doi: 10.56294/mw2024557
REVIEW
Nursing approach to puerperal psychosis associated with heart disease: Integrated care for mental and cardiac health
Abordaje enfermero de la psicosis puerperal asociada a cardiopatía: Atención integrada a la salud mental y cardiaca
William Bedoia de
Albuquerque Junior1 ![]() *, Isabella
Cristini Amaral de Almeida1
*, Isabella
Cristini Amaral de Almeida1 ![]() *, Patrícia
Facina Soares Caracol1
*, Patrícia
Facina Soares Caracol1 ![]() *, Edilene
Ramos Correia Rocha1
*, Edilene
Ramos Correia Rocha1 ![]() *, Aline
Albuquerque Cirimbelli Souza2
*, Aline
Albuquerque Cirimbelli Souza2 ![]() *, William
Alves dos Santos1
*, William
Alves dos Santos1 ![]() *
*
1Faculdade Anhanguera de Jacareí, Enfermagem. Jacareí, Brasil.
2Faculdade Anhanguera de Jacareí, Psicologia. Jacareí, Brasil.
Cite as: de Albuquerque Junior WB, Amaral de Almeida IC, Facina Soares Caracol P, Ramos Correia Rocha E, Cirimbelli Souza AA, Alves dos Santos W. Nursing approach to puerperal psychosis associated with heart disease: Integrated care for mental and cardiac health. Seminars in Medical Writing and Education. 2024; 3:557. https://doi.org/10.56294/mw2024557
Submitted: 06-11-2023 Revised: 12-03-2024 Accepted: 02-07-2024 Published: 03-07-2024
Editor:
PhD.
Prof. Estela Morales Peralta ![]()
Corresponding author: William Bedoia de Albuquerque Junior *
ABSTRACT
Introduction: puerperal psychosis is a serious psychiatric condition that can arise after childbirth, characterized by hallucinations, delusions and agitated behaviour. Although rare, the severity of the symptoms requires immediate attention. Risk factors include a history of mental disorders and birth complications. Treatment involves hospitalization, antipsychotic medication and psychosocial support, and the presence of pre-existing heart disease aggravates the condition, requiring specialized nursing care. Multidisciplinary collaboration is essential for the well-being of mother and baby. This literature review examines the relationship between puerperal psychosis and heart disease, offering insights for clinical practice. To identify nursing behaviors in women with puerperal psychosis associated with heart disease.
Method: bibliographic review based on articles from the LILACS and BDENF databases, published in the last 6 years. Exclusion criteria: articles in languages other than those used in the research, more than 10 years old or incomplete. The search involved the DeCS.
Results: puerperal psychosis associated with heart disease requires a multidisciplinary approach. The role of nursing is essential in education, emotional support and early monitoring. Adherence to treatment faces challenges such as social stigma and lack of resources.
Conclusion: the study highlights the importance of nursing care for women with puerperal psychosis and heart disease, emphasizing the need for integrated health policies and professional training to improve clinical outcomes.
Keywords: Psychotic Disorders; Postpartum Period; Nursing; Psychiatry; Cardiopathies.
RESUMEN
Introducción: la psicosis puerperal es un trastorno psiquiátrico grave que puede aparecer tras el parto, caracterizado por alucinaciones, delirios y comportamiento agitado. Aunque es poco frecuente, la gravedad de los síntomas requiere atención inmediata. Los factores de riesgo incluyen antecedentes de trastornos mentales y complicaciones en el parto. El tratamiento implica hospitalización, medicación antipsicótica y apoyo psicosocial, y la presencia de cardiopatías preexistentes agrava el cuadro, por lo que requiere cuidados de enfermería especializados. La colaboración multidisciplinar es esencial para el bienestar de la madre y el bebé. Esta revisión bibliográfica examina la relación entre la psicosis puerperal y la cardiopatía, ofreciendo ideas para la práctica clínica. Identificar las conductas de enfermería en mujeres con psicosis puerperal asociada a cardiopatía.
Método: revisión bibliográfica basada en artículos de las bases de datos LILACS y BDENF, publicados en los últimos 6 años. Criterios de exclusión: artículos en idiomas diferentes de los utilizados en la investigación, con más de 10 años de antigüedad o incompletos. La búsqueda incluyó el DeCS.
Resultados: la psicosis puerperal asociada a cardiopatía requiere un abordaje multidisciplinar. El papel de la enfermería es esencial en la educación, el apoyo emocional y el seguimiento precoz. La adherencia al tratamiento se enfrenta a retos como el estigma social y la falta de recursos.
Conclusión: el estudio pone de manifiesto la importancia de los cuidados de enfermería a mujeres con psicosis puerperal y cardiopatía, enfatizando la necesidad de políticas sanitarias integradas y de formación profesional para mejorar los resultados clínicos.
Palabras clave: Trastornos Psicóticos; Periodo Posparto; Enfermería; Psiquiatría; Cardiopatías.
INTRODUCTION
Puerperal psychosis or postpartum psychosis (PPP) is a serious psychiatric disorder that affects some women after childbirth. Characterized by psychotic symptoms such as hallucinations, delusions, disorganized thinking and agitated behaviour, this condition usually manifests itself in the first few weeks after the baby is born. The incidence is relatively low, but the severity of the symptoms demands immediate attention. Risk factors include a personal or family history of mental disorders, birth complications and significant stress.(1) Early diagnosis and therapeutic intervention are crucial to ensure the mother’s well-being and the baby’s safety. Treatment often involves hospitalization, antipsychotic medication and psychosocial support. Understanding the triggering factors and sensitizing health professionals are key to an effective and compassionate approach to puerperal psychosis.(2) When this condition is associated with pre-existing heart disease, the complexity of the situation increases considerably, requiring a thorough and specialized nursing approach.(3)
Although it is a rare disease, puerperal psychosis is one of the most serious puerperal illnesses because it is characterized by a rapid worsening of mental health, causing women to experience delusions, hallucinations, emotional instability and confused thoughts.(2) The postpartum period is already an emotionally vulnerable phase for many women, and adding puerperal psychosis to the equation intensifies psychological suffering. When this condition occurs in conjunction with pre-existing heart disease, it creates a complex and challenging clinical scenario that demands an integrated healthcare approach.(4) The epidemiology of puerperal psychosis in Brazil reflects a significant concern for maternal mental health. Studies indicate a variable prevalence, with estimates generally hovering around 1 to 2 cases per 1,000 births. Despite the low incidence compared to other postpartum psychiatric disorders, puerperal psychosis is recognized as a medical emergency, requiring immediate intervention due to its severity.(5) Puerperal psychosis, a serious psychiatric condition that occurs after childbirth, can be aggravated by various medical conditions. Affective disorders, such as bipolar disorder, and anxiety disorders can intensify the emotional stress, while schizophrenia and a history of psychotic disorders significantly increase the risk. Thyroid disorders, such as hypothyroidism or hyperthyroidism, can impact the endocrine system, contributing to hormonal imbalances associated with puerperal psychosis. Epilepsy, affecting the neurological system, is also correlated with a higher risk. Autoimmune diseases, such as lupus, can involve multiple systems, including the nervous and immune, contributing to psychotic vulnerability. Severe infections, by affecting the immune and nervous systems, can trigger or aggravate psychotic symptoms. The presence of pre-existing heart disease, which encompasses a variety of cardiac conditions such as heart failure, hypertension, congenital or acquired heart disease, amplifies the complexity of the clinical picture.(6) Emotional imbalance can trigger adverse responses, so women facing PPP associated with myocardial disease face a higher risk of complications.(4) In addition, the medication used to treat puerperal psychosis should be carefully evaluated, taking into account its cardiovascular safety. Nurses play a crucial role in the early identification of puerperal psychosis in women with pre-existing heart disease.(7)
Careful observation of the patient’s behavior, emotional response and signs of worsening symptoms is essential. Nurses should be alert to any changes in sleep patterns, appetite and mood, as well as any signs of confusion or agitated behavior. Identifying puerperal psychosis at an early stage can allow for more effective intervention and minimize the risk of cardiovascular complications.(8) It is unquestionable that nurses contribute to a multidisciplinary team that includes cardiologists, psychiatrists, psychologists and social workers, due to the serious nature of puerperal psychosis associated with heart disease. Effective management requires continuous communication and coordination between these professionals to ensure that all the woman’s needs are fully met.(9)
Nurses play an extremely important role in educating women about the importance of managing their heart condition and in promoting strategies for coping with emotional stress.(8) Taking into account heart conditions and psychotic symptoms, nurses have a responsibility to provide personalized care to women.(7) This includes administering psychotropic medication, constantly monitoring vital signs and evaluating the response to treatment. Since it is a complex task, this calls for specialized nursing skills and multidisciplinary collaboration to address postpartum psychosis in women with heart disease.(10) Nurses play a vital role in the early identification, care management and promotion of patient recovery, contributing significantly to the health and safety of women facing heart disease.(8) Special attention and understanding of clinical variants must be given to ensure that these women receive the support they need at this critical time in their lives.
Objective
To identify nursing procedures for women with puerperal psychosis associated with heart disease.
METHOD
This article consists of an integrative review of the literature with an exploratory and descriptive approach to data, which deals with nursing procedures for women with puerperal psychosis associated with heart disease.
To delimit the project, we used the PCC strategy, which consists of a specific strategy for exploratory approaches to the topic to be addressed. Where P (Population): Women in the postpartum period; C (concept): psychotic disorders OR Cardiopathies OR Psychiatry and C (context): Nursing, as described, below (table 1).
The method used to search for and select the articles followed specific criteria to guarantee the quality and relevance of the studies included. The Virtual Health Library (VHL) was used as the main data source. The Health Sciences Descriptors (DeCS) to be used in the search included: “psychotic disorders”, “postpartum period”, “nursing”, “psychiatry” and “heart disease”. The strategy for combining the terms used the Boolean operators “OR” to correlate the subject descriptors. Therefore, the search strategy for definitions based on the aforementioned DeCS was combined with Boolean operators (AND and OR) according to the objective of the review.
The search for this study began in November 2023, and the LILACS (Latin American and Caribbean Health Sciences Literature) and BDENF (Nursing Database) databases were mainly selected for the search for articles. The inclusion criteria were: availability of the full text, articles published in the last 6 years in Portuguese and English and observational studies. The exclusion criteria were articles in languages other than Portuguese and English, studies published more than 10 years ago, systematic reviews and articles that were not complete.
The articles were screened in tiers, with the first tier excluding articles based on the title and abstract, and the second tier reviewing all the articles to check that they met the inclusion criteria. A reviewer was also used in the selection to increase the fidelity of the articles selected, to the point of avoiding disagreements.
To check the quality of the article, risk of bias tools such as the Cochrane Risk of Bias Tool or the Newcastle-Ottawa Scale were not used, as this was an integrative review and not a systematic literature review. However, they were reviewed by another reviewer who took part in the work so that any disagreements could be resolved.
Data was extracted and collected using the free Rayyan ® platform for screening and categorizing articles in systematic reviews, but it can also be useful in integrative reviews.
The authors declare that they have no conflicts of interest that could influence the results of this study.
|
Table 1. Descriptors used to search the data sources. Jacareí, São Paulo, Brazil, 2023 |
|
|
PCC |
DeCS |
|
Population |
Postpartum period |
|
|
AND |
|
Concept |
Psychotic disorders OR Heart disease OR Psychiatry |
|
|
AND |
|
Context |
Nursing |
RESULTS AND DISCUSSION
A table was created with the main findings (table 2) used in this review. The choice of a tabular format allows the information to be organized and presented in a clear and objective way, making it easier to compare the studies. The table presents the objectives of each study, providing a detailed analysis of the evidence related to the topic. This approach contributes to the discussion and substantiation of the conclusions of this study. Analysis and data collection were carried out using the PRISMA® flowTable, following the recommendations of the protocol (figure 1).
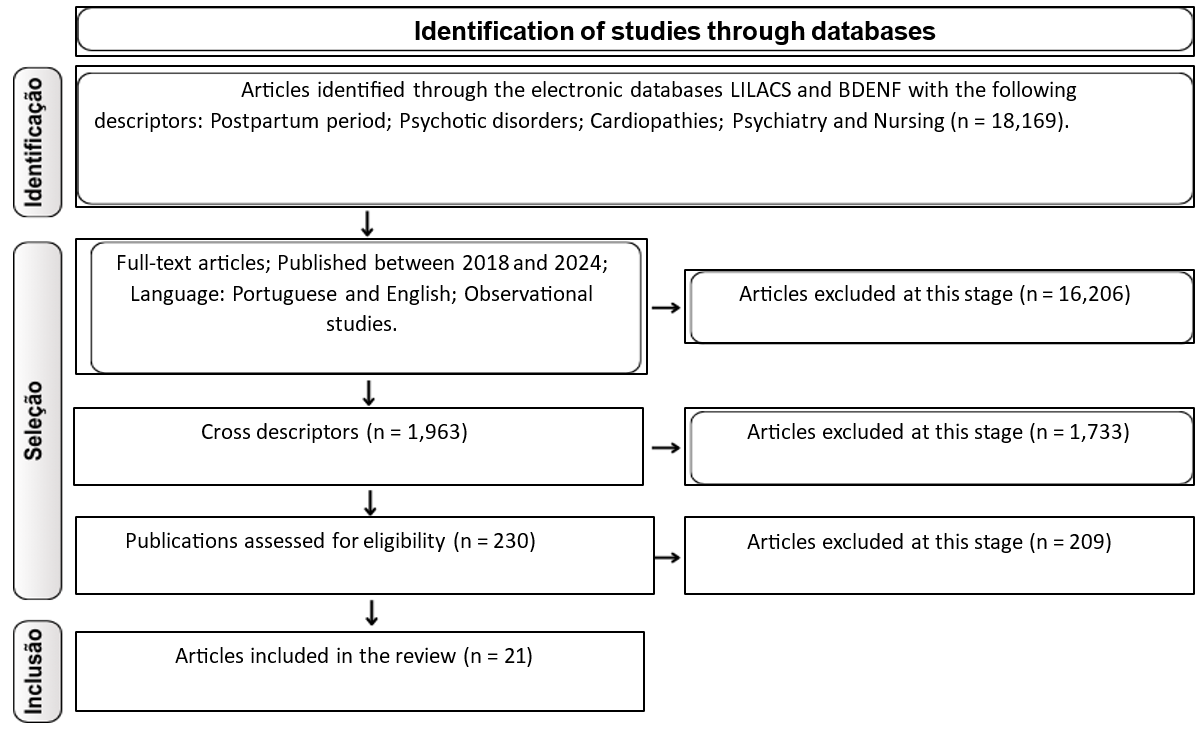
Figure 1. Flowchart of bibliographic information obtained at different stages of the systematic review
|
Table 2. Bibliographic findings used to construct this paper |
|
|
Author/Year |
Objective |
|
Santos. 2022.(1) |
To analyze the clinical characteristics and risk factors for Postpartum Depression (PPD). |
|
Rodriguez-Cabezas l: Clark C. 2018.(2) |
Identify patients who need treatment before their symptoms become severe and become a psychiatric emergency in pregnancy and postpartum. |
|
Machava, Moséstia David. 2019.(3) |
To assess health professionals’ knowledge of peripartum cardiomyopathy. |
|
Davies c. 2020.(4) |
To provide a comprehensive and up-to-date synthesis of the evidence on the association between prenatal or perinatal risk and protective factors and psychotic disorders. |
|
Zhang Y. et al. 2020.(5) |
To provide a comprehensive overview of postpartum psychosis, highlighting its rarity, clinical characteristics and associated risk factors. |
|
Wijayanto, M. A. et al. 2024.(6) |
To evaluate the results of subsequent pregnancies in women with heart disease. |
|
Costa ALV. 2021.(7) |
Knowing, analyzing and understanding the characteristics of puerperal women contributed to a deeper understanding of the subject and to reflecting on the main points to be evaluated in terms of systematized and individualized care, in order to provide a better quality of life for these mothers. |
|
Cardoso. 2019.(8) |
Recognize the nurse’s role in preventing harm to the puerperal woman and her child, by diagnosing acquired postpartum mental disorders early, such as puerperal psychosis and its consequences. |
|
Fraga. 2022.(9) |
To explain and describe the interventions of the PNP technique, analyzing in the literature whether there is evidence of the effectiveness of this psychological tool in the prevention of puerperal disorders, based on an investigation through a bibliographic review. |
|
Teixeira, C.S. 2019.(10) |
To identify the evidence on aspects of pregnancy and puerperium in women with mental disorders in Brazil. |
|
Alves WMC. et al. 2022.(11) |
To analyze how psychological prenatal care can be a comprehensive maternal health care strategy. |
|
González-Blanco L. et al. 2019.(12) |
To explore the experiences, needs and preferences for psychological intervention from the perspective of women with postpartum psychosis and from the perspective of family members. |
|
Assef. 2021.(13) |
To describe and discuss the main psychiatric syndromes that can occur during the puerperium, identifying the factors that cause this pathology and reinforcing the importance of welcoming and humanized care for puerperal women and their babies during this period. |
|
Teixeira P da C. et al. 2019.(14) |
Point out the main complications during the puerperium and describe the nursing care needed to deal with these complications. |
|
Silva, E. da et al. 2022.(15) |
To identify the perception of nurses at a maternity hospital in the interior of São Paulo regarding their knowledge and the way they act in relation to hypertensive diseases specific to pregnancy, from their detection to the puerperium. |
|
Anjos, A. M. dos; Gouveia, H. G. 2019.(16) |
To analyze the practice of the presence of a companion during the parturition process. |
|
Pereira CA. et al. 2022.(17) |
To identify the care provided to women admitted to the Intensive Care Center due to peripartum cardiomyopathy. |
|
Moretto MLT. et al. 2018.(18) |
To investigate the perception of professional psychologists and cardiac patients about psychosocial factors associated with the disease and possibilities for clinical psychological management. |
|
Pavani J. et al. 2020.(19) |
To assess the nursing staff’s knowledge of puerperal mental suffering and provide support for educational actions. |
|
Santos H. et al. 2020.(20) |
Carry out a literature review to identify health care for mental disorders during the puerperium. |
|
Silva EM. et al. 2021.(21) |
Understand the integrality of nursing care from prenatal to puerperium. |
According to Santos et al. (2022) and Assef et al. (2021) puerperal psychosis is a serious condition that affects women in the postpartum period, characterized by psychotic symptoms such as hallucinations, delusions and disorganized thinking. When associated with heart disease, this condition becomes even more complex and challenging to treat, requiring a multidisciplinary approach and specialized care. In this study, we sought to identify the most effective nursing procedures for managing these two concomitant conditions.(1,13)
The results revealed that education and emotional support are fundamental pillars in the care of women with puerperal psychosis and heart disease. Nurses play a crucial role in providing clear information about both conditions, their treatments and possible complications. In addition, the emotional support offered by nurses helps patients cope with the stress and anxiety associated with these conditions, thus
promoting better adherence to treatment and a more positive healthcare experience. One aspect highlighted in the research was the importance of integrated monitoring of psychotic and cardiac symptoms. According to the authors Cardoso et al. (2019) and Silva et al. (2021) nurses play a central role in this process, carrying out regular assessments and using standardized assessment scales to detect any changes in symptoms early on. This allows for rapid and effective intervention, helping to prevent serious complications and improve patients’ clinical outcomes.(8,23)
An interdisciplinary approach is essential for the effective care of women with puerperal psychosis and heart disease. Collaboration between nurses, doctors, psychologists, social workers and other health professionals is key to ensuring comprehensive and coordinated care. Effective communication between team members is crucial to ensure that all patients’ needs are met and that treatment plans are adapted according to their specific conditions, point out the authors Gonzalés et al. (2019) and Moretto et al. (2018) .(12,20)
According to Davies et al. (2020) and Fraga et al. (2022) treatment adherence has been identified as a significant challenge in the care of women with puerperal psychosis and heart disease. Nurses play an important role in providing ongoing support and education to patients, clarifying doubts and concerns about treatment. Strategies to improve adherence, such as developing individualized treatment plans and involving the family in the care process, have been shown to be effective in promoting better clinical outcomes.(4,9)
Although nursing conduct plays a crucial role in the care of women with puerperal psychosis associated with heart disease, we face several challenges in the integrated management of these conditions. According to Teixeira et al. (2019) and Zhang et al. (2020) the lack of adequate resources, the lack of access to specialized services and the social stigma associated with mental illness are some of the obstacles faced by patients and health professionals. It is essential to address these challenges through health policies that prioritize the integration of mental and physical health care, as well as the provision of adequate resources and support for patients and their families.(5,10)
A framework containing nursing behaviors was built in order to optimize the management of this condition. This tool provides a systematic representation of the recommended interventions, facilitating the implementation of care strategies. The framework is a fundamental resource for health professionals, allowing for an organized and grounded approach to meeting patients’ needs.
The ideas for constructing this Table were taken from the NANDA and NIC classifications, which provide a structured basis for nursing practice. These references were fundamental in organizing the information, making it easier to understand the interventions and expected results.
|
Table 3. Nursing care for women with PPP |
|
|
Nursing conduct |
Description |
|
Initial assessment |
Carry out a full assessment of the patient’s psychiatric condition, including the severity of psychotic symptoms. Assess the patient’s cardiac condition, including the presence of heart disease, medical history and medications in use. |
|
Cardiac monitoring |
Continuously monitor the patient’s vital signs, including heart rate, blood pressure and heart rhythm. Watch carefully for signs of angina, dyspnea or other symptoms of worsening heart disease. |
|
Medication |
Administer prescribed psychotropic medication, according to medical advice, to control psychotic symptoms. Ensure that psychotropic medications do not interact negatively with cardiac medications. |
|
Emotional support |
Provide emotional support to the patient, understanding the distressing nature of puerperal psychosis. Offer psychological counseling and referral to support groups, as necessary. |
|
Patient education |
Educate the patient about her heart condition and the importance of adherence to cardiac treatment. Inform about the risks and benefits of psychiatric treatment during the puerperal period. |
|
Stress management |
Teaching stress management techniques, such as relaxation and meditation, to help reduce anxiety and stress. Encourage a calm and supportive environment for the patient. |
|
Communication with the team |
Maintaining effective communication with the multidisciplinary team, including cardiologists and psychiatrists. Sharing critical information about the patient’s physical and mental health to ensure integrated treatment. |
|
Emergency preparedness |
Develop an action plan for emergencies, such as worsening heart disease or psychotic symptoms. Train nursing staff to respond quickly to crises. |
CONCLUSION
It was concluded that this study highlighted the importance of nursing behaviors in caring for women who face the complexity of puerperal psychosis associated with heart disease. By identifying these behaviors, it was possible to highlight the importance of education, emotional support, integrated symptom monitoring, an interdisciplinary approach and strategies to promote adherence to treatment. These aspects proved to be fundamental to providing comprehensive, quality care, aimed not only at physical recovery, but also at the emotional and mental well-being of patients. However, it is crucial to recognize the challenges faced in the integrated management of these conditions, including the scarcity of resources, limited access to specialized services and the stigma associated with mental illness. Overcoming these obstacles requires an ongoing commitment to health policies that prioritize the integration of mental and physical health care, as well as investments in training programs for nursing professionals and other members of the healthcare team.
By strengthening and improving nursing practices, we can significantly improve the clinical outcomes and quality of life of women facing puerperal psychosis associated with heart disease, and provide the support and care needed for a complete and lasting recovery.
REFERENCES
1. Santos FS, Gomes LSM, Lima EP, Gomes JP, da Silva CAM, Fernandes PS, et al. Características clínicas e fatores de risco da depressão pós-parto: uma revisão de literatura. Rev Eletrônica Acervo Médico. 2022;5. doi:10.25248/reamed.e10041.2022.
2. Rodriguez-Cabezas L, Clark C. Psychiatric emergencies in pregnancy and postpartum. Clin Obstet Gynecol. 2018;61(3):615-627. doi: 10.1097/GRF.0000000000000377.
3. Machava MD. Avaliação do conhecimento dos profissionais de saúde sobre a cardiomiopatia periparto na área de saúde do Hospital Geral José Macamo na cidade de Maputo. 2019. 65 p. Disponível em: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1224350.
4. Davies C, Segre G, Estradé A, Radua J, De Micheli A, Provenzani U, et al. Prenatal and perinatal risk and protective factors for psychosis: a systematic review and meta-analysis. Lancet Psychiatry. 2020;7(5):399-410. doi: 10.1016/S2215-0366(20)30057-2.
5. Zhang Y, Liu L, Yang Y, et al. Social support and postpartum depression: a meta-analysis. In: Duran-Perez L, ed. Postpartum Psychosis: A Comprehensive Approach. 1st ed. Cham: Springer; 2020. p. 131-141. doi: 10.1007/978-3-030-91832-3_9.
6. Wijayanto MA, Pranata R, Raharjo SB, et al. Outcomes of subsequent pregnancy in women with peripartum cardiomyopathy: a systematic review and meta-analysis. Open Heart. 2024;10(1). doi:10.1136/openhrt-2024-002626.
7. Costa ALV da, Azevedo FHC. Puerperium and nursing care: a systematic review. Res Soc Dev. 2021;10(14). DOI: 10.33448/rsd-v10i14.22365.
8. Cardoso BV, Da Silva SJ, Melo RS, De Mora Silva H, Teodosio VF. A assistência de enfermagem no diagnóstico precoce da psicose puerperal. In: Anais da Mostra de Pesquisa em Ciência e Tecnologia 2019; Fortaleza, CE. 2019. Disponível em: https://even3.com.br/anais/mpct2019/158437-a-assistencia-de-enfermagem-no-diagnostico-precoce-da-psicose-puerperal/
9. Fraga MP, de Oliveira LC, Macedo DCC. Pré-natal psicológico para gestantes como prevenção aos transtornos puerperais. PsicoDebate. 2022; 19:798. Disponível em: https://www.psicodebate.dpgpsifpm.com.br/index.php/periodico/article/view/798
10. Teixeira P da C, Simões MM de D, Santanna G dos S, Teixeira NA, Koeppe GB, Cerqueira LC da C N. Cuidados de enfermagem no período pós-parto: um enfoque na atuação do enfermeiro diante as complicações puerperais. Nursing (Ed. bras., Impr.). 2019;22(259):3436-46. Disponível em: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1095343.
11. Alves WMC, Guimarães MRP, dos Santos K. Atuação da equipe multiprofissional na prevenção e assistência à saúde mental em puérperas: uma revisão integrativa. PsicoDebate. 2022;12(1):1-9. Disponível em: https://www.psicodebate.dpgpsifpm.com.br/index.php/periodico/article/view/798.
12. González-Blanco L, Losa-García J, de León J, et al. Postpartum psychosis and mother–infant bonding: a qualitative study. BMC Psychiatry. 2019;19(1):345. doi: 10.1186/s12888-019-2378-y
13. Assef MR, Nascimento M, Chaves R. Aspectos dos transtornos mentais comuns ao puerpério. Rev Eletr Acervo Científico. 2021;29. doi: 10.25248/reac.e7906.2021.
14. Teixeira CS, Barbosa TL, Marangoni VSL, Neves ALM, Therense M. Aspectos da gestação e puerpério de mulheres com transtornos mentais. Rev Enferm UFPE on line. 2019;13. doi: 10.5205/1981-8963.2019.239705.
15. Silva E da, Moura MJ, Alexandria P, Braz L, Ornelas J, Spina G. Doenças hipertensivas específicas da gestação: percepção do enfermeiro. CuidArte, Enferm [Internet]. 2022;216–25. Available from: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1434853
16. Anjos AM dos, Gouveia HG. Presença do acompanhante durante o processo de parturição e nascimento: análise da prática. Rev Enferm UERJ. 2019;27. doi:10.12957/reuerj.2019.38686.
17. Pereira CA, Silva LAC, Santos MAF. Cuidados de enfermagem à mulher com miocardiopatia periparto: revisão integrativa. Rev Enferm Atual In Derme. 2022;96(37):1188. doi: 10.31011/reaid-2022-v.96-n.37-art.1188.
18. Moretto MLT, Pacheco A, Andrade T. Fatores psicossociais associados à doença- cardíaca e manejo clínico psicológico: percepção de psicólogos e pacientes. Ver. SBPH. 2018;20(1):7-18. Disponível em: https://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1516-08582018000100007
19. Pavani J, Lima A, Santos C, Pires D, Salgado P. “O impacto da psicose puerperal na saúde mental da mulher e na relação mãe-bebê”. Revista Brasileira de Saúde Materno Infantil. 2020;20(1):21-30. Disponível em: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1421295.
20. Santos H, Lima B, Bezerra L. “Análise das intervenções de enfermagem na psicose puerperal em uma maternidade pública”. Revista Brasileira de Enfermagem. 2020;73(1). Disponível em: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1509750
21. Silva EM, Belarmino AC, Franco RGM, Sombra ICN, Freitas ASF. Integralidade do cuidado de enfermagem do pré-natal ao puerpério. J. Health Biol. Sci. 2021;9(1):1-6. Disponível em: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1362822.
22. Haddaway NR, Page MJ, Pritchard CC, McGuinness LA. PRISMA2020: An R package and Shiny app for producing PRISMA 2020‐compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Systematic Reviews [Internet]. 27 mar. 2022 [citado em 6 ago. 2024];18(2). Disponível em: https://onlinelibrary.wiley.com/doi/full/10.1002/cl2.1230
23. Herdman TH, Kamitsuru S. NANDA International nursing diagnoses: definitions and classification, 2021–2023. Ames, IA: Wiley-Blackwell; 2021. 590 p.
24. Johnson M, Bulechek GM, Butcher HK, Dochterman JM, Maas M, Moorhead S, Swanson E. Ligações NANDA - NOC - NIC: condições clínicas: suporte ao raciocínio e assistência de qualidade. 3. ed. Rio de Janeiro: Elsevier; 2018.
FINANCING
The authors did not receive financing for the development of this research.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: William Bedoia de Albuquerque Junior, William Alves dos Santos.
Data curation: Aline Albuquerque Cirimbelli Souza, William Alves dos Santos.
Formal analysis: William Alves dos Santos.
Research: William Bedoia de Albuquerque Junior.
Methodology: William Alves dos Santos, Aline Albuquerque Cirimbelli Souza.
Project management: Patrícia Facina Soares Caracol.
Resources: Patrícia Facina Soares Caracol.
Software: Isabella Cristini Amaral de Almeida.
Supervision: William Alves dos Santos, Aline Albuquerque Cirimbelli Souza.
Validation: William Alves dos Santos.
Display: Edilene Ramos Correia Rocha.
Drafting - original draft: Patrícia Facina Soares Caracol.
Writing - proofreading and editing: William Alves dos Santos.