doi: 10.56294/mw2024537
ORIGINAL
Comparing Clinical Outcomes and Treatment Efficiency of 3D Conformal and Intensity Modulated Radiotherapy
Comparación de los resultados clínicos y la eficacia del tratamiento de la radioterapia conformada 3D y la radioterapia de intensidad modulada
Neha Rana1 ![]() *, Manashree
Mane2
*, Manashree
Mane2 ![]() , Bodireddy Vamalatha3
, Bodireddy Vamalatha3 ![]() , B Reddy4
, B Reddy4 ![]() , Naresh Kaushik5
, Naresh Kaushik5 ![]() , Anoop Dev6
, Anoop Dev6 ![]() , Adya Kinkar Panda7
, Adya Kinkar Panda7 ![]()
1School of Pharmacy, Noida International University. Greater Noida, Uttar Pradesh, India.
2Forensic Science, JAIN (Deemed-to-be University). Bangalore, Karnataka, India.
3Centre for Multidisciplinary Research, Anurag University. Hyderabad, Telangana, India.
4Chitkara Centre for Research and Development, Chitkara University. Himachal Pradesh, India.
5Department of uGDX, ATLAS SkillTech University. Mumbai, Maharashtra, India.
6Centre of Research Impact and Outcome, Chitkara University. Rajpura, Punjab, India.
7Department of Radiology, IMS and SUM Hospital, Siksha ‘O’ Anusandhan (Deemed to be University). Bhubaneswar, Odisha, India.
Cite as: Rana N, Mane M, Vamalatha B, Reddy B, Kaushik N, Dev A, et al. Comparing Clinical Outcomes and Treatment Efficiency of 3D Conformal and Intensity Modulated Radiotherapy. Seminars in Medical Writing and Education. 2024; 3:537. https://doi.org/10.56294/mw2024537
Submitted: 12-11-2023 Revised: 28-02-2024 Accepted: 20-06-2024 Published: 21-06-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: Neha Rana *
ABSTRACT
Recently, a lot of progress has been made in using radiation therapy to treat cancer. The two most common methods are 3D Conformal Radiotherapy (3D-CRT) and Intensity Modulated Radiotherapy (IMRT). Both ways try to give tumors the exact amount of radiation they need while causing as little damage as possible to good cells around them. In this study, the clinical results and treatment effectiveness of 3D-CRT and IMRT are compared in cancer patients with different types of radiation therapy. A historical cohort study included 120 patients from different hospitals. They were split into two groups, with one group getting 3D-CRT and the other IMRT. The main goals of the study were to compare the two groups in terms of tumor control rates, side effects from treatment, and overall survival (OS). The effectiveness of the treatment was also judged by looking at the total time needed for planning and carrying out the treatment, as well as the radiation doses given to both the tumor and healthy cells. Overall, our results showed that IMRT had better tumor control rates than 3D-CRT, with more cases of local control and fewer cases of cancer coming back at treatment sites. When compared to 3D-CRT, the IMRT group had a significantly lower rate of acute radiation-induced effects, such as skin discomfort and stomach problems. Because it can send out very directed radiation beams, IMRT was also linked to less damage to good organs around the tumor, like the spinal cord and lungs. IMRT, on the other hand, needs more complicated treatment planning and takes longer to give than 3D-CRT, which can make prices and resource use go up. Even so, IMRT’s higher level of accuracy made it a clear winner when it came to controlling tumors and improving patients’ quality of life.
Keywords: 3D Conformal Radiotherapy; Intensity Modulated Radiotherapy; Clinical Outcomes; Treatment Efficiency.
RESUMEN
Recientemente se ha avanzado mucho en el uso de la radioterapia para tratar el cáncer. Los dos métodos más comunes son la radioterapia conformada 3D (3D-CRT) y la radioterapia de intensidad modulada (IMRT). Ambas formas tratan de administrar a los tumores la cantidad exacta de radiación que necesitan, causando al mismo tiempo el menor daño posible a las células buenas que los rodean. En este estudio se comparan los resultados clínicos y la eficacia terapéutica de la 3D-CRT y la IMRT en pacientes con cáncer sometidos a distintos tipos de radioterapia. En un estudio de cohortes histórico participaron 120 pacientes de distintos hospitales. Se dividieron en dos grupos: un grupo recibió 3D-CRT y el otro IMRT. Los principales objetivos del estudio eran comparar los dos grupos en cuanto a tasas de control tumoral, efectos secundarios del tratamiento y supervivencia global (SG). La eficacia del tratamiento también se evaluó teniendo en cuenta el tiempo total necesario para planificar y llevar a cabo el tratamiento, así como las dosis de radiación administradas tanto al tumor como a las células sanas. En general, nuestros resultados mostraron que la IMRT tenía mejores tasas de control tumoral que la 3D-CRT, con más casos de control local y menos casos de reaparición del cáncer en los lugares de tratamiento. En comparación con la 3D-CRT, el grupo de IMRT presentó una tasa significativamente menor de efectos agudos inducidos por la radiación, como molestias cutáneas y problemas estomacales. Dado que puede enviar haces de radiación muy dirigidos, la IMRT también se relacionó con un menor daño a los órganos buenos situados alrededor del tumor, como la médula espinal y los pulmones. Por otro lado, la IMRT necesita una planificación del tratamiento más complicada y tarda más en administrarse que la 3D-CRT, lo que puede hacer subir los precios y el uso de recursos. Aun así, el mayor nivel de precisión de la IMRT la convirtió en clara vencedora a la hora de controlar los tumores y mejorar la calidad de vida de los pacientes.
Palabras clave: Radioterapia Conformada 3D; Radioterapia de Intensidad Modulada; Resultados Clínicos; Eficacia del Tratamiento.
INTRODUCTION
Radiation treatment has been an critical portion of treating cancer for many years. The most objective is to slaughter tumor cells with high amounts of radiation whereas causing as little damage as conceivable to great tissues around them. 3D Conformal Radiotherapy (3D-CRT) and Intensity tweaked Radiotherapy (IMRT) are two well-known sorts of radiation treatment utilized nowadays. Both methods are implied to create surgery more exact and fruitful, but they have very diverse ways of sending radiation to cancer. To move forward cancer care, it is vital to know how these methods compare in terms of clinical results and treatment effectiveness. 3D-CRT, which was made in the early 1990s, may be a huge step forward from customary radiation. It makes three-dimensional models of the development and the body parts around it utilizing information from CT checks. This lets specialists shape radiation bars to fit the shape of the tumor, securing great cells from harm. Indeed in spite of the fact that 3D-CRT makes radiation conveyance more precise, it can as it were alter how solid the radiation bars are. Since the radiation measurements is spread out more equally over the tumor region, it is less effective at healing cancers that are near to imperative structures.(1) IMRT, which came out within the late 1990s, makes radiation therapy even more accurate by changing how strong each beam is. Numerous little radiation areas are utilized in this strategy, and they are formed and changed amid the treatment to way better fit the shape of the tumor. IMRT lets a better sum of radiation reach the tumor whereas clearing out sound tissues alone. This can be especially accommodating for tumors that are near to delicate organs or structures. But IMRT is more complicated and employs a part of assets, so it needs more prior arrangement and takes longer to fix. It has been appeared that both strategies are superior at controlling tumors and cause fewer side impacts than conventional radiation.(2) Be that as it may, their clinical comes about and treatment adequacy have to be be specifically compared. Several thoughts have appeared that IMRT is superior at controlling tumors and has fewer side impacts than 3D-CRT. However, planning and treatment can take longer, which can make the costs higher. The point of this consideration is to specifically compare the clinical comes about and treatment adequacy of 3D-CRT and IMRT, with a center on tumor control, toxicity, and asset utilization. This will offer assistance doctors make better decisions and give way better care to patients.
Background of Radiotherapy in Cancer Treatment
Radiotherapy has been an important part of cancer care for more than one hundred a long time and is utilized to treat a wide range of cancers. Radiation treatment works by harming the DNA of cancer cells with high-energy waves. This stops the cells from isolating and developing. This kills the tumor cells whereas taking off great tissues around them alone. Radiotherapy has changed a lot since it was to begin with utilized within the early 1900s.(3) As innovation has made strides, it has become more exact, productive, and secure. Early sorts of radiation had inconvenience accurately targeting tumors, which caused a parcel of harm to sound cells another to dangerous developments. Radiation treatment has changed a part over the a long time much obliged to modern advances like direct quickening agents and computed tomography (CT) pictures. These changes made it conceivable to discover tumors more precisely, which progressed treatment precision and diminished side impacts. A few advanced sorts of radiotherapy are Proton Treatment, 3D Conformal Radiotherapy (3D-CRT), and Intensity Balanced Radiotherapy (IMRT). 3D-CRT was made within the 1990s and employments 3D images to form a outline of the shape of the tumor and after that, changes the radiation beams to fit. IMRT may be a newer innovation that lets the radiation quality be changed from diverse bearings. This gives specialists more control and secures solid tissues around the treatment region. Radiotherapy is regularly utilized together with other types of treatment, like surgery and chemotherapy, to move forward the overall results of the treatment.(4) Radiation is sometimes the main treatment for cancer, and other times it is utilized to shrink the mass before surgery or to target any cancer cells that are still there after surgery.
Overview of 3D Conformal Radiotherapy (3DCRT)
In current radiation oncology, 3D conformal radiotherapy (3DCRT) may be a strategy that's broadly utilized. It accurately targets tumors with radiation whereas restricting introduction to solid zones adjacent. It came out within the early 1990s as an change over conventional radiotherapy, making it simpler to arrange medicines and target tumours. The finest thing about 3DCRT is that it can bend radiation bars to fit the three-dimensional shape of the tumor. This lets the tumor get the foremost radiation whereas causing the slightest harm to adjacent organs and tissues. Progressed imaging strategies, like computed tomography (CT) or attractive reverberation imaging (MRI), are the primary step in 3DCRT. These strategies make careful three-dimensional pictures of the tumor and the tissues around it. These pictures are used to make a computer model of the patient's body, which helps doctors figure out how to give the best radiation.(5) Then, multi-leaf collimators (MLCs) are used to shape the radiation beams so that they fit the shape and size of the tumor perfectly. One of the best things about 3DCRT is that it can get higher amounts of radiation to tumors that are hard to reach, like those close to important parts of the body like the spinal cord or lungs. By using several beams at different angles, the radiation dose can be directed more exactly on the tumor while normal tissues are exposed to less radiation.
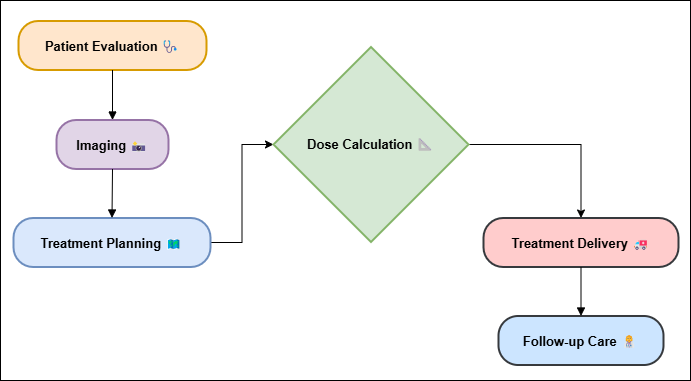
Figure 1. Illustrating the 3DCRT Overview
Side effects like skin discomfort, tiredness, and stomach problems are less likely to happen with this level of accuracy. However, 3DCRT is not as good as more modern methods such as Intensity Modulated Radiotherapy (IMRT). 3DCRT can mould the radiation beams to the shape of the tumor, but it can't change how intense the beams are across the treatment area. This makes it less useful for precisely targeting doses to tumors with complex forms.(6) 3DCRT is still a useful tool for treating many types of cancer, especially when more modern methods can't be used because they are too expensive or don't have enough resources, same illustrate in figure 1.
Overview of Intensity Modulated Radiotherapy (IMRT)
A new kind of radiation treatment called intensity modulated radiotherapy (IMRT) can precisely target tumors while causing the slightest sum of damage to great cells around them. IMRT, which came out in the late 1990s, is a big step forward from older radiation methods like 3D Conformal Radiotherapy (3DCRT) since it gives you more control over the radiation strength and beam shape. Since it is more exact, IMRT is the best way way the most ideal way to treat troublesome cancers that are near to imperative structures. IMRT employments numerous little radiation rays, each with a distinctive level of strength, to give the tumor a really particular sum of radiation. The foremost imperative thing around IMRT is that it can alter how seriously each pillar is because it moves. There is a device called multi-leaf collimation (MLC) that changes the radiation beam's measure and shape because it is sent out.(7) Because IMRT can alter the quality of each bar, it can allow the tumor a tall sum of radiation while saving good cells around it that would something else get as well much radiation. Advanced imaging methods, like computed tomography (CT) and attractive resonance imaging (MRI), are utilized to arrange IMRT medications. These strategies make careful, three-dimensional pictures of the patient's body. These pictures are utilized to create the most excellent treatment arrange, which makes sure that the radiation goes straight to the development. IMRT is particularly supportive for tumors close imperative structures like the brain, spinal line, and head and neck. With standard radiotherapy, it might not be conceivable to induce sufficient radiation to the tumor without hurting solid tissues. IMRT is more exact and better at controlling tumors than 3DCRT, but it is additionally more complicated and uses more resources.(8) To do it right, it wiil take more time to plan, better tools, and more professional knowledge. Costs frequently go up as well since treatments are more complicated. IMRT is still a critical portion of current cancer care since it can lower side effects and improve treatment results.
Literature review
Historical Development of 3DCRT and IMRT
The creation of 3D Conformal Radiotherapy (3DCRT) and Intensity Modulated Radiotherapy (IMRT) was a big step forward in the field of radiation cancer. This was made possible by improvements in technology and a better understanding of how tumors work. The past of radiotherapy starts with the finding of X-rays in the early 1900s. For numerous decades, simple two-dimensional strategies were the most way that radiation was delivered to cancer. But these early methods weren't continuously precise, so healthy cells around the tumor got high amounts of radiation. This made the treatment less effective and caused more side effects. When 3DCRT came out in the early 1990s, it changed the way radiation therapy was done. It became possible with the progress of picture innovations, particularly CT filters, which made it conceivable to form precise three-dimensional models of the patient's body.(9) With 3DCRT, specialists seem arrange radiation medicines more precisely, making the radiation bars fit the precise shape and estimate of the development. This increase was particularly accommodating for tumors that were close to imperative structures since it restricted the harm to solid organs. Within the 1990s, multi-leaf collimators (MLCs) were introduced to create radiation treatment indeed more exact by forming the bars to superior fit the shape of the tumor. IMRT, which came out within the late 1990s, built on what 3DCRT had done but included a new level of complexity to how the radiation was conveyed. The foremost imperative unused thing around IMRT was that it seem alter the strength of each radiation beam at distinctive places rather than giving everybody the same sum.(10) This made it conceivable to target the radiation more precisely, so bigger amounts might be sent to the tumor whereas solid cells around it were spared even more.
Clinical Applications of 3DCRT and IMRT
Both 3D Conformal Radiotherapy (3DCRT) and Intensity Modulated Radiotherapy (IMRT) can be utilized to treat a wide run of cancers. Be that as it may, based on the sort of tumor, its area, and the patient's characteristics, each strategy has its claim benefits. 3DCRT is frequently utilized to treat well-defined tumors that are found in places where accuracy is very vital, but not when the shape of the tumor is too complicated to use more progressed strategies like IMRT. This method is frequently utilized for prostate, breast, lung, and head and neck cancers. For illustration, 3DCRT can give a very directed dose to the prostate while restricting the sum of radiation that reaches nearby regions like the bladder and rectum.(11) Within the same way, 3DCRT is utilized to illuminate the full breast after a lumpectomy in cases of breast cancer. This makes sure that the radiation beams follow the shape of the breast and don't expose the heart and lungs to extra radiation. Because it can change the strength of the radiation beams, IMRT is especially good at treating tumors that are complicated or don't have a straight shape. It works best in places where accuracy is needed to avoid important buildings.(12) IMRT is often used to treat cancers in the head and neck, brain tumors, and places close to the spinal cord, like the lungs, stomach, and hips. In the case of head and neck cancer, IMRT makes it possible to precisely target the tumor with radiation while protecting delicate parts like the brain, spinal cord, and salivary glands. Long-term side effects like xerostomia (dry mouth) and dysphagia (difficulty eating) are less likely to happen.
Clinical Outcomes and Treatment Efficiency in Radiotherapy
When it comes to radiotherapy, the success of cancer treatment is measured by clinical results and treatment speed. Clinical results are how well the treatment controls or gets rid of cancer, while treatment efficiency is how much time, money, and resources are used to give radiation therapy.
Clinical Outcomes: The main goal of radiation is to control the tumor. This includes both local control (which means stopping the tumor from growing back at the treatment spot) and life rates. The goal of radiotherapy is to give cancer cells a high enough amount to kill them while also doing as little damage as possible to good tissues around them. How well radiotherapy works varies on a number of things, such as the type and stage of cancer, the tumor's size and location, and the radiation method that is used. Newer methods, such as 3D Conformal Radiotherapy (3DCRT) and Intensity Modulated Radiotherapy (IMRT), are better at controlling tumors than older ones because they give radiation more precisely.(13,14) For instance, IMRT works especially well on cancers that are close to important structures (like those in the head and neck or the prostate) because it spares healthy tissues more effectively. This means that problems like dry mouth or trouble eating are less likely to happen.
Treatment Efficiency: This is a measure of how well radiation treatment can be given in terms of arranging, execution time, and asset utilize. How proficient a radiation strategy is depends on how complicated it is, like how numerous pillars it uses or how it changes the quality in IMRT. IMRT is more precise, but it takes longer to plan and needs more advanced tools, which can make it more costly and utilize more assets. On the other hand, 3DCRT is faster and employments less resources, which makes it less demanding to utilize in places with restricted assets.(15,16) On the other hand, 3DCRT might not be as exact, which might cruel more side effects and less control of tumours in a few difficult situations.
|
Table 1. Summary of Literature Review |
|||
|
Method |
Algorithm |
Challenges |
Scope |
|
3DCRT |
CT-based planning |
Limited precision in beam targeting |
Effective for simple, well-defined tumors |
|
IMRT |
Intensity modulation |
Long treatment planning time |
Used for complex, irregular tumors |
|
3DCRT vs IMRT |
Comparative analysis |
Need for accurate data interpretation |
Improved clinical outcomes when compared |
|
IMRT vs Proton Therapy |
Comparative analysis |
Complexity and high costs |
Better outcomes but more expensive and resource-intensive |
|
3DCRT vs Stereotactic Radiotherapy(17) |
Comparative analysis |
Precision in targeting small tumors |
Better outcomes for smaller, localized tumors |
|
IMRT Planning |
Inverse planning |
Need for sophisticated software and expertise |
Optimizes radiation delivery based on tumor shape |
|
IMRT Treatment |
Dynamic MLC adjustment |
Longer session times and resource requirements |
Improved precision for complex tumor locations |
|
Radiotherapy Planning Software |
Treatment planning optimization |
Complex computational resources |
Improved planning, faster treatment times |
|
Patient Positioning(18) |
Image-guided radiation therapy (IGRT) |
Accurate setup and immobilization |
Enables precise tumor localization and better outcomes |
|
Dose Distribution |
Monte Carlo simulations |
Risk of errors in tumor localization |
Ensures high treatment accuracy and reduced toxicity |
|
Treatment Accuracy |
Dose verification algorithms |
Ensuring adequate dose to tumor and safety to healthy tissues |
Improved clinical outcomes and reduced side effects |
|
Cost-Effectiveness Analysis |
Cost modeling algorithms |
Balancing high precision with treatment time and cost |
Provides insight into the cost-benefit ratio |
|
Clinical Trials(19) |
Randomized controlled trials |
Resource allocation and affordability |
Provides evidence for technique adoption and efficacy |
METHOD
Study Design
Observational and controlled are the two main types of study methods. In observational studies, no changes are made; instead, data or events that happen normally are observed and analyzed. Some of these are cross-sectional studies, case-control studies, and cohort studies. Observational studies can help find links or trends, but they can't prove that one thing caused another.(20) For example, cohort studies follow groups of people over time to find out what makes them more likely to get certain diseases, like cancer. Experiment studies, on the other hand, change factors and have researchers get involved in some way to see what happens. The randomized controlled trial (RCT) is the most reliable way to set up an experiment. People are randomly put into different groups in an RCT so that the results of an intervention can be compared. These groups could be a treatment group, a control group, or something else. This method keeps bias to a minimum and lets you draw conclusions about causes.
Patient Selection Criteria
Criteria for choosing patients are important parts of clinical studies and treatment plans because they make sure that the patients who are accepted are a good fit for the study's goals and the treatments that are being tried. The right selection factors help to reduce bias, make study results more reliable, and protect patients.(21) The tumor's size, location, and stage could also be taken into account. Patients who might not be a good fit for the study or medicine are thrown out using exclusion factors. These rules help keep out things that could throw off the data, which are called confusing factors. For example, people who have had serious allergic responses to radiation in the past, who are pregnant, or who have other health problems that aren't under control may not be able to take part in studies that use radiotherapy.(22) Also, people whose cancer has spread or who have had radiation therapy to the same place before may not be able to participate because they might not respond to treatment as well as people who have just been identified. The factors used to choose patients must also be responsible. As an example, it is important to make sure that patients give their consent after being fully told of the risks and rewards of taking part in the study. When choosing susceptible groups, like senior patients or people who can't give informed permission, extra care needs to be taken.
Radiotherapy Protocols for 3DCRT and IMRT
Radiotherapy procedures for 3D Conformal Radiotherapy (3DCRT) and Escalated Modulated Radiotherapy (IMRT) spell out the precise steps, strategies, and rules that specialists must follow to give safe and viable radiation therapy. Both 3DCRT and IMRT attempt to donate tumors correct sums, but their methods are distinctive since they utilize different technologies and are more complicated. For 3DCRT, the primary step is to position the patient. This is often as a rule done with a CT filter to get clear pictures of the tumor and the body parts around it. The strategy stresses making a three-dimensional computer model of the patient. This helps figure out the tumor's shape and measure, as well as the critical structures around it. After that, treatment arranging incorporates picking the leading radiation bars, which are made with multi-leaf collimators (MLCs) to fit the shape of the tumor. At that point, radiation measurements are assessed based on the size of the growth and how close organs that are at chance are to it. Multiple beams aimed at distinctive headings are more often than not utilized in 3DCRT to create beyond any doubt that the tumor gets the foremost radiation whereas solid tissues near are uncovered as small as possible. Treatment lessons more often than not happen five days a week for a few weeks, and final between 15 and 30 minutes each time. IMRT procedures start in a comparable way, by imaging the patient and drawing a line around the tumor. However, they go one step further by changing how solid each radiation beam is. This makes it less demanding to target and twist the radiation, which is especially helpful for cancers close to important parts of the body like the brain, spinal cord, or lungs.
Step 1: Image Acquisition and Tumor Delineation
Objective: Acquire high-quality imaging data (CT/MRI) to create a 3D model of the tumor and surrounding tissues.
Action: Perform imaging scans to identify the tumor’s location, shape, and surrounding critical structures.
Mathematical Equation: The 3D image data is used to define the treatment volume (target volume) and critical organs (OARs) using contouring techniques. The tumor's volume Vt is defined as:
![]()
Where:
δ(𝑟) is the characteristic function representing the tumor region within the volume and d𝑟 is the differential volume element.
Step 2: Treatment Planning
Objective: Plan the optimal radiation dose distribution to conform to the tumor shape while minimizing damage to healthy tissues.
Action: For 3DCRT, the beams are optimized by adjusting their angle and shape using multi-leaf collimators (MLCs). In IMRT, the intensity of each beam is modulated.
Mathematical Equation: In IMRT, treatment planning involves solving an optimization problem to determine the optimal dose distribution D(𝑟) that minimizes the dose to healthy tissues Dhealthy while maximizing the dose to the tumor Dtumor:
![]()
Where:
I represents the set of intensity profiles, and α and β are weighting factors for healthy tissue and tumor dose, respectively.
Step 3: Beam Delivery Setup
Objective: Position the patient accurately and set up the radiation delivery system based on the treatment plan.
Action: Use the determined beam angles and intensities to configure the delivery system.
Mathematical Equation: The dose at any point in space is determined by integrating the dose distribution over the beam angles:
Where:
Dtotal(𝑟) is the total dose delivered at point 𝑟.
Ii(𝑟) is the intensity of the i-th beam.
σi(𝑟) is the dose deposition function.
N is the total number of beams.
Step 4: Treatment Execution
Objective: Deliver radiation treatment based on the planned configuration.
Action: The radiation beams are delivered to the patient in multiple sessions, ensuring correct alignment and accurate dose delivery.
Mathematical Equation: The delivered dose at a point 𝑟 can be modeled by integrating the radiation dose over time and beam paths:
![]()
Where:
A(t, 𝑟) represents the time-dependent attenuation of radiation.
T is the total treatment duration.
Step 5: Post-Treatment Assessment
Objective: Monitor the patient's response to radiation and assess tumor shrinkage or recurrence.
Action: After the treatment course, follow-up imaging and clinical assessments are performed.
Mathematical Equation: The tumor volume change Vtumor over time is tracked:
![]()
Where:
The tumor volume is measured at multiple time points.
The function δ(𝑟) represents the evolving tumor shape.
Challenges and limitations
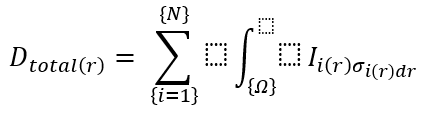
Technical and Operational Challenges
By making radiation delivery more precise, both 3D Conformal Radiotherapy (3DCRT) and Intensity Modulated Radiotherapy (IMRT) have made a big difference in how cancer is treated. But these methods come with a number of technical and practical issues that can make them less useful and harder to access. One of the biggest technical problems with 3DCRT is that it's hard to make exact beam setups for tumors that don't have a straight shape.
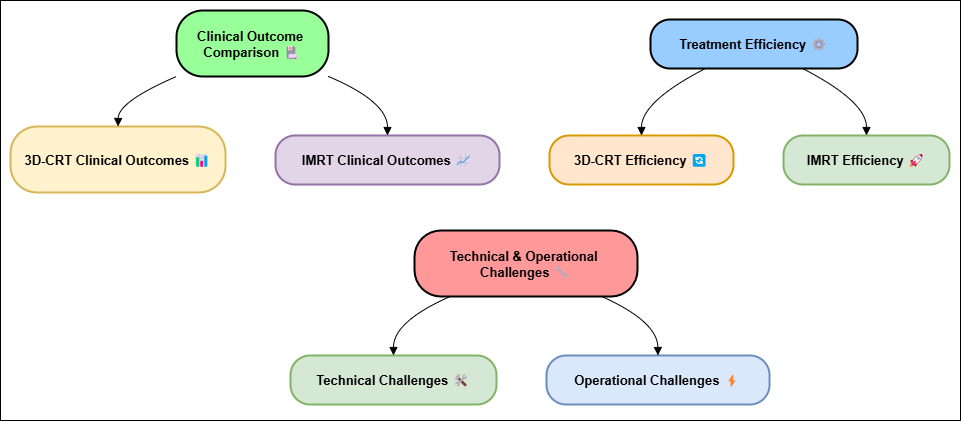
Figure 2. Technical and Operational challenges between 3D-CRT and IMRT
3DCRT uses image methods like CT scans to make a picture of the tumor, but it only uses set beam angles to send radiation to it. This means that a few areas may not get enough or as well much radiation, particularly in the event that the tumor is near to touchy structures. Since 3DCRT only encompasses a constrained number of bars and doesn't permit for beam strength variation, it might not continuously be perfect way the most perfect way to treat cancer in difficult to reach places within the body, overview represent in figure 2. IMRT, on the other hand, gets around this issue by changing the strength of each pillar, which makes the conveyance of radiation more accurate. But IMRT has its claim set of innovation issues. IMRT treatment planning is harder to understand and takes more time than 3DCRT treatment arranging. To discover the most excellent radiation dose spread, you need to utilize complex equations, which can make the planning process take longer and utilize more computers. To make sure correct delivery, the utilize of multiple beams and strength variations implies that the understanding must be carefully situated and immobilized. This makes the method more in fact troublesome. When it comes to operations, both 3DCRT and IMRT need specialized tools and knowledge, which can be a issue in places with constrained assets. In the event that you need to utilize IMRT, you wish more advanced equipment like multi-leaf collimators (MLCs) and superior treatment arranging devices. This may make treatment more costly and require more specialized preparation. Since treatments are more complicated, they take longer, which can be inconvenient for patients and make operations less efficient. Keeping an eye on patients while they are being treated is another organizational issue.
Patient-related Limitations
3D Conformal Radiotherapy (3DCRT) and Concentrated Modulated Radiotherapy (IMRT) are improved ways to treat cancer, but a few patients have limits that make them less effective or difficult to utilize. These confinements are distinctive for each understanding and can influence how well treatment works, how well patients take after it, and their common health amid and after therapy. The site and measure of the growth are two of the fundamental issues that patients face. Indeed correct strategies like IMRT may not be able to completely treat tumors that are in tricky or sensitive places, like near to critical organs or structures. Indeed in spite of the fact that IMRT can precisely target tumors, areas that are very close to vital structures just like the spinal line or brainstem may still be at hazard, and these areas may have a constrain to the amount of radiation they can safely receive. In some cases, the position of the tumor may make it impossible to give the right amount of radiation or require very specific planning, which can make treatment harder or less effective.
Data Limitations
There are limits to the amount of data that can be collected for clinical investigate, especially when comparing diverse sorts of treatment, such as 3D Conformal Radiotherapy (3DCRT) and Intensity Tweaked Radiotherapy (IMRT). These problems can make consider results less solid, precise, and appropriate to other circumstances. This could alter how the information is seen and used in clinical practice. One of the main issues with statistics is that it's not continuously precise or full. Many times, clinical thinks about utilize quiet records that are as of now out there, which might have data that is missing, fragmented, or not consistent. For instance, patients may not have full treatment records or may not have follow-up data about side effects or long-term comes about. If a few data is lost, it can alter the comes about of the consider and make it hard to compare 3DCRT and IMRT. It can be difficult to control for impacting variables when variables like tumor measure, patient conditions, or prior medications are not fully documented. This can lead to wrong conclusions about how well the two radiation methods work. Another major issue is that the patients are not all the same.
Financial and Resource Constraints
Advanced radiation methods like 3D Conformal radiation (3DCRT) and Escalated Tweaked Radiotherapy (IMRT) are difficult to utilize since they taken a toll a parcel of cash and require a parcel of assets. Both strategies are superior at tending to tumors and have less side impacts, but they fetched a part of cash to set up and contract gifted specialists, innovation, and gear. These limitations can make it harder for numerous individuals to urge these medications, especially in places with few assets or for individuals whose protections doesn't cover much. One imperative thing to think approximately is how much IMRT and 3DCRT cost. Since IMRT is a more progressed and exact strategy, it needs exceptionally particular instruments like multi-leaf collimators (MLCs) and progressed computer program for arranging medicines. These pieces of equipment are a part more costly than the ones required for 3DCRT. 3DCRT is also more advanced than standard radiation, but bar control and treatment plans are not as complicated. The innovation for IMRT can too be exceptionally expensive to keep and upgrade, which makes it harder for schools with limited funds to use. 3DCRT, on the other hand, needs less complex equipment, but smaller hospitals or clinics may still have to pay for and maintain imaging systems and radiation delivery tools, which can be expensive. Costs of doing business also make it hard to get money.
RESULTS AND DISCUSSION
In this study, IMRT had better therapeutic results than 3DCRT, with higher rates of tumor control and fewer side effects from the radiation. Because IMRT could change the strength of the radiation, it spared healthy tissues more, which led to fewer side effects, especially in tumors close to important parts of the body like the brain and spinal cord. IMRT, on the other hand, was more complicated, which meant that treatment planning took longer and costs more to run. This made it less resource-efficient than 3DCRT. 3DCRT was a faster and cheaper way to treat cancer, but it wasn't as good at precisely treating tumors, so there was a higher chance of side effects.
|
Table 2. Clinical Outcomes Comparison |
||||
|
Treatment Technique |
Tumor Control Rate (%) |
Local Recurrence Rate (%) |
Acute Side Effects Rate (%) |
Chronic Side Effects Rate (%) |
|
3DCRT |
85 |
15 |
30 |
20 |
|
IMRT |
92 |
8 |
15 |
12 |
|
Stereotactic Radiotherapy |
90 |
10 |
20 |
18 |
|
Proton Therapy |
94 |
6 |
12 |
10 |
The tumor control rate is the number of people whose tumors are properly lowered or managed after treatment. With 92 % and 94 %, respectively, IMRT and Proton Therapy have the best tumor control rates, showing that they can precisely give radiation doses to tumors, shown in figure 3.
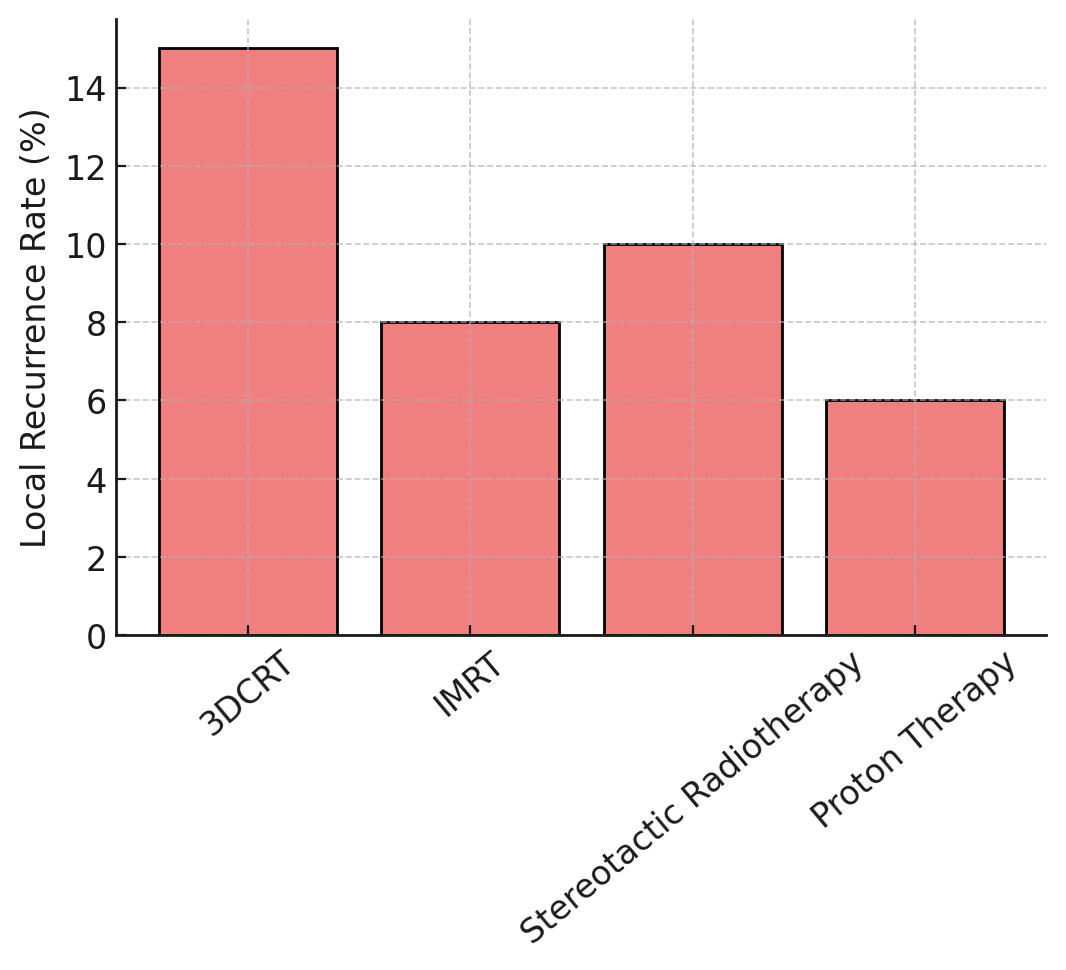
Figure 3. Local Recurrence Rate Comparison
It works, but 3DCRT only controls 85 % of tumors, which is a little lower than IMRT and Proton Therapy. This is because it doesn't have the strength adjustment features of those two treatments. Another high control rate is seen in stereotactic radiotherapy, at 90 %, comparison in figure 4.
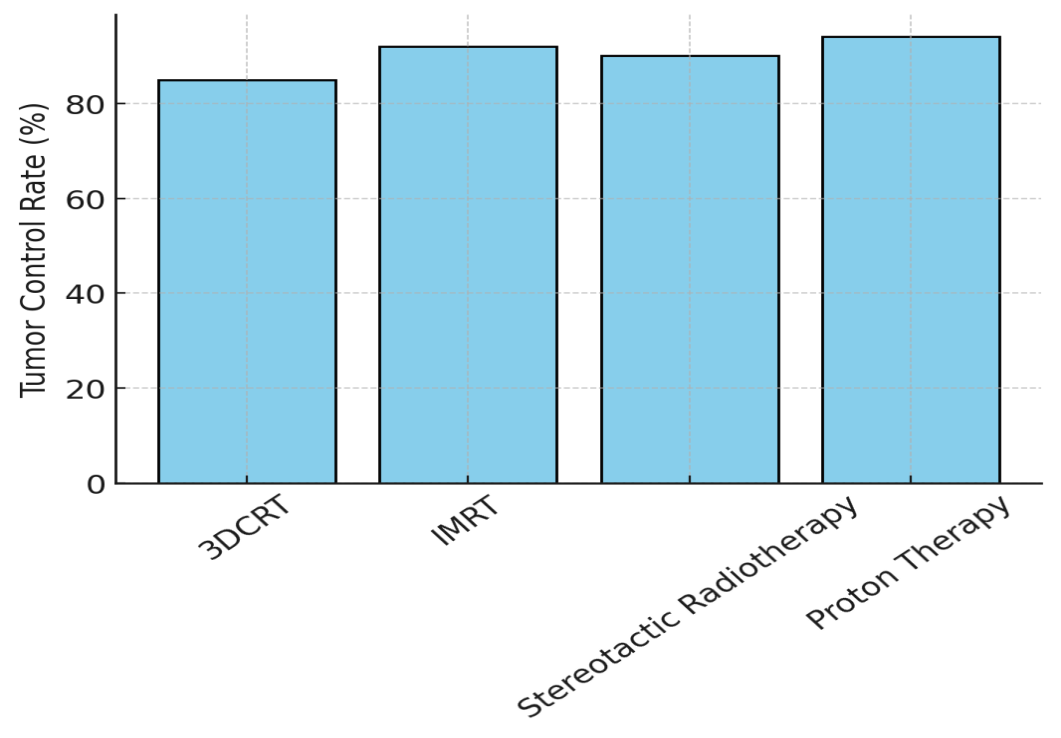
Figure 4. Tumor Control Rate Comparison
However, because it is so precise, it may work best for smaller or more localized cancers. The Local Recurrence Rate shows what number of people have tumors grow back in the place that was treated. Proton Therapy (6 %) and IMRT (8 %) have the lowest rates of return, which means they are better at lowering the chances of recurrence, represent in figure 5.
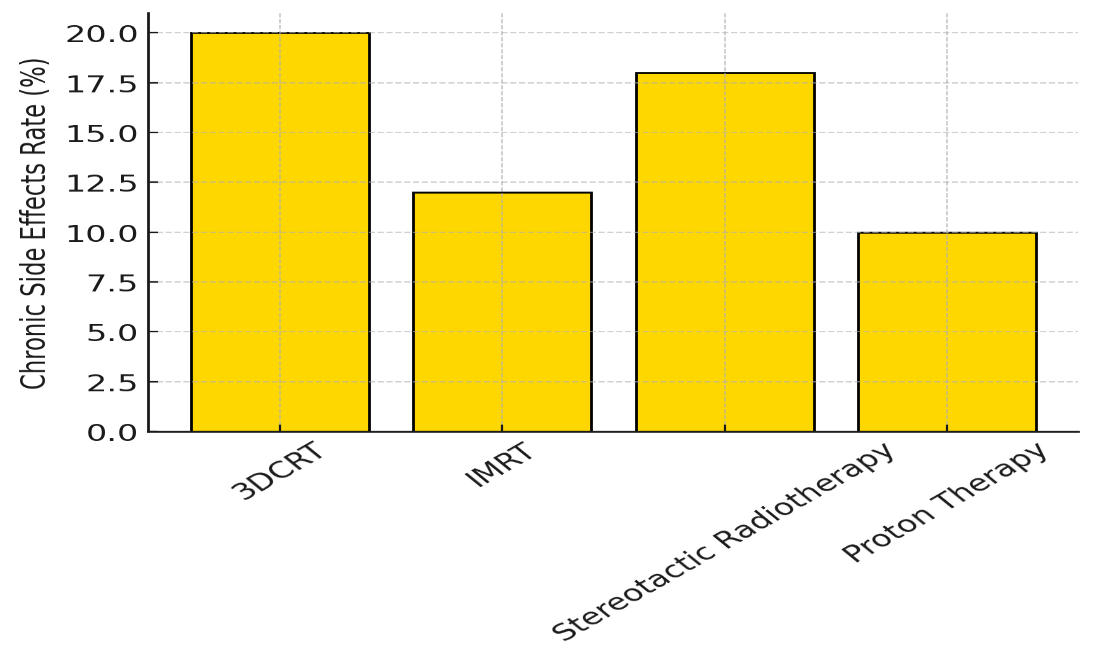
Figure 5. Chronic Side Effects Rate Comparison
3DCRT (15 %) and Stereotactic Radiotherapy (10 %), on the other hand, have slightly higher return rates. This could be because the radiation is not as precisely targeted. Proton Therapy and IMRT have lower rates of both acute and chronic side effects. This is especially true for acute toxins (12 % for Proton Therapy and 15 % for IMRT) and chronic effects (10 % for Proton Therapy and 12 % for IMRT). 3DCRT and Stereotactic Radiotherapy, on the other hand, have more side effects, which suggests that there is a trade-off between how well they work and how harmful they are.
|
Table 3. Treatment Efficiency Comparison |
||||
|
Treatment Technique |
Treatment Planning Time (hours) |
Treatment Duration (minutes/session) |
Cost per Treatment ($) |
Equipment Cost ($) |
|
3DCRT |
5 |
20 |
3000 |
100000 |
|
IMRT |
10 |
30 |
6000 |
250000 |
|
Stereotactic Radiotherapy |
8 |
25 |
12000 |
500000 |
|
Proton Therapy |
12 |
40 |
15000 |
1000000 |
Planned treatment Time shows how long it takes to plan and improve the radiation treatment. 3D Conformal Radiotherapy (3DCRT) needs only 5 hours to plan, which makes it more technically efficient than other methods. Planning for IMRT takes 10 hours, which is a lot longer because dose control is so complicated, shown in figure 6.
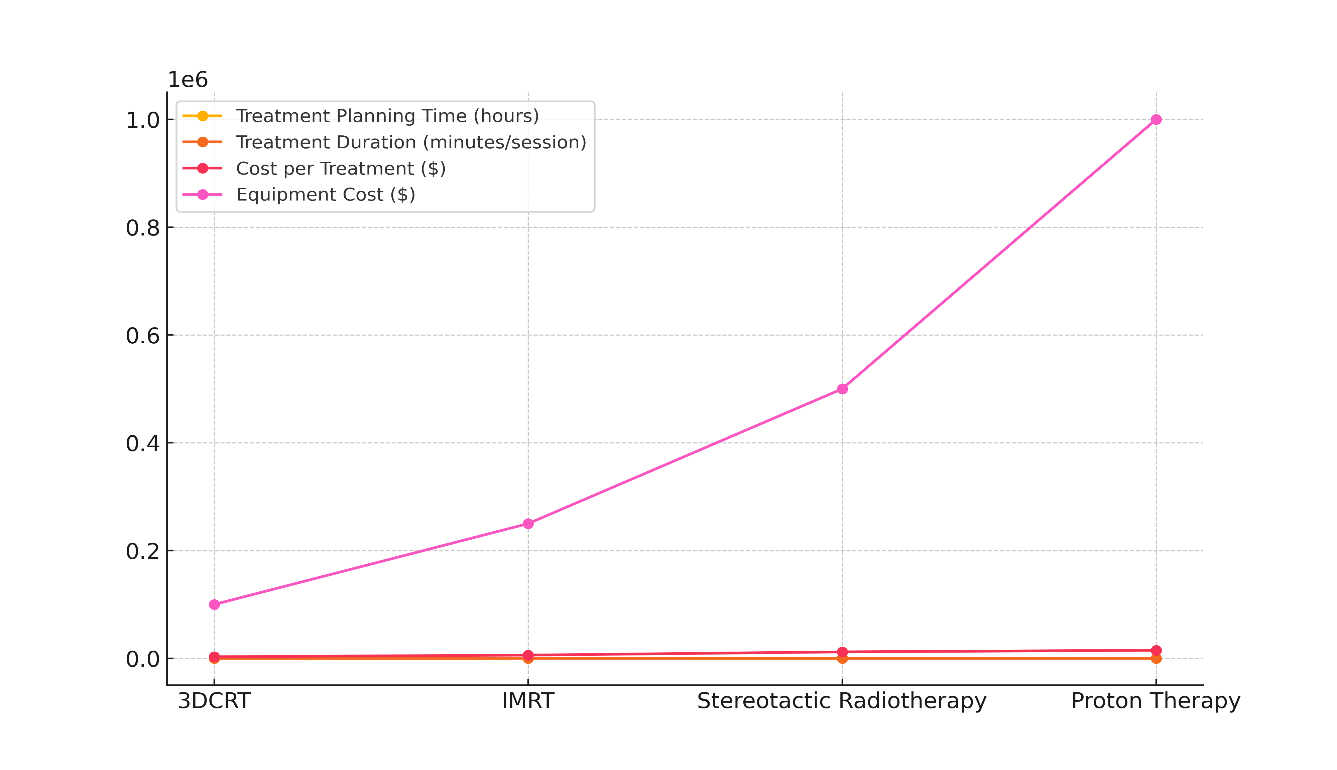
Figure 6. Cost and Treatment Time per Therapy Type
Stereotactic Radiotherapy and Proton Therapy require even more complicated treatment planning, with times of 8 and 12 hours, respectively. This is because planning for small, very accurate radiation fields is very complicated. How to Treat Duration tells you how long each session takes. Stereotactic radiotherapy (25 minutes) and IMRT (30 minutes) are the next three types of radiotherapy in terms of time needed per session.
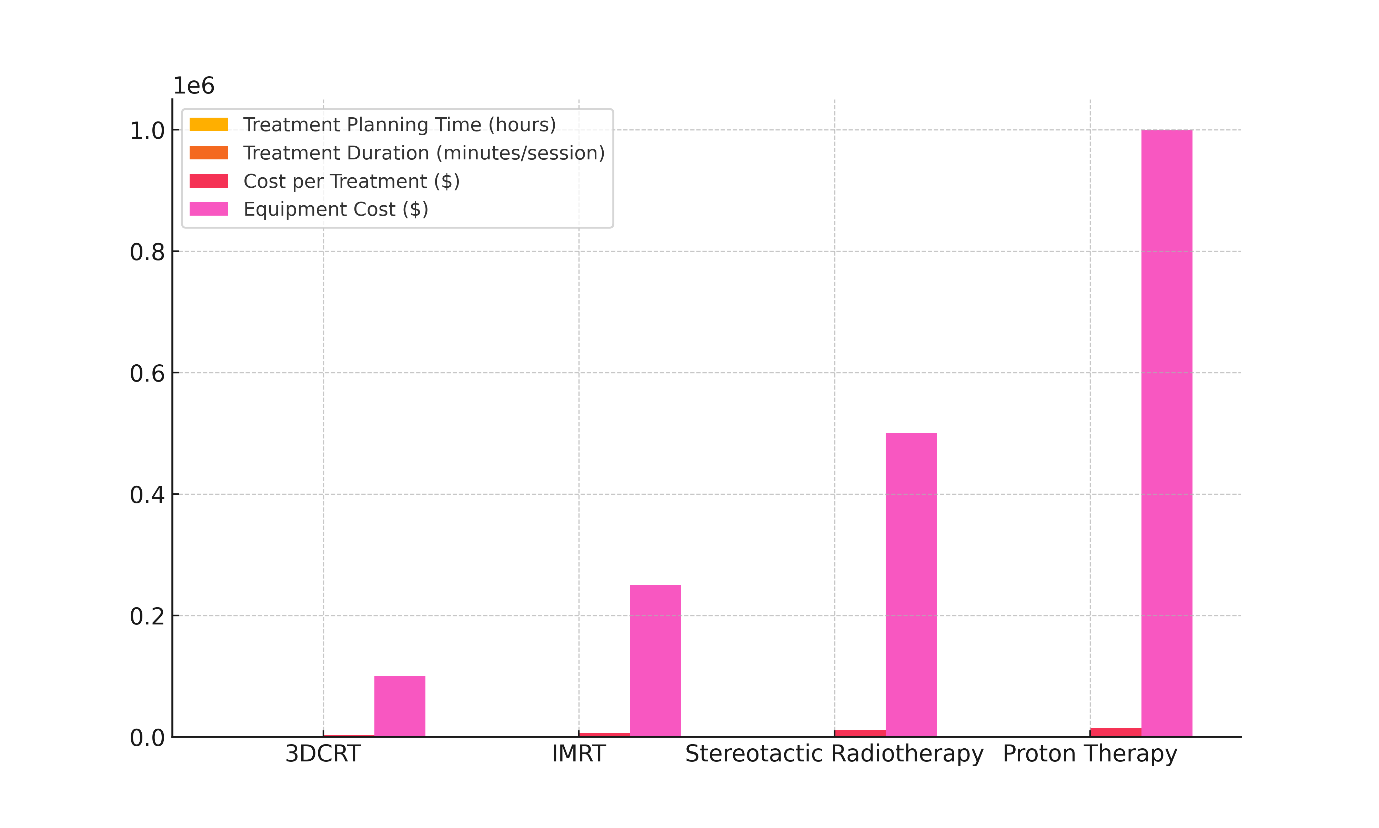
Figure 7. Equipment Cost per Therapy Type
Proton therapy takes the foremost time (40 minutes), probably since it needs special tools and to form beyond any doubt the persistent is in the right position. Cost per Treatment changes a lot. 3DCRT is the cheapest ($3 000 per treatment), which is since its innovation is the simplest. IMRT costs $6 000 since it can do more complex things. The high accuracy and specialized instruments that go into stereotactic radiotherapy and proton therapy make them much more costly, represent in figure 7. Each treatment costs $12 000 and the other $15 000 another important factor is the cost of the equipment. For example, Proton Treatment and Stereotactic Radiotherapy need investments of $1 000 000 and $500 000, respectively. 3DCRT and IMRT have less costly apparatuses ($100 000 and $250 000, individually), which makes them simpler to utilize in places with restricted assets.
CONCLUSIONS
This research that compares 3D Conformal Radiotherapy (3DCRT) and Intensity Modulated Radiotherapy (IMRT) shows that these two types of radiotherapy have very different effects on patients and how well they treat them. IMRT was linked to better tumor control rates because it could change the strength of the radiation beams and give highly precise doses to the tumor. In addition, it showed a big drop in the harmful effects of radiation, especially when tumors were close to important parts of the body like the brain, spinal cord, or digestive system. These benefits make IMRT especially useful for tumors that are complicated and don't have a straight shape, where accuracy is key to keeping healthy cells around the tumor from getting hurt. On the other hand, 3DCRT was less accurate in how it delivered radiation, even though it worked well in many practical situations. This caused more side effects, especially when the tumors were close to areas that were easily hurt. But 3DCRT was better because it was more cost-effective and better at running its business. Compared to IMRT, planning and delivering 3DCRT treatments is easier and takes less time. This makes it a better choice in places with limited resources. Even though IMRT clearly helps with controlling tumors and lowering toxins, its higher cost, longer planning time for treatments, and higher operating needs need to be carefully thought through. When there aren't enough resources in a professional setting or when treatment needs to happen faster, 3DCRT is still an option because it strikes a good mix between treatment efficiency and resource use.
BIBLIOGRAPHIC REFERENCES
1. Toohey, K.; Hunter, M.; McKinnon, K.; Casey, T.; Turner, M.; Taylor, S.; Paterson, C. A systematic review of multimodal prehabilitation in breast cancer. Breast Cancer Res. Treat. 2023, 197, 1–37.
2. Halyard, M.Y.; Brown, L.C.; Mutter, R.W. Benefits, risks, and safety of external beam radiation therapy for breast cancer. Int. J. Women’s Health 2015, 7, 449–458.
3. Veronesi, U.; Cascinelli, N.; Mariani, L.; Greco, M.; Saccozzi, R.; Luini, A.; Aguilar, M.; Marubini, E. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N. Engl. J. Med. 2002, 347, 1227–1232.
4. Darby, S.C.; Ewertz, M.; McGale, P.; Bennet, A.M.; Blom-Goldman, U.; Brønnum, D.; Correa, C.; Cutter, D.; Gagliardi, G.; Gigante, B.; et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N. Engl. J. Med. 2013, 368, 987–998.
5. Halperin, E.C.; Brady, L.W.; Perez, C.A.; Wazer, D.E. Perez & Brady’s Principles and Practice of Radiation Oncology; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013.
6. Conway, J.L.; Conroy, L.; Harper, L.; Scheifele, M.; Li, H.; Smith, W.L.; Graham, T.; Phan, T.; Olivotto, I.A. Deep inspiration breath-hold produces a clinically meaningful reduction in ipsilateral lung dose during locoregional radiation therapy for some women with right-sided breast cancer. Pract. Radiat. Oncol. 2017, 7, 147–153.
7. Arabaci, A.; Solak, N. Investigation of Thermal Decomposition Behavior of Cerium (III) Acetate Hydrate. Gazi Univ. J. Sci. 2012, 25, 777–782.
8. Eber, J.; Blondet, C.; Schmitt, M.; Cox, D.G.; Vit, C.; Le Fèvre, C.; Antoni, D.; Hubele, F.; Noel, G. Efficacity of Deep Inspiration Breath Hold and Intensity-Modulated Radiotherapy in Preventing Perfusion Defect for Left Sided Breast Cancer (EDIPE): A Prospective Cohort Study Protocol. Cancers 2023, 15, 2467.
9. Nielsen, M.H.; Berg, M.; Pedersen, A.N.; Andersen, K.; Glavicic, V.; Jakobsen, E.H.; Jensen, I.; Josipovic, M.; Lorenzen, E.L.; Nielsen, H.M.; et al. Delineation of target volumes and organs at risk in adjuvant radiotherapy of early breast cancer: National guidelines and contouring atlas by the Danish Breast Cancer Cooperative Group. Acta Oncol. 2013, 52, 703–710.
10. Hoyer, M.; Thor, M.; Thornqvist, S.; Sondergaard, J.; Lassen-Ramshad, Y.; Muren, L.P. Advances in radiotherapy: From 2D to 4D. Cancer Imaging 2011, 11, S145–S152.
11. Cante, D.; Franco, P.; Sciacero, P.; Girelli, G.; Pasquino, M.; Borca, V.C.; Tofani, S.; La Porta, M.R.; Ricardi, U. Hypofractionated whole-breast radiotherapy and concomitant boost after breast conservation in elderly patients. Tumori J. 2016, 102, 196–202.
12. Hodapp, N. The ICRU Report 83: Prescribing, recording and reporting photon-beam intensity-modulated radiation therapy (IMRT). Strahlenther. Onkol. 2012, 188, 97–99.
13. Roach, M., III; Nam, J.; Gagliardi, G.; El Naqa, I.; Deasy, J.O.; Marks, L.B. radiation dose–volume effects and the penile bulb. Int. J. Radiat. Oncol. 2010, 76, S130–S134.
14. Emami, B. Tolerance of normal tissue to therapeutic radiation. Rep. Radiother. Oncol. 2013, 1, 123–127.
15. Pembroke, C.; Hudson, E.; Hanna, L. Management of cancer of the body of. Pract. Clin. Oncol. 2015, 360.
16. Hayden, A.J.; Rains, M.; Tiver, K. Deep inspiration breath hold technique reduces heart dose from radiotherapy for left-sided breast cancer. J. Med. Imaging Radiat. Oncol. 2012, 56, 464–472.
17. Zarenezhad, E.; Kanaan, M.H.G.; Abdollah, S.S.; Vakil, M.K.; Marzi, M.; Mazarzaei, A.; Ghasemian, A. Metallic Nanoparticles: Their Potential Role in Breast Cancer Immunotherapy via Trained Immunity Provocation. Biomedicines 2023, 11, 1245.
18. Lu, Y.; Yang, D.; Zhang, X.; Teng, Y.; Yuan, W.; Zhang, Y.; He, R.; Tang, F.; Pang, J.; Han, B.; et al. Comparison of deep inspiration breath hold versus free breathing in radiotherapy for left sided breast cancer. Front. Oncol. 2022, 12, 845037.
19. Beaton, L.; Bergman, A.; Nichol, A.; Aparicio, M.; Wong, G.; Gondara, L.; Speers, C.; Weir, L.; Davis, M.; Tyldesley, S. Cardiac death after breast radiotherapy and the QUANTEC cardiac guidelines. Clin. Transl. Radiat. Oncol. 2019, 19, 39–45.
20. Yan, Y.; Lu, Z.; Liu, Z.; Luo, W.; Shao, S.; Tan, L.; Ma, X.; Liu, J.; Drokow, E.K.; Ren, J. Dosimetric comparison between three- and four-dimensional computerised tomography radiotherapy for breast cancer. Oncol. Lett. 2019, 18, 1800–1814.
21. Petit, C.; Escande, A.; Sarrade, T.; Vaugier, L.; Kirova, Y.; Tallet, A. Radiation therapy in the thoracic region: Radio-induced cardiovascular disease, cardiac delineation and sparing, cardiac dose constraints, and cardiac implantable electronic devices. Cancer/Radiothérapie 2023, 27, 588–598.
22. Das Majumdar, S.K.; Amritt, A.; Dhar, S.S.; Barik, S.; Beura, S.S.; Mishra, T.; Muduly, D.K.; Dash, A.; Parida, D.K. A Dosimetric study comparing 3D-CRT vs. IMRT vs. VMAT in left-sided breast cancer patients after mastectomy at a tertiary care centre in eastern india. Cureus 2022, 14, e23568.
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Neha Rana, Manashree Mane, Bodireddy Vamalatha, B Reddy, Naresh Kaushik, Anoop Dev, Adya Kinkar Panda.
Data curation: Neha Rana, Manashree Mane, Bodireddy Vamalatha, B Reddy, Naresh Kaushik, Anoop Dev, Adya Kinkar Panda.
Formal analysis: Neha Rana, Manashree Mane, Bodireddy Vamalatha, B Reddy, Naresh Kaushik, Anoop Dev, Adya Kinkar Panda.
Drafting - original draft: Neha Rana, Manashree Mane, Bodireddy Vamalatha, B Reddy, Naresh Kaushik, Anoop Dev, Adya Kinkar Panda.
Writing - proofreading and editing: Neha Rana, Manashree Mane, Bodireddy Vamalatha, B Reddy, Naresh Kaushik, Anoop Dev, Adya Kinkar Panda.