doi: 10.56294/mw2024540
ORIGINAL
Problem-based learning and the use of ICT in medical education: a critical reflection
Aprendizaje basado en problemas y el uso de las TIC en la educación médica: una reflexión crítica
María del Rocío Carranza Alcántar1
![]() *,
Rosana Ruíz Sánchez2
*,
Rosana Ruíz Sánchez2 ![]() , Claudia Islas Torres1
, Claudia Islas Torres1
![]()
1Universidad de Guadalajara, Centro Universitario de los Altos. Tepatitlán, México.
2Universidad de Guadalajara, Centro Universitario de Guadalajara. Tepatitlán, México.
Cite as: G Carranza Alcántar M del R, Ruíz Sánchez R, Islas Torres C. Problem-based learning and the use of ICT in medical education: a critical reflection. Seminars in Medical Writing and Education. 2024; 3:540. https://doi.org/10.56294/mw2024540
Submitted: 12-12-2023 Revised: 09-04-2024 Accepted: 12-08-2024 Published: 13-08-2024
Editor: PhD.
Prof. Estela Morales Peralta ![]()
Corresponding Author: María del Rocío Carranza Alcántar *
ABSTRACT
Problem-Based Learning (PBL) and the use of Information and Communication Technologies (ICT) are transforming medical education, as they allow teaching and learning to adapt to the needs of the modern environment, which favors the development of practical skills to solve problems of future physicians. Based on the above, a theoretical reflection was made on the integration of PBL and ICT in medical education, based on the literature review in different databases, through which challenges and strategies for its implementation were identified. The results show that the main challenges are insufficient teacher training in PBL and ICT, resistance to change towards non-traditional methodologies and deficiencies in infrastructure; the need to update teaching materials and develop assessment methods that reflect competencies as practices also stands out. It is concluded that the integration of PBL and ICT in medical education is relevant to align teaching with current and future demands of the health sector, so higher education institutions must commit to these improvements to adequately prepare physicians in a constantly changing environment.
Keywords: ABP; ICT; Medical Education; Pedagogical Innovation.
RESUMEN
El Aprendizaje Basado en Problemas (ABP y el uso de las Tecnologías de la Información y la Comunicación (TIC) están transformando la educación médica, ya que permiten adaptar las necesidades del entorno moderno a la enseñanza y el aprendizaje, lo que favorece el desarrollo de habilidades prácticas para resolver problemas de los futuros médicos. A partir de lo anterior se realizó una reflexión teórica sobre la integración de ABP y TIC en la educación médica, con base en la revisión de literatura en distintas bases de datos, a través de los cuales se identificaron desafíos y estrategias para su implementación. Los resultados muestran que los principales desafíos son la capacitación insuficiente docentes en ABP y TIC, la resistencia al cambio hacia metodologías no tradicionales y las deficiencias en la infraestructura; también sobresale la necesidad de actualizar materiales didácticos y desarrollar métodos de evaluación que reflejen competencias como prácticas. Se concluye que la integración del ABP y las TIC en la educación médica es de relevancia para alinear la enseñanza a las demandas actuales y futuras del sector salud, por lo que las instituciones de educación superior deben comprometerse a estas mejoras para preparar adecuadamente a los médicos en un entorno en constante cambio.
Palabras clave: ABP; TIC; Educación Médica; Innovación Pedagógica.
INTRODUCTION
In recent years, active learning methodologies have boomed due to how they have been shown to support students in achieving the required learning. This has been coupled with technologies that have significantly transformed society, driving scientific advances in this field.(1)
In such a way, in the current context, where technology permeates every aspect of our lives, the significant impact that Information and Communication Technologies (ICT) and now Artificial Intelligence (AI) have had in education is indisputable. Adopting these new active methodologies and the tools in the classroom is not a luxury but an emerging necessity to adapt to the rapid and constant changes demanded by the knowledge society.(2)
In this sense, problem-based learning (PBL) is one of the methodologies that has been used the most in medical education,(3) that is, to teach those who study medicine and who wish to enter the workforce on a daily basis. It is an inductive learning technique where the student is the main agent of his or her education, focusing on developing practical skills in addition to the mere accumulation of knowledge.
The effectiveness of this active learning methodology is well established; however, one of the problems that frequently arises is that those in charge of the subjects or who are teachers in the medical field are unfamiliar with the use of PBL.(4) This presents a significant challenge since without the training and adaptability of teachers in this active methodology, it limits student learning.
If we add the infrequent use of technologies by teachers, or currently of AI, the implementation of new strategies is limited by instructors' lack of teaching and digital skills. As (5) indicates, the gap between what PBL requires, the use of technologies, and the current abilities of medical teachers can seriously hinder the teaching process.
On the other hand, resistance to change is also a critical factor affecting the adoption of PBL with ICT in medical education, as most medical professionals have traditionally relied on more directive teaching methods and may perceive PBL as a threat to their conventional methodologies.(6)
Another problem facing medical education when trying to implement PBL is designing relevant problems that integrate ICT or AI since, for this methodology to be genuinely successful, the difficulties posed must be authentic and reflect real situations that doctors face in their practice.(7)
For its part, the evaluation of learning in PBL environments that use ICT has been one of the significant complications since this methodology must measure not only theoretical knowledge but also practical and critical thinking skills, so designing an evaluation in this sense requires expertise and time to analyze both the qualitative and quantitative data generated from the use of technology in combination with problem-based learning.(8)
Linked to the above, technological infrastructure is an essential requirement for the success of PBL with ICT, but it is not always guaranteed, as the digital divide is still vast. In many institutions, the lack of reliable access to advanced technology and technical support can limit the implementation of these methodologies, such that without this infrastructure, this type of innovative methodology cannot be effectively executed.(9)
Based on the above, this critical reflection is presented on the subject of Problem-Based Learning (PBL) and the use of Information and Communication Technologies (ICT) in medical education, which aims to contribute to the academic literature by offering new perspectives and data to enrich it, as well as identifying gaps in existing research and defining the prospects for studies that can explore in depth the interactions between PBL, technologies and learning in medicine.
Problem-Based Learning (PBL)
PBL is an active learning methodology because it uses complex real-life problems as a starting point for learning, in which students work in small groups with the guidance of a tutor to explore and solve problems, to motivate students to acquire knowledge and skills autonomously and collaboratively.(10)
The main characteristics of this methodology are critical thinking, the practical application of knowledge, creative problem-solving, and the development of unique and essential skills for training students in medical education.(11) Thus, this strategy is presented as innovative in a critical and self-training sense.
According to (12), PBL has revolutionized several fields of study, including medical education, although it has also spread to other disciplines such as law, administration, and even engineering; however, for the field of medicine, it can be fundamental for the development of professional skills in doctors.(3)
In particular, for teaching and learning in the field of medicine, the PBL methodology is almost ideally suited due to the complex nature and practice of this discipline, mainly because through it, problems can be developed that are representative of doctors, as well as preparing students for clinical reasoning and decision making in real environments.(13)
In this sense, PBL encourages and improves autonomous learning, which is considered indispensable for medical professionals, in addition to allowing the integration of knowledge from various disciplines that help in the analysis of the problems that arise in such a way that it not only improves the educational process but also prepares students to be competent and reflective, enabling them to face the challenges of modern medical care.(14)
In order to carry out a PBL correctly, the teacher must first develop representative problems, such as involving a patient with multiple symptoms that the students must diagnose and treat. Subsequently, small groups are formed in which discussion and collaboration are facilitated. In this case, the role of the teacher is more one of guidance and support, allowing the students to direct their own learning.
It is also important for the teacher to identify the learning needs. This can be done when the students discuss the problem and identify gaps in their knowledge that need to be filled in order to resolve the problem successfully. The students must then carry out independent research to gather the required information. Here, they can apply the review of medical literature, database consultation, or discussions with experts in the field.
At the end of the PBL application, a synthesis must be carried out, and solutions to the problem must be found, integrating what has been learned to formulate diagnoses, treatments, and follow-up strategies. It is also essential to evaluate the knowledge acquired and the skills developed. In this sense, continuous feedback from the teacher is crucial, as it improves focus and understanding.(10)
Use of ICT and PBL
With the increasing digitization of education, PBL is also adapting to the online environment, as digital educational platforms are beginning to incorporate elements of virtual PBL, allowing for greater flexibility and accessibility for students worldwide. Furthermore, with the growing interdisciplinarity in higher education, PBL is finding new applications in programs that cross traditional disciplinary boundaries, promoting an integrated and holistic approach to education.(1)
In this way, the use of ICT and PBL can enhance the teaching-learning process, as it becomes a dynamic, adaptive, and accessible methodology that strengthens the development of critical skills and the practical application of knowledge, facilitating collaborative support.(5)
With ICT, students can access digital resources, which they can use to research and solve the problems posed in the PBL. These resources provide perspectives and sources of information that complement learning. Students can also use collaborative platforms that aid communication and teamwork, as well as share documents and manage tasks.
Specifically for the medical field, they can provide advanced simulations and software that allow students to explore realistic scenarios and do virtual experiments, which can appeal to learners, as well as experiment in a controlled and safe environment.(15)
Various technologies, such as adaptive learning platforms, augmented and virtual reality, discussion forums and chats, and applications, allow for digital evaluation and feedback; however, the use of these devices and technologies in the field of medical education is still poorly documented.(16)
METHOD
A methodology that integrated documentary analysis and theoretical reflection was adopted to carry out the critical reflection(17) on the implementation of Problem-Based Learning (PBL) combined with the use of ICT.
A systematic literature search was carried out in various databases such as Google Scholar, Scopus, and PudMed; inclusion criteria corresponded to studies published in Spanish in the last ten years, and articles that provided empirical data or theoretical analysis on the problem in question were selected. Finally, data was extracted on the challenges of implementing PBL and using ICT for teaching and learning in medicine.
For the critical analysis, content analysis was used to identify recurring themes, and the following categories were obtained:
· Teacher training.
· Resistance to change.
· Creation of teaching material.
· Evaluation of PBL.
· ICT and PBL.
Based on the above, the coherence of the arguments presented in the sources consulted was evaluated, the theoretical and empirical basis was considered, and consensus and discrepancies between the studies were identified. Subsequently, we reflected on how the findings related to current practice in medical education. The relevance of the challenges of PBL and ICT in global trends in higher education and technology was analyzed.
In the final stage, conclusions and recommendations were drawn based on the reflection and analysis.
RESULTS
Below, we present the results obtained from the critical reflection on Problem-Based Learning and the use of ICT. Figure 1 shows a diagram with the main areas of impact, benefits, and challenges that interact and contribute to the educational process.
The main challenges are teacher training, evaluating PBL with the use of ICT, and the need for technological infrastructure that allows for the proper development of the active methodology; in addition to this, the benefits are shown, such as the importance of teachers being motivated and committed to their students and interested in improving their competencies and skills. In terms of areas of impact, these include communication and collaboration between teachers and students and implementing strategies and technologies that enable the personalization of learning.
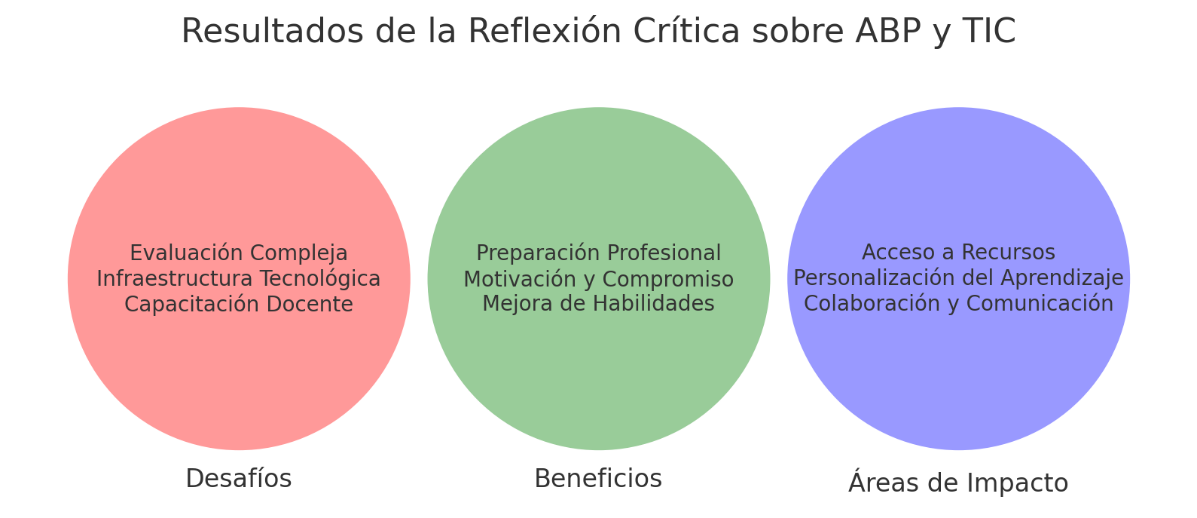
Figure 1. Results of the critical reflection on PBL and ICT
Figure 2 shows the challenges of implementing PBL and the use of ICT in medical education. According to the documents analyzed, each bar represents the level of challenge faced by both teachers and higher education institutions offering medical degrees. Each bar shows the level of challenge, with five being the most critical, as is the case with technological infrastructure, which highlights the need for technologies to be used to support PBL.As we have seen previously, another of the major challenges is teacher training and the evaluation of learning through ICT and the use of the PBL methodology, which ranked fourth due to the need for continuous teacher training focusing on the development of adaptive assessment tools.
The categories of resistance to change and creation of teaching materials are also presented, with a challenge level of 3 indicating significant problems. Still, they are potentially more manageable through management strategies and institutional collaboration.
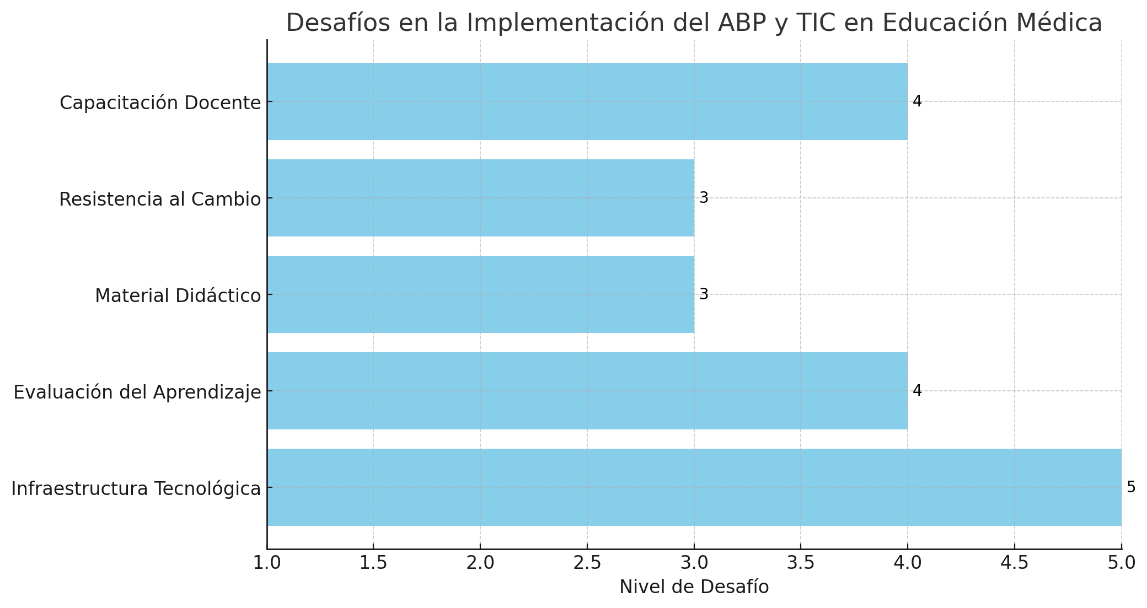
Figure 2. Results of the critical reflection on PBL and ICT
This critical reflection emphasizes the importance of having an adequate and reliable ICT infrastructure since the lack of appropriate technological resources severely limits the effective implementation of PBL and ICT. This reflects the complexity of integrating PBL and ICT into medical education and highlights the need to address these challenges proactively and systematically to improve the training of future medical professionals.
CONCLUSIONS
Applying PBL with the use of ICT in the medical field represents a pedagogical innovation that promises to transform the training of future doctors and is therefore considered to be of great relevance for education. Through critical reflection on this methodology, several key challenges have been identified, and areas of opportunity to overcome them have been identified, such as offering adequate training to those who use PBL, developing high-quality materials, and innovating how learning and teaching are evaluated.
Based on the literature review, implementing a PBL methodology could align pedagogical models with current trends in teaching university medical sciences, providing teachers with new tools for their practice.
In this sense, integrating ICT into the application of PBL requires a change in pedagogical beliefs and a shift in approaches to building them more collaboratively. This situation demands not only time and resources but also a commitment from the institutions to support the teachers in these changes. The above coincides with what has been pointed out(11) when expressing the need to turn towards a pedagogical training approach for the teacher.
To create these complex scenarios, it is concluded, as in (5), that the teacher and the institution itself must be aware of the time it will take them to make these changes and design the PBL methodology using technological tools, so it is considered essential to form multidisciplinary teams to support the design of the cases that the students will solve, so that they are constantly updated and that cutting-edge technology is used.(18)
Another aspect that is concluded is that there are still teachers, especially in the medical area, who are not familiar with technological tools for evaluation or even some with the design of the PBL methodology. Therefore, a focus is required on this aspect since regardless of how teaching is developed, if the teachers are not prepared to implement it, learning could be diminished.
In this respect, educational institutions must also emphasize infrastructure since even the most innovative teaching plans cannot be implemented effectively without this tool. In addition, they must not only acquire but also install it, maintain it, and keep it updated. They must also have trained and expert staff who can support teachers in optimizing its use.
Finally, combining PBL and ICT is a powerful synergy that improves learning effectiveness. It prepares students to better understand their field of study and supports them in developing essential skills for their professional practice. It is also important to highlight that students are prepared to be critical thinkers and solve problems effectively in their work environment by using this methodology.
Critical reflection allows for a deep identification of the opportunities and challenges of using PBL and ICT. This provides a solid basis for the development of strategies that improve implementation. Critical reflection also supports the generation of literature, which, in this case, is scarce since, in the search carried out, there were few studies that jointly showed the subject dealt with in this paper.
The limitations of this reflection are the generalization and applicability of its findings, as the data are merely qualitative and may be subject to personal bias. There is also a possible lack of depth in the analysis of causes and solutions and, above all, the absence of empirical evaluation. Therefore, it is suggested that future research be more rigorous and continuously updated to maintain the relevance of this methodology in a changing context.
The prospects for the integration of PBL and ICT in medical education are considered to have enormous potential for transforming medical training since, as technologies advance, PBL can also become more effective and accessible; however, to achieve this, educational institutions must proactively address the challenges identified and ensure that they are in line with the changing needs of students and educational innovations.
BIBLIOGRAPHIC REFERENCES
1. Buzón García, O., & Romero García, C. (2021). Metodologías activas con TIC en la educación del siglo XXI. Madrid: Dykinson.
2. Cárdenas Cordero, N. M., Guevara Vizcaíno, C. F., Moscoso Bernal, S. A., & Álvarez Lozano, I. (2023). Metodologías activas y las TIC en los entornos de aprendizaje. Conarado, 19(91), 397-405. Disponible en http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1990-86442023000200397&lng=es&nrm=iso>. accedido en 06 marzo 2025. Epub 30-Abr-2023
3. Manso López, A. M., & Garrido Tapia, E. (2021). Aprendizaje Basado en Problemas: una estrategia en la educación médica superior cubana. EdumedHolguín. Disponible en https://edumedholguin2021.sld.cu/index.php/edumedholguin/2021/paper/view/219/0
4. Vidal Villa, A., Illesca Pretty, M., González Osorio, L., & Godoy-Pozo, J. (2023). Aprendizaje basado en problemas en modalidad virtual con tutor par en pandemia: Opinión estudiantes primer año de medicina. Revista médica de Chile, 151(5), 551-559. doi: https://dx.doi.org/10.4067/s0034-98872023000500551
5. Tapia-Rodríguez, R. A., Cortes-Roldan, D. A., Cruz-Hernández, P. A., Chávez-Martínez, L. C., & Camacho-yLópez, S. M. (2022). Aprendizaje basado en problemas, un desafío para la praxis académica en medicina. XIKUA Boletín Científico de la Escuela Superior de Tlahuelilpan, 10(19), 42-46. doi: https://doi.org/10.29057/xikua.v10i19.8113
6. Hechavarria, T., García, C., & Tosar, P. (2021). Referentes históricos de la medicina natural y tradicional para la formación del residente de medicina interna. MediSan, 25(02), 489-506. Obtenido de https://www.medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=104793
7. Arana Delgado, J. C., Carpio Vásquez, W. d., & Carpio Vásquez, W. N. (2022). Aprendizaje Basado en el Problema Modalidad Virtual en pregrado de Medicina Humana. Sinergias educativas. doi: https://doi.org/10.37954/se.vi.243
8. Amaya Chávez , D. (2021). Diseño, análisis y evaluacion de un método de aprendizaje basado en problemas mediado por tecnologías interactias desarrollado con estudiantes de ingeniería. Granada, España: Universidad de Granada.
9. Corzo Camacho, M. A. (2022). Construcción de un módulo educativo para la enseñanza de los grandes síndromes geriátricos por medio del uso de aprendizaje basado en problemas y tecnologías de la información y la comunicación. Universidad Nacional de Colombia.
10. Julca-Asto, J. M., & Duran-Llaro, K. L. (2022). El método Aprendizaje Basado en Problemas (ABP) en el proceso enseñanza –aprendizaje. Polo del Conocimiento: Revista científico-profesional, 7(6), 2310-2321.
11. Torres Paez, F. F., & Londoño, J. A. (2024). Aportes del Aprendizaje Basado en Problemas al logro de aprendizajes significativos en la formación en Medicina. Revista Española de Educación Médica, 5(4). doi: https://doi.org/10.6018/edumed.619851
12. Luy-Montejo, C. (2019). El Aprendizaje Basado en Problemas (ABP) en el desarrollo de la inteligencia emocional de estudiantes universitarios. Propósitos y Representaciones, 7(2), 353-383. doi: https://doi.org/10.20511/pyr2019.v7n2.288
13. Gutiérrez Gutiérrez, B. (2021). El aprendizaje basado en problemas como mecanismo de formación docente: caso alumnos LEI BUAP. Ciencia Latina Revista Multidisciplinar, 5(5), 9531-9556. doi: https://doi.org/10.37811/cl_rcm.v5i5.1000
14. Lozano Terrón, C., Lorenzo Álvarez, R., & Sendra Portero, F. (2024). Una experiencia de aprendizaje basado en problemas en un rotatorio de radiología para estudiantes de sexto curso de Medicina. Radiología, 66(3), 207-218. doi: https://doi.org/10.1016/j.rx.2022.10.012
15. Velásquez, A. & Universidad Pontificia Bolivariana Experiencias frente al uso de las TIC en el proceso de aprendizaje de estudiantes de medicina del semestre básico de la Fundación Universitaria San Martín, Sede Sabaneta. [Internet]. 2023. [citado: 2025, marzo] Disponible en: http://hdl.handle.net/20.500.11912/11154
16. Steven García, L., Zúñiga, J., & Perez-Trejos, L. E. (2021). Las Tecnologías E-Learning y TIC en el Aprendizaje a Largo Plazo de la Anatomía Humana en Estudiantes del Área de la Salud: Una Revisión de la Literatura. International Jourgnal of Morphology, 39(2), 396-400. doi: https://dx.doi.org/10.4067/S0717-95022021000200396
17. Menéndez, R. C. (2012). El concepto metodológico de reflexión en Husserl y en Ricoeur. Investigaciones Fenomenológicas (9), 249-268.
18. Palomino Alca, J. T., & Osorio Vidal, V. G. (2023). El aprendizaje basado en problemas para el logro de competencias en educación superior. Revista Dilemas Contemporáneos(2). doi: https://doi.org/10.46377/dilemas.v2i10.3484
FINANCING
The authors did not receive financing for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: María del Rocío Carranza Alcántar.
Data curation: Claudia Islas Torres.
Formal analysis: Rosana Ruíz Sánchez.
Research: María del Rocío Carranza Alcántar, Rosana Ruíz Sánchez.
Methodology: Claudia Islas Torres.
Project management: María del Rocío Carranza Alcántar.
Supervision: Rosana Ruíz Sánchez.
Validation: Claudia Islas Torres.
Drafting - original draft: María del Rocío Carranza Alcántar.
Writing - proofreading and editing: María del Rocío Carranza Alcántar.