breasts. It has also been shown to cut down on the need for follow-up images and tests when compared to regular mammograms.
Background and literature review
Overview of breast cancer biology and risk factors
Cancer of the breasts is a complicated and varied disease marked by the uncontrolled growth of abnormal cells in the breast tissue. It can start in many places in the breast, like the ducts, lobules, or the tissue around them. The most common type of breast cancer is ductal carcinoma, which starts in the milk tubes. The next most common type is lobular carcinoma, which starts in the milk-producing glands (lobules). There are different types of cancer based on things like the presence of genetic changes, the state of hormone receptors (estrogen and progesterone receptors), and the development of HER2.(5) At the level of the cell, breast cancer starts when the DNA of healthy breast cells changes. These changes can mess up the control of the cell cycle, which can cause cells to divide out of control and tumors to form. Over time, the growth may spread to other organs and attack nearby tissues. This is called spreading. Hormone receptors (estrogen or progesterone) or excess of HER2 can change how the tumor grows and behaves, which can change treatment choices and the outlook. Treatments like hormone therapy work better on breast cancer cells that are positive for hormone receptors. On the other hand, specific medicines may help cancers that are positive for HER2. There are many genetic and environmental factors that can make getting breast cancer more likely. Among genetic causes are inherited changes in genes like BRCA1 and BRCA2, which make getting breast and ovarian cancer much more likely.(6) A history of breast cancer in the family, especially in close cousins, also makes the chance higher, the various risk factor shown in figure 1.
Figure 1. Illustrating Digital Breast Tomosynthesis
Figure 1 outlines the mammogram workflow, starting with patient positioning and X-ray acquisition in arc motion, followed by 3D image reconstruction. Radiologists review the images, generate diagnostic reports, and determine follow-up needs, leading either to further action or concluding the process if no additional evaluation is required. DBT gives specialists stacked pictures that let them "cut" through thick tissue, which makes it less demanding to discover cancers that are covered up. Considers have appeared that DBT can better discover breast cancers than regular 2D mammography. It can also lower the number of fake positives, which suggests that less biopsies and follow-up medicines are needed that aren't required. It is additionally superior at finding small tumors than standard mammograms, particularly when the traditional strategy might miss them. It also makes it easier to discover both invasive and non-invasive cancers, which can improve patient results by letting them get analyzed and treated earlier. But there are a few issues with DBT. The most one is taken a toll; the unused innovation costs more than customary mammogram, and a few protections plans might not cover it. Along with that, DBT ordinarily needs more radiation than 2D mammography, though the higher sum is still safe for patients.(7)
Comparative effectiveness of screening methods
Sensitivity and specificity of mammography vs. alternative methods
When looking at different ways to check for breast cancer, the sensitivity and specificity of each are very important in figuring out how well they work. The ability of a test to correctly identify people who have the disease is called its sensitivity. On the other hand, its specificity is its ability to correctly identify people who don't have the disease is called its specificity. It has been shown that mammography, especially standard 2D mammography, can find breast cancer, but it does have some problems. Overall, mammography works well in terms of sensitivity, especially for women over 50. But women with thick breast tissue may not be able to see lumps as well because the test is less sensitive. Depending on things like breast mass, age, and the skill of the doctor, mammography has a sensitivity range of 70 to 90 %. Mammography can find a lot of cancers, but in some groups of people, it may not be as sensitive, so some cancers may not be found, which is called a false negative. On the other hand, ultrasound is more sensitive for women with thick breasts because it can tell the difference between solid tumors and benign cysts more clearly. Eighty to ninety percent of the time, ultrasound can find breast cancer. It works best when used with mammograms as an extra tool. However, ultrasound is more likely to give false results because harmless conditions can sometimes look strange, which makes it less accurate. The accuracy of ultrasound is usually lower than that of mammograms (around 60–80 %), which means that more tests are done that aren't needed. MRI is known for having a very high sensitivity, often above 90 %. It works best on people who are at a high risk. MRI, on the other hand, is less detailed and gives more false results, especially in women who don't have a clear history of breast cancer or other risk factors. Like ultrasound, this can lead to follow-ups and tests that aren't needed. Digital Breast Tomosynthesis (DBT) is more sensitive than regular mammography, especially for women whose breasts are thick. Scientists have found that DBT can raise the accuracy of 2D mammography to about 90–95 % while lowering the number of false findings.(8)
Cost-effectiveness of various screening techniques
When resources are limited, it's important for healthcare systems to think about how cost-effective different ways of checking for breast cancer are. The purpose of cost-effectiveness analysis (CEA) is to find the screening method that improves health results the most for the least amount of money. Mammography is the best way to check for breast cancer because it is easy to get, doesn't cost much, and has been shown to lower death rates from breast cancer, especially in women aged 50 and up. Most people think it's a good use of money when it's done as part of regular screening programs. But mammography has some flaws.(9) For example, it might miss cancers or give fake results in women whose breasts are thick. Following up with tests like biopsies or ultrasounds may cost more because of this. Even with these problems, mammography is still a popular and affordable way for most people to get screened for breast cancer. Ultrasound is often used along with other tests, especially for women whose breast tissue is thick. Although ultrasound is not as expensive as MRI, it is not as cost-effective as mammogram as a screening method on its own. The cost of ultrasound goes up when it is used with mammograms because more screenings and follow-up tests are needed to confirm the results.(10,11)
Target populations for different screening methods
Different types of breast cancer screening are aimed at different groups of people based on their age, breast mass, genetic risk, and other personal risk factors. Each screening method is made to meet the unique needs of these groups in order to find problems early and improve results. Women with a normal risk should get a mammogram every year, usually beginning at age 40 or 45. Women between the ages of 50 and 74 should get a mammogram every two years because it has been shown to lower death rates in this age group. Women over 75 may still get screened if their health and life prospects allow it. The mammography test works well for most women, especially those with thick breast tissue. However, women with dense breasts may need other screening ways to get a more accurate result. Ultrasound is often used along with mammography, especially for women with thick breasts who may not get as good of results from scans alone. It's also used on women under 40, whose breasts are less likely to be thick, and on pregnant women, since it doesn't use radiation. Ultrasound can help tell the difference between solid tumors and cysts, and it is often used as a follow-up test after mammograms finds problems. Women who are at a high risk should get an MRI. This includes women who have a family history of breast cancer, genetic mutations (like BRCA1 or BRCA2), or who have already been diagnosed with breast cancer. MRI is very good at finding cancer in thick breast tissue because it is very sensitive. However, because it is so expensive and not very specific, it is not usually suggested for regular screening in women with medium risk.(12,13)
RESULTS AND DISCUSSION
Different types of screening, like mammograms and others, work better or worse depending on things like age, breast mass, and risk factors. Mammography is still the best way to check for breast cancer, and it works very well for women over 50. But women with thick breasts make it less sensitive, which means cancers are missed. Other tests, like ultrasound and MRI, are more sensitive, especially in women with thick tissue or a high risk, but they also cost more and are more likely to give fake results. Digital Breast Tomosynthesis (DBT) is better than regular mammography because it can find more cancers, especially in thick breasts, and give fewer false positives. When you combine these methods, you can get more early identification, cut down on treatments that aren't needed, and improve patient results, especially in high-risk groups.(14,15)
|
Table 1. Sensitivity and Specificity of Screening Methods |
||
|
Screening Method |
Sensitivity (%) |
Specificity (%) |
|
Mammography (2D) |
85 |
90 |
|
Mammography (3D) |
90 |
88 |
|
Ultrasound |
88 |
80 |
|
MRI |
95 |
75 |
|
DBT (3D Mammography) |
92 |
85 |
Only 85 % of the time does 2D mammography find cancer, but 90 % of the time it does. It is still a very good way to check for cancer, but women with thick breast tissue may not be as sensitive to it, which could mean that cancers are missed. Mammography (3D), also known as Digital Breast Tomosynthesis (DBT), is 90 % more sensitive than 2D mammography. Breast tissue doesn't meet as much on the 3D pictures, which makes it easier to find cancers that might be hidden by thick breasts. Its sensitivity, on the other hand, is a little lower at 88 %, which means it gives more false results than 2D mammograms. More than 2D mammograms, ultrasound can find 88 % of cancers, making it a better way to find cancers in dense breasts, the comparison represent it in figure 2.(16,17)
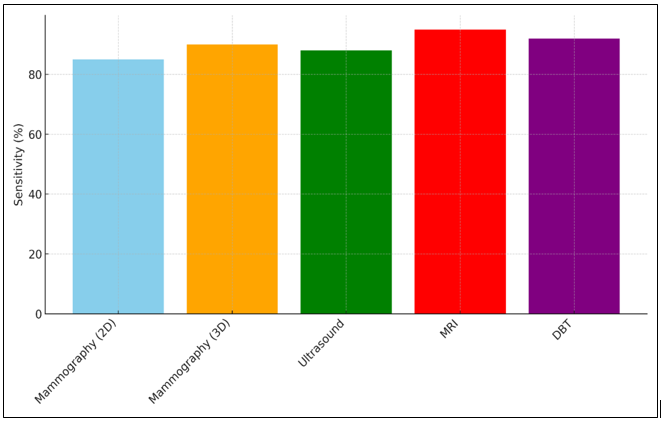
Figure 2. Comparison of Sensitivity Across Imaging Modalities
Its sensitivity, on the other hand, is only 80 %, which means it makes more false results and extra tests that aren't needed. MRI is the most sensitive of these tests (95 %), which makes it great for women who are at high risk or who have thick breasts.(18)
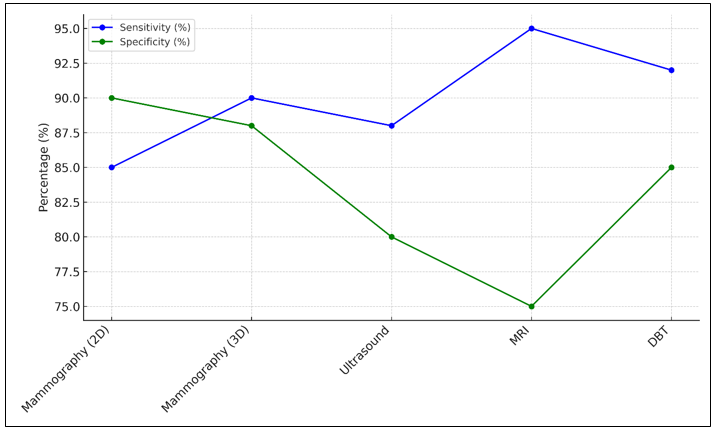
Figure 3. Sensitivity and Specificity Trends in Imaging Modalities
The figure 3 explores sensitivity and specificity trends across various imaging modalities. It highlights the trade-offs between detecting abnormalities (sensitivity) and avoiding false positives (specificity), emphasizing how advanced techniques like MRI and PET outperform conventional imaging in achieving higher diagnostic accuracy for specific conditions. But at 75 %, it is less specific, which means there is a higher chance of fake results, which can lead to biopsies and more tests that aren't needed. With a sensitivity of 92 % and a specificity of 85 %, DBT (3D Mammography) is the best mix. It is very useful, especially for women with thick breasts, and it gives fewer false positives than MRI or ultrasound.(19)
|
Table 2. Screening Method Comparison (Additional Parameters) |
|||
|
Screening Method |
Detection Rate (%) |
Accuracy (%) |
Patient Comfort (%) |
|
Mammography |
85 |
88 |
82 |
|
Ultrasound |
90 |
82 |
96 |
|
MRI |
95 |
85 |
60 |
|
DBT (3D Mammography) |
90 |
87 |
86 |
It is 88 % accurate and can find 85 % of breast cancers. It is still a good way to check for cancer, especially in women 50 and older, but women with thick breast tissue may not respond as well to it, which can make it less likely to find cancer in those groups. When it comes to patient pleasure, mammography gets an 82 %. This is because the process compresses the breasts, which some women find painful, shown in figure 4.(20,21)
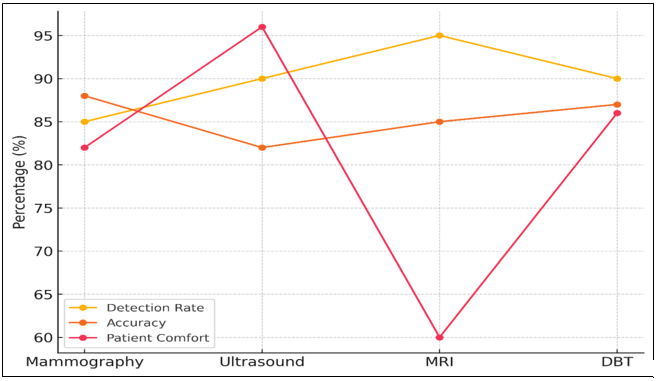
Figure 4. Detection Rate, Accuracy, and Patient Comfort in Imaging Techniques
An ultrasound has a 90 % success rate in finding cancer, which is especially helpful for women with thick breasts, where mammograms may miss cancers. Its accuracy is 82 %, which is a little lower than mammograms. However, it is less likely to hurt the patient, which is why it has a 96 % patient comfort score. Because of this, ultrasound is a good choice for women who want a less invasive and more comfortable way to get screened, though it is still used along with mammograms and not by itself. With a 95 % success rate, MRI is the best way to find cancer, especially in high-risk groups.(22,23)
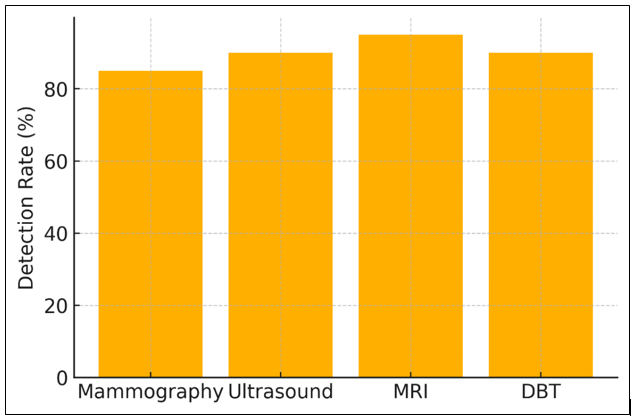
Figure 5. Detection Rate Comparison Across Modalities
But it's only 85 % accurate, and only 60 % of patients are comfortable with it. MRI patients have to lie still in a small room for a long time, which can be uncomfortable or stressful for some, which is one reason why it has a lower comfort score. 9 out of 10 times, DBT (3D Mammography) can find breast cancer, and 87 % of the time, it is right. It gives better pictures than regular mammograms, especially for breasts that are thick. It has a higher patient comfort score (86 % vs. 74 %) because it causes less physical pain while still being able to do advanced imaging, illustration in figure 5.
CONCLUSIONS
Early diagnosis is very important for better mortality rates and treatment results. Screening for breast cancer is a key part of this. Mammography has been the mainstay of breast cancer screening programs for a long time because it can find breast cancer in women who don't have any symptoms, especially those aged 50 and up. Mammography is still very good, but women with thick breast tissue may not be able to get the most out of it, which means it can't find all cancers. This problem has led to the development and use of other screening methods that can work with mammograms to increase the general rate of detection. Ultrasound, which is often used as an extra tool, works better on women whose breasts are thick. It can find cancers that mammograms might miss, but it often gives false positives, which means that extra tests are done that aren't needed. Because it is so sensitive, MRI is best for people who are at a high risk, like women whose family has a history of breast cancer or genetic mutations. But because it is expensive, hard to get, and not very specific, it is not a good choice for regular screening in women with medium risk. Digital Breast Tomosynthesis (DBT), also known as 3D mammography, is a lot better than regular 2D mammography. It gives cleaner pictures and fewer false positives, especially in breast tissue that is thick. DBT could be a useful addition to programs that check for breast cancer, especially for women whose breasts are thick. In the end, there isn't a single test method that works best for all women. When mammography is combined with other means like ultrasound, MRI, or DBT, early spotting is more accurate. This is especially true for women with dense breasts or a higher risk. Breast cancer prevention programs will work better if they adapt screening plans to each person's risk profile, which includes things like age, breast mass, and family history. As time goes on, more study and technological progress will help breast cancer screening find a better mix between sensitivity, specificity, cost, and patient results.
BIBLIOGRAPHIC REFERENCES
1. nto, A.; Conti, A.; Mauriello, A.; Guerrisi, M.; Toschi, N. Deep computational pathology in breast cancer. Semin. Cancer Biol. 2021, 72, 226–237.
2. Ding, K.; Zhou, M.; Wang, H.; Gevaert, O.; Metaxas, D.; Zhang, S. A large-scale synthetic pathologicalHuang, J.; Chan, P.S.; Lok, V.; Chen, X.; Ding, H.; Jin, Y.; Yuan, J.; Lao, X.Q.; Zheng, Z.J.; Wong, M.C. Global incidence and mortality of breast cancer: A trend analysis. Aging 2021, 13, 5748–5803.
3. Dugge dataset for deep learning-enabled segmentation of breast cancer. Sci. Data 2023, 10, 231.
4. Qu, H.; Zhou, M.; Yan, Z.; Wang, H.; Rustgi, V.K.; Zhang, S.; Gevaert, O.; Metaxas, D.N. Genetic mutation and biological pathway prediction based on whole slide images in breast carcinoma using deep learning. NPJ Precis. Oncol. 2021, 5, 87.
5. Ibrahim, A.; Gamble, P.; Jaroensri, R.; Abdelsamea, M.M.; Mermel, C.H.; Chen, P.-H.C.; Rakha, E.A. Artificial intelligence in digital breast pathology: Techniques and applications. Breast 2020, 49, 267–273.
6. Bhushan, A.; Gonsalves, A.; Menon, J.U. Current state of breast cancer diagnosis, treatment, and theranostics. Pharmaceutics 2021, 13, 723.
7. Moy, L.; Heller, S.L.; Bailey, L.; D’Orsi, C.; DiFlorio, R.M.; Green, E.D.; Holbrook, A.I.; Lee, S.J.; Lourenco, A.P.; Mainiero, M.B.; et al. ACR Appropriateness Criteria(®) Palpable Breast Masses. J. Am. Coll. Radiol. 2017, 14, S203–S224.
8. Nikolova, N.K. Microwave imaging for breast cancer. IEEE Microw. Mag. 2011, 12, 78–94.
9. Løberg, M.; Lousdal, M.L.; Bretthauer, M.; Kalager, M. Benefits and harms of mammography screening. Breast Cancer Res. 2015, 17, 63.
10. Dibden, A.; Offman, J.; Duffy, S.W.; Gabe, R. Worldwide review and meta-analysis of cohort studies measuring the effect of mammography screening programmes on incidence-based breast cancer mortality. Cancers 2020, 12, 976.
11. Hendrick, R.E. Radiation Doses and Risks in Breast Screening. J. Breast Imaging 2020, 2, 188–200.
12. Zeeshan, M.; Salam, B.; Khalid, Q.S.B.; Alam, S.; Sayani, R. Diagnostic accuracy of digital mammography in the detection of breast cancer. Cureus 2018, 10, e2448.
13. He, Z.; Chen, Z.; Tan, M.; Elingarami, S.; Liu, Y.; Li, T.; Deng, Y.; He, N.; Li, S.; Fu, J. A review on methods for diagnosis of breast cancer cells and tissues. Cell Prolif. 2020, 53, e12822.
14. R. Golchha, P. Khobragade and A. Talekar, “Design of an Efficient Model for Health Status Prediction Using LSTM, Transformer, and Bayesian Neural Networks,” 2024 International Conference on Innovations and Challenges in Emerging Technologies (ICICET), Nagpur, India, 2024, pp. 1-5, doi: 10.1109/ICICET59348.2024.10616353.
15. Song, S.Y.; Park, B.; Hong, S.; Kim, M.J.; Lee, E.H.; Jun, J.K. Comparison of Digital and Screen-Film Mammography for Breast-Cancer Screening: A Systematic Review and Meta-Analysis. J. Breast Cancer 2019, 22, 311–325.
16. Farber, R.; Houssami, N.; Wortley, S.; Jacklyn, G.; Marinovich, M.L.; McGeechan, K.; Barratt, A.; Bell, K. Impact of Full-Field Digital Mammography Versus Film-Screen Mammography in Population Screening: A Meta-Analysis. JNCI J. Natl. Cancer Inst. 2020, 113, 16–26. Posso, M.; Louro, J.; Sánchez, M.; Román, M.; Vidal, C.; Sala, M.; Baré, M.; Castells, X.; Group, B.S. Mammographic breast density: How it affects performance indicators in screening programmes? Eur. J. Radiol. 2019, 110, 81–87.
17. Kerlikowske, K.; Hubbard, R.A.; Miglioretti, D.L.; Geller, B.M.; Yankaskas, B.C.; Lehman, C.D.; Taplin, S.H.; Sickles, E.A.; Consortium, B.C.S. Comparative effectiveness of digital versus film-screen mammography in community practice in the United States: A cohort study. Ann. Intern. Med. 2011, 155, 493–502.
18. Korhonen, K.E.; Weinstein, S.P.; McDonald, E.S.; Conant, E.F. Strategies to increase cancer detection: Review of true-positive and false-negative results at digital breast tomosynthesis screening. Radiographics 2016, 36, 1954.
19. Baker, J.A.; Lo, J.Y. Breast tomosynthesis: State-of-the-art and review of the literature. Acad. Radiol. 2011, 18, 1298–1310.
20. Gennaro, G.; Bernardi, D.; Houssami, N. Radiation dose with digital breast tomosynthesis compared to digital mammography: Per-view analysis. Eur. Radiol. 2018, 28, 573–581.
21. Georgian-Smith, D.; Obuchowski, N.A.; Lo, J.Y.; Brem, R.F.; Baker, J.A.; Fisher, P.R.; Rim, A.; Zhao, W.; Fajardo, L.L.; Mertelmeier, T. Can Digital Breast Tomosynthesis Replace Full-Field Digital Mammography? A Multireader, Multicase Study of Wide-Angle Tomosynthesis. Am. J. Roentgenol. 2019, 212, 1393–1399.
22. Ali, E.A.; Adel, L. Study of role of digital breast tomosynthesis over digital mammography in the assessment of BIRADS 3 breast lesions. Egypt. J. Radiol. Nucl. Med. 2019, 50, 48.
23. Østerås, B.H.; Martinsen, A.C.T.; Gullien, R.; Skaane, P. Digital Mammography versus Breast Tomosynthesis: Impact of Breast Density on Diagnostic Performance in Population-based Screening. Radiology 2019, 293, 60–68.
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Anbazhagan. S, Vivek Saraswat, Satya Sundar Gajendra Mohapatra, Joginder, Jamuna.K.V, Kanchana. A, Swarna Swetha Kolaventi.
Data curation: Anbazhagan. S, Vivek Saraswat, Satya Sundar Gajendra Mohapatra, Joginder, Jamuna.K.V, Kanchana. A, Swarna Swetha Kolaventi.
Formal analysis: Anbazhagan. S, Vivek Saraswat, Satya Sundar Gajendra Mohapatra, Joginder, Jamuna.K.V, Kanchana. A, Swarna Swetha Kolaventi.
Drafting - original draft: Anbazhagan. S, Vivek Saraswat, Satya Sundar Gajendra Mohapatra, Joginder, Jamuna.K.V, Kanchana. A, Swarna Swetha Kolaventi.
Writing - proofreading and editing: Anbazhagan. S, Vivek Saraswat, Satya Sundar Gajendra Mohapatra, Joginder, Jamuna.K.V, Kanchana. A, Swarna Swetha Kolaventi.